Abstract
Objective
The growing importance of electronic medical records (EMRs) to healthcare systems is evident, yet the debate concerning their impact on patient-provider communication during encounters remains unresolved. For this study, we hypothesize that providers' use of the EMR will improve patientprovider communication concerning self-care during the medical encounter.
Design
Cross-sectional, observational study.
Setting
A primary-care outpatient clinic of the South Texas Veterans Health Care System in San Antonio, TX, USA.
Methods
A convenience sample of 50 patient/physician encounters was videotaped, transcribed verbatim, and analyzed to determine the time that the physician spent using the EMR and self-care topics discussed. Self-care topics included medication use, recognition of disease symptoms, diet, exercise, management of physical and emotional distress, self-monitoring activities, cigarette smoking, alcohol consumption, and family support/community resources. Two observers independently coded for the kind of self-care topics (kappa = 0.91) using the Atlas.ti software package.
Results
Encounters averaged 22.6 minutes (range: 5–47, SD = 8.9). We identified two encounter types based on EMR usage: low use (n = 13), with EMR use of two minutes or less, and moderate to high EMR use (n = 37), with EMR use of five minutes or more. Average time for encounters was 25 minutes for moderate to high EMR use encounters and 16 minutes for low EMR use encounters (t test, p < 0.001). Issues pertaining to facets of self-care management were discussed in every physician-patient interaction (100 percent). The most frequently discussed self-care topics were medication use (100 percent), physical distress (76 percent), and disease symptoms (76 percent). Self-monitoring activities, exercise, and diet were discussed in 62 percent, 60 percent, and 46 percent of the 50 encounters respectively. Emotional distress (26 percent), smoking (30 percent), family support/community resources (26 percent), and alcohol consumption (20 percent) were the least discussed issues.
Encounters were similar with respect to the kinds of self-care elements discussed. However, EMR use encounters were more likely to include a higher number of self-care topics raised by physicians than low EMR use encounters, particularly on disease symptoms (odds ratio = 4.4, p = 0.05), and physical distress (odds ratio = 7.4, p = 0.006). A significant correlation was observed between the number of self-care elements discussed and time spent on the EMR (r = 0.6, p < 0.05), but no correlation was observed between the length of the encounter and self-care discussion (r = 0.009, p = 0.90).
Conclusions
The use of an EMR during encounters is associated with an increase in the number of self-care topics raised by physicians. EMRs offer the opportunity to involve patients and physicians in discussion of self-care during patients' visits. Given the current emphasis on the widespread implementation of EMRs, future EMRs should be designed to systematically facilitate the integration of EMRs into clinical exchanges about self-care.
Key Words: electronic medical records, self-care, clinical communication
Introduction
Many studies have documented the impact of physician-patient communication on self-care behaviors.1–3 Self-management programs aim to give patients the knowledge and skills to manage their illnesses daily in their own living environments.4–6 Self-care management encompasses a variety of actions and skills important for both treatment of an illness and prevention of its complications.7 Examples of self-care themes include recognition of disease symptoms, medication use, management of physical and emotional distress, self-monitoring activities, exercise, diet, smoking cessation, alcohol consumption, and family support/community resources.8
A systematic review of randomized clinical trials and descriptive observational studies of physicianpatient communication confirmed a positive influence of verbal communication on health outcomes.9 Physician-patient communication about self-care management can empower and prepare patients to manage their health and healthcare by emphasizing patients' central role in taking responsibility for their own health.10 The collaborative interpretation model, for example, is based on training patients and providers to generate building blocks for a more complete and coherent exchange about treatment plans.11,12 This model is also consistent with the activated patient described in the health education literature and the theory of reciprocal exchange in the medical visit described by Hall and Roter in 1984.13
In spite of this overwhelming evidence regarding the importance of patient-provider communication on patients' adherence to self-care regimens, in usual practice physician-patient communication concerning disease management remains inadequate.14,15 We and others have found that providers' use of an electronic or computerized medical record (EMR) during encounters improves patient-provider verbal communication and helps move the system toward patient-centered care (PCC).16,17
Study theoretical approach:
The Chronic Care Model (CCM) identifies clinical information systems (e.g., electronic medical records) and self-management support as essential elements to foster productive communication between patients and providers and better chronic illness care outcomes.18 Studies have shown that each element, as well as the combination of these two elements, fosters productive interactions between informed patients who take an active part in their care and providers with resources and expertise.19,20 The EMR is one essential component of the clinical information system that promises significant advances in patient care.21 Effective self-management support means more than telling patients what to do. It means acknowledging the patients' central role in their care, a role that fosters a sense of responsibility for their own health.22–26 Using the Chronic Care Model as a theoretical approach, we examined the role of EMR usage in patient-provider communication about self-care during patients' visits.
Investigating the role of EMR use in self-care communication is critical to enlighten us about future EMR design to improve self-care communication during patients' visits and to advance our knowledge regarding the interface between information technology, self-care management, and the human dimension of medical encounters.
Method
We performed a cross-sectional, observational study to examine the content of 50 adult primary-care clinic encounters carried out by six staff physicians at the Audie L. Murphy Memorial Veterans Hospital (VHA) in San Antonio, TX. The encounters took place during 2002 and were videotaped to allow for the assessment of the actual form and content of the patient-provider communication about self-care and to study the role of EMR usage in facilitating these communications.
