Abstract
Objectives
This study evaluated the effectiveness of a medication reconciliation program conducted by doctor of pharmacy (PharmD) students during an advanced pharmacy practice experience.
Methods
Patients admitted to medicine or surgery units at 3 hospitals were included. Students were instructed to interview each patient to obtain a medication history, reconcile this list with the medical chart, and identify and solve drug-related problems.
Results
Eleven students reconciled medications for 330 patients over 10 months and identified 922 discrepancies. The median number of discrepancies found per patient was 2, and no discrepancies were found in 25% of the cases. In cases in which discrepancies were identified, a greater number of medications had been prescribed for the patient (7.9 ± 4.0 medications compared to 5.4 ± 3.9 medications; p < 0.05). The students completed 59 interventions. Differences were found in the numbers of discrepancies and drug-related problems that different students at different sites identified (p < 0.05).
Conclusions
Pharmacy students provided a valuable service to 3 community hospitals. The students improved the quality of patient care by identifying and solving significant drug-related problems, identifying drug allergy information, and resolving home and admission medication discrepancies.
Keywords: medication reconciliation, advanced pharmacy practice experience
INTRODUCTION
Colleges and schools of pharmacy are continuously seeking new sites for advanced pharmacy practice experiences (APPEs). The increasing number of colleges of pharmacy, students, and the Accreditation Council for Pharmacy Education (ACPE) requirement for students to complete a hospital or health system pharmacy APPE rotation make placing students in institutional sites challenging.
Identifying a student service that can assist a site in meeting its goal is helpful when striving to maintain or increase site participation in APPEs. One such service is medication reconciliation.
The Joint Commission has included reconciliation of medications across the continuum of care as a 2007 National Patient Safety Goal.1 The JCAHO patient safety goal implementation expectations states, “The organization with the patient's involvement creates a complete list of the patient's current medications at admission/entry.” Literature reports have documented problems with the reconciliation of medications used prior to and at the time of admission. Lau reported that 25% of prescription drugs in use were not recorded in the medical chart and 61% of patients had 1 or more drugs that had not been recorded.2 Only 4.9% of nonprescription drugs taken by patients prior to admission are recorded in the hospital medical chart.3 Eighty-three percent of elderly patients' hospital medication records had at least 1 error and 46% had 3 or more errors.4 A study evaluating the prevalence of medication errors in 36 health care facilities reported that the most frequent errors were in dosing, timing of administration, omission, and unauthorized drug use.5 In a study of unintended medication discrepancies at the time of hospitalization, Cornish reported that “38.6% of the discrepancies had the potential to cause moderate to severe discomfort or clinical deterioration.”6 A study conducted in critical care documented a decrease in medication errors as a result of a medication reconciliation program initiated on admission and discharge from the unit.7 Thus, the requirement for health systems to conduct medication reconciliation provides both a an educational and service opportunity for PharmD students.
At the Albany College of Pharmacy, PharmD students complete five 5-week APPEs in a variety of required and elective settings and a 10-week APPE takes place in an institutional setting. Albany College of Pharmacy is a private institution that offers 2 options for obtaining the PharmD degree: a 0-6 program that follows a traditional academic scheduling year, culminating in a final year of 35 weeks of APPEs; and an accelerated option that allows students to complete the last 4 years of the program in 3 calendar years, with the final year including the 35 weeks of APPEs. The accelerated students typically have an undergraduate or graduate degree in another field of study.
The objective of this study was to evaluate the potential role of PharmD students in conducting patient medication reconciliation in an institutional setting, a valuable service that would potentially benefit the rotation site. This activity would also serve as an educational experience for students in patient interview technique and identifying drug-related problems and medication discrepancies.
METHODS
A study of the medicine reconciliation project was conducted from June 2005 to March 2006. Patients newly admitted to each of the 3 participating hospital study sites served as the study population.
The number of beds at each of the sites was 160 at Bassett Healthcare Cooperstown, 40 at Bassett Hospital-Cobleskill, and 23 at O'Connor Hospital. The approximate number of admissions per day was 25-40 at Bassett Healthcare Cooperstown, 4 at Bassett Hospital-Cobleskill, and 2 at O'Connor Hospital. At the time of this study, the institutions that participated did not have a formal process for the involvement of pharmacy in medication reconciliation. Medication histories were completed by a nurse and/or physician so the student's evaluation/assessment served as a second history. Each of the hospital sites were APPE clerkship sites for the College. The institutional review board at the Albany College of Pharmacy approved the study.
