Abstract
INTRODUCTION
Anal fissures are commonly encountered in routine colorectal practice. Developments in the pharmacological understanding of the internal anal sphincter have resulted in more conservative approaches towards treatment. Simple measures are often effective for early fissures. Glyceryl trinitrate is well established as a first-line pharmacological therapy. The roles of diltiazem and botulinum, particularly as rescue therapy, are not well understood. Surgery has a defined role and should not be discounted completely.
METHODS
Data were obtained from Medline publications citing ‘anal fissure’. Manual cross-referencing of salient articles was conducted. We have sought to highlight various controversies in the management of anal fissures.
FINDINGS
Acute fissures may heal spontaneously, although simple conservative measures are sufficient. Idiopathic chronic anal fissures need careful evaluation to decide what therapy is suitable. Pharmacological agents such as glyceryl trinitrate (GTN), diltiazem and botulinum toxin have been subjected to most scrutiny. Though practices in the UK vary, GTN or diltiazem would be suitable as first-line therapy with botulinum toxin used as rescue treatment. Sphincterotomy is indicated for unhealed fissures; fissurectomy has been revisited and advancement flaps have a role in patients in whom sphincter division is not suitable.
Keywords: Anal fissures, Glyceryl trinitrate, Diltiazem, Botulinum toxin, Sphincterotomy
An anal fissure is a split in the skin of the distal anal canal. Young adults of both sexes are affected equally. Patients present with anal pain commonly during defaecation and/or rectal bleeding. Whilst acute fissures heal spontaneously or with simple therapeutic measures, a proportion progress to form a chronic linear ulcer. Chronicity of a fissure relates to duration of greater than 6 weeks with fibres of the internal anal sphincter visible at the base of the fissure. Associated pathology may include a sentinel ‘pile’ distally and a fibro-epithelial polyp at the apex. Most anal fissures are idiopathic with no identifiable underlying disease process. There is no simple and unified theory to explain their genesis though constipation and lack of dietry fibre are implicated. Most fissures occur in the posterior midline; this may be anatomically related as there is a lack of tissue support posteriorly within the anal canal. Fissures associated with pregnancy are commonly located anteriorly and are often associated with low anal canal pressures. Other causes of fissures include Crohn's disease, syphilis, human immuno-deficiency virus (HIV) or tuberculosis. These are secondary fissures and are most appropriately treated by addressing the underlying disease process.
Treatment of anal fissures
Conservative measures
The initial approach in the treatment of anal fissures is non-operative. An acute anal fissure may heal spontaneously or in response to medical therapy with warm baths, stool softeners, bulk laxatives, analgesics, topical anaesthetics and re-assurance.1 Dietary bran supplements and warm sitz baths are superior to topically applied, local anaesthetic or hydrocortisone cream2 and fibre ingestion results in fewer recurrences.3 Regular anal dilatation to treat anal fissures is not recommended.4 Other therapies such as cautery, suppositories and sitz baths have been disappointing with low healing rates and high long-term recurrences.5
Operative strategies
Most chronic anal fissures are associated with a raised internal anal sphincter (IAS) pressure and reduced vascular perfusion at the base. Current treatment has aimed at reducing resting anal pressure by diminishing sphincter tone and improving blood supply at the site of the fissure, thus promoting the healing rate.
ANAL DILATATION
Manual dilatation of the anus first described by Récamier in 1838 is a simple procedure and previously a popular treatment option. Its re-introduction by Goligher and Watts led to its popularisation.6 However, incontinence was a concern and endo-anal ultrasonography provided an insight as to the degree of damage associated with this procedure; fragmentation is often seen.7-8 In an attempt to minimise incontinence, some have advocated gentle digital dilatation of the anus under total neuromuscular blockade, with incontinence seen in 9 (3.8%) of 273 patients following this procedure in one study.9 Despite these reports, incontinence is a concern and current opinion is that manual dilatation of the anus for the treatment of anal fissures is not recommended.
INTERNAL ANAL SPHINCTEROTOMY
Early advocates of sphincterotomy recommended a generous division of the IAS muscle and, in some cases, total division extending to the circular muscle of the rectum. By 1959, the ‘standard internal sphincterotomy’ comprised division of only half of the IAS to the dentate line in its lateral or posterolateral part.10 Posterior sphincterotomy results in a ‘keyhole deformity’ that can cause mucous leakage in approximately a third of patients and should no longer be performed.11
Notaras12 is credited for promoting the technique of lateral subcutaneous internal sphincterotomy. In this technique, the lower part of the internal sphincter is divided by introducing the knife blade at the anal verge between the anal canal mucosa and the IAS, then directing the cutting edge laterally towards the IAS. Hoffman and Goligher modified this technique by passing the blade between the internal and external sphincters and cutting medially. Both the subcutaneous and open techniques seem equally efficacious with regards to extent of division and effect on anal pressures.13
There are certain principles that should be noted:
The sphincterotomy should be away from the fissure site so that intact mucosal bridges fill the gap between divided muscle fibres to allow rapid healing.