Subjects:
We recruited staff primary care physicians (internists). All physicians were expected to record their progress notes on an EMR. The EMR was available in each exam room as well as in the doctor's conference room. Patients were recruited as part of a convenience sample of all patients attending the clinic on days staff members were videotaping encounters. Patients' demographic characteristics were obtained from their medical records. Physicians' demographic characteristics were collected using a short survey e-mailed to them after the encounter. All participants (patients and physicians) read and signed a consent form approved by the Institutional Review Board at the University of Texas Health Science Center at San Antonio.
EMR usage:
The EMR was used in each of the encounters in this study. The computer, a desktop unit with an attached monitor, keyboard, and mouse, was located in the middle of the physician's desk. The EMR was used to review and update a patient's medical record as well as to place orders for consultations, medications, and laboratory investigations.
We defined EMR usage as any contact with the computer, regardless of whether or not the physician was talking to the patient. The proportion of time spent on using the EMR equals the time spent using the EMR in each encounter divided by the total time of each encounter. This was measured by using a stopwatch to document the total time the physician made eye contact with the computer screen and/or physically utilized any part of the device, such as the keyboard, during the videotaped encounter.
Upon reviewing the videotapes and analyzing the EMR usage time, we noticed that usage of the EMR varied considerably between physicians and between encounters with the same physician and found a natural cut point defining two groups of encounters. In 13 encounters, physicians used the EMR for two minutes or less. During these encounters, the physicians also tended to utilize paper charts as a supplement to obtaining information about the patients' medications, x-ray reports, laboratory results, and so forth. In the remaining 37 encounters, physicians used the EMR for at least five minutes and for an average of 11.35 minutes. This was just under 50 percent of the average encounter time for these patients. On the basis of these observations, we created two groups: moderate to high EMR use encounters (5–27 minutes) and low EMR use encounters (two minutes or less).
Videotaped encounters:
All videotaped encounters were transcribed in order to examine patientprovider self-care communication during patients' visits. A qualified, trained research assistant performed all transcriptions. These were generated verbatim by watching and listening to the videotapes. The research assistant replayed each tape when necessary until she reached satisfaction according to the study protocol. In some cases when the research assistant could not understand certain sentences, she would consult the team. All transcribed videotapes were checked for accuracy by a second trained research assistant.
Patient-provider self-care communication:
All transcribed videotapes were content analyzed regarding patient-provider self-care communication. Content of self-care was defined as themes that consistently emerged during the encounter about self-care topics. Examples of self-care topics include discussion about medication, physical distress, disease symptoms, self-monitoring activities, exercise, diet, cigarette smoking, family support/community resources, emotional distress, and alcohol consumption (Table 1). Identification and classification of utterances about self-care by either provider or patient were coded from transcripts. To enhance the efficiency of the coding method, we used the qualitative software program Atlas.ti to code for all exchanges related to self-care as they occurred in the encounter. We noticed that exchanges regarding self-care topics were distributed throughout the visit, often with several interruptions in between. Therefore, coders used transcribed, not videotaped, encounters to code for self-care topics.
Table 1.
Definition of Self-Care Elements
| Element of Self-Care | Definition |
| Disease symptoms | Physical or psychological changes/indicators as a result of having chronic illness(es); examples include discussion of hypoglycemic symptoms, such as dizziness |
| Self-monitoring activities | Actions that patients should do on a regular basis in order to manage their diseases; examples include checking blood pressure or blood glucose level |
| Physical distress | Patients' experience of pain that interferes with their ability to manage their diseases; examples include fatigue and pain |
| Diet | Quality and quantity of patients' intake; examples include the kind and amount of high-carbohydrate food or drink such as soda consumed |
| Exercise | Regular physical activity, including leisure and recreational activities; examples include walking or swimming |
| Cigarette smoking | Tobacco use |
| Alcohol consumption | Alcohol intake |
| Medication use | Knowledge of medication name, description, and dosage information, and occurrence of side effects |
| Emotional distress | Patients' feelings as a result of their illnesses that interfere with their ability to manage the illness; examples include anxiety or depression |
| Family support/community resources | Family members, social clubs, religious organizations, and neighbors that provide physical and emotional assistance to the patients |
A detailed code book was developed to define and specify categories based on self-care literature and methods for coding each self-care element in the transcribed encounters. Intra-rater reliability and percent agreement in coding categories were assessed by having two researchers code a sample of five encounters and then code them again two weeks later. The overall kappa for the intra-rater reliability was 0.90.
To establish inter-rater reliability, two observers coded the same 10 transcribed encounters, and then their coding agreement patterns were compared using kappa measures. An initial comparison between the self-care categories revealed moderate agreement between the two observers (kappa = 0.65). In order to improve the kappa measures, we examined the source of discrepancies between coders. For example, initially one observer coded patient-provider discussion about medication use under the category of selfmonitoring activities. The second observer coded exchanges about of self-monitoring activities as medication use. In order to improve the level of agreement among coders, we developed a detailed protocol to specify the coding procedures and to accurately define the different self-care categories expected to be observed during the medical encounters. Therefore, the definitions of self-care categories were further revised; self-monitoring activities was defined as actions that patients should do on a regular basis to obtain quantitative measures of their disease or clinical status such as blood pressure, weight, or glucose monitoring. The medication use category was defined as patient-provider exchange about patients' medications such as those regarding the medications' kind (name of medication), dosage (amount/quantity), and interval (time between dosages). This comparison was the beginning for organizing more detailed definitions of the different self-care categories. After several meetings, we agreed on 10 operational definitions of the elements of self-care (Table 1). The findings presented in this paper showed a kappa of 0.91 for the 10 self-care topics. The kappa results indicate very good agreement, as indicated by Elwood.27
Data analysis:
Content analysis focused on identifying all self-care topics that consistently emerged during the encounters. A distinct exchange about a specific self-care element was identified as the basic unit of analysis. A distinct exchange begins with initiation of a self-care topic (e.g., diet) by either the patient or the practitioner and continues until a shift in topic occurs. The analysis was based on conversation analysis and ethnomethodology. This method analyzes interactions as they naturally occur and identifies emergent components of conversation.28,29 For each self-care theme (e.g., recognition of disease symptoms, smoking cessation), an initial matrix was constructed. The rows of the matrix were defined by the observed answers, and a column was created for each participant. The cells consisted of blocks of text, either quotations or summations. Patterns identified in these reviews formed the basis for further classification into higher-level matrices in which various themes were identified. Finally, the initial information obtained from the transcribed encounters was reduced to keywords, summarizing the trends and patterns observed in each of the sets. Herein we present two case examples to illustrate selfcare themes. The content of these exchanges was not modified; only potentially identifying information was omitted to protect participants' privacy.
