Abstract
Biomedical interventions promise achievement of health-related Millennium Development Goals provided social-, capacity- and knowledge-based constraints to scaling up and reaching marginalized people at risk, are addressed, and balance between prevention and treatment is struck. We argue for a new approach: multi-stakeholder capacity building and learning for empowerment: MuSCLE. MuSCLE is used as a way to frame three systemic weaknesses in traditional health science and policy approaches: 1) a lack of engagement with people at risk to build a collective understanding of the contexts of health problems; 2) a lack of multi-criteria evaluation of alternative interventions; and 3) a lack of attention paid to integrated capacity building. The MuSCLE framework responds in three ways: 1) Participatory assessment of the ecological, socio-cultural, economic and political contexts of health, identifying priorities using risk and vulnerability science, and modeling drivers; 2) Selection among intervention alternatives that makes ecological, socio-cultural, economic and political tradeoffs transparent; and 3) Integrated capacity building for sustainable and adaptive interventions. Literature and field lessons support the argument, and guidelines are set down. A MuSCLE approach argues for a transformation in health science and policy in order to achieve Millennium Development Goals for health.
Keywords: poverty, risk, vulnerability, capacity building
1.0 INTRODUCTION
In 2000, the Millennium Declaration set out ambitious targets - Millennium Development Goals (MDGs) - for substantial reductions in poverty and hunger, child mortality, and disease as well as significant improvements in maternal health, gender equality, primary education, and environmental sustainability. In 2005, in the five-year progress report, the UN concluded that business-as-usual approaches will not get us there: “if current trends persist there is a risk that many of the poorest countries will not be able to meet many of [the MDGs]” [1]. Investment of political and intellectual capital and planned mobilizing of financial capital have never been stronger. By 2015, all 191 Member States of the United Nations have pledged to meet the MDGs [2].
The UN Millennium Project (MP) is an independent advisory board commissioned by the Secretary General to advise on strategies to achieve the MDGs [3]. The MP views country-level changes as key to achieving the goals: improvements in governance; engaging and empowering civil society; promoting entrepreneurship; mobilizing domestic resources; increasing aid; and reforming global trade policies that favor rich nations [3]. Their report calls for a “bold, needs-based, goal-oriented investment framework over 10 years” [3, p. 24], and recommends that “countries” (i.e. central governments) follow four-steps: i) map dimensions and underlying determinants of extreme poverty; ii) use poverty maps to undertake needs assessment for public investment; iii) convert the assessment into a 10-year action plan; and iv) include a 3–5 year “quick win” poverty reduction strategy within the plan. For rapid scale-up of interventions to a national scale the MP further states governments must: a) set out objectives and work plans with clear deliverables and timelines; b) build national and local capacity for management, human resources and infrastructure; c) adopt replicable, locally appropriate delivery mechanisms for interventions; and d) monitor progress and allow mid-course correction. The MP recognizes that involvement and ownership by communities, and long-term donor funding and technical assistance are conditions for success. It strategically targets countries with governance that is weak because of weak capacity, not because of corruption or a lack of will.
The MP Task Force Reports for the health-related MDGs have laid out a comprehensive set of recommendations and priority actions. However, the recommendations tend to be prescriptive and descriptive, rather than being operational and empowering. An inclusive, transparent and evidence-based process for turning the the MP recommendations into actions is still needed. This paper focuses on how to achieve the MDGs for health on the ground in partnership with multiple stakeholders. We argue for a transformative multi-stakeholder process that fosters social learning and strengthens social capital with three main features:
Participatory, systems-based assessment of the ecological, socio-cultural, economic and political contexts of health challenges and responses, identifying priorities using risk and vulnerability science, and modeling drivers;
Selection among intervention alternatives that makes ecological, socio-cultural, economic and political tradeoffs transparent; and
A support system of capacity building to sustain selected interventions, and adapt to changing conditions and priorities over time.
The objective of the paper is to make the case for a “MuSCLE”-type process - multi-stakeholder capacity building and learning for empowerment – by exploring its theoretical and practical foundations, drawing from literature traditionally outside the scope of biomedical and public health fields, and supported by lessons from the field.
2.0 SOCIAL LEARNING FRAMEWORK
The organizing framework for MuSCLE is a multi-stakeholder process that fosters social learning and strengthens social capital. Social learning has been defined as “a framework for thinking about knowledge processes that underlie social adaptation and innovation” [4, p.64]. Much useful knowledge of social learning has come from natural resource management experience in developing countries, but has yet to be applied to health. Guangxia and Lianmin [5] found that effective social learning for forest management in Chinese study sites occurred as a result of a productive cycle of conflict and consensus. Strong cultural values allowed villagers to share the goal of forest conservation, and stakeholder interaction was mediated by respected elders. Success resulted from social learning, effective leadership and effective communication. Effective leaders – innovators – are able to exploit culturally accepted networks to stimulate collective action for change, and also accommodate special interests of some stakeholders. Biomedical professionals are often skeptical of community-based health approaches, but this stems from a perception that any such methods will exclude biomedical science and knowledge of proven intervention technologies. We advocate health scientists, practitioners, policy makers and communities-at-risk work together as a knowledge collaborative.
Buck et al. [6] signal four aspects of effective social learning for forest management, equally relevant to health: i) conflict mitigation based on understanding power relations; ii) an innovation and problem solving climate; iii) communication and relationship building; and iv) capacity building and organizational development. Daniels and Walker [7] claim mutual learning derived from the interaction of differing values, capacities, perspectives, methods and historical experiences can transform collective understanding. Potential barriers include insufficient trust and transparency among participants, and resistance from power and knowledge elites – including some donors and “experts” - who are invested in the status quo.
2.1 Communication for Social Change
A growing number of development communication specialists are calling for an approach which stimulates debate and dialogue. Recognizing the limits of traditional communication in development which is more focused on changing individual behaviors, the emerging communication for social change approach champions public and private dialogue through which people define who they are, what they want and how they can achieve it. The approach aims to change emphasis: a) away from people as the objects for change and toward communities as agents of their own change; b) away from designing, testing and delivering messages and toward fostering dialogue and debate; c) away from a focus on individual behaviors and toward better understanding of social norms, policies, culture and the need for an enabling environment; d) away from persuading people to do something and toward negotiating the best way forward in a partnership; e) away from technical experts in “outside” agencies dominating a process and toward the people most affected by the problem playing a central role [8]. The experience of the global polio eradication initiative, paralyzed by a boycott against vaccination by a poor, politically marginalized group in Northern Nigeria, is a compelling example of the need to take in account the broader socio-cultural and political contexts of health initiatives and actively engage those most affected early in the planning. (Box 1).
BOX 1. Embattled polio vaccination shows perils of ignoring socio-political and cultural factors
In 2000, in the midst of the global polio eradication initiative, Nigeria had reduced the total number of cases of polio to 28. In mid-2003, following persuasion by religious leaders questioning the safety of the vaccine, the governor of Kano State in Northern Nigeria declared a boycott on polio vaccination across the state. The boycott lasted eleven months, while numbers of polio cases escalated to nearly 800 in Nigeria and polio cases - traced to Nigeria - emerged in fifteen countries which had not seen a case of polio for over a year, some for over four years. Although the boycott ended in mid-2004, the cost of the refusal to vaccinate continued into 2005, when two more countries saw outbreaks, after not having seen polio in over six years.* The polio virus had jumped continents from Africa to Asia because of the refusal to vaccinate by one of the poorest, disenfranchised communities in the world. The polio eradication program was perceived as externally imposed both by a central government and the “West” which, according to local Muslim religious leaders, was intent on sterilizing Muslim populations through the polio vaccine. There was also a general frustration among communities that they were not receiving health services they perceived as being high priority. Similar vaccination refusals had emerged in Northern India, for some of the same reasons. The strategy that successfully turned the resistance around in India included building alliances with local Muslim medical colleges and trusted local leaders. In Nigeria, the boycott ended due to a combination of a locally led investigation of the safety of the vaccine, a change in the vaccine source to dominantly Muslim Indonesia, local and global political pressures due to the growing polio outbreak in and outside of Nigeria, increased involved of local community members in the vaccination campaigns(vaccinators from the local area rather than from other parts of the country), and building alliances with trusted religious leaders in and outside of Nigeria, e.g. AlAzhar University in Cairo).