The entire thickness of the lower internal sphincter must be divided, as any remaining intact fibres go into intense spasm to compensate for the divided fibres.
The mucosa over the sphincterotomy site should not be breached as this would predispose to infection.
The upper one-third of the sphincter must remain intact for continence.
The length of the sphincterotomy should be ‘tailored’ to the length of the anal fissure.
Sphincterotomy induces a sustained reduction of maximum resting anal pressure.14 The largest review of the sequelae of internal sphincterotomy for chronic fissure in ano showed rates of flatus incontinence in 715 patients, occurring ‘sometimes’ to ‘infrequently’ in 255 (35.7%), faecal urgency in 35 (4.9%) and soiling in 152 (21.2%).15 Incontinence may be minimised by a ‘tailored sphincterotomy’ where the sphincter is divided to the length of the fissure; this does not appear to compromise the healing rate.16
FISSURECTOMY/FISSURECTOMY AND SPHINCTEROTOMY
Fissurectoniy has a role in midline fissures complicated by underlying fistula. Though further work by Bode et al., Gingold and Di Castro et al. demonstrated fissurectoniy as a viable treatment option, its use has remained sporadic. The recent use with pharmacological agents such as topical isosorbide dinitrate to treat fissures has led to its reintroduction.17
ANAL ADVANCEMENT FLAP
This is indicated for patients with primary or recurrent fissures and for women with a complicated obstetric history with low resting anal canal pressure. In order to aid selection of suitable cases, prior manometry and endosonography is employed. This operation avoids further disruption to the internal sphincter and avoids factors that might otherwise jeopardise continence. Skin flaps can either be triangular (Y-V), a square-shaped sliding graft or a C-anoplasty.18
Endo-anal ultrasound imaging of the anal sphincters
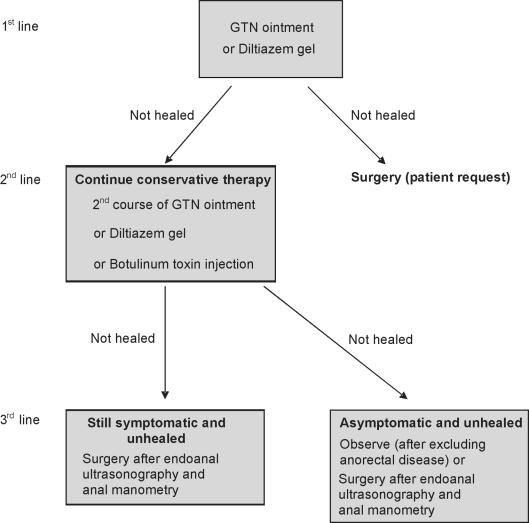
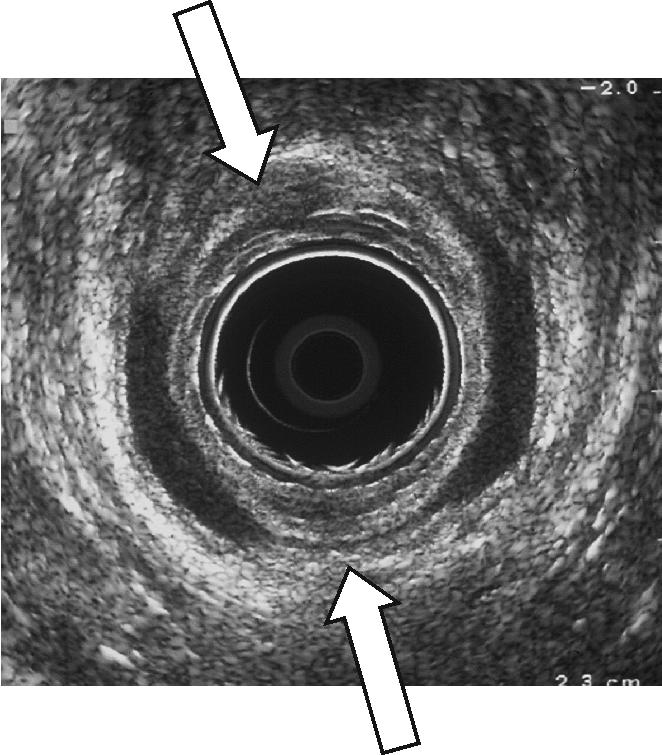
Anal dilatation can be regarded as an uncontrolled tearing procedure that damages the sphincter muscles with considerable detriment to anal function (Fig. 1). Lateral sphincterotomy results in a discrete defect of the IAS; in women, the extent of the division can be greater due the relatively shorter anal canal length (Fig. 2). Endo-anal ultrasonography has also identified inadvertent division of the EAS or inadequate division as reasons for failure of a fissure to heal.19
Figure 1.