Quantitative analysis:
Quantitative variables such as patients' demographic characteristics and length of the encounters were assessed by using descriptive statistics. We computed the odds ratio of discussing each of the 10 self-care elements during a clinical encounter between low EMR use encounters and moderate to high EMR use encounters, and we used the Fisher exact test to infer the significance of the EMR use effect.30 To further describe differences between low EMR use encounters and moderate to high EMR use encounters, we investigated the relationship between the time spent using the EMR and the total duration of each encounter. Regression analyses were performed in order to observe relationships between continuous variables, such as total encounter time and the total number of minutes the EMR was used by the physicians. We performed t tests in order to observe differences between low EMR use encounters and moderate to high EMR use encounters. The desired significance level was set at 0.05 for each of the inferential tests. The SPSS 9.0 statistical package was used for quantitative analysis purposes.
Results
Encounters/subjects:
The average length of encounter time for the 50 encounters was 22.6 minutes (range: 5–47, SD = 8.9). The average number of encounters videotaped per physician was 8 (range: 3–11, SD = 3.2). The majority (49) of the patients was male, and the mean age of the enrolled patients was 64.5 years (range: 40–86, SD = 13.4). The mean number of years the patients had been seeing their providers was 4.8 years (range: 3–5.75, SD = 0.74). Twenty-two patients (44 percent) were Hispanic; 20 (40 percent) were non-Hispanic white; 6 (12 percent) were African American; and 2 (4 percent) identified their ethnic background as “other.” All six of the staff physicians were non-Hispanic white, four (66 percent) were female, and each physician had been in practice at least eight years.
Patients came to the clinic with different kinds of chronic illnesses. The most frequent diseases encountered were diabetes (20 patients, 40 percent), hypertension (14 patients, 28 percent), and cardiovascular diseases (9 patients,18 percent). Depression (3 patients, 6 percent), arthritis (2 patients, 4 percent), and cancer (2 patients, 4 percent) were also seen. Frequency distributions of different illnesses were very similar between low EMR use encounters and moderate to high EMR use encounters (Table 3). For example, among patients with the most frequent diagnoses, such as diabetes, 15 patients (30 percent of all patients) were in the group with moderate to high EMR use encounters while 5 patients (10 percent of all patients) were in the group with low EMR use encounters. Similarly, for patients with hypertension, 10 (20 percent of all patients) were in the group with moderate to high EMR use encounters while 4 (8 percent of all patients) were among the group with low EMR use encounters.
Table 3.
Frequency Distribution of Different Illnesses by EMR Use in Encounters
| Low EMR Use Encounters (n = 13) | Moderate to High EMR Use Encounters (n = 37) | Total Encounters (n = 50) | |
| Diabetes | 5 (10%) | 15 (30%) | 20 (40%) |
| Hypertension | 4 (8%) | 10 (20%) | 14 (28%) |
| Cardiovascular disease | 2 (4%) | 7 (14%) | 9 (18%) |
| Depression | 1 (2%) | 2 (4%) | 3 (6%) |
| Arthritis | 1 (2%) | 1 (2%) | 2 (4%) |
| Cancer | 0 (0%) | 2 (4%) | 2 (4%) |
EMR usage:
In 13 encounters, physicians used the EMR for two minutes or less (low use), whereas in 37 encounters, physicians used the EMR for five minutes or more (moderate to high use). For three physicians, all encounters fell among the moderate to high category, while the other three had both low use and moderate to high use encounters (Table 2). The average length of encounters among moderate to high EMR use encounters was 25 minutes, compared to 16 minutes for encounters with low EMR use (t test, p < 0.001).
Table 2.
Computer Usage by Providers
| 2 Minutes or Less (n = 13) | 5 Minutes or More (n = 37) | |
| Provider number | ||
| 1 | 6 encounters | 5 encounters |
| 2 | 1 encounter | 8 encounters |
| 3 | 6 encounters | 2 encounters |
| 4 | 0 encounters | 8 encounters |
| 5 | 0 encounters | 11 encounters |
| 6 | 0 encounters | 3 encounters |
Self-care elements discussed during the encounters:
Issues pertaining to different facets of selfcare management were discussed in every physician-patient interaction. Table 4 describes the frequency distribution of self-care elements by high and low EMR use encounters. The most frequent self-care topics discussed were medication (50 encounters, 100 percent), followed by physical distress (38 encounters, 76 percent) and disease symptoms (38 encounters, 76 percent). Self-monitoring activities were discussed in 31 encounters (62 percent), while exercise and diet were discussed in 30 encounters (60 percent) and 23 encounters (46 percent) respectively. Smoking (15 encounters, 30 percent), family support/community resources (13 encounters, 26 percent), emotional distress (13 encounters, 37 percent), and alcohol consumption (10 encounters, 20 percent) were the least discussed issues.
