Abstract
With the government backing the concept of electronic health records (EHR), and with technology being used in every walk of life, more and more hospitals are looking into implementing EHR systems. A national survey of U.S. hospitals was conducted in February/March 2005 to identify the status of EHR systems in hospitals regarding the core functionalities implemented (as identified by the Institute of Medicine), and to determine the perceived benefits, risks, and barriers to adoption of EHR systems in relation to the size of the hospital.
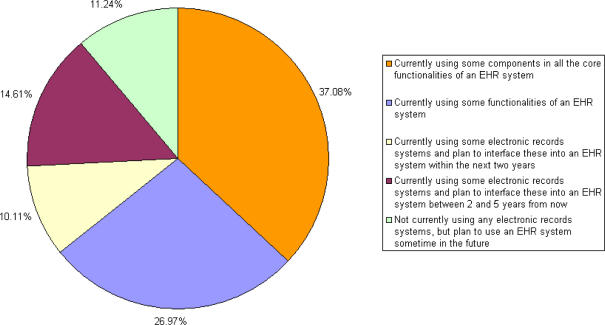
The results showed that 37 percent of the hospitals that participated had some components in all of the core functionalities of an EHR system, while 27 percent were using at least some of the core functionalities. There was a significant relationship in some of the perceived benefits and barriers to adoption of EHR systems based on the size of the hospital. With regard to perceived benefits, a large correlation was found between the “medical staff's work efficiency and time management” and size of the hospital. As to perceived barriers to adoption, the cost of hardware and the size of the hospital were interwoven.
Key Words: EHR systems; risks, benefits, barriers of EHRs; information technology in healthcare
Introduction
With the growing emphasis on providing the right information to the right person anywhere at any time in today's globally interconnected world, the U.S. healthcare industry has been moving toward an electronic health record (EHR) system. It has become obvious that the paper record system is incapable of supplying caregivers with all the patient information they need in a way that they can utilize it. This problem, as well as concerns for better quality and reduced costs, is being realized more and more. Studies report that EHR systems could save billions of dollars; in fact, one such study indicated the systems could save up to $81 billion in healthcare costs annually, as well as improve healthcare quality.1 Financially sound hospitals and physician offices are leaping into adopting EHR systems. However, at the same time, some small hospitals and small physician offices are lagging behind in the use of EHR systems, creating a digital divide.2 This may be due to lack of significant return on investment (ROI) in the short-term, considering the high costs associated with the adoption of EHR systems. In an article published in Mathematica Policy Research, Inc., Lorenzo Moreno noted that, “Although EHRs have the potential to improve quality of care, reduce medical errors, and lower administrative costs, incorporating them into clinical practice will require large investments in technology, in addition to changes in existing systems and processes.”3
Health information technology professionals and governmental leaders are promoting EHRs. David Brailer, former national coordinator for health information technology, emphasized the important role that EHR systems play in improving quality, increasing patient safety, increasing operational efficiency, and reducing costs.4 President Bush announced that most Americans will have EHRs within the next 10 years to allow doctors and hospitals to share patient records nationwide.5
Many organizations are working to develop initiatives and goals to help meet the needs of the healthcare industry. Some of these include (1) the Electronic Health Information Management (e-HIM) initiative by the American Health Information Management Association (2) the charge to the Office of the National Coordinator for Health Information Technology, by the U.S. Department of Health and Human Services (DHHS), to move EHRs into clinical practice and (3) the charge by the DHHS to an Institute of Medicine committee to identify basic functionalities of EHR systems.6–8
The core functionalities of an EHR system and its components as identified by the Institute of Medicine (IOM) committee were health information and data, results management, order entry/management, decision support, electronic communication and connectivity, patient support, administrative processes, and reporting and population health management.9 See the Appendix for a description of each of these IOM core functionalities.
Purpose of the Study
With the advent of new technologies in the healthcare arena, the risks, benefits, and barriers to adoption of EHR systems are constantly changing. The concept of the “digital divide” as described by Goldschmidt in the adoption of EHR systems calls for a closer look at these risks, benefits, and barriers and how they relate to the size of the hospital. 10
The main purposes of this study were (1) to identify the core functionalities (defined by IOM) being used by hospitals throughout the U.S., (2) to identify the perceived level of greatest risks, benefits, and barriers of using EHR systems, and (3) to determine if there was a significant relationship between the risks, benefits, and barriers and the size of the hospital. In order to meet the goals of the study, a national survey was conducted to answer the following research questions:
RQ1. What are the EHR core functionalities (such as health information and data, results management, order entry/management, decision support, electronic communication, patient support, administrative processes, reporting and population health management) utilized by healthcare systems?