Endo-anal ultrasound demonstrating the appearance of the internal anal sphincter (IAS) after manual dilatation for chronic anal fissure. The white arrows indicate the defects in the IAS.
Figure 2.
Endo-anal ultrasound demonstrating the appearance of the internal anal sphincter (IAS) after lateral sphincterotomy for chronic anal fissure. The white arrow indicates the defect in the IAS.
Chemical sphincterotomy
This term refers to pharmacological manipulation of anal sphincter tone as an alternative modality to surgery for the treatment of anal fissures. The optimal treatment for anal fissures is to induce a temporary reduction of anal canal pressure to promote healing of the fissure without permanently disrupting normal sphincter function. A reduction in anal sphincter tone is achievable by enhancing IAS relaxation through direct action on internal anal sphincter smooth muscle cells. These mechanisms serve to reduce intracellular Ca2+, which reduces the tonic state of the muscle. These can occur through nitric oxide donation, direct intracellular Ca2+ depletion, muscarinic receptor stimulation, α-adrenergic inhibition or β-adrenergic stimulation.20
Nitric oxide donors
GLYCERYL TRINITRATE
Glyceryl trinitrate (GTN) and isosorbide dinitrate act as nitric oxide donors and probably aid healing through an increase in local blood flow secondary to a reduction in intra-anal pressure and perhaps also by vasodilatation of the vessels supplying the anal musculature. Early studies with GTN focused on optimal dose schedules, healing rates and side effects. These were validated by numerous trials. Whilst GTN was advocated as first-line treatment for chronic anal fissures with encouraging results, concerns about its effectiveness in clinical practice outside clinical trials emerged.21–23 There was also evidence that the duration of topical GTN was limited24 and that GTN was possibly ineffective altogether.25 Furthermore, data from randomised, controlled trials have shown that GTN is not superior to lateral sphincterotomy.26,27 It would seem that those fissures present for greater than 6 months and those with an associated sentinel pile are more likely to fail treatment.28 Alternative modes such as nitroglycerin patches have shown promise but have not been established as common practice.29
ISOSORBIDE DINITRATE
Isosorbide dinitrate (ISDN) is an alternative nitric oxide donor that has been used successfully in the treatment of anal fissures. The problems encountered are similar to those with GTN but long-term effectiveness has been questioned.30,31
Calcium antagonists
Nifedipine is a dihydropyridine calcium-channel blocker (less correctly referred to as a ‘calcium-antagonist’), which inhibits calcium ion entry through voltage-sensitive areas of vascular smooth muscle and myocardium. Topical and oral formulations of nifedipine have been evaluated but not used in routine clinical practice.32,33
Diltiazem, a non-dihydropyridine calcium-channel blocker, also effects vascular smooth muscle relaxation and dilatation. Topical 2% diltiazem reduces maximum resting pressure (MRP) by approximately 28% and this effect lasts 3–5 h after application.34 Early studies by Carapeti et al.35 and Knight et al.36 reported healing rates of chronic anal fissures of 67% and 73%, respectively. Side effects are minimal with diltiazem and include peri-anal dermatitis. Oral diltiazem has been assessed as part of a randomised trial and shown to heal anal fissures; however, significant side effects were noted.37 The topical formulation of diltiazem has been subjected to rigorous scrutiny and is a valid alternative to GTN with similar reductions in MRP, improved healing rates and lower rates of recurrence.38–41 There are also data to suggest that topical diltiazem heals GTN-resistant fissures.42
Muscarinic agonists and sympathetic neuromodulators
Carapeti et al.,35 using 1% bethanecol gel in 10 volunteers, showed a dose-dependent reduction in the maximum resting anal canal pressure. Its use in a small trial showed that after 8 weeks, in 9 of 15 (60%), the fissure had healed with no side effects. After an initial encouraging study with oral indoramin as an α1-adrenoceptor antagonist which reduced maximum resting anal canal pressure,43 Pitt et al.44 proceeded to conduct a double-blind, randomised, placebo-controlled trial of oral indoramin to treat 23 patients with chronic anal fissure. Nine subjects withdrew within the first 2 weeks of treatment due to side effects which included fatigue, dizziness, headache, dry mouth, nasal congestion and retrograde ejaculation. At 6 weeks, the fissure healed in only one (7%) compared with two (22%) in the placebo group.44 The trial was terminated.