* (data table) www.polioeradication.org
Beyond the polio case, current global health challenges expose the serious limitations of traditional bio-medical approaches to both explaining health disparities and responding adequately to them. More evident than ever, the fields of biomedicine and public health must join forces with each other, and with key disciplinary allies – anthropology, environmental science, management science to name but a few - to encompass socio-cultural, political, economic, and ecological risk factors [9, 10, 11, 12 among many]. Arguably, HIV/AIDS research has learned the most about the need to work with people at risk, and has also advanced the science of vulnerability assessment considerably [13, 14, 15, 16, 17, 18 among many]. Lessons from the field of HIV/AIDS also provide empirical evidence that supports a MuSCLE-type approach (Box 2).
BOX 2: Confronting HIV/AIDS collaboratively makes inroads
The response to HIV/AIDS has been a pathfinder in multi-stakeholder, trans-disciplinary approaches and vulnerability science. HIV/AIDS was the first health issue to be “owned” widely outside of the health sector and the first disease-specific issue to be tabled at the UN Security Council. While sectors outside of health have long recognized the importance of addressing AIDS, the challenge was in negotiating and understanding so many different partners’ roles in the response. When asked why communities in the South Pacific were so able to quickly mobilize themselves to organize funerals and all the rituals which surround them, even getting the word out to relatives living on remote islands, while health programs rarely saw such mobilization efforts, the response was “Everyone knows their role. Everyone knows exactly what they need to do for a funeral.” [19].
Insights such as “everyone knows what they need to do” have been important cues to guide the response to HIV/AIDS. Other lessons learned from HIV/AIDS, include the importance of sensitive issues being communicated by trusted community members, not technical “specialists” from a far-away place. In Argentina, having drug users design AIDS prevention messages was “valuable for their own recuperative process, as well as being effective for identifying appropriate language or jargon.” [20] In Rwanda, similar experience meant that prevention programs engaged “people who live in the same area, share the same ways of life, speak the same language and even have the same jokes and idioms” in order to ensure that important AIDS prevention information was more easily understood [21].
2.2 Participatory Methods
While people’s participation in policy and development decisions that impact them is a widely accepted, human rights-based principle, effective participation is often unrealized. Community-based water management experience in developing countries provides one sound literature footing [22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33]. Methods used for over 20 years by development practitioners include participatory rural appraisal (PRA), applied in Africa and Asia since the 1980s, and participatory action research (PAR), applied from 1994–1998 by IRC and partners in Nepal, Pakistan, Kenya, Cameroon, Guatemala and Colombia [22]. An increasing number of environment-development scholar-practitioners recognize the need for a new conceptual and operational framework for poverty eradication and health promotion: a “bottom-up meets top-down” approach that brings governments and communities together to better understand then solve problems. As Martin Luther King declared: “No great victories are won in a war for the transformation of a whole people without total participation” [34].
Participation by those at risk in health research projects has tended to be limited to the provision of solicited information about exposure to risk and health effects [35, 36, 37, 38, 39, 40, 41, 42]. However, the tide is turning towards more collaborative methods; a special issue of the U.S. National Institute of Environmental Health Science (NIEHS) journal Environmental Health Perspectives dedicated to the future of environmental health research featured three articles on active collaborations between scientists and communities at risk that resonate with elements of our proposed process [43, 44, 45]. NIEHS has funded an ongoing project (Downs is co-PI) that tests MuSCLE on the ground (Box 3). This is a reflection of growing awareness of the need to encompass socio-cultural, political, economic, and ecological vulnerability factors in explaining and addressing health disparities [9, 10, 12 among many].
BOX 3: MuSCLE approach gains traction in old urban industrial city
We are gaining practical experience of a MuSCLE approach in inner city, marginalized communities of Worcester, Massachusetts, once heartland of the Industrial Revolution in the USA, now blighted by high pollution burdens and socio-economic pressures. Action research funded by the National Institute of Environmental Health Science’s “Environmental Justice: Partnerships for Communication” Program is being undertaken during 2004–2008 by a collaborative comprising five main stakeholders: Clark University; Family Health Center (primary care facility with 30 years experience); Regional Environmental Council (environmental health outreach NGO with 20 years experience); and the Worcester Youth Center (community based organization providing youth development services to at-risk youth); and representatives of the target population - vulnerable residents. Target neighborhoods are Main South and Piedmont which represent conditions of high risk and vulnerability because of ecological, socio-political, economic and cultural vulnerability factors. Priority stressors include: a) chronic pollution (e.g. lead in household paint, dust and soil, mold, particulate matter indoors and outdoors); b) lack of green-space for recreation; c) abundance of brownfields (vacant lots and abandoned factories suspected to be, or known to be contaminated); d) pervasive trash, sidewalk and street disrepair; and e) a climate of insecurity, drug abuse and crime. The population is of highly ethnic diversity (25% immigrant or refugee, with over 40% Latino). Over 40% live below the poverty line, many in old rented, delapidated housing.
Working groups of stakeholders have become task forces mobilized to tackle specific priority issues: health impacts, health services, pollution, and trash,. Their action planning and capacity building is informed by mixed-methods, trans-disciplinary research with three aspects: i) household surveys of health problems, vulnerabilities and existing capacities to cope; ii) focus groups and listening sessions to discuss issues, resources and needs openly and informally; and iii) environmental sampling. Teenagers from the Youth Center are trained as part of the research team, and are involved in action planning that targets asthma, greenspace and youth activity initiatives.
2.3 Proposed Learning Cycle
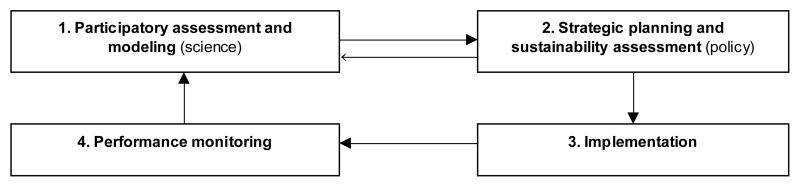
Multi-stakeholder engagement with all four stages of an adaptive learning cycle (Figure 1) - assessment and modeling, planning, implementation, and monitoring – is central to attaining the MDGs through a MuSCLE-type approach. The main stakeholders encompass: communities at risk (including women, children and minorities); local, district and state government agencies; non-governmental health organizations; the private sector; donors; and academics. The cycle reflects Holling’s [46] ecological concept of complex systems ‘backlooping’ to remain adaptive to ever-changing conditions. In practice the stages of the learning cycle are quasi-sequential, to allow known urgent problems to receive quick attention, and sustain buy-in from stakeholders.
Figure 1. Multi-stakeholder learning cycle at the core of MuSCLE.
We place stakeholders into a dynamic experiential learning cycle that includes all four stages of a typical project: assessment, planning, implementation and monitoring. Note the two-way interchange between assessment and planning, and how monitoring re-informs our understanding. Thus, learning is adaptive to changing conditions and priorities over time. In practice, stages of the learning cycle overlap. Priority problems are addressed first and as tangible benefits become visible, stakeholder buy-in is accrued and sustained.