RQ2. What are the greatest risks, benefits, and barriers as perceived by directors of health information management (and other information technology and medical professionals)?
RQ3. Is there a significant relationship between the perceived risks/benefits/barriers of using an EHR system and the size of the hospital (as measured by number of beds in the hospital)?
Background and Related Work
The overall status of EHR systems and the effects of using them are topics of growing interest to researchers. A recent study, conducted in 2006 by the Healthcare Financial Management Association (HFMA), surveyed senior healthcare finance executives at hospitals and health systems of various sizes and regions. The purpose was to identify how healthcare financial executives view the barriers to EHR adoption and the actions government can take to encourage adoption. Based on the 176 responses, the functions in which the greatest number of hospitals reported significant progress were order entry (38 percent), results management (27 percent), and electronic health information/data capture (23 percent). The most significant barriers were lack of national information standards and code sets (62 percent), lack of available funding (59 percent), concern about physician (51 percent), and lack of interoperability (50 percent).11
One of the most comprehensive studies on the trends and usage of EHR systems is an annual study that has been conducted in recent years by the Medical Records Institute (MRI). The findings of the 2005 survey were based on 280 provider respondents in the environments of ambulatory, hospitals, IHDSOs, and others. Most of the respondents were information technology (IT) managers and professionals (42 percent), including medical information systems professionals, health information managers, MIS managers, CIOs, network managers, and others with similar titles. The specific applications or functions used by a majority of respondents were in administrative and financial application; the data capture, review, and update capabilities; and e-mail categories. The motivating factors or driving forces for implementing EHR systems that were marked by 75 percent or more of these respondents were the need to (1) improve clinical processes or workflow efficiency, (2) improve quality of care, (3) share patient record information with healthcare practitioners and professionals, and (4) reduce medical errors. The only major barrier to implementation marked by a majority of respondents (57 percent) was lack of adequate funding or resources.12
The American Hospital Association (AHA) conducted a survey of all community hospitals in 2005 to measure the extent of information technology (IT) use among hospitals and better understand the barriers to further adoption. CEOs from 900 community hospitals (19.2 percent) participated in the study. The study found that 92 percent of the respondents were actively considering, testing, or using IT for clinical purposes. The remaining 8 percent that were not considering IT were primarily small, rural, nonteaching, and nonsystem hospitals. The study reported that more than 50 percent of the respondents fully implemented the EHR functions results review—lab, order entry—lab, order entry—radiology, access to patient demographics, and results review—radiology report.13
This study also reported that 50 percent of the rural hospitals specified they were just “getting started" on IT system implementation, whereas 48 percent of the urban hospitals indicated “moderate” or “high" levels of implementation of IT systems. Cost was the number one barrier to the adoption of EHR systems; 59 percent of the hospitals found that initial cost was a significant barrier; 58 percent found acceptance by clinical staff as somewhat of a barrier. Among the smaller hospitals with bed size less than 300, more than 50 percent saw cost as a significant barrier.14
A study was conducted in 2004 by Healthcare Informatics in collaboration with AHIMA to measure the level of readiness of health information management (HIM) professionals and the extent of EHR implementation in their organization. The findings showed the industry is continuing to see more movement toward EHR. For example, when organizations were asked to describe their progress toward an EHR, 17 percent of respondents indicated they were extensively implemented; 26 percent indicated they were partially implemented; 27 percent said they were selecting, planning, or minimally implemented, and 21 percent indicated they were considering implementation and gathering information about it.15
In a study conducted during the summer of 2004 by the American Academy of Family Physicians (AAFP), nearly 40 percent of respondents, who were members of AAFP, indicated they either had completely converted to EHRs or were in the process of doing so. Twenty-four percent had purchased the EHR system within the first half of the year. Findings showed that cost remained a major barrier for physicians in small and medium practices in the move to EHR systems.16
Previous research on risks of EHR systems identified privacy and security as major concerns.17–19 Other risks identified were financial risk (billing errors in software), software systems becoming obsolete, software vendors going out of business, computer crashes, data capture anomalies, programming errors, automated process issues, and populating invalid information in the decision support systems module of EHR systems.20,21