Botulinum toxin
The precise anatomical position in which to inject botulinum toxin has been a matter of some debate as comparable healing rates are seen when injected into the internal or external sphincter (Tables 1 and 2). Jones et al.45 have shown that botulinum toxin reduces the internal sphincter tone through its effect on the sympathetic nervous system. Despite concerns with the injection, patients seemed to accept its use in the out-patient setting, though in the UK most users would advocate injection under general anaesthesia. To address this, investigators have treated chronic anal fissures with botulinum delivered in an out-patient setting through a high-pressure device.46 This mode of delivery needs further exploration.
Table 1.
Effect of injection of botulinum toxin type A injected into the external ana sphincter in patients with anal fissures
| Authors | Dose (Units) | Patients (n) | Review (weeks) | Healing rate (%) | Maximum reduction in resting pressure (%) | Maximum reduction in voluntary pressure (%) |
|---|---|---|---|---|---|---|
| Jost & Schimrigk (1993) | 2.5 | 1 | 12 | 100 | No data | No data |
| Jost & Schimrigk (1994) | 2.5 | 12 | 12 | 83 | No data | No data |
| Jost & Schimrigk (1995) | 5 | 26 | 12 | 81 | No data | No data |
| Jost (1997) | 2.5–5 | 100 | 12 | 82 | No data | No data |
| Jost & Schrank (1999)* | 20 | 50 | 12 | 76 (20 U) | No data | No data |
| 40 | 80 (40 U) | |||||
| Jost & Schrank (1999) | 5 | 20 | 12 | 70 (5 U) | No data | No data |
| 10 | 30 | 63 (10 U) | ||||
| Jost (2001) | 200 | 10 | 4 | 70 | No data | No data |
| Thompson et al. (2002)# | 50 | 26 | 12 (not complete) | 81 | No data | No data |
Dysport used for injection.
Botulinum toxin type B used for injection.
Table 2.
Effect of injection of botulinum toxin type A injected into the internal anal sphincter in patients with anal fissures
| Authors | Dose (Units) | Patients (n) | Review (weeks) | Healing rate (%) | Maximum reduction in resting pressure (%) | Maximum reduction in voluntary pressure (%) |
|---|---|---|---|---|---|---|
| Giu et al. (1994) | 15 | 10 | 8 | 70 | 25 | 21 |
| Mason et al. (1996) | 0.125–1 ng | 5 | 12 | 60 | 16 | No data |
| Espi et al. (1998) | 10–15 | 36 | 24 | 65 (10 U) | No data | No data |
| 81 (15 U) | ||||||
| Maria et al. (1998) | 20 | 15 | 4 & 8 | 53 (4 weeks) | 28 | 44 |
| 73 (8 weeks) | ||||||
| Maria et al. (1998) | 15–20 | 57 | 8 | 44 (15 U) | 29(15 U) | 17 (15 U) |
| 67 (20 U) | 28 (20 U) | 13 (20 U) | ||||
| Brisinda et al. (1999) | 20 | 25 | 8 | 96 | 29 | 6 |
| Minguez et al. (1999) | 10–21 | 69 | 24 | 83 (10 U) | 5(10 U) | 17 (10 U) |
| 78 (15 U) | 13 (15 U) | 17 (15 U) | ||||
| 90 (21 U) | 16(21 U) | 35 (15 U) | ||||
| Fernandez et al. (1999) | 80 | 76 | 12 | 67 | No data | No data |
| Maria et al. (2000) | 20 | 50 | 8 | 74 | 32 | 5 |
| Lysy et al. (2001) | 20 ± ISDN | 30 | 12 | 73 (ISDN) | 24 (ISDN) | 4.8 (ISDN) |
| 66 | 21 | 4.4 | ||||
| Madalinski et al. (2001) | 50 | 13 | No data | 54 | No data | No data |
| Gecim (2001) | 5 | 27 | 6 | 80 | No data | No data |
| Brisinda et al. (2002) | 20–50 | 150 | 8 | 89 (20 ± 30 U) | 30 (20 ± 30 U) | 0 (20 ± 30 U) |
| 96 (30 ± 50 U) | 34 (30 ± 50 U) | 8 (30 ± 50 U) | ||||
| Katory et al. (2002) | 50 | 20 | 6 | 80 | No data | No data |
As with diltiazem, botulinum toxin is effective in treating fissures that have failed to heal with topical agents. Botulinum toxin can also be combined with surgical modalities. Lindsey et al.47 showed that, following injection of 25 U of Botox into the internal sphincter combined with fissurectomy in 30 patients (19 of whom had failed both GTN and botulinum toxin injection), 28 (93%) had healed after a median of 16.4 weeks' follow-up. Dysport is an alternative tolerable commercial formulation of botulinum toxin to Botox; however, the change in dose needs attention as, in one study by Brisinda et al.,48 patients with fissures were randomised to receive 50 U of Botox formulation or 150 U of Dysport.