Social learning and social capital building lie at the core of health and development progress. Three of the ten core recommendations of the Millennium Project [3, p.1–3] acknowledge this. One states “developing country governments should craft and implement the MDG-based poverty reduction strategies in transparent and inclusive processes, working closely with civil society organizations, the domestic private sector, and international partners”. The second recommends that “civil society organizations should contribute actively to designing policies, delivering services, and monitoring progress”. A third calls for launching a “massive effort to build expertise at the community level….expertise in health, education, agriculture, nutrition, infrastructure, water supply and sanitation, and environmental management… and training to promote gender equality and participation”. The reality remains that meaningful stakeholder participation remains largely ad-hoc. Although participation in local development projects is commonplace, participation by those most affected in higher decision-making forums such as public health policy-making is rare.
3.0 SYSTEMS UNDERSTANDING
3.1 Health as a Dynamic System
Health is part of a much larger human-environment dynamic system, disease a biological signal of stress. Therefore a participatory, trans-epistemological approach to assessment is crucial, taking stock of the socio-cultural, political, economic, and ecological contexts of health, and integrating different types of knowledge, including anecdotal and indigenous types. With this fuller contextual analysis, risks and vulnerabilities can be used to identify and anticipate priority problems. A systems-based perspective also allows us to model what is driving the risks and vulnerabilities in a given context, and act strategically to control drivers and prevent disease.
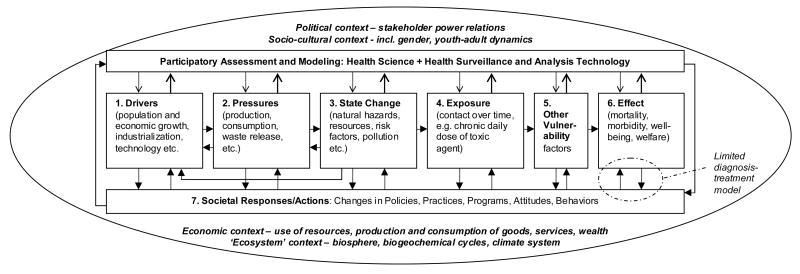
A strong argument can be made that only by employing such inclusive approaches can we build an adequate, sustainable response to health needs. Expanding the World Health Organization [47, p.5] Pressure -> State -> Impact -> Response (PSIR) model into seven levels to include: drivers, pressures, state changes, exposures (contact over time with risk agents), vulnerabilities (amplifiers or attenuators of risk), effects (disease expression) and societal responses (interventions and policies) will be instrumental for sustainable health gains (Figure 2). There are interdependencies among levels, and feedbacks, making the model non-linear.
Figure 2. Societal-ecological health system levels.
A health system is socially and ecologically dynamic and fuller understanding of these dynamics allows for a more comprehensive, multi-level and sustainable health response. Some drivers (e.g. clean technologies) lead to positive health outcomes while others (e.g. polluting technologies) lead to negative ones. Traditional biomedical approaches tend to focus only on health effects (level 6) and specific treatments (e.g. vaccines, drugs). Interactions are shown among levels 1, 2 and 3, and between responses and each level, so the system is non-linear with multiple feedbacks. Participatory assessment and modeling is shown as an enabling part of the societal response. Four types of context are also shown.
We must also place the health model in its political, socio-cultural, economic and ecological contexts: a ‘model within models’. For example, a model of the political context explains how power is distributed within the society, how health and development policy decisions are made, and the relationships among stakeholders, and is fundamental to effective intervention. A socio-cultural perspective is needed that describes gender dynamics, youth-adult relations, tribal and ethnic dynamics. A model of the economic system tends to reflect power relations and help explain them, and places health in the context of the stock and flows of wealth, different types of capital, goods and services. Understanding the economic context of health challenges is especially important in a rapidly globalizing economy since economic forces operate at multiple geographical and political scales. A prime example of this is the role of large pharmaceutical companies and large donors in health system dynamics. At the other end of Figure 2, it is important for health innovators to understand the existing health care system’s structure, organization and function, its strengths and weaknesses, and its capacity building priorities. Lessons from the management sciences on process innovation need to be applied to strengthen technical and administrative capacity, especially human resources (see 5.0).
Data at each level of Figure 2 can be gathered, for example, in a GIS spatial database that allows data layers to be viewed separately or together. Today’s GIS technology can be combined with statistical software so that multiple correlations and regressions and spatial cluster analyses on point-pattern data (like disease cases) can be carried out to improve scientific understanding of the relationships between key variables and parameters. Mapping health risk “hot spots” with GIS has great potential: triangulation can proceed as follows:
Start with health effects data (level 6) and work back to explore known or suspected risk/vulnerability factors that may explain health outcomes (epidemiological “back-casting”);
Start with state variables such as pollution, exposures and vulnerabilities and work forward can help predict health outcomes (quantitative risk analysis “forward-casting”);
Examine local and anecdotal information on perceived causes and effects that can contribute to the overall assessment.
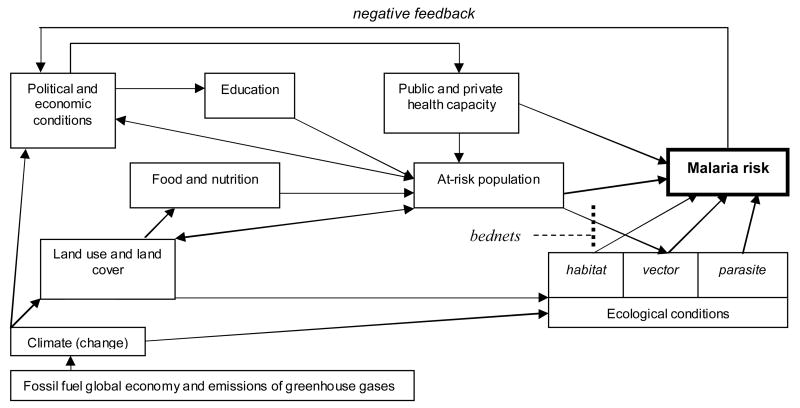
Acute respiratory infections (ARIs, e.g. child pneumonia) and enteric infections (diarrheas) are the number one and two killers of children under five [48]. Environmental state variables for ARIs and enterics include particulate matter levels in personal air, and pathogen levels in drinking water respectively (level 3, Figure 2). Exposure indicators are dose rates of these contaminants (level 4). Candidate vulnerability indicators for many health problems (level 5) include nutritional status, literacy, education level, income, age, gender, and access to health care. Sharing data-gathering tasks among multiple stakeholders is a practical way to enrich the scope of the analysis. Few diseases illustrate the need for systems-based understanding and multi-level indicators and responses better than malaria (Figure 3, Box 4).
Figure 3. Malaria system.
The model shows the need to understand the contextual richness of the disease, identify drivers. Interventions based on systems understanding emphasize prevention, are more strategic, sustainable and cost-effective; bednets should be one component of an integrated response (after [49]).
BOX 4. Losing the battle with malaria: a loud call for collaboration with vulnerable communities and systems-based understanding
We are also using the approach to design community-based malaria intervention. Malaria has been described as a national tragedy for Kenya, killing over 90 children under five a day [50]. Insecticide-treated bednets (ITNs) are a mainstay of existing programs, like the global Roll-Back Malaria program launched by WHO and the World Bank in 1998. But ITNs are often unaffordable or otherwise inaccessible to the rural poor, especially those in remote rural areas. Even when a household can buy one, it is often the male head of household who sleeps under it, leaving vulnerable children exposed. The nets are often considered uncomfortable and may only last a year [51]. Millennium Project calls for free bednets [3], but this perpetuates dependency, and leaves structural drivers unaddressed (Figure 3).