All patients newly admitted to the hospital on a general medicine or general surgery service who were greater than 18 years of age and could be interviewed within 36 hours of admission were included in the study. Exclusion criteria included the following: patient could not speak English or had a language barrier; patient was non-responsive; and patient was admitted to the intensive care, psychiatric or obstetrics unit.
Students assigned to the hospitals for a 10-week institutional APPE participated in the study. During the first week of the APPE, students were trained in the study procedure and patient interview technique by the site investigator (rotation preceptor) and the College's faculty study investigator. The training for obtaining an accurate patient medication history consisted of a required reading on interviewing the patient from Boh's Pharmacy Practice Manual and observation of the first patient interview by the site investigator (rotation preceptor).8 The College faculty member investigator reviewed the study protocol approved by the IRB, data collection forms, and study procedure with each participating student. The students were supplied with a script which outlined a general approach to conducting the patient interview (Appendix 1). Students were given a goal of interviewing at least 5 patients per week, depending on admission and inclusion/exclusion criteria. The student characteristics of age, gender, number of previously completed rotations, grade point average, type of program (accelerated or traditional), and previous hospital experience were recorded.
The students obtained a daily list of newly admitted patients, which was generated in the pharmacy department at each of the sites. The students assessed each patient for inclusion and exclusion criteria prior to initiating the patient interview. Patients agreeing to participate were interviewed by the student on their medication use prior to admission including use of prescription and nonprescription drugs and herbal medications. In addition, they were asked about a history of prior adverse drug reactions and allergies. Students called the patient's community pharmacy on an “as needed” basis to obtain any information (dose, drug name, formulation) the patient was not able to provide during the interview. Following the interview, the student compared the interview medication list with the medication list in the patient's chart and documented discrepancies. Discrepancies were defined as any variation between medications taken prior to admission as recoded by the student and the current list of inpatient medications. Acute care medications such as antibiotics were not included as discrepancies. Vitamins and dietary supplements were categorized as nonprescription drugs and nondietary supplements were categorized as herbal medications. The students reviewed the medication list to identify drug-related problems and then documented the problems along with a proposed solution. All discrepancies, drug-related problems, and proposed solutions were presented to the student's preceptor prior to any intervention. A faculty investigator not involved in the student or preceptor training reviewed all documented drug-related problems for clinical significance using the Hatoum criteria.9 Students documented a chronic diagnosis count for each patient by reviewing the patient's chart for physician admission notes on past and current medical history. Statistix, Version 8 (2003, Analytical Software, Tallahasee, Fla) was used to conduct the statistical analysis. Kruskal-Wallis one-way nonparametric test was used to compare the students and sites in terms of number of discrepancies, drug-related problems identified, site, number of patients interviewed, number of medications per patient, student type (accelerated or traditional program), student age, student grade point average (GPA), and the number of APPEs the student had previously completed. A 2-sample t test and multiple regression analysis were used to evaluate the relationship between number of discrepancies and total medications per patient. The percentage of patients interviewed was calculated by dividing the number of patients interviewed by the total number eligible admissions for the period of the rotation. A p value less than 0.05 was considered significant.
RESULTS
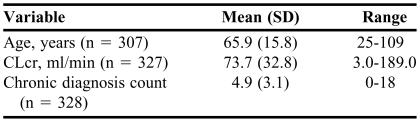
Eleven students interviewed 330 patients. This represented 30% of Bassett Healthcare Cooperstown (40 bed), 13% of Bassett Hospital-Cobleskill (160 bed), and 68% of O'Connor Hospital (23 bed) patient admissions meeting the inclusion criteria. The total number of interviews conducted at Bassett Hospital-Cobleskill was 67; at Bassett Healthcare Cooperstown, 222; and at O'Connor Hospital, 41. The average time to complete the patient interview was 9.3 ± 5.3 minutes (range: 2-35 minutes). The patient demographic data for the study population is summarized in Table 1. New medication allergy information was identified in 15 patients (5%). The average number of medications recorded by patient interview was 7.2 ± 4.1 (range: 0-20). Students contacted the community pharmacist to obtain medication information for 28 patients and 118 medications.
Table 1.
Clinical Variables of Patients Screened by PharmD Students Participating in a Drug Reconciliation Program*
CLcr = creatinine clearance
Students were unable to collect all data from some patients so the n value for each of the variables differs.