Conclusions
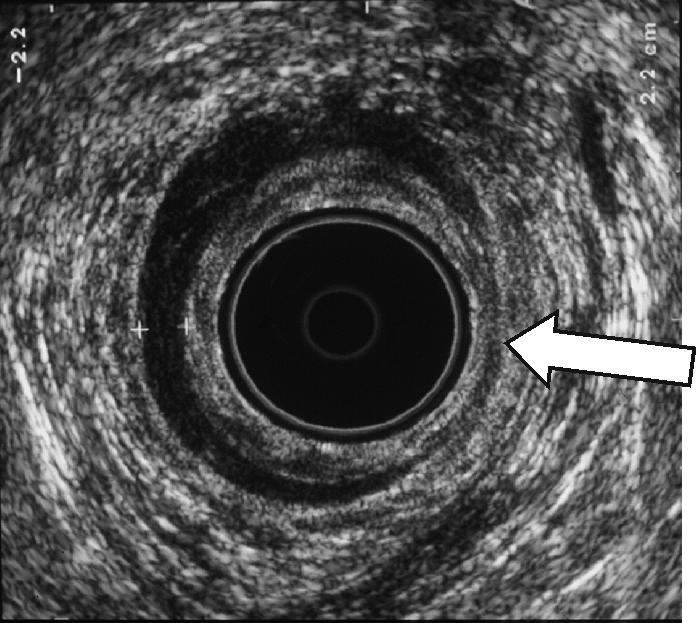
The first-line treatment of chronic anal fissures with topical agents has led to management algorithms that can be employed effectively.49 Lindsey et al.50 gave an excellent overview of the current treatment of chronic anal fissures and introduced the idea of poly-pharmacy with and without surgery. This synergy between topical, injectable and operative modalites requires continued appraisal. A practical algorithm that we think is evidence based and encompasses changing practice for the treatment of anal fissures is shown in Figure 3.
Figure 3.
Treatment algorithm for chronic anal fissures. If patients heal, a follow-up out-patient appointment should be considered.
Acknowledgments
The authors gratefully acknowledge the valuable assistance of Prof. PB Boulos in reviewing material included whilst in preparation for an MD thesis submitted from the Surgical Research Unit of the Royal Free and University College Hospital, London.
