Abstract
A novel case of squamous cell carcinoma of scrotum that developed in a well-healed, uncomplicated scar following an infertility procedure.
Keywords: Genital tumour, Scrotal cancer, Squamous cell carcinoma
Squamous cell carcinoma of scrotum has been a topic of special interest for clinical and historical reasons as it was the first cancer directly associated with a specific occupation.1 Since its classical description in chimney sweeps by Pott in 1775, it has been referred to frequently as Pott's cancer or chimney sweep cancer. Scrotal squamous cell carcinoma is a rare tumour; due to improved working conditions, occupation-related scrotal cancers have become even less frequent.2,3 Although two cases of squamous cell carcinoma of scrotum have been reported to develop in a Fournier gangrene scar,4,5 its development in a well-healed, uncomplicated scar following an infertility procedure has not been previously reported.
Case report
A 63-year-old retired, healthy Indian male presented with a painless, hard, midline swelling close to the penoscrotal junction, where he had a scar from previous treatment for infertility. He had had testicular biopsy and right-sided vaso-epididymal anastomosis for obstructed vas deferens 30 years previously. Postoperative vasogram showed patent vas and he made an uneventful recovery. He never had any particular problem related to the scrotal scar thereafter, until he noticed this swelling. He did have some evidence of tinea cruris involving scrotal region that was treated with topical Clotrimazole cream and also, long-standing bilateral varicose eczema affecting his legs.
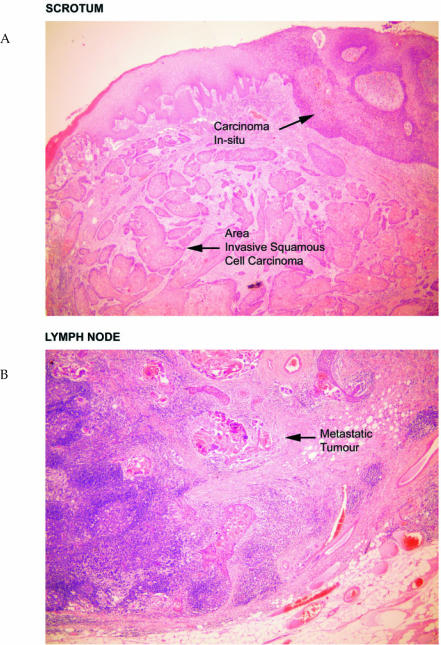
On examination, he had a 4-cm painless, firm lump over the penoscrotal junction where he had scar from previous operation. There was no palpable inguinal lymphadenopathy. Staging CT did not show any lymphatic or distant metastasis. He underwent a wide local excision of scrotal lump under general anaesthesia. Subsequent histology showed a moderately differentiated invasive squamous cell carcinoma stage pT1 (Fig. 1A). Excision appeared to be complete with no lymphovascular invasion. Subsequently, follow-up CT scan of his abdomen and pelvis at 6 months showed a small volume, but significant, bilateral inguinal lymphadenopathy (right > left), liver was normal, and there was no feature of distant metastasis.
Figure 1.
(A) Histopathology of scrotal excision biopsy specimen showing area of squamous cell carcinoma and carcinoma in situ.
(B) Histopathology from inguinal lymph node showing metastatic tumour.
He underwent fine needle aspiration of inguinal lymph nodes under ultrasound guidance. As FNAC was negative for malignant cells, he was followed up with another repeat scan 6 months later that showed the inguinal lymphadenopathy to be persistent and increasing. He underwent bilateral bloc dissection of inguinal lymph nodes followed by adjuvant radiotherapy and made an uneventful recovery from both treatment modalities. Histology from the bilateral bloc dissection showed the presence of metastasis in one out of six nodes on the left side (Fig. 1B) only but no metastasis detected on the right side. Postoperatively, he developed scrotal oedema that settled gradually with conservative management. After 42 months of follow-up with regular annual CT scans of abdomen and pelvis, he remains recurrence free.