Some of the main benefits of EHR systems that have been identified include reducing medical errors, improving quality of care, conserving physician time, sharing patient information among healthcare practitioners, and workflow efficiency.22,23
The major barrier to adoption of an EHR system, as identified by some studies, was misalignment of cost and benefits or financial reimbursement.24, 25 Brailer (as cited in Mon) said that reimbursing physicians for using EHR systems and reducing their risk of investing in them should accelerate the adoption of EHR systems in physicians' offices.26
Other barriers that have been identified are technical issues, system interoperability, concerns about privacy and confidentiality, lack of health information data standards, lack of a well-trained clinician informatics workforce to lead the process, the number of vendors in the marketplace, and the transience of vendors.27–29
These studies and other previous research conducted in the area of EHR systems determined the risks, benefits, and barriers as well as analyzed the relationship between the adoption of EHR systems and the size of the hospital or physician office.30, 31 Moreno stated, “The evidence from our literature review suggests that large physician groups and hospitals are at the forefront of using EHRs; however, the extent to which small physician practices—those made up of eight or fewer physicians representing nearly 80 percent of all physicians in the US—have adopted EHRs nationally remains unclear.”32
The perceived level of greatest risks, benefits, and barriers to adoption of EHR systems are addressed in this study, as well as the relationship of these factors to the size of the hospital.
Methodology
In order to gain a better understanding of electronic record systems used in healthcare systems and terminology related to electronic health systems, the researchers conducted interviews at three hospitals within a 65-mile radius of their midwestern university. The researchers interviewed seven healthcare and information systems professionals from the three hospitals. After these interviews, and a thorough review of the literature, the research team decided that the target population should be directors of health information management since they are the core individuals using the electronic health record systems. The researchers then developed a draft of a survey instrument to gather answers to the research questions stated above. A panel of experts, which included an additional group of medical personnel and information systems personnel in local hospitals, reviewed the survey instrument. The researchers revised the survey instrument, and the Human Subjects Committee at the university approved it prior to pilot testing. Next, the survey was addressed to the director of HIM of eight randomly selected hospitals from a national list of hospitals for pilot testing, and revised again based on their feedback.
The research team obtained a database of randomly selected 1,000 member hospitals of the American Hospital Association from Third Wave Research. A mailing including a cover letter, survey instrument, a diagram with definitions of the core functionalities as identified by the IOM, and a self-addressed return envelope was mailed in February 2005 to the director of health information management of these 1,000 randomly selected hospitals. A follow-up mailing was sent in March. The response rate was slightly less than 10 percent and the findings described on the following pages are based on the 90 usable surveys that were returned. The low response rate was a limitation to the study, and it could have been due to reasons such as (1) the long length of the survey instrument, or (2) the reluctance of some individuals to respond if they felt their hospital was slow in adopting an EHR system. This low response rate limits the ability to generalize the findings to the total population. Responses to this study were coded onto Scantron sheets and analyzed using Statistical Product and Service Solutions (SPSS), version 14.
Results
Demographics of Respondents and Hospitals Surveyed
In general, the respondents had several years of experience as indicated by a mean of 20 years; 58 percent of the respondents had 20 years or more of experience in the field, while only 16 percent had less than 10 years. The majority of the respondents (61 percent) indicated their job title was health information manager or director of health information, and the next largest group was directors of medical records (15 percent). Some of the other titles included chief information officer, vice president of information services, HIM director and privacy officer, patient health education coordinator, and chief financial officer. The hospitals varied greatly in size. The average number of beds in each facility was 209 (Table 1). The smallest hospital had 12 beds and the largest had 1,460 beds (Table 1). Table 1 shows the number of beds per facility as organized according to the groupings used by the AHA. The average number of beds in the entire healthcare system, not just in each facility, was 546, with the smallest healthcare systems containing 20 beds and the largest containing 6,000 beds.
Table 1.
Number of Beds in Facility
| Beds | Number | Percent | Percent from AHA Statistics* |
| Less than 100 | 30 | 34.88 | 47.46 |
| 100–199 | 24 | 27.91 | 23.86 |
| 200–299 | 12 | 13.95 | 12.75 |
| 300–399 | 7 | 8.14 | 7.13 |
| 400–499 | 7 | 8.14 | 3.51 |
| 500 or more | 6 | 6.98 | 5.29 |
| Total | 86 | 100.00 | 100.00 |
Based on AHA 2003 statistics of 4,895 U.S. community hospitals.