Table 4.
Frequency Distribution of Self-Care Elements Discussed during Encounters among Moderate to High EMR Use Encounters and Low EMR Use Encounters (N = 50)
| Self-Care Element | Moderate to High EMR Use (n = 37) | Low EMR Use (n = 13) | Odds Ratio (p value) and 95% Confidence Interval for Overall Self-Care Discussion | |||
| Total Frequency (%) | Total Frequency (%) | |||||
| Disease symptoms | 31 | 84 | 7 | 54 | 4.4 (0.05) | |
| 22.143 | ||||||
| 0.8645 | 3 | |||||
| Self-monitoring activities | 25 | 68 | 6 | 46 | 2.4 (0.2) | |
| 10.775 | ||||||
| 0.5509 | 2 | |||||
| Discussion of medication use | 37 | 100 | 13 | 100 | *Not available (1.0) | |
| *Not available | ||||||
| Diet | 19 | 51 | 4 | 30 | 2.3 (0.3) | |
| 0.5317 | 12.287 | |||||
| Exercise | 22 | 59 | 8 | 62 | 0.9 (1.0) | |
| 0.1959 | 3.9497 | |||||
| Alcohol consumption | 8 | 22 | 2 | 15 | 1.5 (1.0) | |
| 16.729 | ||||||
| 0.2423 | 6 | |||||
| Cigarette smoking | 14 | 38 | 1 | 7 | 7.3 (0.07) | |
| 334.13 | ||||||
| 0.8653 | 6 | |||||
| Family support/community resources | 9 | 24 | 4 | 31 | 0.7 (0.71) | |
| 0.1514 | 4.028 | |||||
| Emotional distress | 12 | 32 | 1 | 8 | 5.7 (0.14) | |
| 266.40 | ||||||
| 0.6733 | 1 | |||||
| Physical distress | 32 | 86 | 6 | 46 | 7.4 (0.006) | |
| 40.082 | ||||||
| 1.4159 | 3 | |||||
This is because the odds for both groups are infinity (37/0 and 13/0).
Initiation of self-care exchanges during the patients' visits:
Table 5 displays the self-care topics by who initiated the discussion of them. Interestingly, medication use was discussed in every physicianpatient interaction, with 25 encounters (50 percent) in which physicians initiated the discussion related to this topic and 25 encounters (50 percent) in which patients initiated the discussion. Exercise and diet were discussed in about 50 percent of the encounters. Discussion pertaining to diet was initiated by physicians in 15 encounters (30 percent) and by patients in 8 encounters (16 percent). Discussion of disease symptoms was more often initiated by physicians (21 encounters, 42 percent) than by patients (17 encounters, 34 percent). Discussion of physical distress was initiated by patients in 23 encounters (46 percent) and by physicians in 15 encounters (30 percent); in 12 encounters (24 percent) the topic of physical distress was not included.
Table 5.
Discussion of Self-Care Elements Initiated by Patients and Physicians during Encounters (N = 50)
| Self-Care Element | Initiated by Physician | Initiated by Patient | Total Discussed | Not Discussed |
| Frequency (%) | Frequency (%) | Frequency (%) | Frequency (%) | |
| Disease symptoms | 21 (42) | 17 (34) | 38 (76) | 12 (24) |
| Self-monitoring activities | 23 (46) | 8 (16) | 31 (62) | 19 (38) |
| Discussion of medication use | 25 (50) | 25 (50) | 50 (100) | 0.0 (0.0) |
| Diet | 15 (30) | 8 (16) | 23 (46) | 27 (54) |
| Exercise | 15 (30) | 15 (30) | 30 (60) | 20 (40) |
| Alcohol consumption | 8 (16) | 2 (4) | 10 (20) | 40 (80) |
| Cigarette smoking | 13 (26) | 2 (4) | 15 (30) | 35 (70) |
| Family support/community resources | 7 (14) | 6 (12) | 13 (26) | 37 (74) |
| Emotional distress | 7 (14) | 6 (12) | 13 (26) | 37 (74) |
| Physical distress | 15 (30) | 23 (46) | 38 (76) | 12 (24) |
| Total | 149 | 112 | 261 | 239 |
EMR usage and self-care exchanges in encounters:
We examined the proportion of time providers spent using the EMR and the total number of self-care elements discussed during encounters. The mean proportion of EMR usage was 0.35 (range: 0-0.7, SD = 0.23) for all encounters. The mean proportion of EMR usage was 0.46 (range: 0.13–0.7, SD = 0.16) among moderate to high EMR use encounters, while it was 0.02 (range: 0–0.06, SD = 0.02) among low EMR use encounters (t test, p = 0.04).
The average number of self-care elements discussed was 7 (range: 2–13; SD = 2.7) among moderate to high EMR use encounters, compared to 3.4 (range: 2–9, SD = 1.8) for low EMR use encounters (t test, p < 0.05). A significant correlation was observed between the number of self-care elements discussed and the proportion of time spent on the EMR (r = 0.6, p < 0.05). No significant relationship was found between the length of the encounters and self-care discussion (r = 0.009, p = 0.90).