Discussion
The earliest description of scrotal cancer dates back to 1731 by Bassius and 1740 by Treyling, but it was Sir Percival Pott in 1975, who stated:3 ‘there is a disease peculiar to a certain set of people that has not, at least to my knowledge, been publicly noticed: ….chimney sweep cancer…. They are most frequently treated with great brutality and almost starved from cold and hunger; are thrust up narrow and sometimes hot chimneys where they are sometimes bruised and burned and sometimes they get suffocated and when they get to puberty, are peculiarly prone to noisome, painful and fatal disease.’ Further investigators have shown this cancer to be related to exposure of certain carcinogens in specific occupations such as tar workers, petroleum wax pressmen, paraffin and shale oil workers, cotton mule operators and the screw making industry.2 The incidence of occupation-related scrotal cancer is falling because of better hygiene, protective clothing and awareness of the carcinogenicity of industrial oils.3 Several new risk factors were identified based on an American series including exposure to coal tar and arsenic-based treatments for psoriasis, multiple epitheliomas and history of human papilloma virus.2 Also, it may occur as a result of non-specific factors such as poor hygiene and chronic irritation,6–8 which may partially be explained by the similarity in the mechanism of formation of scar by fibrosis and tumourigenesis.5
Development of squamous cell carcinoma has been well described in chronic burn scars (Marjolin's ulcer) and there are reported cases of scrotal cancers developing in areas previously affected by Fournier's gangrene.4,5 However, scrotal squamous cell cancer developing in a well-healed scar following a minor infertility procedure has never been reported. The development of scrotal cancer in this case could probably be explained by the added effect of chronic irritation secondary to fungal infection and poor hygiene.
The well-accepted treatment for primary lesion is wide local excision although there had been issues relating to the extent of regional dissection – inguinal or ilioinguinal? Our patient underwent superficial inguinal bloc dissection followed by external beam radiotherapy to the pelvis and has been recurrence free for the last 30 months.
Most authors recommend ilio-inguinal bloc dissection in biopsy-proven inguinal lymph nodes but this conclusion should be tempered by the limited nature of the experience and insufficient data in these series. Despite initial disagreement about the role of radiotherapy in treatment of squamous cell carcinoma of scrotum, use of adjuvant radiotherapy and combination chemotherapy with Bleomycin, methotrexate and cisplatinum has been recommended.9
Conclusions
This case is reported to highlight the development of aetiological diversity to a very rare form of cancer. Scrotal squamous cell carcinomas may well develop in well-healed scars unlike Marjolin's ulcer that are usually associated with chronic, non-healing scars.
References
- 1.Melicow MM. Percival Pott (1713–1788): 200th anniversary of first report of occupation-induced cancer of scrotum in chimney sweepers (1775) Urology. 1975;6:745. doi: 10.1016/0090-4295(75)90812-2. [DOI] [PubMed] [Google Scholar]
- 2.Andrews PE, Farrow GM, Oesterling JE. Squamous cell carcinoma of the scrotum: long-term follow up of 14 patients. J Urol. 1991;146:1299–304. doi: 10.1016/s0022-5347(17)38073-4. [DOI] [PubMed] [Google Scholar]
- 3.Lowe FC. Squamous cell carcinoma of the scrotum. J Urol. 1983;130:423–7. doi: 10.1016/s0022-5347(17)51233-1. [DOI] [PubMed] [Google Scholar]
- 4.Schneider PR, Russell RC, Zoo EG. Fournier gangrene of the penis: a report of two cases. Ann Plast Surg. 1986;17:87–90. doi: 10.1097/00000637-198607000-00016. [DOI] [PubMed] [Google Scholar]
- 5.Chintamani, Shankar M, Singhal V, Singh JP, Bansal A, Saxena S. Squamous cell carcinoma developing in the scar of Fournier gangrene – case report. BMC Cancer. 2004;4:16. doi: 10.1186/1471-2407-4-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gerber C, von Hochstetter AR, Schuler G, Hofmann V, Rosenthal C. Penis carcinoma in a young chimney sweep. Case report 200 years following the description of the first occupational disease. Schweiz Med Wochenschr. 1995;125:1201–5. [PubMed] [Google Scholar]
- 7.Futter NG. Scrotal cancer: deja vu. Can J Urol. 1998;5:558–9. [PubMed] [Google Scholar]
- 8.Polyak L, Czvalinga I, Frang D. Primary carcinomas of the scrotum – 5 cases. Z Urol Nephrol. 1987;80:455–8. [PubMed] [Google Scholar]
- 9.Stern RS. Genital tumors among men with psoriasis exposed to psoralens and ultraviolet A radiation (PUVA) and ultraviolet B radiation. N Engl J Med. 1990;322:1093–7. doi: 10.1056/NEJM199004193221601. [DOI] [PubMed] [Google Scholar]