The average number of hospitals in each healthcare system was 14 with a range from 1 to 172; 48 percent of the systems had only one hospital, while 43 percent had 2 to 28 hospitals. The remaining 9 percent had more than 50 hospitals in their entire healthcare system.
Status of Core Functionalities
Research Question #1
During the literature review and the interviews with healthcare and IT professionals, it was clear that there are many different terms often used interchangeably with EHR system, including automated medical record (AMR) system, computer-based patient record system (CPRS), and electronic medical record (EMR) system. Also, the systems can be purchased with some or all of the core functionalities depending on the funds available. To determine hospitals' use of EHR systems, the respondents were asked two questions. First, they were asked to mark the EHR system status of their facility from a list of options as shown in Figure 1. The largest number of the respondents (37 percent) indicated that they currently used some components in all of the eight core functionalities and 27 percent used only some of the eight core functionalities of an EHR system (Figure 1).
Figure 1.
Status of Facility in Regard to Use of EHR System
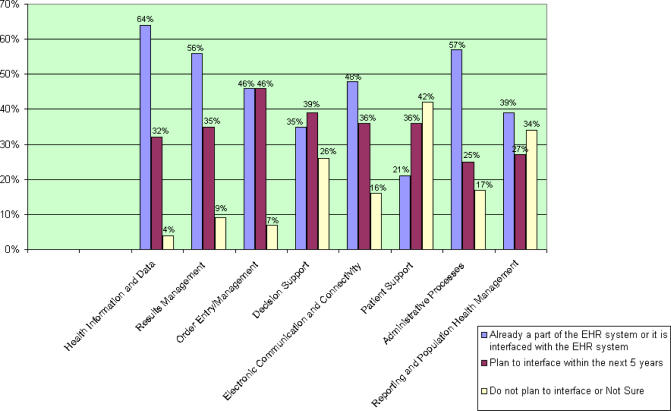
Second, they were asked to mark the core functionalities of the EHR system that their facility had or planned to have within the next five years (Research Question #1). Health information and data, results management, and administrative processes were the only core functionalities that were currently part of or interfaced with the EHR system in more than 50 percent of the respondents' facilities (Figure 2).
Figure 2.
Status of Core Functionalities within Facility
Perceived Risks, Benefits, and Barriers of EHR Systems
Research Question #2
A separate list of risks, benefits, and barriers were provided to the respondents and they were asked to rank them based on importance, with the highest number assigned to the item of greatest degree of risk, benefit, or barrier. The two greatest risks (Table 2) of the adoption of an EHR system as identified by the respondents were (1) privacy of data—access control (4.63 out of 7) and (2) inaccurate patient information due to periodic and not real-time updates (4.34 out of 7). Table 2 shows the list of seven risks provided and the mean rankings assigned to them.
Table 2.
Risks of Using an EHR System
| Risk | Mean Rank |
| Privacy of data (access control) | 4.63 |
| Inaccurate patient information due to periodic and not real-time updates | 4.34 |
| EHR system being unavailable due to technical problems (i.e., downtime) | 4.31 |
| Security of data | 4.29 |
| Legal issues | 3.82 |
| Staff not seeking other information due to over reliance on EHR system | 3.78 |
| Patients finding out things about their condition that may frighten them | 2.88 |
The two greatest benefits (Table 3) to the adoption of an EHR system were (1) interoperability (exchanging patient information electronically) with other departments within the facility (7.33 out of 10) and (2) quality of care (6.84 out of 10). When looking at barriers (Table 4) to the adoption of an EHR system, the greatest ones identified by the respondents were (1) software cost (7.31 out of 10), (2) hardware cost (6.92 out of 10), and (3) participation from physicians (5.95). Tables 3 and 4 provide the list of 10 benefits and 10 barriers, respectively, along with the mean rankings.
Table 3.
Benefits of Using an EHR System
| Benefit | Rank |
| Interoperability (exchanging patient information electronically) with other departments within the facility | 7.33 |
| Quality of care | 6.84 |
| Clinical workflow | 6.25 |
| Medical staff's work efficiency and time management | 5.76 |
| Patient safety | 5.66 |
| Interoperability outside the facility, but still within the entire healthcare system | 5.35 |
| Patient privacy and confidentiality | 4.87 |
| Business processes (strategic and operations) | 4.72 |
| Patient-doctor relationship | 4.38 |
| Cost of care | 3.95 |
Table 4.