References
- 1.Sharp FR. Patient selection and treatment modalities for chronic anal fissure. Am J Surg. 1996;171:512–5. doi: 10.1016/S0002-9610(96)00017-7. [DOI] [PubMed] [Google Scholar]
- 2.Jensen SL. Treatment of first episodes of acute anal fissure: prospective randomised study of lignocaine ointment versus hydrocortisone ointment or warm sitz baths plus bran. BMJ. 1986;292:1167–9. doi: 10.1136/bmj.292.6529.1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jensen SL. Maintenance therapy with unprocessed bran in the prevention of acute anal fissure recurrence. J R Soc Med. 1987;80:296–8. doi: 10.1177/014107688708000513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McDonald P, Driscoll AM, Nicholls RJ. The anal dilator in the conservative management of acute anal fissures. Br J Surg. 1983;70:25–6. doi: 10.1002/bjs.1800700109. [DOI] [PubMed] [Google Scholar]
- 5.Shub HA, Salvati EP, Rubin RJ. Conservative treatment of anal fissure: an unselected, retrospective and continuous study. Dis Colon Rectum. 1978;21:582–3. doi: 10.1007/BF02586401. [DOI] [PubMed] [Google Scholar]
- 6.Watts JM, Bennett RC, Goligher JC. Stretching of anal sphincters in treatment of fissure-in-ano. BMJ. 1964;2:342–3. doi: 10.1136/bmj.2.5405.342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.MacDonald A, Smith A, McNeill AD, Finlay IG. Manual dilatation of the anus. Br J Surg. 1992;79:1381–2. doi: 10.1002/bjs.1800791248. [DOI] [PubMed] [Google Scholar]
- 8.Speakman CT, Burnett SJ, Kamm MA, Bartram CI. Sphincter injury after anal dilatation demonstrated by anal endosonography. Br J Surg. 1991;78:1429–30. doi: 10.1002/bjs.1800781206. [DOI] [PubMed] [Google Scholar]
- 9.Strugnell NA, Cooke SG, Lucarotti ME, Thomson WH. Controlled digital anal dilatation under total neuromuscular blockade for chronic anal fissure: a justifiable procedure. Br J Surg. 1999;86:651–5. doi: 10.1046/j.1365-2168.1999.01128.x. [DOI] [PubMed] [Google Scholar]
- 10.Lockhart-Mummery HE. Fissure-in-ano. In: Rob C, Smith R, editors. Operative Surgery. London: Butterworth; 1957. pp. 11–3. [Google Scholar]
- 11.Hawley PR. The treatment of chronic fissure-in-ano: a trial of methods. Br J Surg. 1969;56:915. doi: 10.1002/bjs.1800561212. [DOI] [PubMed] [Google Scholar]
- 12.Notaras MJ. Lateral subcutaneous sphincterotomy for anal fissure – a new technique. Proc R Soc Med. 1969;62:713. [PMC free article] [PubMed] [Google Scholar]
- 13.Boulos PB, Araujo JG. Adequate internal sphincterotomy for chronic anal fissure: subcutaneous or open technique? Br J Surg. 1984;71:360–2. doi: 10.1002/bjs.1800710517. [DOI] [PubMed] [Google Scholar]
- 14.Chowcat NL, Araujo JG, Boulos PB. Internal sphincterotomy for chronic anal fissure: long term effects on anal pressure. Br J Surg. 1986;73:915–6. doi: 10.1002/bjs.1800731123. [DOI] [PubMed] [Google Scholar]
- 15.Khubchandani IT, Reed JF. Sequelae of internal sphincterotomy for chronic fissure in ano. Br J Surg. 1989;76:431–4. doi: 10.1002/bjs.1800760504. [DOI] [PubMed] [Google Scholar]
- 16.Littlejohn DR, Newstead GL. Tailored lateral sphincterotomy for anal fissure. Dis Colon Rectum. 1997;40:1439–42. doi: 10.1007/BF02070709. [DOI] [PubMed] [Google Scholar]
- 17.Engel AF, Eijsbouts QA, Balk AG. Fissurectomy and isosorbide dinitrate for chronic fissure in ano not responding to conservative treatment. Br J Surg. 2002;89:79–83. doi: 10.1046/j.0007-1323.2001.01958.x. [DOI] [PubMed] [Google Scholar]
- 18.Leong AF, Seow-Choen F. Lateral sphincterotomy compared with anal advancement flap for chronic anal fissure. Dis Colon Rectum. 1995;38:69–71. doi: 10.1007/BF02053862. [DOI] [PubMed] [Google Scholar]
- 19.Farouk R, Monson JR, Duthie GS. Technical failure of lateral sphincterotomy for the treatment of chronic anal fissure: a study using endoanal ultrasonography. Br J Surg. 1997;84:84–5. [PubMed] [Google Scholar]