We also examined the role of EMR usage in patient-provider communication regarding self-care by comparing self-care discussion between moderate to high EMR use encounters and low EMR use encounters (Table 4 and table 6). We computed the odds ratio (Table 6) of discussing each self-care element during the clinical encounter between the two EMR usage groups, and we used the Fisher exact test to infer the significance of the EMR usage. During moderate to high EMR use encounters physicians were more likely to initiate self-care topics than during low EMR use encounters, particularly on disease symptoms (odds ratio = 4.4, p = 0.05) and physical distress (odds ratio = 7.4, p = 0.006) (Table 4).
Table 6.
Odds Ratio (p value) and 95% Confidence Interval for Self-Care Discussion and EMR Use
| Self-Care Element (Total Times Discussed) | Odds Ratio (p value) and 95% Confidence Interval for Physician-Initiated Self-Care Discussion | Odds Ratio (p value) and 95% Confidence Interval for Patient-Initiated Self-Care Discussion | ||
| Disease symptoms (38) | 5.8 (0.04) | 0.76 (0.74) | ||
| 1.0146 | 59.1178 | 0.175 | 3.6752 | |
| Self-monitoring activities (31) | 0.9 (1.0) | Infinity (0.09) | ||
| 0.2328 | 4.3372 | 0.6422 | +Inf | |
| Discussion of medication use (50) | 0.7 (0.75) | 1.36 (0.75) | ||
| 0.1585 | 3.1553 | 0.3169 | 6.3105 | |
| Diet (23) | 1.6 (0.72) | 2.8 (0.6) | ||
| 0.322 | 10.6103 | 0.2976 | 136. 547 | |
| Exercise (30) | 2.8 (0.19) | 0.25 (0.1) | ||
| 0.5839 | 18.2576 | 0.0459 | 1.4156 | |
| Alcohol consumption (10) | 2.8 (0.66) | 0.33 (0.45) | ||
| 0.2976 | 136.547 | 0.0041 | 28.3 285 | |
| Cigarette smoking (15) | 5.7 (0.14) | Infinity (0.1) | ||
| 0.6733 | 266.401 | 0.0648 | +Inf | |
| Family/community support (13) | 0.8 (1.0) | 0.66 (0.64) | ||
| 0.1183 | 10.284 | 0.0824 | 8.3967 | |
| Emotional distress (13) | Infinity (0.16) | 1.87 (1.0) | ||
| 0.5287 | + Inf | 0.1789 | 95.9 665 | |
| Physical distress (38) | 7.3 (0.07) | 1.5 (0.70) | ||
| 0.8653 | 334.136 | 0.3533 | 7.0 15 | |
The role of EMR usage in facilitating communication regarding self-care:
Direct observations of the videotaped encounters showed that physicians' use of the EMR enhanced the discussion of self-care during encounters by giving the physicians easy access to patients' data such as lab results and vital signs (including the pain rating collected by the nurse while taking vital signs). It seems that the use of an EMR during patients' visits has both direct and indirect impact on physicians' initiation of questions related to self-care. A direct impact could be through physicians' use of the list of problems that is embedded in the notes. Reviewing the list of problems with the patients will prompt more probing for symptoms, whereas looking at the vital signs results or the presence of pain medication on the medication list will raise questions about physical distress or pain.
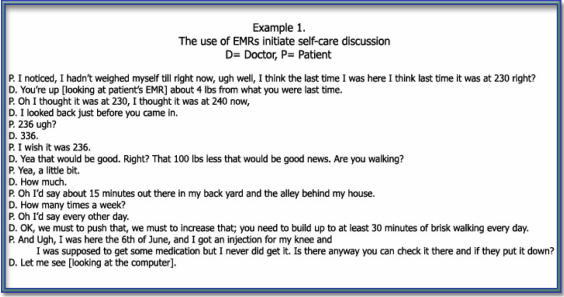
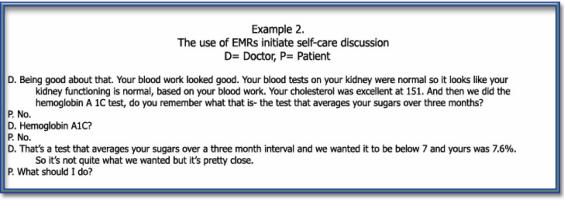
Furthermore, the use of an EMR might have an indirect impact on physicians' initiations of self-care topics and result in better informational exchange about self-care. For example, the use of the lab data provided physicians with information about control of blood glucose or the vital signs data about blood pressure and weight. This information initiates discussion of a specific element of self-care such as diet that in turn leads to expansion to other related self-care elements. In Case Example 1, the physician used the EMR to review the patient's vital signs. The patient's increase in weight led to further discussion about other important self-care topics, such as physical activity. The physician initiated several questions concerning the kind and duration of the patient's physical activities. This in turn advanced the self-care discussion to unfold important issues about the patient's physical pain and medication problems. In Case Example 2, the physician was reviewing the patient's lab work and sharing the information with the patient. The physician asked and initiated the discussion of the patient's HbA1c results. The patient asked questions about the purpose of the test. This patient's question initiated several question-and-response exchanges that provided more informational flow between the physician and the patient.
Case Example One.
Case Example Two.
Discussion
The impact of patient-provider communication on healthcare is now well established in the literature.31–33 Learning how to translate this effect into strategies to improve self-care management in chronic illness is essential.34,35 Our data showed that all examined encounters were similar with respect to the kinds of self-care elements discussed. However, moderate to high EMR use encounters were more likely to increase the number of self-care topics raised by physicians than low EMR use encounters, particularly on disease symptoms and physical distress. We examined the impact of several potential confounders on the use of the EMR and self-care communication during patients' visits. These confounders included the timing of the interviews, the specialties of the physicians seeing patients, and the diagnoses of patients in the study. No significant relationship was found between these confounders and self-care discussion.