A total of 922 medication discrepancies were identified by the students, of which 4% involved herbal medications, 32% involved nonprescription drugs, and 64% involved prescription drugs (range: 0-18 per patient). Medication discrepancies identified during the study included omission of medication (prescription and nonprescription drugs), different doses, therapeutic substitution of one medication for a similar medication from the same class, change of drug from prescription to nonprescription (most often pain medication), and change from a combination product to a single agent. The mean number of discrepancies identified per patient was 2.8 ± 3.1. The median number of discrepancies identified per patient was 2 and 25% of patients had no identified discrepancies. The patients with medication discrepancies had a greater number of medications compared with those without discrepancies (7.86 ± 3.96 medications vs. 5.44 ± 3.87 medications; p < 0.05). There was a significant relationship between the number of discrepancies identified and the total number of medications prescribed for a patient (p < 0.05), with a higher number of discrepancies found among patients taking 6 or more medications.
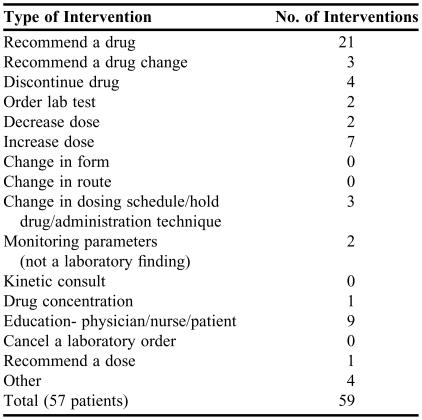
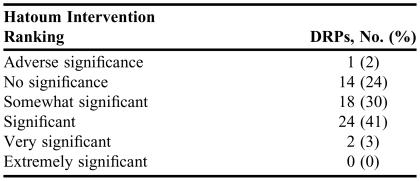
Students identified and provided a recommendation and intervention for a total of 59 drug-related problems for 57 patients (17%) during the course of the study. The types of drug-related problems that were identified are summarized in Table 2. Table 3 lists the intervention ranking for each of the identified and solved drug-related problem according to the definition of Hatoum.9 Seventy-five percent of the completed intervention recommendations were considered significant according to the Hatoum criteria. Forty-eight percent of the interventions were accepted and/or completed by the hospital/patient care team.
Table 2.
Summary of Drug-Related Problem Interventions Conducted by 11 PharmD Students Participating in a Medication Reconciliation Project
Table 3.
Hatoum Intervention Ranking for Drug-related Problems Identified by PharmD Students Participating in a Medication Reconciliation Project (N = 59)*
Hatoum AT, Hutchinson RA, Witte KW, Newby G.P. Evaluation of the contribution of clinical pharmacists: Inpatient care and cost reduction. Drug Intelligence and Clinical Pharmacy. 1988;22:252-9
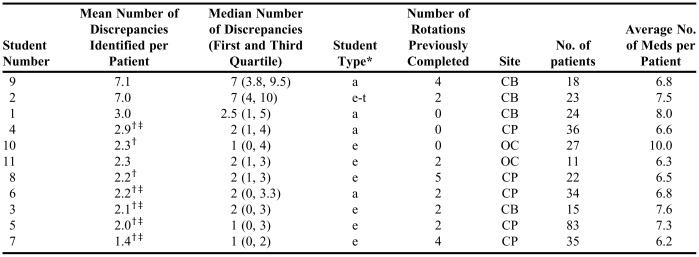
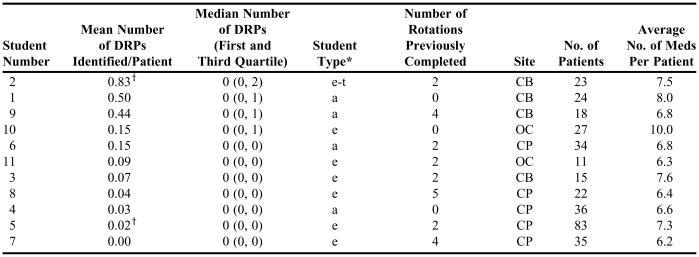
There were significant differences (p < 0.05) between the students in the number of discrepancies and drug-related problems identified (Tables 4 and 5). Students 2 and 5 were significantly different in terms of the number of drug-related problems each identified. There were no differences identified among the other students in terms of number of drug-related problems identified. There were significant differences in the number of discrepancies identified by students 2 and 9 and the majority of the other students. Students 2 and 9 each identified the largest mean number of discrepancies identified per patient. There were no significant differences between the students in terms of number of previously completed advanced practice rotations, GPA, student age, number of patients interviewed, or number of medications per patient. Only student 5 reported previous work history in the institutional practice setting. There was a significant difference (p < 0.05) between the sites in drug-related problems and discrepancies identified. The Bassett Hospital-Cobleskill site was significantly different compared to both O'Connor Hospital and Bassett Healthcare Cooperstown in terms of the number of discrepancies identified by students. The Bassett Hospital-Cobleskill site was significantly different compared to the Bassett Healthcare Cooperstown site in terms of number of drug-related problems identified by students.
