Abstract
Objectives
To examine teaching experiences in residency programs accredited by the American Society of Health-System Pharmacists (ASHP) and how they relate to career choices of residents.
Methods
An online survey instrument was developed that asked former residents about the type of teaching experiences they completed during their residency and the effect of these experiences on the decision to pursue an academic career. Our target population was pharmacists completing accredited residencies from 2003-2006.
Results
Four hundred fifty-five (11% of the target population) pharmacists who had completed a residency responded. Former residents who completed 2 years of postgraduate training were significantly more likely to participate in all teaching experiences identified by this survey (p < 0.008). Former residents in college- or school-affiliated programs were significantly more likely to participate in all of the teaching experiences identified (p < 0.003). Former residents who went on to take a faculty position were more likely to have given lectures, participated in problem-based learning (PBL) or small group seminars (SGS), and served as a primary preceptor (p < 0.008) during their residency.
Conclusions
Residents who eventually became faculty members were more likely to have acquired training and experience in teaching during their residency programs.
Keywords: residency training, teaching experience, pharmacy faculty shortage, scholarship of teaching and learning certificate (STLC) program
INTRODUCTION
The demand for pharmacists has increased steadily in the United States over the past decade. In 2000, the National Association of Chain Drug Stores reported a pharmacist position vacancy rate between 6% and 7%.1 The same year, the American Society of Health-System Pharmacists (ASHP) reported a vacancy rate of slightly over 9%.1 Contributing factors to the increasing demand for pharmacists include aging of the population, increased use of prescription medications, and expansion of clinical services provided by pharmacists. A 2004 analysis of clinical pharmacy services staffing estimated that in order to provide core clinical pharmacy services (drug information, adverse drug reaction management, drug protocol management, medical rounds, and admission drug histories) to all inpatients by 2020, an increase of 14,508 full-time equivalent (FTE) pharmacists would be necessary.2 One way to meet this large demand for pharmacists and pharmacy services is to increase the supply of PharmD graduates. Established colleges and schools of pharmacy are increasing class size and new pharmacy programs are opening. Pharmacy student enrollment has increased by an average of 7% each year for the past 5 years.3 As a result of the large increase of pharmacy students, a shortage of faculty members has developed. A 2004 survey conducted by the American Association of Colleges of Pharmacy (AACP) revealed 396 vacant faculty positions at 76 schools of pharmacy.4 The reason cited for more than half (55.7%) of these vacancies was a lack of qualified applicants. A search through the Personnel Placement Service (PPS), a job recruitment service in association with ASHP, revealed that 41 colleges and schools of pharmacy were actively recruiting for pharmacy practice faculty positions as of December 2006.5 Most of these colleges and schools were recruiting for multiple positions. Many qualified candidates for faculty positions are pharmacists who have recently completed an ASHP-accredited residency. However, as evidenced by the low number of applicants for faculty positions, the majority of pharmacists who complete residency training do not go on to work in academia. Instead most opt for positions as clinical specialists or choose careers in management or industry. A possible reason why few pharmacists enter academia upon completion of a residency is that during residency training they have limited exposure to and/or training in the variety of teaching experiences that would be expected of a faculty member. These teaching experiences include experiential teaching (precepting students on advanced pharmacy practice experiences [APPEs]), didactic teaching (giving formal classroom lectures), and problem-based learning (teaching in a small group setting).
Three major components in the job description of a pharmacy practice faculty member are clinical practice, scholarship, and teaching. The emphasis on the individual components varies between institutions; however, competence in all of these areas is necessary for success in academia. During residency training, a pharmacist will work to develop the necessary clinical skills to be a successful practitioner through multiple required rotations. The outcomes required to attain this are further defined in the ASHP pharmacy residency accreditation standards.6,7 Completion of a research project or medication use evaluation (MUE) is also a requirement of ASHP-accredited residencies. When a pharmacist uses a residency to prepare for a career in academia, the missing training component may be teaching experience.