Additionally, our data showed that providers but not patients initiated higher numbers of self-care topics during moderate to high EMR use encounters. Self-care topics initiated by patients were comparable between the two EMR usage groups. The use of EMRs during clinical encounters has the potential to improve self-care communication. EMRs offer the opportunity to involve patients and providers in effective discussion about the different aspects of self-care.36
The use of the EMR during outpatient visits can be conceptualized as a system-based, qualityimprovement intervention that directly and indirectly prompts physicians to initiate specific questions related to self-care. Our findings indicated that EMR usage allowed providers immediate access to large amounts of medical data for each patient. As physicians access the EMR to review their patients' lab data, they exchange what they see with their patients. Physicians raise specific questions with the patients in the case of abnormal lab findings. These questions initiate a chain of question-and-response sequences related to self-care management, inviting patients to participate in self-care exchanges during the visit. This finding is supported by a previous study that demonstrated that physicians who used EMRs adopted a more active role in clarifying information, encouraging questions, and ensuring completeness of the visit compared to those who did not use EMRs.37,38
Generally speaking, we found that patients and providers tended to initiate disease-based but not behavior-based self-care discussions. For example, both patients and providers initiated discussions of medication use and physical distress, whereas discussions of issues pertaining to exercise and diet were less frequent and more likely initiated by physicians. Exchanges related to alcohol consumption and smoking occurred least frequently, and when those topics were raised, the discussions were mainly initiated by physicians. This finding is not surprising; several studies have shown that the current healthcare system is disease centered, in which physicians make treatment decisions based largely on clinical practice guidelines, clinical experience, and data from various medical tests.39 Our findings bring attention to the importance of integrating and involving patients in exchanges specific to evidence-based, behavior-specific self-care management during visits. Examples include discussion about diet, exercise, cigarette smoking, and alcohol consumption. Integrating behavior-specific self-care communication may allow physicians to find out about reasons for noncompliance and try to address them.
Future EMRs hold the potential for self-care management enhancements. We anticipate at least two directions in which future EMRs might evolve. One direction is the development of software enhancements that take into consideration the interface between EMR use and self-care communication. Examples of the type of software enhancements that might emerge as both feasible and potentially effective from our observational work include
patient self-assessments that could be filled out on tablet PCs before visits and uploaded into an EMR for use during visits. This enhancement is feasible and avoids issues related to patients' limited access to the Internet or limited computer literacy. Patients' self-assessments could include weight, food intake, exercise logs, or glucose meter data.
Software enhancements could also include additional graphic display capabilities, in particular of medication refill histories to display to patients the effects of gaps in refills combined with blood pressure readings or glucose readings.
The second direction of future EMR enhancement could aim to improve the clinical microsystem. Examples of the types of changes include
placement of a large monitor in the exam room to allow easy information exchange and graphic display for patients' review, such as to display lab results on the computer to patients during encounters, and
placement of readily available printers for ease of giving printouts to patients. Different kinds of health-related materials, such as medication lists, could be printed from the EMR for presenting results to patients.
The potential implications of EMR use presented in this study add to the existing efforts of linking data at multiple levels-patients, providers, and caregivers.40,41 Future EMRs may offer a new level of connectivity for health information across multiple domains to enhance self-care activities such as selfmonitoring, diet, and exercise and therefore improve the care of chronically ill people. The attention to electronic medical records comes not only from the need to communicate but also from a desire to reduce administrative costs and to improve services and quality of care to patients.42 As physicians recognize the potential benefits of increased office efficiency and improved patient care, general health providers and specialists will begin to implement and use EMRs in their work.43 This will signify stepping stones that are leading to the transformation of the healthcare system. Eventually, an information-enabled system will emerge that is very different and more efficient than today's document-bound, fragmented delivery system.44,45
Limitations of the findings:
The study focused on conducting an in-depth analysis to understand the role of EMR usage on patient-provider communication regarding self-care among a small group of providers. Our goal was not to generalize the findings to a broader population of patients and providers. Our data have provided some important insights regarding the current and potential future role of EMR usage on patient-provider self-care communication, yet they have some limitations. Our analysis focused on describing the use of EMRs during patients' visits just after the VA had implemented the system in an outpatient primary-care clinic. A control group of physicians who did not use the EMR system was not part of the study. Future research should address whether physicians who had higher self-care communication skills have done better than the other physicians regardless of whether or not they used the electronic medical record system.
Additionally, data were collected based on a cross-sectional study design with only one visit for each patient-provider dyad, which limited our understanding of how the use of an EMR affects discussion of self-care during patients' visits over time. A longitudinal study would be an important future inquiry to substantiate the cause-and-effect relations and to enhance our understanding of the dynamic of self-care communication during patients' visits over time. Self-care is a dynamic process, and discussion regarding self-care might vary from a patient's first visit to subsequent visits. We attempted to address this limitation by using the encounters as our unit of analysis, instead of patients or providers. By doing that, we were able to examine the 50 encounters as a whole to analyze self-care exchanges.
Also, our study included analysis of a sample with a majority of male veteran patients. The provider sample in our study was small (N = 6), and all were non-Hispanic white. These limitations did not allow us to examine the influence of gender or ethnicity on patient-provider self-care communication. Future studies of the impact of ethnicity and gender on the use of EMRs and self-care communication are justified.