As well as the limitations of existing ITN-based programs, drug therapies are another mainstay with serious constraints on the ground. In the Bunda District, Mara Region of Western Tanzania, for example, a community survey showed that while the District promotes the use of the sulfur drug SP (of which it has a large supply), people dislike its side effects and self-medicate with chloroquine. But local malaria resists both SP and choroquine [51]. Meanwhile, WHO recommends artemisinin as a first line therapy [52]. Recently, the Government of Zambia and the Roll Back Malaria Program have formed a Malaria Control and Evaluation Partnership supported by a nine-year US$35 million grant from the Gates Foundation. The Zambian Health Ministry will coordinate efforts to purchase and distribute hundreds of thousands of ITNs, thousands of doses of artemisinin combination therapy, and enough insecticide to spray the walls of eligible homes in Zambia. This top-down approach, while larger in scale and more integrated, still lacks the features we advocate, and its impact could be greatly increased were they to be included in revised strategies.
Looking at the persistent human tragedy of malaria though the MUSCLE lens it is possible to view the potential for much more sustainable, integrated solutions. These solutions may combine several or all of the following components for a contextualized response: i) ITNs provided free from the outside; ii) establishment of a local cottage industry to make affordable ITNs with local materials and skills (perhaps treated with a natural insecticide); iii) an educational program to raise awareness of risks and simple ways to mitigate them; iv) vulnerability reduction that tackles socioeconomic and cultural factors that heighten risk (lifestyle and livelihood strategies); v) drug therapy based on artemisinin made available at local clinics; vi) improved nutrition and iron supplements (malaria contributes to iron-deficiency anemia); vii) careful, targeted insecticide spraying; viii) re-vegetation that cools the landscape to temperatures below the breeding range of mosquitoes; ix) swamp reclamation (cool, shaded swamps are not a vector habitat); x) swamp conversion to cropland that uses the fodder crop nappier grass to shade shallow irrigation channels that otherwise become habitat; and xi) changing other land-use practices that encourage the vector, for example stopping brush-clearing that people perceive to be effective but which perversely increases the vector habitat of warm stagnant puddles created by cattle hoofprints. To promote social learning, as well as local stakeholder working groups, we plan to employ health promoters from the affected communities (to be trained in malaria etiology, prevention and treatment methods, and risk communication). Networks are to be set-up to link communities, share knowledge, and build social capital and collective capacity.
3.2 Prioritizing Health Problems
How do we prioritize health problems? Risk and vulnerability theory (RVT) offers a sound, evidence-based approach to prioritization. “Risk” is the probability of an outcome multiplied by the severity of the consequence should it occur [53]: risk “hot spots” are where both probability and consequence are high. WHO [54, p.52] defines risk as the “likelihood of identified hazards causing harm in exposed populations in a specific time frame, including the magnitude of that harm and/or consequences”. Quantitative risk assessment (QRA) involves identification of hazards (specific toxicities of chemical and biological agents), dose-response relationships that model the probability of a given health effect as a function of exposure, and exposure assessment that estimates contact between agents and human targets over time. QRA yields a risk estimate in terms of order-of-magnitude individual or population-level probabilities of a particular disease or endpoint.
An extension of risk theory, vulnerability is defined as: “differential capacity to deal with hazards, based on the position of groups and individuals within both the physical and social worlds” [55, p.59]. Vulnerability may be analyzed in terms of potential exposures, susceptibility to harm, and ability to avoid exposure and cope with harm [56]. Vulnerability comprises: 1) differential exposure to risk agents or stressors, like toxics, floods, droughts, hurricanes; 2) differential susceptibility or sensitivity to adverse outcomes if exposed; 3) differential preparedness to respond to stressors; and 4) differential ‘coping’, ‘resilience’ or ‘adaptability’ or ability to recover from adverse effects [56, 57]. Coping or adaptability involves finding ways to reduce risks by either reducing the probability of an adverse outcome and/or the severity of the outcome should it occur.
Thus high vulnerability to disease can be explained by a combination of three determinants: a) enhanced sensitivity/susceptibility to adverse outcomes from higher-than-background exposure to risk agents (biological, chemical, social, political, and economic) plus a higher probability of adverse response as a result; b) reduced capacity to adapt autonomously; and c) severely reduced or zero planned adaptive capacity. Differential exposure to risks is a function of the quality of the environment(s) people come into contact with, and the type and amount of contact they have: time-activity-environment patterns. Differential sensitivity may be a function of gender, age, immune status etc. (e.g. lead poisoning in infants and small children), while differential adaptability is a function of socio-economic variables. Vulnerability assessment owes much to epidemiology, especially in the case of HIV/AIDS [13, 14, 15, 16, 17, 18].
For policy, a risk and vulnerability approach combined with systems understanding (Fig. 2) expands the range of intervention available to reduce vulnerability. Vulnerability and sustainability can be considered two halves of the same environment-development coin: vulnerability is reduced, sustainability increased, when adaptive capacity is strengthened. The attention paid to capacity building is also reinforced. (see 5.0). A vulnerability approach to assessment also stimulates dialogue and social learning as it creates a space of convergence among different disciplines (e.g. health science, geography, economics and anthropology), types of knowledge (local, anecdotal, indigenous, scientific), and interests.
4.0 SELECTING AMONG INTERVENTIONS
Once priority health problems have been identified and placed in their societal and ecological contexts stakeholders need to identify alternative solutions/interventions and compare the ecological, socio-cultural, economic and political tradeoffs among them; i.e. undertake a sustainability assessment of them. We seek cost-effective, efficient and sustainable interventions. Cost effectiveness is best estimated in terms of expected changes in the risk of disease (prevalence and incidence) per unit resource cost, with resources measured in terms of money, personnel and information.
The call for a new type of multi-criteria analysis to guide decision making stems from a realization of the limitations of two closely linked conventional practices: environmental impact assessment (EIA) and cost-benefit analysis (CBA). EIA is applied to the screening of proposed development projects like roads, hospitals, dams, and factories. It suffers from bias in favor of proposed projects, discourages active participation by the public, and has become a regulatory end in itself, rather than a means to better development choices as originally intended [58]. CBA is widely used to screen and select among project or policy alternatives. Heinzerling and Ackerman [59] launched a strong critique of the method, listing major weaknesses: i) more efficient decisions are not possible because reducing the value of life, health and nature to monetary units is flawed; ii) use of monetary discounting systematically and improperly devalues long-term environmental risks and health effects, and any action that protects the interests of future generations; iii) CBA also reinforces existing patterns of economic, ecological and socio-political inequities, since the method ignores how costs and benefits are distributed in society; and iv) the method as practiced is far from being transparent or objective, and the top-down nature of analysis precludes participation by people most affected by the decisions. They also highlight weakness in practical implementation: benefits are often not quantified (or cannot be), and costs are often skewed in favor of an option preferred by those undertaking or paying for the analysis.
Daly and Cobb [60] scrutinized CBA, arguing it only works as a rational model if one can compare investing in a given project with depositing money in a bank and accruing interest. Satisfaction of many social, political, cultural and ecological needs, either within a current generation or a future one, cannot be valued exclusively in this way [60]. While the use of CBA in policy and regulation is treated with growing skepticism by scholars [59, 60, 61, 62, 63] when incorporated as part of a wider multi-criteria assessment, the limitations of CBA can be overcome. Criteria for health intervention selection can include the following: a) social/health criteria: projected positive and negative impacts (“benefits” and “costs” respectively); b) economic criteria: projected positive and negative impacts in terms of resources (personnel, money, information, facilities); c) ecological criteria: the projected positive and negative impacts in terms of ecology and the natural environment.