Outcomes related to teaching are included in the ASHP accreditation standards; however, they do not necessarily mandate the completion of the types of teaching experiences for which a faculty member would be responsible. The post-graduate year 1 (PGY1) accreditation standards contain an outcome that states “Provide medication and practice-related education/training.” This may include patient counseling, education of other health care professionals, and education of the public.6 In the PGY2 accreditation standards, one of the stated goals is “to deliver effective education and training programs.”7 The PGY2 standards also include the goal to “Enhance the skills of pharmacy technicians, pharmacy students, pharmacy residents, or pharmacists.” Residents will need to complete some teaching experiences to meet these goals; however, they may not have the opportunity to get the quantity and quality of teaching experiences they need to be prepared for a career in academia.
No one has described the type of teaching experiences residents have during an accredited residency or if these impact future career decisions or prepare residents for an academic career. This project was designed to examine teaching experiences in ASHP-accredited residency programs and how they relate to the decision to pursue an academic career.
METHODS
This study was approved by the Texas Tech University Health Sciences Center Institutional Review Board for the Protection of Human Subjects. The target study population consisted of pharmacists who had completed an ASHP-accredited residency during the years 2003-2006. A list of residency directors was generated from the ASHP residency listings. An e-mail was sent to all residency directors (approximately 800), asking them to forward the e-mail which contained a link to an online survey instrument to their residents from the previous 3 years (2003-2006). The survey instrument asked former residents about the type of teaching experiences completed during accredited residency training. The effect of these experiences on the decision to pursue an academic career was assessed. Individuals who pursued a career in academia were asked to reflect on how well their residency experience prepared them for their position. All responses were maintained within a web survey program. Anonymity was maintained at all times. After 4 weeks, the survey was closed and responses were transferred to an Excel spreadsheet and evaluated using Analyze-it (Analyse-it Software, Ltd, Leeds, England, United Kingdom) for Microsoft Excel. Nominal data were analyzed via Chi square and Fisher's exact test as appropriate. Alpha level of significance was defined as <0.05.
RESULTS
Based on the ASHP-published resident rosters, approximately 4000 pharmacists completed an accredited residency between 2003 and 2006. We received 455 submissions, accounting for approximately 11% of the total number of targeted residents. Thirteen percent (59) of respondents went on to take faculty positions after completion of residency training. Forty-six percent (205) of residents were in programs affiliated with a college or school of pharmacy (COP/SOP). Sixty-nine percent (266) of residents who chose a nonacademic career indicated they currently precept pharmacy students.
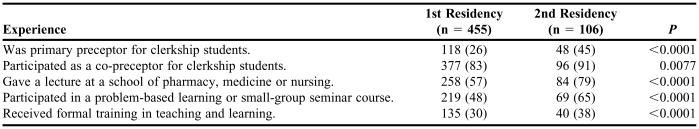
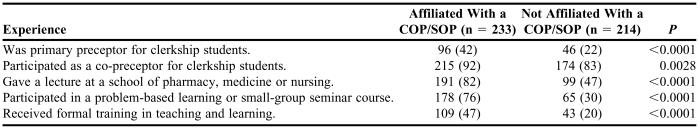
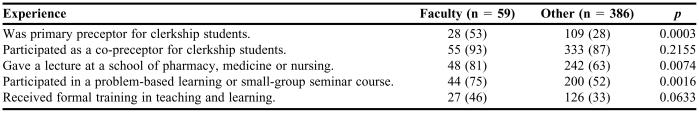
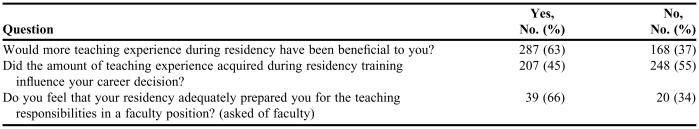
Table 1 lists the teaching experiences reported by survey respondents. Residents who completed 2 years of postgraduate training were significantly more likely to participate in all teaching experiences identified by this survey (p < 0.008). A comparison of teaching experiences between residents at COP/SOP-affiliated programs and those who were not is shown in Table 2. Residents in COP/SOP-affiliated programs were significantly more likely to participate in all teaching experiences identified by this survey (p < 0.003). Table 3 compares the teaching experiences of residents who went on to take faculty positions with those who did not. Residents who went on to take a faculty position were more likely to have given lectures, participated in problem-based learning (PBL) or small group seminars (SGS), and served as a primary preceptor (p < 0.008). There was a trend towards those that became faculty having received formal training in teaching (p = 0.0633). Resident responses to questions about the effect of teaching experiences during residency are shown in Table 4.