Barriers to Adoption of the EHR System
| Barrier | Mean Rank |
| Software cost | 7.31 |
| Hardware cost | 6.92 |
| Participation from physicians | 5.95 |
| Interoperability among different electronic systems and the true EHR system | 5.61 |
| Inability to find the software that meets the requirements of the true EHR system | 5.17 |
| Organizational culture | 5.10 |
| Participation from nursing staff | 5.03 |
| Standards | 4.81 |
| Return on investment (ROI) | 4.73 |
| Personnel cost | 4.54 |
Research Question #3
In order to determine if there was a significant relationship in the perceived rankings of risks based on the size of the hospital, as measured by number of beds, both the Pearson correlation and the Spearman rho correlation were performed. No significant relationships were found in any of the rankings of risks in either of the tests of correlation. This implies that the size of the hospital was not significantly associated with the risk of using EHR systems as perceived by the respondents.
When testing to see if there was a correlation between the ranking of benefits and the size of the hospital, the Pearson correlation again found no significant relationships. However, the Spearman rho correlation found that there was one benefit in which the ranking varied significantly based on the size of the hospital (Table 5). The benefit of “medical staff's work efficiency and time management” was significant at the alpha level 0.05. The correlation coefficient as seen in Table 5 was −0.236 with a p value of 0.042. The negative correlation indicates that as the size of the hospital went up, the ranking for this benefit went down, indicating it was not perceived to be as much of a benefit for larger hospitals. No other benefits showed a significant relationship between rank and hospital size. Table 5 shows the correlation coefficients and probabilities for each of the benefits.
Table 5.
Spearman Rho Correlation between Benefits and Size of Hospitals
| Benefit | Spearman Rho | p |
| Interoperability with other departments within the facility | 0.021 | 0.860 |
| Quality of care | −0.240 | 0.838 |
| Clinical workflow | −0.134 | 0.252 |
| Medical staff's work efficiency and time management | −0.236* | 0.042* |
| Patient safety | 0.176 | 0.132 |
| Interoperability outside the facility, but still within the entire healthcare system | 0.086 | 0.462 |
| Patient privacy and confidentiality | −0.024 | 0.836 |
| Business processes (strategic and operations) | 0.029 | 0.807 |
| Patient-doctor relationship | 0.097 | 0.406 |
| Cost of care | 0.017 | 0.883 |
p < 0.05.
When testing for a correlation between rankings of barriers and size of hospital, the Pearson correlation and Spearman rho found a significant relationship between one barrier to adoption of an EHR system and the size of hospital. Both identified the significant relationship between hardware costs and the size. The Pearson coefficient was −0.245 with a p value of 0.036; the Spearman rho coefficient was −0.426 with a p value of 0.035 (Table 6). Since the correlation was negative, it means that as the size of the hospital increased, the perception of hardware costs (as a barrier) decreased. One more significant correlation was found with the Spearman rho test; this was “participation from physicians,” which had a coefficient of 0.255 and a p value of 0.028 as seen in Table 6. Since the correlation between the barrier of physician participation and size of hospital was positive, it implies that as the size of the hospital increased so did the perception of the participation from physicians as a barrier.
Table 6.
Spearman Rho Correlation between Barriers and Size of Hospital
| Barrier | Spearman Rho | p |
| Software cost | −0.101 | 0.391 |
| Hardware cost | −0.426* | 0.035* |
| Participation from physicians | 0.255* | 0.028* |
| Inability to find the software that meets the requirements of the true EHR system | 0.174 | 0.141 |
| Interoperability among different electronic systems and the true EHR system | −0.039 | 0.744 |
| Organizational culture | −0.072 | 0.547 |
| Participation from nursing staff | 0.156 | 0.185 |
| Standards | −0.074 | 0.529 |
| Return on investment (ROI) | 0.041 | 0.730 |
| Personnel cost | −0.110 | 0.352 |
p < 0.05.
Summary and Discussion
The push to use EHR systems in the healthcare industry is coming from all sides, including the government. It is important to understand the direction hospitals are moving toward the adoption of EHR systems. About a third of the respondents (37 percent) of this study indicated they currently used some components in all of the eight core functionalities identified by the IOM and 27 percent used only some (Figure 1). In a majority of respondents' hospitals, health information and data, results management, and administrative processes were the three core functionalities currently part of or interfaced with the EHR system (Figure 2).