This type of transparent multi-criteria sustainability assessment of alternative interventions, with stakeholder agreement on which alternatives to compare, criteria and tradeoffs is basic to fostering both trust and ownership of interventions. It is particularly important to compare scenarios of the future for unstable infectious diseases like malaria and AIDS, assuming each of the different interventions considered. What does a business-as-usual future of AIDS, and malaria look like 10 years, 20 years from now (based on our Figure 2 understanding), and how do alternatives compare? Integrated solutions that control system drivers, and meld prevention and treatment can be devised and compared against the baseline conventional approach. Notably, such sustainability assessment is both conducive of stakeholder dialogue and social learning, and a result of them. Revealing the possibility of an alternative, more positive future - especially for those who see none - is a transformative process.
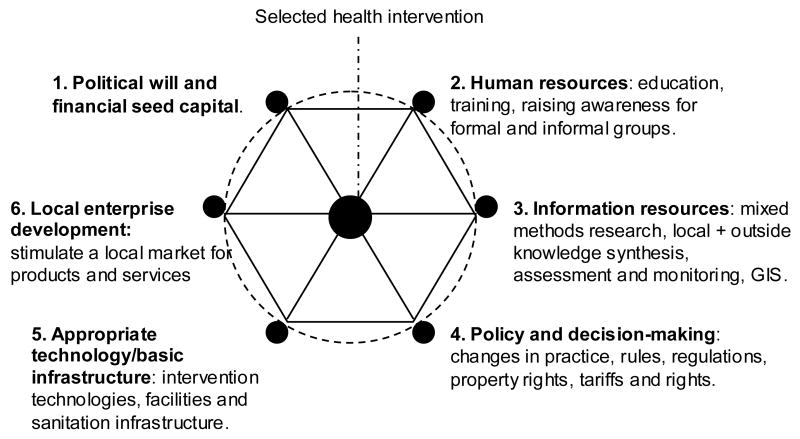
5.0 BUILDING CAPACITY
The last feature of the MuSCLE framework is building societal capacity to sustain selected interventions, and adapt to changing conditions and priorities over time. According to UNDP [64] capacity building is the sum of efforts to develop, enhance and utilize the skills of people and institutions. Systematized capacity building is fundamental to sustainable poverty reduction and health promotion under the MDGs. Participatory integrated capacity building (PICB) is an approach synthesized from literature, international experiences and empirical evidence [65, 66, 67]. Case studies of many types of development projects were compared based on their relative sustainability and key characteristics. Relatively sustainable projects were those yielding a steady stream of net benefits over time after external donor support was withdrawn. Such projects were in the minority (10% of the sample) and distinguished themselves from the majority of case studies by having two distinct predictors of success: a) a project process that built several complementary levels of capacity among stakeholders and the wider society they represented; and b) constructive stakeholder interaction that fostered trust, ownership of a problem and its solution, and empowerment. The approach was originally developed to build multi-stakeholder capacity to sustain urban water supply and sanitation in Mexico [65] and was later extended conceptually to sustaining health risk mitigation [66]. Evidence suggests that to sustain net benefits over time requires the co-strengthening of six interdependent levels of societal capacity:
Political will and financial seed capital to initiate transitions and improve existing policies and practices;
Human resource strengthening – education, training, communication, and raising awareness within formal and informal institutions and among stakeholder groups;
Information resource strengthening – monitoring, data synthesis, analysis and modeling to characterize baseline conditions, identify priority problems and infer drivers;
Policy making and planning – the design, enactment and enforcement of responsive policies, practices, laws, regulations, tariffs, and rights, with equity, accountability and incentive mechanisms;
Basic infrastructure and appropriate technologies – health care facilities, prevention and treatment technologies, and sanitation infrastructure;
Enterprise development and investment stimulation – provision of products and services, stimulation of entrepreneurial activities (especially local) that provide economic sustainability to the health program, substitute seed finance, and subsidize the costs of primary care for the poor.
These six ‘hexagonal’ levels interact with each other to support the program objectives and health solutions at the center (Figure 4). To make the approach practical, each of the six levels is further broken down into smaller operational elements. For example, if reducing under-five mortality by two thirds is the goal (MDG 4), and we have identified a preferred ‘most sustainable’ package of disease-specific interventions for ARI, enterics, malaria etc., the capacity building system supports the interventions as follows:
Figure 4. Capacity building system to sustain health interventions.
A) Based on the work of Downs [65, 66, 67], the health solution is sustained using a system of six different categories of capacities, shown here as a hexagon with the intervention/solution at the center. The intervention plan from the strategic planning stage (stage 2 of Figure 1) - answering what to do, how, where, when, why, with whom, at what cost – includes this hexagonal support system.
Level 2 capacity may include a community education program for children and parents about reducing risks and adopting the interventions; and training for health practitioners;
Level 3 may include a GIS-based monitoring system to evaluate impacts of interventions;
Level 4 may include responsive primary care policies and regulations with accountability;
Level 5 may include health care facilities to deliver the intervention, and sanitation infrastructure; and
Level 6 may include ancillary health care and sanitation products and services.
For a full account of the application of this approach to health risk management, and urban water supply and sanitation in Mexican pilot cities, see Downs [66] and Downs [65] respectively. The hexagonal capacity building actually happens at two levels under MuSCLE: a) micro-level: focused on the specific target priority problem and intervention, and built into the action plan; and b) macro-level: evolving from, and supportive of the social learning process as a whole.
6.0 OVERALL APPROACH: IMPLEMENTATION
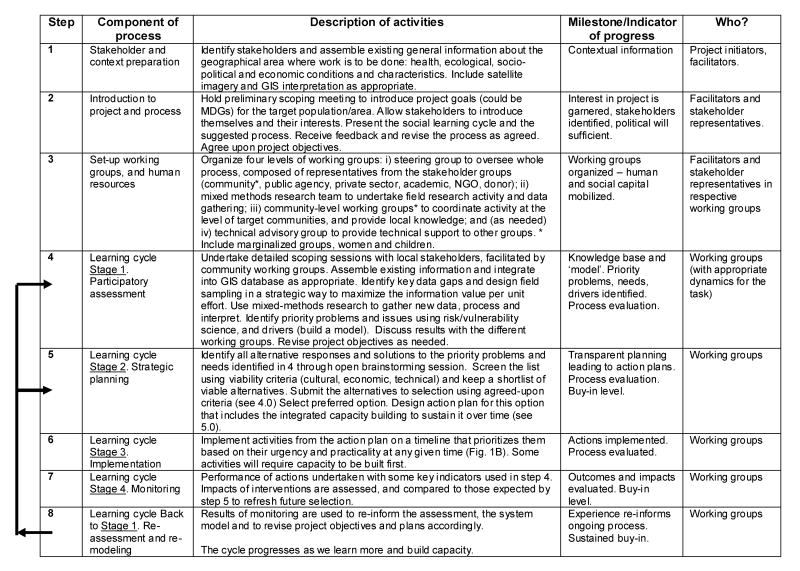
We argue for multi-stakeholder capacity-building and learning for empowerment – MuSCLE - that fosters social learning and strengthens social capital. The MuSCLE process has three main features: 1) Participatory, systems-based assessment of health challenges and responses; 2) Selection among intervention alternatives that makes tradeoffs transparent; and 3) A support system of capacity building to sustain adaptive interventions. In theory, the process is transferable across different, yet interrelated MDG sectors – health, energy, agriculture, industry, water - such that economies of scale can be exploited in severely resource-limited settings. It derives from and maintains a “living dialogue with genuine needs” that Havel [68, p.119] advocates, favoring partnerships between formal and informal structures that encourage creative thought, communication and social learning. Table 1 describes generic guidelines for implementation, while Box 5 sets down ten operating principles.