Table 1.
Number of PharmD Residents Completing Teaching Experiences During Residency, No. (%)
Table 2.
Teaching Experiences of Residents Who Completed College- or School-affiliated Residencies Compared to Those Who Completed Residencies Not Affiliated With a College or School of Pharmacy, No. (%)
COP = college of pharmacy; SOP = school of pharmacy
Table 3.
Teaching Experiences of Residents Who Took a Faculty Position Upon Completion of a Residency Compared With Those Who Did Not, No. (%)
Table 4.
Resident Thoughts About Teaching Experiences During Residency Training
DISCUSSION
Recruiting pharmacy practice faculty members is challenging. Approximately 20% of pharmacy students choose to pursue residency training.8 In our study population, only 13% of residents went on to take faculty positions. Given these statistics, only about 2% of pharmacy students are taking the path to a faculty position. A 5-year study ending in 2001 showed a turnover of 10.6% among pharmacy practice faculty.9 The expansion in the number of pharmacy practice faculty positions at many institutions is creating even more vacancies. If these trends continue, the number of new faculty candidates each year will not keep pace with the number of vacant positions.
Our data suggest that the chances of a resident choosing a career in academia are increased if they acquire experience in the various types of teaching described in our survey. We have also shown that COP/SOP-affiliated residencies and residents completing 2 years of residency had a positive association with the amount of teaching experience residents received during their training. The majority of past residents agreed that more teaching experience during residency training would be beneficial. However, outside of co-precepting, many residents in accredited programs get little teaching experience.
One potential solution to this problem is the implementation of a scholarship of teaching and learning certificate program (STLC) for pharmacy residents. Originally described by Romanelli et al,10 this type of program was designed under the premise that “great experts do not always make great teachers” and its purpose is to provide pharmacy residents with supplemental formal training in teaching. The components of the program include a seminar series, problem-based learning activities, preparation and delivery of didactic lectures, and development of a teaching portfolio. Residents are evaluated and given feedback for all teaching activities completed. The program is an optional experience offered to both PGY1 and PGY2 residents. It can be completed over 1 or 2 years. A follow-up evaluation of this program was published in 2005.11 The authors administered a survey to past residents to assess confidence in teaching ability before and after residency training. The survey showed that residents who completed the STLC program had a significantly greater improvement in confidence in teaching ability than residents who did not complete the program.
It may be beneficial to expand on the work of Romanelli et al to make separate formal teaching/learning education programming for PGY1 and PGY2 residents. For example, precepting may be the primary focus of PGY1 programming, as our data suggest that a large proportion of pharmacists who complete PGY1 residencies go on to precept students in their next position. PGY2 programming may be structured to provide more education in other areas of teaching such as lecture preparation, objective writing, etc. This would provide PGY2 residents with some of the skills necessary to take on careers with a larger teaching component such as pharmacy practice faculty positions. This would also prevent duplication of topics for residents who complete multiple residencies at the same institution. Further defining the educational goals and outcomes related to teaching within both PGY1 and PGY2 residencies should be considered to ensure that residents receive adequate preparation for both faculty and nonfaculty positions. This may include specific requirements for residents to precept students, prepare and deliver lectures, and participate in problem-based learning experiences. Another way to train residents to teach and stimulate interest in academia is to develop a teaching and learning elective rotation for residents. The idea of developing a teaching rotation for pharmacy students has been previously described in the literature.12-14 This type of rotation should be offered to pharmacy residents to provide further exposure to teaching and the challenges and rewards of an academic career. A continuum of exposure to teaching is important to increase interest in academia. This includes offering elective teaching rotations for pharmacy students, encouraging students to pursue residencies, providing training and experience in teaching during residency, encouraging PGY1 residents to complete PGY2 residencies, further exposing PGY2 residents to academia, and finally encouraging PGY2 residents to consider careers in academia.