Acknowledgements
This work was funded by VA Health Services Research and Development/Veterans Evidence-based Research, Dissemination, and Implementation Center/Audie L. Murphy Memorial Veterans Hospital, San Antonio, Texas. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Contributor Information
Nedal H Arar, University of Texas Health Science center and and investigator at VERDICT, a VA HSR&D Research Enhancement and Advancement Program in San Antonio, TX.
Chen-Pin Wang, University of Texas Health Science center and VERDICT, a VA HSR&D Research Enhancement and Advancement Program in San Antonio, TX.
Jacqueline A Pugh, University of Texas Health Science center and VERDICT, a VA HSR&D Research Enhancement and Advancement Program in San Antonio, TX..
Notes
- 1.Cegala D. J, McClure L, Marinelli T. M, Post D. M. The Effects of Communication Skills Training on Patients' Participation during Medical Interviews. Patient Education and Counseling. 2000;41:209–22. doi: 10.1016/s0738-3991(00)00093-8. [DOI] [PubMed] [Google Scholar]
- 2.Stewart M, Brown J. B, Donner A, McWhinney I. R, Oates J, Weston W. W, et al. The Impact of Patient-centered Care on Outcomes. Journal of Family Practice. 2000;49:796–804. [PubMed] [Google Scholar]
- 3.Stewart C. J, Cash. W. B. Interviewing: Principles and Practices. 9th ed. Boston: McGraw-Hill College; 2000. [Google Scholar]
- 4.Norris S. L, Engelgau M. M, Narayan K. M. Effectiveness of Self-Management Training in Type 2 Diabetes: A Systematic Review of Randomized Controlled Trials. Diabetes Care. 2001;24:561–87. doi: 10.2337/diacare.24.3.561. [DOI] [PubMed] [Google Scholar]
- 5.Renders C. M, Valk G. D, Griffin S, Wagner E. H, Eijk J. T, Assendelft W. J. Cochrane Database of Systematic Reviews. 2001. Interventions to Improve the Management of Diabetes Mellitus in Primary Care, Outpatient and Community Settings; p. CD001481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Corbin J, Strauss A. Unending Work and Care: Managing Chronic Illness at Home. San Francisco: Jossey-Bass; 1988. [Google Scholar]
- 7.Johnson S. B. Methodological Issues in Diabetes Research: Measuring Adherence. Diabetes Care. 1992;15:1658–67. doi: 10.2337/diacare.15.11.1658. [DOI] [PubMed] [Google Scholar]
- 8.American Diabetes Association. Diabetes and Exercise: The Risk-Benefit Profile. In: Devlin J, Ruderman N, editors. The Health Professional's Guide to Diabetes and Exercise. Alexandria, VA: American Diabetes Association; 1995. pp. 3–4. [Google Scholar]
- 9.Hall J. A, Roter D. L, Katz N. R. Meta-analysis of Correlates of Provider Behavior in Medical Encounters. Medical Care. 1988;26:657–75. doi: 10.1097/00005650-198807000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Center for Health Studies of Group Health Cooperative of Puget Sound. An Indexed Bibliography on Self-Management for People with Chronic Disease. 1st ed. Washington, DC: Center for the Advancement of Health; 1996. [Google Scholar]
- 11.Teutsch C. Patient-Doctor Communication. Medical Clinics of North America. 2003;87:1115–45. doi: 10.1016/s0025-7125(03)00066-x. [DOI] [PubMed] [Google Scholar]
- 12.Von Korff M, Gruman J, Schaefer J, Curry S. J, Wagner E. H. Collaborative Management of Chronic Illness. Annals of Internal Medicine. 1997;127:1097–1102. doi: 10.7326/0003-4819-127-12-199712150-00008. [DOI] [PubMed] [Google Scholar]
- 13.Hall, J. A., D. L. Roter, and N. R. Katz. “Meta-analysis of Correlates of Provider Behavior in Medical Encounters.” [DOI] [PubMed]
- 14.Cegala, D. J., L. McClure, T. M. Marinelli, and D. M. Post. “The Effects of Communication Skills Training on Patients' Participation during Medical Interviews.” [DOI] [PubMed]
- 15.Hall, J. A., D. L. Roter, and N. R. Katz. “Meta-analysis of Correlates of Provider Behavior in Medical Encounters.” [DOI] [PubMed]
- 16.Arar N. H, Wen L, McGrath J, Steinbach R, Pugh J. A. Communicating about Medications during Primary Care Outpatient Visits: The Role of Electronic Medical Records. Informatics in Primary Care. 2005;13:13–22. doi: 10.14236/jhi.v13i1.576. [DOI] [PubMed] [Google Scholar]
- 17.Makoul G, Curry R. H, Tang P. C. The Use of Electronic Medical Records: Communication Patterns in Outpatient Encounters. Journal of the American Medical Informatics Association. 2001;8:610–15. doi: 10.1136/jamia.2001.0080610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Von Korff, M., J. Gruman, J. Schaefer, S. J. Curry, and E. H. Wagner. “Collaborative Management of Chronic Illness.” [DOI] [PubMed]
- 19.Hall, J. A., D. L. Roter, and N. R. Katz. “Meta-analysis of Correlates of Provider Behavior in Medical Encounters.” [DOI] [PubMed]
- 20.Center for Health Studies of Group Health Cooperative of Puget Sound. An Indexed Bibliography on Self-Management for People with Chronic Disease. [Google Scholar]
- 21.Arar, N. H., L. Wen, J. McGrath, R. Steinbach, and J. A. Pugh. “Communicating about Medications during Primary Care Outpatient Visits: The Role of Electronic Medical Records.” [DOI] [PubMed]