Table 4.
Number and Type of Medication Discrepancies Identified by PharmD Students Participating in a Medication Reconciliation Project
*Student type: e = traditional student; e-t = transfer traditional student; a= accelerated student
†Statistical differences compared to student 2 (p < 0.05)
‡Statistical differences compared to student 9 (p < 0.05)
CB = Bassett Hospital-Cobleskill; OC = O'Connor Hospital; CP = Bassett Healthcare Cooperstown
Table 5.
Number and Type of Drug-Related Problems Identified by PharmD Students Participating in a Medication Reconciliation Project
*Student type: e = traditional student; e-t = transfer traditional student, a = accelerated student
†Statistical Difference (p < 0.05)
DPRs=drug-related problems; meds = medications; CB = Bassett Hospital-Cobleskill; OC = O'Connor Hospital; CP = Bassett Healthcare Cooperstown
Two of the submitted patient data forms were completely excluded form the analysis: one because the patient was nonresponsive and the student had to interview the family to get the medication history, and the other because the patient was discharged early and the student was unable to complete the data collection. Twenty-three of the data collection forms did not have a patient age, 3 did not have a creatinine clearance value, and 2 did not have a list of chronic diseases. These forms were included in the analysis since these data were used as descriptive statistics.
DISCUSSION
The students provided a valuable site service during the course of this study and advanced their pharmacy knowledge by identifying medication discrepancies, contacting community pharmacists to clarify medication histories, solving drug-related problems, and obtaining additional medication allergy information for newly admitted patients. The mean and median number of admission discrepancies identified per patient were 2.8 and 2, respectively, and 25% of patients had no discrepancies. The majority of identified discrepancies involved prescription products. Our definition of discrepancy included therapeutic substitution. We included this as a discrepancy since it may lead to drug-related problems upon discharge due to duplicate therapy. Rodehaver reported a case of a patient switched to a hospital formulary statin product on admission who experienced readmission secondary to rhabdomyolysis due to inadvertent duplicate therapy upon discharge.10 The students were effective at obtaining medication and allergy histories for patients admitted to the medicine or surgical service. Nester reported on the effectiveness of pharmacists and pharmacy students in identifying problems in patient's self reported medication and allergy history.11 Our study confirmed this finding with the large number of discrepancies that were identified by the students.
Gleason studied hospital admission medication reconciliation conducted by pharmacists and PharmD students.12 This study reported a mean number of discrepancies per patient of 1.2 ± 1.5 and 45% with no discrepancy, compared with our report of 2.8 and 25%. Some of this difference may be due to our requirement that the students interview the patients within 36 hours of admission while the timeframe for the Gleason study was 24-48 hours. The longer timeframe may have allowed for more complete admission orders. Lessard reported on admission medication discrepancies for 63 senior patients.13 This study was conducted by pharmacists and PharmD students and reported that 35% of patients had no discrepancy and 1.5 ± 1.6 discrepancies per patient. The Lessard study had medication histories obtained within 24 hours of admission and did not include therapeutic substitution.
Our study confirmed the result of a correlation between number of admission medications and discrepancies. Gleason reported that in cases where discrepancies were found, a significantly higher number of medications had been prescribed for the patient compared to cases in which no discrepancies were found (8.2 versus 6.6, which is comparable to our reported finding of 7.8 versus 5.4).12 Our study identified the presence of greater than 6 medications as a significant indicator for a medication discrepancy. This finding may be of use in identifying those patients at greatest risk when only a limited number of pharmacy students are available to provide medication reconciliation.
The students identified a total of 59 drug-related problems in 57 patients. This represented 17% of the total number of patients interviewed. A limitation of the study was the lack of information collected on the classification of the discrepancy as intended or unintended. This may explain the small number of drug-related problem interventions, since students did not intervene on intended discrepancies. The low acceptance rate of 48% was influenced by the lack of time to solve drug-related problems due to rapid discharge of patients secondary to short length of stay, and failure to communicate the discharge date and time to the student Anderson reported 242 drug-related problem interventions made by 29 PharmD students in the community pharmacy setting and ranked them for significance utilizing the Hatoum definition.14 The percentage of interventions ranked as somewhat significant, significant, or very significant was 88% in that study compared to 75% reported in our study. Our study had a higher percentage of significant interventions (41% versus 30%).
