Abstract
Background
Female patients, abused by their partner, are heavy users of medical services. To date, valid indicators of partner abuse of women are lacking.
Aim
To outline the healthcare utilisation in family practice of women who have suffered abuse, and compare this to the average female population in family practice.
Design of study
As part of a primary study on the role of family doctors in recognising and managing partner abuse a retrospective study was performed. Anonymised data from the electronic medical records of women who have suffered abuse were collected over the period January 2001–July 2004. These data were compared to those from the average female population of the Second Dutch National Survey in General Practice 2001 (DNSGP-2).
Setting
Family practices in Rotterdam and surrounding areas in 2004.
Method
The numbers of consultations and prescriptions for pain medication, tranquillisers and antidepressants of women who have suffered abuse (n = 92) were compared to those of the female population of the DNSGP-2 (n = 210 071). The presented health problems and referrals of the studied group were examined.
Results
Pain, in all its manifestations, appeared to be the most frequently presented health problem. Compared to the female population of the DNSGP-2, in all age categories, women who have suffered abuse consult their family doctor almost twice as often and receive three to seven times more pain medication.
Conclusion
A doubled consultation frequency, chronic pain and an excessively high number of prescriptions for pain medication are characteristics of healthcare utilisation of women have been abused in this study. These findings contribute to the development of the concept of the ‘symptomatic’ female patient.
Keywords: electronic medical record, family medicine, healthcare utilisation, partner abuse
INTRODUCTION
Women who have been abused by their partner visit healthcare providers more often and use more medication than women not being abused.1–10
However to date, specific characteristics which raise suspicion of partner abuse in a female patient, have rarely been supported by evidence of the medical record.9,11–15 A study in family practice on the actual healthcare utilisation of women who have suffered abuse should contribute to the development and validation of the concept of the ‘symptomatic’ abused female patient.
The aim of this study was to find out how women who have suffered abuse differ from the average female population in family practice and to describe characteristics of their healthcare utilisation.
METHOD
Study design, data collection
Electronic medical records of female patients who have suffered abuse were collected as part of a primary study on the effects of training on recognition of intimate partner abuse in female patients in Rotterdam and surrounding areas (Netherlands) in 2003.16 In this study 118 female patients confirmed partner abuse. In June 2004 all family doctors (n = 41) who reported women who had been abused were contacted and asked to dispense as many as possible, printed, anonymous medical records over the period 1 January–1 July 2004. The records were coded with a patient's study number and electronic file number.
Thirty-two doctors cooperated and 92 medical records were obtained. Data on the number of doctor–patient consultations, all prescriptions, complaints, disorders, referrals, demographic information and length of period enrolled in practice were collected.
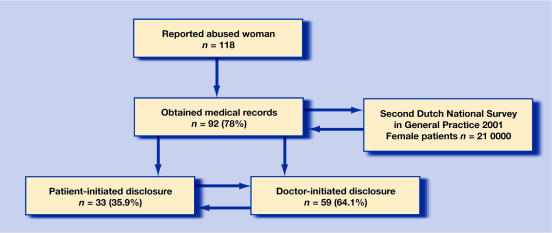
The data were compared to those of female patients, who consulted their family doctor in 2001, in the Second Dutch National Survey in General Practice, 2001 (DNSGP-2).17 This prospective study (n = 415 983) delivered a broad range of data on diseases and healthcare utilisation in the Netherlands and guarantees a nationwide representativeness. The study design is explained in Figure 1.
Figure 1.
Design of study.
Data processing
The most frequently prescribed medication groups were examined: pain medication, tranquillisers, antidepressants, and gastrointestinal medication.3,5,13 Complaints and disorders from electronic medical records were converted into International Classification of Primary Care (ICPC) codes by the research assistant. Referrals for diagnostic tests, to physiotherapists, mental health providers, and social workers were not documented systematically. It was reported whether a woman was referred at least once in the observed period. Interventions for preventive health care (cervical cytology, mammograms) were excluded. Following this procedure, all data were recorded on a registration form and into an SPSS file.
Possible bias of the sample
To assess whether the sample represented a selected population of women who have suffered abuse two disclosure groups were compared:
‘Patient-initiated disclosure’: patient broached the abuse without a doctor's question.
‘Doctor-initiated disclosure’: patient confirmed abuse in answer to a doctor's question.
Information on type of disclosure was previously gathered at the time the doctor reported the patient to the researcher.16
Analysis
The frequency of consultation and prescription rates for pain medication and for the nervous system of this sample were compared to those of the female population of the DNSGP-2, with One-Sample t-test (SPSS version 11.0). The data on presented health problems and referrals were also explored with descriptive statistics.