- 20.Cook TA, Brading AF, Mortensen NJ. The pharmacology of the internal anal sphincter and new treatments of ano-rectal disorders. Aliment Pharmacol Ther. 2001;15:887–98. doi: 10.1046/j.1365-2036.2001.00995.x. [DOI] [PubMed] [Google Scholar]
- 21.Pitt J, Dawas K, Dawson PM. Disappointing results of glyceryl trinitrate ointment in the treatment of chronic fissure-in-ano in a district general hospital. Colorect Dis. 1999;1:204–6. doi: 10.1046/j.1463-1318.1999.00042.x. [DOI] [PubMed] [Google Scholar]
- 22.Dorfman G, Levitt M, Platell C. Treatment of chronic anal fissure with topical glyceryl trinitrate. Dis Colon Rectum. 1999;42:1007–10. doi: 10.1007/BF02236692. [DOI] [PubMed] [Google Scholar]
- 23.Jonas M, Lobo DN, Gudgeon AM. Lateral internal sphincterotomy is not redundant in the era of glyceryl trinitrate therapy for chronic anal fissure. J R Soc Med. 1999;92:186–8. doi: 10.1177/014107689909200406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jonas M, Amin S, Wright JW, Neal KR, Scholefield JH. Topical 0.2 percent glyceryl trinitrate ointment has a short-lived effect on resting anal pressure. Dis Colon Rectum. 2001;44:1640–3. doi: 10.1007/BF02234384. [DOI] [PubMed] [Google Scholar]
- 25.Thornton MJ, Kennedy ML, King DW. Prospective manometric assessment of botulinum toxin and its correlation with healing of chronic anal fissure. Dis Colon Rectum. 2005;48:1424–31. doi: 10.1007/s10350-005-0025-9. [DOI] [PubMed] [Google Scholar]
- 26.Richard CS, Gregoire R, Plewes EA, Silverman R, Burul C, Buie D, et al. Internal sphincterotomy is superior to topical nitroglycerin in the treatment of chronic anal fissure: results of a randomized, controlled trial by the Canadian Colorectal Surgical Trials Group. Dis Colon Rectum. 2000;43:1048–57. doi: 10.1007/BF02236548. [DOI] [PubMed] [Google Scholar]
- 27.Libertiny G, Knight JS, Farouk R. Randomised trial of topical 0.2% glyceryl trinitrate and lateral internal sphincterotomy for the treatment of patients with chronic anal fissure: long term follow-up. Eur J Surg. 2002;168:41–2. doi: 10.1080/110241502320789113. [DOI] [PubMed] [Google Scholar]
- 28.Pitt J, Williams S, Dawson PM. Reasons for failure of glyceryl trinitrate treatment of chronic fissure-in-ano: a multivariate analysis. Dis Colon Rectum. 2001;44:846–7. doi: 10.1007/BF02234710. [DOI] [PubMed] [Google Scholar]
- 29.Zuberi BF, Rajput MR, Abro H, Shaikh SA. A randomized trial of glyceryl trinitrate ointment and nitroglycerin patch in healing of anal fissures. Int J Colorectal Dis. 2000;15:246–7. doi: 10.1007/s003840000230. [DOI] [PubMed] [Google Scholar]
- 30.Lysy J, Israelit-Yatzkan Y, Sestiere-Ittah M, Keret D, Goldin E. Treatment of chronic anal fissure with isosorbide dinitrate: long-term results and dose determination. Dis Colon Rectum. 1998;41:1406–10. doi: 10.1007/BF02237057. [DOI] [PubMed] [Google Scholar]
- 31.Werre AJ, Palamba HW, Bilgen EJ, Eggink WF. Isosorbide dinitrate in the treatment of anal fissure: a randomised, prospective, double blind, placebo-controlled trial. Eur J Surg. 2001;167:382–5. doi: 10.1080/110241501750215294. [DOI] [PubMed] [Google Scholar]
- 32.Antropoli C, Perrotti P, Rubino M, Martino A, De Stefano G, Migliore G, et al. Nifedipine for local use in conservative treatment of anal fissures: preliminary results of a multicenter study. Dis Colon Rectum. 1999;42:1011–5. doi: 10.1007/BF02236693. [DOI] [PubMed] [Google Scholar]
- 33.Cook TA, Humphreys MM, Mortensen NJ. Oral nifedipine reduces resting anal pressure and heals chronic anal fissure. Br J Surg. 1999;86:1269–73. doi: 10.1046/j.1365-2168.1999.01292.x. [DOI] [PubMed] [Google Scholar]
- 34.Carapeti EA, Kamm MA, Evans DE, Phillips RKS. Diltiazem lowers resting anal sphincter pressure – a potential low side-effect alternative to glyceryl trinitrate for fissures. Gastroenterology. 1998;114:A7. [Google Scholar]