- 22.Clement S. Diabetes Self-Management Education. Diabetes Care. 1995;18(8):1204–14. doi: 10.2337/diacare.18.8.1204. [DOI] [PubMed] [Google Scholar]
- 23.Glasgow R. E, Anderson R. M. In Diabetes Care, Moving from Compliance to Adherence Is Not Enough: Something Entirely Different Is Needed. Diabetes Care. 1999;22(12):2090–92. doi: 10.2337/diacare.22.12.2090. [DOI] [PubMed] [Google Scholar]
- 24.Krein S. L, Hayward R. A, Pogach L, BootsMiller B. J. Department of Veterans Affairs' Quality Enhancement Research Initiative for Diabetes Mellitus. Medical Care. 2000;38(6, Suppl. 1):I38–I48. doi: 10.1097/00005650-200006001-00005. [DOI] [PubMed] [Google Scholar]
- 25.Renders, C. M., G. D. Valk, S. Griffin, E. H. Wagner, J. T. Eijk, and W. J. Assendelft. “Interventions to Improve the Management of Diabetes Mellitus in Primary Care, Outpatient and Community Settings.” [DOI] [PMC free article] [PubMed]
- 26.Center for the Advancement of Health. Health Behavior Change in Managed Care: A Status Report. Washington, DC: Center for the Advancement of Health; 2000. Selected Evidence for Behavioral Approaches to Chronic Disease Management in Clinical Settings: Asthma. [Google Scholar]
- 27.Elwood J. M. Critical Appraisal of Epidemiological Studies and Clinical Trials. 2nd ed. New York: Oxford University Press; 1998. [Google Scholar]
- 28.Miles M, Huberman A. Qualitative Data Analysis: An Expanded Source Book. 2nd ed. Thousand Oaks, CA: Sage; 1994. [Google Scholar]
- 29.Pelto J, Pelto G. H. Field Methods in Medical Anthropology. In: Johnson T. M, Sargent C. E, editors. Medical Anthropology: Contemporary Theory and Method. New York: Praeger; 1990. pp. 269–297. [Google Scholar]
- 30.Vuong Q. H. Likelihood Ratio Tests for Model Selection and Non-nested Hypotheses. Econometrica. 1989;57:307–33. [Google Scholar]
- 31.Cegala, D. J., L. McClure, T. M. Marinelli, and D. M. Post. “The Effects of Communication Skills Training on Patients' Participation during Medical Interviews.” [DOI] [PubMed]
- 32.Stewart, M., J. B. Brown, A. Donner, I. R. McWhinney, J. Oates, W. W. Weston, et al. “The Impact of Patient-centered Care on Outcomes.” [PubMed]
- 33.Stewart C. J, Cash W. B. Interviewing: Principles and Practices. [Google Scholar]
- 34.Hunt L. M, Arar N. H. The Contrasting Perspectives Model for Studying Treatment Behaviors in Chronic Disease Management: The Case of Type 2 Diabetes. Medical Anthropology Quarterly. 2001;153:1–21. doi: 10.1525/maq.2001.15.3.347. [DOI] [PubMed] [Google Scholar]
- 35.Heisler M, Bouknight R. R, Hayward R. A, Smith D. M, Kerr E. A. The Relative Importance of Physician Communication, Participatory Decision Making, and Patient Understanding in Diabetes Self-Management. Journal of General Internal Medicine. 2002;17:243–52. doi: 10.1046/j.1525-1497.2002.10905.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bates D. W, Leape L, Cullen D, Laird N, Seger L. Effect of Computerized Physician Order Entry and Team Intervention on Prevention of Serious Medical Errors. Journal of the American Medical Association. 1998;280:1311–16. doi: 10.1001/jama.280.15.1311. [DOI] [PubMed] [Google Scholar]
- 37.Ibid.
- 38.Litvin C. B, Ornstein S. M, Anthony W. E, Tanner D. Quality Improvement Using Electronic Medical Records: A Case Study of a High-performing Practice. Topics in Health Information Management. 2001:59–64. [PubMed] [Google Scholar]
- 39.Von Korff, M., J. Gruman, J. Schaefer, S. J. Curry, and E. H. Wagner. “Collaborative Management of Chronic Illness.” [DOI] [PubMed]
- 40.Hippisley-Cox J, Pringle M, Cater R, et al. The Electronic Patient Record in Primary Care-Regression or Progression? A Cross Sectional Study. British Medical Journal. 2003;326:1439–43. doi: 10.1136/bmj.326.7404.1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Winkelman W. J, Leonard K. J, Rossos P. G. Patient-Perceived Usefulness of Online Electronic Medical Records: Employing Grounded Theory in the Development of Information and Communication Technologies for Use by Patients Living with Chronic Illness. Journal of the American Medical Informatics Association. 2005;12(3):306–14. doi: 10.1197/jamia.M1712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nelson R. Connecting the Providers in Your Healthcare Community: One Step at a Time. Frontiers of Health Services Management. 2005;22(2):13–28. [PubMed] [Google Scholar]
- 43.Goradia V. K. Electronic Medical Records for the Arthroscopic Surgeon. Arthroscopy. 2006;22(2):219–224. doi: 10.1016/j.arthro.2005.11.014. [DOI] [PubMed] [Google Scholar]
- 44.Sachs M. A. Transforming the Health System from the Inside Out. Frontiers of Health Services Management. 2005;22(2):3–12. [PubMed] [Google Scholar]
- 45.Drury B. M. Ambulatory EHR Functionality: A Comparison of Functionality Lists. Healthcare Information Management. 2006;20(1):61–70. [PubMed] [Google Scholar]