To investigate whether this sample was biased as a result of the study design, the data of both disclosure groups were compared with the independent samples t-test.
RESULTS
Comparison of the sample to the DNSGP-2 female population
Consultation frequency
In all age categories, a relevant difference in mean consultation frequency, between the women who have suffered abuse and the female patients of the DNSGP-2, occurred. For comparison of the abused women to the DNSGP-2 female patients see Table 1.
Table 1.
Comparison of mean (range) consultation rate per patient/year between: study group and national survey17 (DNSGP-2).a
| Age groups | Study group | DNSGP-2 group | P-value | 95% CI |
|---|---|---|---|---|
| All ages (18–65 years) | 7.47 (6.5 to 8.4) | 4.20 | <0.001e | 2.31 to 4.23 |
| Youngest age groupb | 5.03 (4.2 to 5.8) | 3.35 | 0.001e | 87 to 2.50 |
| Middle aged groupc | 7.79 (5.9 to 9.7) | 3.99 | <0.001 | 2.50 to 5.08 |
| Oldest age groupd | 7.81 (4.8 to 10.9) | 5.25 | 0.012 | 74 to 5.26 |
All female patients: (n = 210 071).
Youngest age group: 18–25 years in study group (n = 14), 15–24 years in DNSGP-2.
Middle aged group: 26–45 years in study group (n = 56), 25–44 years in DNSGP-2.
Oldest age group: 46–65 years in study group (n = 22), 45–64 years in DNSGP-2.
Significant. Compared with one-sample t-test (SPSS).
Prescription rate
During the observed period, 84.8% of the women in this sample received one or more prescriptions for painkillers; 57.6% for tranquillisers; 54.3% for gastrointestinal medication and 39.1% for antidepressants. For comparison of the prescription rates for pain medication and tranquillisers together with antidepressants of the abused women and the DNSGP-2 female patients see Table 2.
Table 2.
Comparison of mean prescriptions per patient/year between women in study group and national survey17 (DNSGP-2).
| Medication type/age groups | Study groupa | DNSGP-2 group | P-value | 95% CI |
|---|---|---|---|---|
| Pain medication | ||||
| Youngest and middle aged groupc | 2.010 | 0.303 | <0.001b | 1.04 to 2.38 |
| Oldest age groupc | 2.041 | 0.601 | 0.021 | 0.24 to 2.64 |
| Tranquillisers/antidepressantsd | ||||
| Youngest and middle aged groupc | 2.111 | 0.743 | 0.058 | −0.05 to 2.78 |
| Oldest age groupc | 3.534 | 1.788 | 0.109 | −0.42 to 3.92 |
Mean number of prescriptions per patient/year: corrected for period enrolled in practice.
Significant.
Youngest and middle aged group from the DNSGP-2: 20–44 years were compared to the study group: 18–45 years (n = 70) and the oldest age group from the DNSGP-2: 45–64 years to our study group: 46–65 years (n = 22).
DNSGP-2: included all nervous system medication. Comparison with one-sample t-test (SPSS).
Pain medication
Similar to the DNSGP-2 study, the prescribed pain medication was predominantly non-steroid anti-inflammatories. The youngest and middle-aged groups of female patients who had been abused received significantly more pain medication. A relevant difference occurred in the oldest age group.
Tranquillisers and antidepressants
In this sample data of tranquillisers and antidepressants were combined to enable comparison to ‘all nervous system’ prescriptions of the DNSGP-2. Although this sample received more prescriptions, the difference was not significant.
Presented health problems and referrals
In this group of women, pain of neck, back, abdominal, stomach and headache (46.5%), was presented much more often than mental health problems such as depression, sleeping problems, anxiety and hyperventilation (18.8%). Relationship problems were found in two-thirds of the medical records.
Four of the 92 women did not receive any referral during the observed period of 3.5 years, while the large majority (85.9%) received more than one type of referral, mostly for diagnostics (83.7%), specialists (59.8%) and physiotherapists (46.7%) and less to mental health providers (39%).
Comparison of the disclosure groups
The sample of 92 female patients who have suffered abuse consisted of 33 women (35.9%) who initially disclosed and 59 women (64.1%) who did so after the doctor had asked. Comparing the disclosure groups for demographics with the independent samples t-test, no significant differences for age-category, residential district or period enrolled in practice were found.
Comparing the disclosure groups for healthcare utilisation with the independent samples t-test, revealed no significant differences.