Table 1. Practical guidelines for implementing a MuSCLE approach.
The steps assume that funding has been obtained for a project in a target population and setting. If funding has not yet been obtained, initiators may undertake steps 1–2 and develop a funding proposal that competes for funds to complete the process. While the steps are generic, details of what happens and how is driven by specific project objectives and context. The working groups are informal and change as the project evolves and objectives change. Steps 4–8 reflect an iterative process, with knowledge and lessons learned being actively incorporated to improve understanding and progress.
Box 5. Guiding principles for a MuSCLE approach
People-at-risk need to be full partners in understanding and solving their own health problems.
Prevention and treatment options should be melded, with more emphasis on the former.
Invest in social learning that builds trust, social capital and capacities to target priority health problems, stimulating ownership of problems and solutions.
The partnership should comprise representatives from: i) formal community-based organizations (CBOs); ii) informal civil society groups (especially marginal groups, women and youth); iii) academic researchers; iv) donors; v) governmental health agencies (local, district, state, including health practitioners); vi) non-governmental agencies (NGOs); and vii) private sector businesses.
Partners are involved in appropriate ways in all four stages of a learning cycle: assessment, planning, implementation and monitoring that re-informs assessment. Rules of engagement, and the roles and responsibilities of partners are explicit and agreed-upon by all those involved.
Disruptive forces - corruption, destructive political interactions, and burdensome transaction costs - are to be monitored and mitigated. Understanding power relations and institutional frameworks is essential.
The knowledge base about health conditions, characteristics, priorities and drivers is built collectively, inclusive of indigenous knowledge. Priorities are identified based on an evidence-based risk and vulnerability approach. The integrated systems-based understanding of health problems includes their socio-cultural, political and economic contexts. Any model should be as simple as possible, no simpler.
Decision making is transparent, with agreement about priority problems, viable alternative solutions, by what criteria they are to be compared, and how this is to be done.
Capacity building benefits for partners are made explicit and equitable to ensure sustained buy-in and commitment, and action plans include the requisite capacity building needed to sustain solutions.
Economies of scale across problems and sectors should be exploited for cost effectiveness, sustainability and maximum impact.
6.1 Risks and Obstacles
Institutional inertia and resistance to new approaches must be overcome for the process to flourish. This is best done by making benefits explicit, proving the success of the approach in high-profile pilot projects, and demonstrating transferability. Three major risks are corruption, high transaction costs and destructive politics among stakeholders, but these risks can be minimized and/or mitigated by a carefully crafted MuSCLE approach that stimulates dialogue, builds collective understanding, and distributes the benefits of social learning and capacity building. The relationship between corruption and poverty has been explored by Downs [67] in the context of elites that regulate the flow of information within a society, and discourage community empowerment by placing high transaction costs on bureaucratic and legal procedures. The relationship between corruption, health, poverty and development is far from simple; scholar-practitioners need to undertake research to better understand it in a given setting [69, 70, 71]. Strong community ownership of a sanitation project on the Mexican side of the US-Mexico Border, for example, successfully mitigated attempts by corrupt groups to gain control of the project [67].
High transaction costs are a major risk for multi-stakeholder projects, and have been partly responsible for skepticism with the public participation and partnership process. Falconer [72] flags the risks of high transaction costs for farmers and the state involved in inefficient participatory processes for agro-environmental schemes in the European Union. She recommends governments rationalize how farmers apply to different schemes, minimizing overhead costs, and promote longer-term capacity building for farmer networks. Successful NGOs build their own capacity to mitigate high transaction costs, and can act as facilitators of a MuSCLE approach. Cameron [73] draws on 50 years of modern development economics, and the past ten years of New Institutional Economics (NIE) to assert that NGOs working on micro-finance and income generation can be agents who redistribute transaction and transition costs, risks and uncertainties, in favor of the poor. Without due care, interactions among stakeholders may deteriorate into conflict that expends large amounts of social and financial capital, and leave project goals unmet. Businesses have significantly reduced transaction costs by internalizing them through diversified networks [74], and networks that cross-subsidize each others’ capacities can attain formidable capacity in partnership.
Looking at the constraints and determinants of women’s participation in local groups in Chad and Kashmir, Weinberger and Jutting [75] identified the risk that the middle classes appropriate the process, while the high opportunity costs and low bargaining power of the poor conspire to exclude them. This highlights the importance of any process being broadly representative of diverse interests in a community and horizontal in organization [19]. Working in China, Shenkar and Yan [76] also remind us to pay attention to political dynamics and power relations among stakeholders (see 3.2). Trying to explain the failure of international cooperative ventures simply using limited theories of transaction costs, partner selection, or bargaining and learning may neglect an underlying destructive dynamic of political behavior. Svendsen et al. [77] argue that prosperity differences between rich and poor countries can be explained by stocks and flows of social capital that promote informal human exchanges and the voluntary provision of collective goods like trust that mitigate destructive politics.
7.0 CONCLUSION
In his 1961 inaugural speech, President John F. Kennedy spoke of the need to “forge a grand and global alliance” against the “common enemies of Man: tyranny, poverty, disease and war itself” [78]. The case for using a MuSCLE-type approach to design health interventions - a trans-epistemological, multi-stakeholder process that fosters social learning and builds societal capacity for sustainable health improvement and poverty reduction - is compelling. Biomedical responses to global health concerns must evolve to become integral partners in this creative, organic and collaborative endeavor. The process is necessarily transferable across development sectors and priorities, and can be scaled up or down to suit project objectives. A MuSCLE-bound process fostering ownership of health and poverty problems and their solutions promises significant progress; we should fully explore its potential between now and 2015. Without it, or something a lot like it, global health goals will remain unmet. With it those goals can not only be met, but likely surpassed.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Timothy J. Downs, Environmental Science and Policy Graduate Program, Department of International Development, Community and Environment (IDCE) and George Perkins Marsh Research Institute, Clark University, 950 Main Street, Worcester, Massachusetts 01610, USA. Tel: (+1) 508 421 3814; Fax: (+1) 508 793 8820; email: tdowns@clarku.edu.
Heidi J. Larson, Harvard Center for Population and Development Studies, 9 Bow Street, Cambridge, Massachusetts 02138. Tel: (+1) 646 764 5161; Fax: (+1) 617 495 5418 email: hlarson@hsph.harvard.edu
References Cited
- 1.UN. Millennium Development Goals Report 2005. 2005 http://unstats.un.org/unsd/mi/pdf/MDG%20Book.pdf, consulted 04/06.
- 2.UN. 2005 United Nations website: http://www.un.org/millenniumgoals/, consulted 01/05.