Limitations
Although we received 455 survey responses, this number represented only 11% of all residents completing accredited residencies during the years 2003-2006. Thus, this sample may not accurately reflect the whole population of pharmacists who completed residency training during this time. The survey had to be forwarded from residency directors to past residents to be completed. This extra step likely contributed to the low response rate. Selection bias is a potential issue in this survey in that past residents who were interested in teaching may have been more likely to respond. The respondents were not given definitions of the teaching activities (ie, lecture, PBL, etc) so it is possible that this led to inconsistent interpretation of some survey items.
CONCLUSIONS
Gaining teaching experience is an important but often overlooked aspect of pharmacy residency training. Pharmacists who eventually became faculty members were more likely to have acquired training and experience in teaching during residency training. Second-year residencies and affiliation with a school of pharmacy have a positive association with increased opportunities to acquire teaching experience. Ensuring that pharmacy residents get training and experience in teaching may help to alleviate the current shortage of pharmacy faculty members as well as provide well-rounded clinicians who can meet the increasing demand for qualified preceptors.
REFERENCES
- 1. The Pharmacist Workforce – A study of the supply and demand for pharmacists. Department of Health and Human Services. 2000. Available at: ftp://ftp.hrsa.gov/bhpr/nationalcenter/pharmacy/pharmstudy.pdf.
- 2.Bond CA, Raehl CL, Patry R. Evidence-based core clinical pharmacy services in United States hospitals in 2020: services and staffing. Pharmacotherapy. 2004;24:427–40. doi: 10.1592/phco.24.5.427.33358. [DOI] [PubMed] [Google Scholar]
- 3. Academic pharmacy's vital statistics. American Association of Colleges of Pharmacy. 2006. Available at: http://www.aacp.org/Docs/MainNavigation/InstitutionalData/6676_2005-03.pdf.
- 4. American Association of Colleges of Pharmacy. Vacant budgeted and lost faculty positions – Academic year 2004-05. Available at: http://www.aacp.org/Docs/MainNavigation/InstitutionalData/7309_IRBNo6-Facultyvacancies.pdf.
- 5. Personnel Placement Service. Online directory. American Society of Health-System Pharmacists. Available at: http://www.careerpharm.com/.
- 6. American Society of Health-System Pharmacists accreditation standards for residency in pharmacy practice. Available at: http://www.ashp.org/emplibrary/PGY1Standard.pdf.
- 7. American Society of Health-System Pharmacists accreditation standards for residency (PGY2). Available at: http://www.ashp.org/rtp/Word/G&Os_AdvancedPharm.doc.
- 8.The research agenda of the American College of Clinical Pharmacy. Pharmacotherapy. 2007;27:312–24. doi: 10.1592/phco.27.2.312. [DOI] [PubMed] [Google Scholar]
- 9.Carter O, Nathisuwan S, Stoddard GJ, Munger MA. Faculty turnover within academic pharmacy departments. Ann Pharmactother. 2003;37:197–201. doi: 10.1177/106002800303700206. [DOI] [PubMed] [Google Scholar]
- 10.Romanelli F, Smith KM, Brandt BF. Certificate program in teaching for pharmacy residents. Am J Health-Syst Pharm. 2001;58:896–8. doi: 10.1093/ajhp/58.10.896. [DOI] [PubMed] [Google Scholar]
- 11.Romanelli F, Smith KM, Brandt BF. Teaching residents how to teach: A scholarship of teaching and learning certificate program (STLC) for pharmacy residents. Am J Pharm Educ. 2005;(2):69. Article 20. [Google Scholar]
- 12.Selander LK, Bjornson DC. Description of an elective PharmD teaching clerkship. Am J Pharm Educ. 1995;59:273–8. [Google Scholar]
- 13.Hammer DP, Paulsen SM. An innovative clerkship in pharmacy education. Am J Pharm Educ. 2001;65:284–93. [Google Scholar]
- 14.Sylvia LM. An advanced pharmacy practice experience in academia. Am J Pharm Educ. 2006;70 doi: 10.5688/aj700597. Article 97. [DOI] [PMC free article] [PubMed] [Google Scholar]