DISCUSSION
Summary of main findings
Compared to an average female patient in family practice, abused women's patterns display almost double the consultation rate together with a sevenfold prescription rate of pain medication in the youngest and middle age categories and threefold in the oldest age group. This striking picture of increased healthcare utilisation by women who have suffered abuse appearing from this study confirms the findings of a recent New Zealand study with a different design.5
Frequent consultations for pain, seems to be a major characteristic of female patients who have suffered abuse, contrary to the expected mental health problems such as depression, anxiety and sleeping disorders.
Pain requires relief and women who have suffered abuse apparently receive far more prescriptions for painkillers than average female patients do. Not surprisingly, almost one out of two women have been referred to a physiotherapist at least once.
Although two-thirds of the abused women had registered relationship problems and one-third mental complaints, referrals to mental health care or social work were much less than for somatic healthcare referrals. An explanation for this discrepancy is that women who have suffered abuse present predominantly with unexplained somatic complaints and mostly remain unidentified, resulting in medical care instead of referrals to manage the abuse situation.
The ‘symptomatic’ abused woman in family practice appears to be one who consults her doctor twice as often than the average comparable woman for unexplained chronic pain and using a lot of painkillers. Patients more often referred to a physiotherapist, a specialist, and for diagnostic tests should also alert family doctors to the possibility of abuse.
Comparison with existing literature
Earlier studies, with different designs, report chronic undefined pain and an increased use of medical services in women who had been abused.11,13,14 In this respect, this study confirms these findings and supplies them with evidence from the abused female patient's medical record. Women who have suffered abuse are known to present physical or mental symptoms rather than disclose the abuse, and usually remain unidentified.5,14,18 One study that used medical records to review healthcare utilisation of women who have suffered abuse (n = 62), enrolled in a Health Maintenance Organisation, found that the rate of medical visits and estimated costs were 1.6 times higher than for other female patients.15 In spite of the different healthcare system, these outcomes approximate this study's findings.
Strengths and limitations of the study
The strength of this study is that it compares characteristics of a sample of women who have suffered abuse to the average female population as provided by the nationwide representative survey: the DNSGP-2.
The electronic medical records provided the opportunity to seek anonymously for characteristics of presented health problems and prescriptions in a convenient way. The findings correspond to those from other studies with different designs and provide evidence from the medical records of women who had been abused.1,3,5,11,14,19.
However, this study was limited by the retrospective design, which impaired the retrieval of more accurate data on referrals. The healthcare system in the Netherlands, which is both available and accessible to the entire population, may possibly create a utilisation that cannot be generalised to healthcare systems with a different design. Another limitation is that this study was part of an intervention study and risked bias. Nevertheless, comparing disclosure groups did not lead to meaningful differences. Whether bias of improved communication skills of the participants played an important role in inducing more spontaneous disclosures, remains unanswered.
Implications for clinical practice and future research
To date, there are no validated characteristics of an abused female patient.20 This study supports the development of the concept of the ‘symptomatic’ abused female patient. An increased consultation frequency and a high use of pain medication should raise suspicions of intimate partner abuse. Doctors, who recognise this female patient, can no longer avoid asking further questions. This is a vital first step to facilitate disclosure and enables more appropriate and effective care for female patients who have suffered abuse.
Acknowledgments
We wish to thank all 32 participating family doctors for their generous cooperation in providing the anonymous data; Margriet Straver, research assistant, for contacting the participating doctors and for processing the data. Hans Bor, statistician (IVES, Radboud University Medical Centre) for statistical advice; Jan-Marc van Dam (Chelmsford, UK) for English language corrections.