- 3.MP. Millennium Project; New York: 2005. Investing in development: a practical guide to achieve the Millennium Development Goals. UN 2005. http://www.unmillenniumproject.org/goals/goals02.htm, consulted 05/04/05) [Google Scholar]
- 4.Woodhill J, Röling NG. The second wing of the eagle: the human dimension in learning our way to more sustainable futures. In: Röling NG, Wagemakers MAE, editors. Facilitating sustainable agriculture. Cambridge University Press; Cambridge: 1998. pp. 46–71. [Google Scholar]
- 5.Guangxia C, Lianmin Z. In: Social learning in community forests. Wollenberg E, Edmunds D, Buck L, Fox J, Brodt S, editors. CIFOR and East-West Center; Jakarta, Indonesia: 2001. pp. 109–126. [Google Scholar]
- 6.Buck LE, Wollenberg E, Edmunds D. Social learning in collaborative management of community forests: lessons from the field. In: Wollenberg E, Edmunds D, Buck L, Fox J, Brodt S, editors. Social learning in community forests. CIFOR and East-West Center; Jakarta, Indonesia: pp. 1–20. [Google Scholar]
- 7.Daniels S, Walker G. Rethinking public participation in natural resources management: concepts from pluralism and five emerging approaches. FAO; Pluralism and sustainable forestry and rural development. Proceedings of an international workshop; 9–12 December 1997; Food and Agriculture Organization, Rome. 1999. pp. 29–48. [Google Scholar]
- 8.Gray-felder D, Deane J. Communication for Social Change: A position paper and conference report. 1999 www.communicationforsocialchange.org.
- 9.Kawachi I, O’Neill M. Exploration of heaqlth disparities. Essays on the future of environmental health research: a tribute to Dr. Kenneth Olden. In: Goehl TJ, editor. Environmental Health Perspectives and NIEHS. Research Triangle Park; NC: pp. 100–107. [Google Scholar]
- 10.Corburn J. Confronting the challenges in reconnecting urban planning and public health. American Journal of Public Health. 2004;94(4):541–546. doi: 10.2105/ajph.94.4.541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Larson H, Narain J. Beyond 2000: Responding to HIV/AIDS in the New Millennium. World Health Organization; New Delhi: 2001. [Google Scholar]
- 12.Lebel J. Health: An ecosystem approach. Ottawa, Canada: International Development Research Center; 2003. p. 84. [Google Scholar]
- 13.Galea S, Ahern J, Karpati A. A model of underlying socioeconomic vulnerability in human populations: evidence from variability in population health and implications for public health. Social Science Medicine. 2005;60(11):2417–2430. doi: 10.1016/j.socscimed.2004.11.028. [DOI] [PubMed] [Google Scholar]
- 14.Piwoz EG, Bentley ME. Women’s voices, women’s choices: the challenge of nutrition and HIV/AIDS. Journal of Nutrition. 2005;135(4):933–937. doi: 10.1093/jn/135.4.933. [DOI] [PubMed] [Google Scholar]
- 15.Abel E, Chambers K. Factors that influence vulnerability to STDs and HIV/AIDS among Hispanic women. Health Care Women International. 2004;25(8):761–780. doi: 10.1080/07399330490475601. [DOI] [PubMed] [Google Scholar]
- 16.Bates I, Fenton C, Gruber J, Lalloo D, Lara AM, Squire SB, Theobald S, Thomson R, Tolhurst R. Vulnerability to malaria, tuberculosis and HIV/AIDS infection and disease. Part 1: determinants operating at individual and household levels. Lancet Infectious Disease. 2004a;4(5):267–277. doi: 10.1016/S1473-3099(04)01002-3. [DOI] [PubMed] [Google Scholar]
- 17.Bates I, Fenton C, Gruber J, Lalloo D, Lara AM, Squire SB, Theobald S, Thomson R, Tolhurst R. Vulnerability to malaria, tuberculosis and HIV/AIDS infection and disease. Part 1: determinants operating at environmental and institutional levels. Lancet Infectious Disease. 2004b;4(5):267–277. doi: 10.1016/S1473-3099(04)01047-3. [DOI] [PubMed] [Google Scholar]
- 18.De Moura SL. The social distribution of reports of health-related concerns among adolescents in Sao Paulo, Brazil. Health Education Research. 2004;19(2):175–184. doi: 10.1093/her/cyg023. [DOI] [PubMed] [Google Scholar]
- 19.Larson H. Light my Fire: Community mobilization and HIV/AIDS. Working paper prepared for UNAIDS; Geneva: 1998. [Google Scholar]
- 20.Rossi D. Drug Users involvement in AIDS prevention. Paper presented at the 10th International Conference on AIDS.1994. [Google Scholar]
- 21.Murphy JP. Pragmatism: from Pierce to Davidson. Westview Press; Boulder, CO: 1990. [Google Scholar]
- 22.IRC. Community management: the way forward. Report of the workshop; 19–27 November 2001; Rockanje, Netherlands. 2001a. [Google Scholar]
- 23.IRC. From system to service – scaling-up community management. Report of the conference; 12–13 December 2001; The Hague, Netherlands. 2001b. [Google Scholar]
- 24.Bolt E, Khadka R. Sustainable Development International. 3. ICG Publishing Ltd; London: 2000. Water supply management by communities: a new challenge for support agencies; pp. 65–70. [Google Scholar]
- 25.Brikke F. Operation and maintenance of rural water supply and sanitation systems: a training package for managers and planners. World Health Organization; Geneva, Switzerland: 2000. [Google Scholar]
- 26.CEFOC. Modèles de gestion privée oue déléguée de la maintenance de systèmes d’AEP. Training session on management of maintenance for drinking water in rural areas, EIER/ETSHER. 1999:8–26. March, 1999. [Google Scholar]
- 27.Chambers R. Understanding professionals: small farmers and scientists. IADS Occasional Paper; International Agriculture Development Service, New York. 1980. [Google Scholar]
- 28.Chambers R. Rural development: Putting the last first. Longman 1992 [Google Scholar]
- 29.Estienne C. Making community management of piped water systems in the secondary towns of Senegal river valley more professional. In: Le Jalle C, et al., editors. Water supply and sanitation in peri-urban areas and small centers. GRET, Programme; 1999. pp. 129–131. [Google Scholar]
- 30.Livingstone AJ. WHO and WSSCC Working Group on Operation and Maintenance, Operations and maintenance of water supply and sanitation systems: case studies. World Health Organization; Geneva, Switzerland: 1994. Community management of small urban water supplies in Sudan and Ghana; pp. 44–56. [Google Scholar]
- 31.Moriarty PB. Broadening water supply to address rural livelihoods. Proceedings of 27th WEDC Conference, People and systems for water, sanitation and health; 20–24 August 2001; Lusaka, Zambia. 2001. [Google Scholar]
- 32.World Bank. World development report: infrastructure for development. Oxford University Press; Oxford, UK: 1994. p. 254. [Google Scholar]
- 33.WSSCC. Vision 21: Water for People – a shared vision for hygiene, sanitation and water supply. Water Supply and Sanitation Collaborative Council; Geneva, Switzerland: 2000. [Google Scholar]
- 34.King ML. Where do we go from here: Chaos or Community? Harper & Row; New York: 1967. [Google Scholar]
- 35.Lynn FM. Community-scientist collaboration in environmental research. American Behavioral Scientist. 2000;44(4):649–663. [Google Scholar]
- 36.Arcury TA, Austin CK, Quandt SA, Saavedra R. Enhancing community participation in intervention research: farmworks and agricultural chemicals in North Carolina. Health Education and Behavior. 1997;26(4):563–578. doi: 10.1177/109019819902600412. [DOI] [PubMed] [Google Scholar]
- 37.Ashford NA, Rest KM. Public participation in contaminated communities. Cambridge, MA: Center for Technology, Policy and Industrial Development, MIT; 1999. [Google Scholar]
- 38.Couto R. Failing health and new prescriptions: community-based approaches to environmental risks. In: Hill CE, editor. Contemporary health policy issues: an applied social perspective. University of Georgia Press; Athens: 1984. [Google Scholar]
- 39.Israel BA, Schultz AJ, Parker EA, Becker AB. Review of community-based research: assessing partnership approaches to improve public health. Annual Review of Public Health. 1998;19:173–204. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- 40.Lynn FM, Busenburg G. Citizen advisory committee and environmental policy. Risk Analysis. 1995;15:147–162. [Google Scholar]
- 41.Scammell M. In: Environmental justice: partnerships for communication and community-based prevention-intervention research. Jackson MS, editor. Starkville: National Institute of Environmental Health Sciences and Mississippi State University; 1999. Proceedings October 4–6, 1999. [Google Scholar]
- 42.Schell L, Tarbell A. A partnership study of PCBs and the health of Mohawk youth: lessons from our past and guidelines for our future. Environmental Health Perspectives. 1998;106(Suppl 3):833–840. doi: 10.1289/ehp.98106833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Northridge ME, Shoemaker K, Jean-Louis B, Ortiz B, Swaner R, Vaughan RD, Cushman LF, Hutchinson VE, Nicholas SW. Using community-based participatory research to ask and answer questions regarding the environmental and health. In: Goehl TJ, editor. Essays on the future of environmental health research: a tribute to Dr. Kenneth Olden. Environmental Health Perspectives and NIEHS; Research Triangle Park, NC: pp. 34–41. [Google Scholar]
- 44.Wing S. Environmental justice, science and public health. In: Goehl TJ, editor. Essays on the future of environmental health research: a tribute to Dr. Kenneth Olden. Environmental Health Perspectives and NIEHS; Research Triangle Park, NC: 2005. pp. 54–63. [Google Scholar]
- 45.Cranmer JM. The role of town meetings in environmental health research. In: Goehl TJ, editor. Essays on the future of environmental health research: a tribute to Dr. Kenneth Olden. Environmental Health Perspectives and NIEHS; Research Triangle Park, NC: 2005. pp. 152–161. [Google Scholar]
- 46.Holling CS. Understanding the complexity of economic, ecological and social systems. Ecosystems. 2001;4:390–405. [Google Scholar]
- 47.WHO. Environmental health indicators: framework and methodologies. WHO, Geneva: Report WHO/SDE/OEH/99.10; 1999. [Google Scholar]
- 48.WHO. Reducing mortality from major childhood killer diseases. 2005 Fact Sheet #180. http://www.who.int/child-adolescent-health/New_Publications/IMCI/fs_180.htm, consulted 05/05.