Many studies have been conducted in the area to gauge the use of EHR systems and the risks, benefits, and barriers these systems have to offer. However, as more and more hospitals plan to implement EHR systems, and various EHR system software programs become available, the risks, benefits, and barriers to implementation are changing and becoming more transparent. Also, the findings of the studies vary based on the roles of the respondents. The greatest risk of the adoption of an EHR system as identified by the respondents was privacy of data (Table 2). Interoperability (exchanging patient information electronically) with other departments within the facility was identified as the greatest benefit (Table 3). According to the respondents, software cost was the greatest barrier (Table 4). The study by AHA found that cost is the number one barrier in the adoption and use of EHR systems. The HFMA study reported that funding was a greater concern (64 percent) for hospitals indicating a low level of adoption, but of less concern (44 percent) for those further along in adoption. Financial return was a greater concern (38 percent) for hospitals indicating a low level of adoption, but of less concern (19 percent) for those further along in adoption. Midsize hospital financial leaders were more concerned about funding as a barrier to adoption than were either large or small hospital leaders. The HFMA study also found that funding was a less significant concern for nonrural hospitals than for rural hospitals.
When comparing the many studies on EHR systems, it is clear that the roles of the respondents varied as well as the sample size. The roles of those surveyed included financial executives, CEOs, providers, HIM professionals, and members of healthcare organizations (Table 7). The study presented here surveyed the HIM professionals and identified software and hardware cost and physician acceptance as the major barriers to EHR system adoption. The AHIMA study that also surveyed the HIM professionals reported lack of funding and physician acceptance as the top two barriers.
Table 7.
Comparison of Major Studies Identifying Top EHR Barriers
| Organization | Role of Respondents | Number of Respondents | Barriers |
| HFMA, 2006 | Senior healthcare finance executives at hospitals and health systems of all sizes | 176 |
|
| AHA, 2005 | CEOs of community hospitals | 900 |
|
| MRI, 2005 | Provider responses (28% in hospital environment; 42% were IT managers and professionals) | 280 |
|
| AHIMA, 2004 | Members of AHIMA working in all settings including clinical settings (80 percent), hospitals (55 percent) and ambulatory care, long-term care, behavioral health, and other settings. The majority (83 percent) identified themselves as HIM professionals: “director” and “manager” | 284 |
|
Each study conducted by a specific agency found that lack of funding or cost was either the main barrier or at least in the top two barriers (Table 7). In fact, all studies except the one conducted by the Healthcare Financial Management Association, which surveyed the finance executives at hospitals, found that cost was the number one barrier. This group indicated national information standards and code sets as the main barrier (slightly above lack of funding). See Table 7 for a listing of each of the studies, the role and number of respondents, and major barriers to EHR systems.
This study found there was a significant relationship in some of the perceived benefits and barriers to adoption of these systems based on the size of the hospital. With regard to perceived benefits (Table 5), a significant relationship was found between the benefit “medical staff's work efficiency and time management” and size of the hospital. This seems to imply that the automation of work flow offered through an EHR system does not provide as much benefit when the size of the hospital increases.
In the perceived barriers to adoption category (Table 6), there was a significant relationship between the cost of hardware and the size of the hospital. This may be due to the fact that the smaller hospitals have to build the infrastructure to implement an EHR system from the ground up whereas some larger hospitals have more electronic systems already in place and may not need as much hardware. The study by AHA found that the cost to adopt and use EHR systems is seen as a major barrier in smaller hospitals versus the larger ones, and it reported that large hospitals use more IT than smaller ones. Another barrier with a significant relationship was participation from physicians (Table 6). The correlation indicated that as the hospital size increased so did the perception of the “participation from physicians” as a barrier. This could be due to the greater number of physicians needing to participate in the larger hospitals. The AHA study reported that physicians use EHR systems less frequently when compared to nurses and other medical staff.
Conclusions and Recommendations
To make the adoption of EHR systems successful in hospitals, it is important to look at the benefits, risks, and barriers based on the size of the hospital. The survey results indicated a significant relationship in some benefits and barriers to adoption of EHR systems based on the size of the hospital. However, due to the low response rate, these findings may not be generalizable to other hospitals throughout the country. If built for various hospital sizes, EHR systems could reduce barriers such as hardware costs for small hospitals, and could increase benefits such as work efficiency and time management by implementing process improvement for large hospitals. Specialized software systems such as EHR systems need not come in “one size fits all.” Various other industry software programs, such as customer relationship management, content management, and web portal applications, are available in different editions to fit the needs of the large enterprise and also the small and medium-size businesses. Following this kind of approach might also be beneficial in the healthcare industry.