Funding body
This project received a research grant from Theia Foundation, Zilveren Kruis Achmea Health Insurance (200173)
Ethics committee
The study was undertaken with the consent of the ethical committee of the University Medical Centre St Radboud: Commissie Mensgebonden Onderzoek, region Arnhem – Nijmegen (CMO-nr.2002/275)
Competing interests
The authors have stated that there are none
REFERENCES
- 1.Campbell JC. Health consequences of intimate partner violence. Lancet. 2002;359(9314):1331–1336. doi: 10.1016/S0140-6736(02)08336-8. [DOI] [PubMed] [Google Scholar]
- 2.Bergman B, Brismar B, Nordin C. Utilisation of medical care by abused women. BMJ. 1992;305(6844):27–28. doi: 10.1136/bmj.305.6844.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hegarty K, Gunn J, Chondros P, Small R. Association between depression and abuse by partners of women attending general practice: descriptive, cross sectional survey. BMJ. 2004;328(7440):621–624. doi: 10.1136/bmj.328.7440.621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coid J, Petruckevitch A, Feder G, et al. Relation between childhood sexual and physical abuse and risk of revictimisation in women: a cross-sectional survey. Lancet. 2001;358(9280):450–454. doi: 10.1016/s0140-6736(01)05622-7. [DOI] [PubMed] [Google Scholar]
- 5.Fanslow J, Robinson E. Violence against women in New Zealand: prevalence and health consequences. N Z Med J. 2004;117(1206):U1173. [PubMed] [Google Scholar]
- 6.Kramer A, Lorenzon D, Mueller G. Prevalence of intimate partner violence and health implications for women using emergency departments and primary care clinics. Women's Health Issues. 2004;14(1):19–29. doi: 10.1016/j.whi.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 7.McCauley J, Kern DE, Kolodner K, et al. The ‘battering syndrome’: prevalence and clinical characteristics of domestic violence in primary care internal medicine practices. Ann Intern Med. 1995;123(10):737–746. doi: 10.7326/0003-4819-123-10-199511150-00001. [DOI] [PubMed] [Google Scholar]
- 8.Petersen R, Gazmararian J, Andersen Clark K. Partner violence: implications for health and community settings. Womens Health Issues. 2001;11(2):116–125. doi: 10.1016/s1049-3867(00)00093-1. [DOI] [PubMed] [Google Scholar]
- 9.Dickinson LM, deGruy FV, III, Dickinson WP, Candib LM. Health-related quality of life and symptom profiles of female survivors of sexual abuse. Arch Fam Med. 1999;8(1):35–43. doi: 10.1001/archfami.8.1.35. [DOI] [PubMed] [Google Scholar]
- 10.Zachary MJ, Mulvihill MN, Burton WB, Goldfrank LR. Domestic abuse in the emergency department: can a risk profile be defined? Acad Emerg Med. 2001;8(8):796–803. doi: 10.1111/j.1553-2712.2001.tb00209.x. [DOI] [PubMed] [Google Scholar]
- 11.Victoria SG. The health costs of violence. Measuring the burden of disease caused by intimate partner violence. A summary of findings. Carlton South, Victoria, Australia: Victorian Health Promotion Foundation; 2004. [Google Scholar]
- 12.WHO. Violence against women. Health consequences. Geneva: World Health Organisation; 1997. [Google Scholar]
- 13.Campbell J, Jones AS, Dienemann J, et al. Intimate partner violence and physical health consequences. Arch Intern Med. 2002;162(10):1157–1163. doi: 10.1001/archinte.162.10.1157. [DOI] [PubMed] [Google Scholar]
- 14.Hamberg K, Johansson EE, Lindgren G. ‘I was always on guard’ — an exploration of woman abuse in a group of women with musculoskeletal pain. Fam Pract. 1999;16(3):238–244. doi: 10.1093/fampra/16.3.238. [DOI] [PubMed] [Google Scholar]
- 15.Ulrich YC, Cain KC, Sugg NK, et al. Medical care utilization patterns in women with diagnosed domestic violence. Am J Prev Med. 2003;24(1):9–15. doi: 10.1016/s0749-3797(02)00577-9. [DOI] [PubMed] [Google Scholar]
- 16.Lo Fo Wong SH, Wester F, Mol SSL, Lagro-Janssen ALM. Increased awareness of intimate partner abuse after training. A randomised controlled trial. Br J Gen Pract. 2006;56(525):249–257. [PMC free article] [PubMed] [Google Scholar]
- 17.Cardol M, Dijk van L, Jong de JD, et al. Huisartsenzorg: wat doet de poortwachter? 1 edn. Utrecht: NIVEL Netherlands Institute for Research on Health Care; 2004. [General Practitioners' care: what are gate watchers doing?] Second National Survey in General Practice. [Google Scholar]
- 18.Hegarty KL, Taft AJ. Overcoming the barriers to disclosure and inquiry of partner abuse for women attending general practice. Aust N Z J Public Health. 2001;25(5):433–437. [PubMed] [Google Scholar]
- 19.Hathaway JE, Mucci LA, Silverman JG, et al. Health status and health care use of Massachusetts women reporting partner abuse. Am J Prev Med. 2000;19(4):302–307. doi: 10.1016/s0749-3797(00)00236-1. [DOI] [PubMed] [Google Scholar]
- 20.Taket A, Wathen CN, MacMillan H. Should health professionals screen all women for domestic violence? PLoS Medicine. 2004;1(1):e4. doi: 10.1371/journal.pmed.0010004. [DOI] [PMC free article] [PubMed] [Google Scholar]