- 49.Fischhoff B, Fischhoff IR, Casman EA, Dowlatabadi H. Integrated assessment of malaria risk. In: Casman EA, Dowlatabadi H, editors. The contextual determinants of malaria. Resources for the Future; Washington, D.C: 2002. pp. 331–348.pp. 382 [Google Scholar]
- 50.Laakonnen H. 2005. Quoted in East African Standard April 20, 2005.
- 51.Malaika Project. 2005 Malaika Project website: www.malaikaproject.org, consulted 05/2005.
- 52.WHO. The use of Artemisinin and its derivatives as anti-malarial drugs. 1998 At: http://www.who.int/malaria/docs/artrep.htm#p7, consulted 05/05.
- 53.Wilson R, Crouch EAC. Risk-benefit analysis. Cambridge: Harvard University Press; 2001. p. 370. [Google Scholar]
- 54.WHO. Guidelines for Drinking Water Quality. 3. World Health Organization; Geneva: 2005. [Google Scholar]
- 55.Clark, et al. Assessing the vulnerability of coastal communities to extreme storms: the case of Revere, MA, USA. In: Goehl TJ, editor. Mitigation and adaptation strategies for global change. 1998. pp. 59–82. [Google Scholar]
- 56.Ahmad QK, et al. Summary for policy makers. In: Climate change 2001: impacts, adaptation and vulnerability. In: McCarthy JJ, Canziani OF, Leary N, Dokken DJ, White K, editors. Contribution of the Working Group II to the Third Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge: 2001. [Google Scholar]
- 57.NEJAC/EPA. Ensuring Risk Reduction in Communities with Multiple Stressors: Environmental Justice and Cumulative Risks/Impacts. Report developed from the National Environmental Justice Advisory Council Meeting; April 13–16, 2004; USEPA, Washington, DC. 2004. [Google Scholar]
- 58.Brown AL. Decision scoping. Environmental methods review: retooling impact assessment for the new century. In: Porter AL, Fittipaldi JJ, editors. Army Environmental Policy Institute (AEPI) and International Association for Impact Assessment (IAIA) The Press Club; Fargo, ND: 1998. pp. 135–143. [Google Scholar]
- 59.Heinzerling L, Ackerman F. Georgetown Environmental Law and Policy Institute. Georgetown University Law Center; Washington, D.C: 2002. Pricing the priceless: cost-benefit analysis of environmental protection. [Google Scholar]
- 60.Daly HE, Cobb JB., Jr . For the common good: redirecting the economy toward community, the environment, and a sustainable future. 2. Beacon Press; Boston: 1994. p. 531. [Google Scholar]
- 61.Goodstein E. Polluted data. American Prospect 8. 1997 www.prospect.org.
- 62.Richardson HS. The stupidity of the cost-benefit standard. Journal of Legal Studies. 2000;29:971–1003. [Google Scholar]
- 63.Harrington W, Morgenstern RD, Nelson P. On the accuracy of regulatory cost estimates. Journal of Policy Analysis and Management. 2000;19:297–322. [Google Scholar]
- 64.UNDP. About Capacity 21. UNDP. 2001 website: http://www.unescap.org/drpad/vc/orientation/M3anx_pic_c21.htm, consulted 01/05.
- 65.Downs TJ. Making sustainable development operational: Integrated capacity building for the water supply and sanitation sector in Mexico. J Environmental Planning and Management. 2001a;44(4):525–544. [Google Scholar]
- 66.Downs TJ. Sustainable health risk management and the role of cross-disciplinary professionals in developing countries: Mexican experience. Environment Development & Sustainability. 2001b;3(1):60–81. [Google Scholar]
- 67.Downs TJ. Changing the culture of underdevelopment and unsustainability. J Environmental Planning and Management. 2000;43(5):601–621. [Google Scholar]
- 68.Havel V. Living in truth. Faber and Faber; London: 1986. p. 315. [Google Scholar]
- 69.Qizilbash M. Corruption and human development: a conceptual discussion. Oxford Development Studies. 2001;29(3):265–278. [Google Scholar]
- 70.Caiden G. Corruption, development and underdevelopment. Journal of Public Administration Research and Theory. 1(4):484–488. [Google Scholar]
- 71.Palmier L. Corruption, development and inequality. Journal of Public Administration Research and Theory. 1990;10(4):475–476. [Google Scholar]
- 72.Falconer K. Farm-level constraints on agri-environmental scheme participation: a transaction perspective. Journal of Rural Studies. 2000;16(3):379–394. [Google Scholar]
- 73.Cameron J. Development economics: the new institutional economics and NGOs. Third World Quarterly. 2000;21(4):627–635. [Google Scholar]
- 74.Lee JW. The nature of Chaebol restructuring: two lessons from Professor Coase. Journal of International and Area Studies. 2002;9(2):23–41. [Google Scholar]
- 75.Weinberger K, Jutting JP. Women’s participation in local organizations: conditions and constraints. World Development. 2001;29(8):1391–1404. [Google Scholar]
- 76.Shenkar O, Aimin Y. Failure as a consequence of partner politics: learning from the life and death of an international corporate venture. Human Relations. 2002;55(5):565–601. [Google Scholar]
- 77.Svendsen GLH, Svendsen GT. On the wealth of nations: Bourdieuconomics and social capital. Theory and Society. 2003;32:607–631. [Google Scholar]
- 78.Kennedy JF. Presidential inaugural address. http://www.jfklibrary.org/j012061.htm.