In the future, an in-depth study should be conducted to understand the specific process workflow, benefits, and barriers to adoption of EHR systems based on the size of the hospital. This would help focus on the requirements of hospitals by size, which would in turn assist the advocates of EHR systems to focus on gains and issues in adopting these systems and also propose ways to overcome such issues. Also, addressing the financial incentives and costs involved in adopting EHR systems by hospitals and physician offices could take the healthcare industry a step toward eliminating this major barrier.
Appendix
Health Information and Data—A defined data set that includes medical and nursing diagnoses, a medication list, allergies, demographics, clinical narratives, and laboratory test results for access by care providers when needed.
Results Management—A feature that manages lab test results and radiology procedures results, does results reporting and results notification, and handles multimedia support-images, waveforms, pictures, sounds.
Order Entry/Management—Computerized provider order entry (CPOE) for such areas as electronic prescribing, laboratory, microbiology, pathology, XR, ancillary, nursing, supplies, consults. Even with little or no decision support they can still improve workflow processes by eliminating lost orders and ambiguities caused by illegible handwriting, generating related orders automatically.
Decision Support—A computerized decision support system that enhances clinical performance by providing drug alerts, other rule-based alerts, reminders, clinical guidelines and pathways. It also helps in improving drug dosing and drug selection. It can be used for chronic disease management, clinician work lists, diagnostic decision support, and automated real-time surveillance.
Electronic Communication and Connectivity—Electronic communication can be between provider-provider, patient-provider, trading partners such as pharmacies, insurers, laboratory, radiology, and among team members for coordination. Electronic connectivity includes integrated medical record within facility, within different facilities of the same healthcare system, and among different healthcare systems.
Patient Support—Patient support includes patient education, family and informal caregiver education, data entered by patient, family, and/or information caregiver such as home monitoring.
Administrative Processes—Administrative processes include electronic scheduling systems for hospital admissions, inpatient and outpatient procedures, and identifying eligible or potential eligible patients for clinical trials.
Reporting and Population Health Management—This feature would report patient safety and quality data, public health data, and disease registries. It makes the reporting process less labor-intensive and time-consuming (Institute of Medicine, 2003).
Source: Institute of Medicine. “Key Capabilities of an Electronic Health Record System,” 2003. Available at http://books.nap.edu/html/ehr/NI000427.pdf (accessed June 26, 2004).
Contributor Information
Minal Thakkar, Minal Thakkar is an assistant professor of information systems at Southern Illinois University Carbondale, IL.
Diane C Davis, Diane C. Davis, PhD, is a professor information systems at Southern Illinois University Carbondale, IL..
Notes
- 1.Hillestad Richard, Bigelow James, Bower Anthony, Girosi Federico, Meili Robin, Scoville Richard, Taylor Roger. Can Electronic Medical Record Systems Transform Health Care? Potential Health Benefits, Savings, and Costs. Health Affairs. 2005;24(5):1103–1117. doi: 10.1377/hlthaff.24.5.1103. [DOI] [PubMed] [Google Scholar]
- 2.Goldschmidt Peter G. HIT and MIS: Implications of Health Information Technology and Medical Information Systems. Communications of the ACM. 2005;48(10):69–74. [Google Scholar]
- 3.Moreno, Lorenzo. “Electronic Health Records: Synthesizing Recent Evidence and Current Policy.” Mathematica Policy Research, Inc. (2005): 1-4. Available at http://www.mathematicampr.com/publications/pdfs/electronichealth.pdf (accessed February 22, 2006).
- 4.Mon Donald T. Next Steps for the EHR Draft Standard: Core Functionality and Conformance Criteria Key for Accreditation. Journal of American Health Information Management Association. 2004;75(10):50–51. [PubMed] [Google Scholar]
- 5.Cassidy, Bonnie S. “Skills for Success in Managing an EHR Environment.” Advance Online Editions for Health Information Professionals, May 2004. Available at http://www.advanceforhim.com/common/Editorial/PrintFriendly.aspx?CC=34975 (accessed June 18, 2004).