- 35.Carapeti EA, Kamm MA, Phillips RK. Topical diltiazem and bethanecol decrease anal sphincter pressure and heal anal fissures without side effects. Dis Colon Rectum. 2000;43:1359–62. doi: 10.1007/BF02236630. [DOI] [PubMed] [Google Scholar]
- 36.Knight JS, Birks M, Farouk R. Topical diltiazem ointment in the treatment of chronic anal fissure. Br J Surg. 2001;88:553–6. doi: 10.1046/j.1365-2168.2001.01736.x. [DOI] [PubMed] [Google Scholar]
- 37.Jonas M, Neal KR, Abercrombie JF, Scholefield JH. A randomized trial of oral vs. topical diltiazem for chronic anal fissures. Dis Colon Rectum. 2001;44:1074–8. doi: 10.1007/BF02234624. [DOI] [PubMed] [Google Scholar]
- 38.Kocher HM, Steward M, Leather AJ, Cullen PT. Randomized clinical trial assessing the side-effects of glyceryl trinitrate and diltiazem hydrochloride in the treatment of chronic anal fissure. Br J Surg. 2002;89:413–7. doi: 10.1046/j.0007-1323.2001.02042.x. [DOI] [PubMed] [Google Scholar]
- 39.DasGupta R, Franklin I, Pitt J, Dawson PM. Successful treatment of chronic anal fissure with diltiazem gel. Colorect Dis. 2002;4:20–2. doi: 10.1046/j.1463-1318.2002.00294.x. [DOI] [PubMed] [Google Scholar]
- 40.Griffin N, Acheson AG, Jonas M, Scholefield JH. Long-term follow up of trial patients treated with diltiazem for anal fissure. Colorect Dis. 2002;2002(Suppl 1):20. [Google Scholar]
- 41.Bielecki K, Kolodziejczak M. A prospective randomized trial of diltiazem and glyceryltrinitrate ointment in the treatment of chronic anal fissure. Colorect Dis. 2003;5:256–7. doi: 10.1046/j.1463-1318.2003.00440.x. [DOI] [PubMed] [Google Scholar]
- 42.Jonas M, Speake W, Scholefield JH. Diltiazem heals glyceryl trinitrate-resistant chronic anal fissures: a prospective study. Dis Colon Rectum. 2002;45:1091–5. doi: 10.1007/s10350-004-6365-z. [DOI] [PubMed] [Google Scholar]
- 43.Pitt J, Craggs MM, Henry MM, Boulos PB. Alpha-1 adrenoceptor blockade: potential new treatment for anal fissures. Dis Colon Rectum. 2000;43:800–3. doi: 10.1007/BF02238017. [DOI] [PubMed] [Google Scholar]
- 44.Pitt J, Dawson PM, Hallan Rl, Boulos PB. A double-blind randomized placebo-controlled trial of oral indoramin to treat chronic anal fissure. Colorect Dis. 2001;3:165–8. doi: 10.1046/j.1463-1318.2001.00227.x. [DOI] [PubMed] [Google Scholar]
- 45.Jones OM, Brading AF, Mortensen NJ. The mechanism of action of botulinum toxin on the internal anal sphincter. Colorect Dis. 2002;2002(Suppl 1):71–2. doi: 10.1002/bjs.4394. [DOI] [PubMed] [Google Scholar]
- 46.Bhardwaj R, Drye E, Vaizey C. Novel delivery of botulinum toxin for the treatment of anal fissures. Colorect Dis. 2006;8:360–4. doi: 10.1111/j.1463-1318.2005.00920.x. [DOI] [PubMed] [Google Scholar]
- 47.Lindsey I, Cunningham C, Jones OM, Francis C, Mortensen NJ. Fissurectomy-botulinum toxin: a novel sphincter-sparing procedure for medically resistant chronic anal fissure. Dis Colon Rectum. 2004;47:1947–52. doi: 10.1007/s10350-004-0693-x. [DOI] [PubMed] [Google Scholar]
- 48.Brisinda G, Albanese A, Cadeddu F, Bentivoglio AR, Mabisombi A, Marniga G, et al. Botulinum neurotoxin to treat chronic anal fissure: results of a randomized ‘Botox vs. Dysport’ controlled trial. Aliment Pharmacol Ther. 2004;19:695–701. doi: 10.1111/j.1365-2036.2004.01895.x. [DOI] [PubMed] [Google Scholar]
- 49.Porrett TRC, Knowles CH, Lunniss PJ. Anal fissures in a district general hospital: creation of a treatment algorithm for nurse-led management. Colorect Dis. 2002;2002(Suppl 1):72. doi: 10.1046/j.1463-1318.2003.00406.x. [DOI] [PubMed] [Google Scholar]
- 50.Lindsey I, Jones OM, Cunningham C, Mortensen NJ. Chronic anal fissure. Br J Surg. 2004;91:270–9. doi: 10.1002/bjs.4531. [DOI] [PubMed] [Google Scholar]