- 6.AHIMA Task Force. A Vision of the e-HIM Future. Chicago: AHIMA; 2003. [Google Scholar]
- 7.Moreno, Lorenzo. “Electronic Health Records: Synthesizing Recent Evidence and Current Policy.”
- 8.Institute of Medicine. Key Capabilities of an Electronic Health Record System, 2003. [PubMed] [Google Scholar]
- 9.Institute of Medicine. “Key Capabilities of an Electronic Health Record System.”
- 10.Goldschmidt, Peter G. “HIT and MIS: Implications of Health Information Technology and Medical Information Systems.”
- 11.Healthcare Financial Management Association. “Overcoming Barriers to Electronic Health Record Adoption.” Results of survey and roundtable discussions conducted by the Healthcare Financial Management Association, February 2006. Available at http://www.hfma.org/NR/rdonlyres/4FE68E23-0A47-4674-ABBA-F1A4AA1E73A9/0/ehr.pdf (Accessed May 3, 2006).
- 12.Medical Records Institute. Medical Records Institute's Seventh Annual Survey of Electronic Health Record Trends and Usage for 2005. 2005. [Google Scholar]
- 13.American Hospital Association. “Forward Momentum Hospital Use of Information Technology,” AHA, 2005. Available at http://www.ahapolicyforum.org/ahapolicyforum/resources/content/FINALNonEmbITSurvey105.pdf p. 3 (accessed March 4, 2006).
- 14.American Hospital Association. “Forward Momentum Hospital Use of Information Technology.”
- 15.Zender Anne. Ready for the EHR? A New Survey Measures EHR Implementation and Individual Readiness. Journal of AHIMA. 2005;76(3):54–55. [PubMed] [Google Scholar]
- 16.Carol Ruth. EHRs, the Doctor Will See You Now. Journal of AHIMA. 2005;76(4):24–28. [PubMed] [Google Scholar]
- 17.Hersh William. Health Care Information Technology: Progress and Barriers. Journal of the American Medical Association. 2004;292(18):2273–2274. doi: 10.1001/jama.292.18.2273. [DOI] [PubMed] [Google Scholar]
- 18.Swartz Nikki. Electronic Medical Records' Risks Feared. Information Management Journal. 2005;39(3):9. [Google Scholar]
- 19.Bates David. Physicians and Ambulatory Electronic Health Records. Health Affairs. 2005;24(5):1180–1189. doi: 10.1377/hlthaff.24.5.1180. [DOI] [PubMed] [Google Scholar]
- 20.Miller Robert H, West Christopher, Brown Tiffany Martin, Sim Ida, Ganchoff Chris. The Value of Electronic Health Records in Solo or Small Group Practices. Health Affairs. 2005;24(5):1127–1137. doi: 10.1377/hlthaff.24.5.1127. [DOI] [PubMed] [Google Scholar]
- 21.Goldschmidt, Peter G. “HIT and MIS: Implications of Health Information Technology and Medical Information Systems.”
- 22.Berman Jeff. Safety Centers and EMRs. Health-IT World; 2004. [Google Scholar]
- 23.Hier Daniel, Rothschild Adam, LeMaistre Anne, Keeler Joy. Differing Faculty and House Staff Acceptance of an Electronic Health Record. International Journal of Medical Informatics. 2005;74(7/8):657–662. doi: 10.1016/j.ijmedinf.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 24.Hersh, William. “Health Care Information Technology: Progress and Barriers.” [DOI] [PubMed]
- 25.Bates, David. “Physicians and Ambulatory Electronic Health Records.” [DOI] [PubMed]
- 26.Mon, Donald T. “Next Steps for the EHR Draft Standard: Core Functionality and Conformance Criteria Key for Accreditation.”
- 27.Brailer David J, Terasawa Emi L. Use and Adoption of Computer-Based Patient Records. California HealthCare Foundation; 2003. pp. 1–42. [Google Scholar]
- 28.Hersh, William. “Health Care Information Technology: Progress and Barriers.” [DOI] [PubMed]
- 29.Bates, David. “Physicians and Ambulatory Electronic Health Records.” [DOI] [PubMed]
- 30.Moreno, Lorenzo. “Electronic Health Records: Synthesizing Recent Evidence and Current Policy.”
- 31.American Hospital Association. “Forward Momentum Hospital Use of Information Technology.”
- 32.Moreno, Lorenzo. “Electronic Health Records: Synthesizing Recent Evidence and Current Policy.”