A medication reconciliation service is one that must be provided on a regular basis. The utilization of students completing an APPE for this service is often questioned by site preceptors because the students will change often or may not be on site over the course of the entire year. Our study objective was to identify a potential role for students to provide this service. Our data documented a significant difference among the students in terms of number of discrepancies and drug-related problems identified per patient. Student 2 and student 9 were significantly different from a number of the other students in terms of identifying medication discrepancies. Interestingly, these students were both assigned to the Bassett Hospital-Cobleskill site. Although there were differences among the students there were also differences among the sites. Bassett Hospital-Cobleskill was significantly different from the other sites in terms of medication discrepancy identification. Only student 2 and student 5 were significantly different from one another in terms of the number of drug-related problems identified. One of these students was assigned to the Bassett Hospital-Cobleskill site and one was assigned to the Bassett Healthcare Cooperstown site. Similar to medication discrepancies, the Bassett Hospital-Cobleskill site was significantly different from Bassett Healthcare Cooperstown in terms of drug-related problems identified. The data indicate that there were differences between the students related to the service tasks, but there were also differences between the sites. Interestingly, the number of previous APPEs completed, age, and GPA did not differ among the students in terms of number of discrepancies and drug-related problems identified. The training received by each of the students was identical at the start of the APPE. The institutional pharmacy practice APPE at Albany College of Pharmacy is set up with a checklist of required activities. At the time of this study, the medication reconciliation activity described in this study was not listed as a required rotation activity. This is a study limitation. It may be that the differences found among the students were related to the time dedicated to the study activity at each of the sites. The site differences may also be the result of the effectiveness of the medication reconciliation process in place at the time of the study. In all 3 sites, the nurse or physician had already conducted the admission interview and the student conducted a second interview.
CONCLUSIONS
Our study demonstrated that PharmD students can provide the valuable service of medication reconciliation for rotation sites. The students added to patient care by identifying and solving significant drug-related problems, identifying drug allergy information, and resolving home and admission medication discrepancies. Participation in the activity provided the students with the opportunity to interview patients in the institutional setting and interact with providers regarding medication discrepancies. There were significant differences in the number of discrepancies and drug-related problems identified among the students and the practice sites.
ACKNOWLEDGMENT
The authors would like to thank the following PharmD candidates for their contribution to the research: Eileen Zuefle, Melissa Witkowski, Amy Langlois, Alison Wilson, Travis Wisniewski, James DeFoe, Evangelo Diamantopoulos, Julie Stark, Lea Becker, Carly Harder, Jason Lafayette.
Appendix 1. Outline for patient interviews conducted by pharmd students participating in a medication reconciliation project
Introduction to Interview
Hello, my name is ____________________ . I am a student at the Albany College of Pharmacy. I am working on a study with the _____________Hospital's Director of Pharmacy , _____________________ and Albany College of Pharmacy, to learn about the medicines people take at home prior to coming to the hospital. Would it be alright with you if I spent about 15 minutes to talk with you to learn about the medicines you take at home, allergies you may have to certain medicines and about your past experiences with medicines?
(Wait a few seconds for the patient to answer?)
Do you have any questions?
Conclusion of Interview
Thank you for taking the time to talk with me about your medicines.
REFERENCES
- 1. Joint Commission on Accreditation of Healthcare Organizations. 2005 Hospitals' National Patient Safety Goals. Available at: http://www.jcaho.org/. Accessed March 15, 2007.
- 2.Lau HS, Florax C, Porsius AJ, Boer A. The completeness of medication histories in hospital medical records of patients admitted to general medicine wards. Br J Clin Pharmacol. 2000;49:597–603. doi: 10.1046/j.1365-2125.2000.00204.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Oborne CA, Luzac ML. Over the counter medicine use prior to and during hospitalization. Pharmacotherapy. 2005;39:268–73. doi: 10.1345/aph.1D160. [DOI] [PubMed] [Google Scholar]
- 4.Beers MH, Munekata M, Storrie M. The accuracy of medication histories in the hospital medical records of elderly persons. J Am Geriatr Soc. 1990;38:1183–7. doi: 10.1111/j.1532-5415.1990.tb01496.x. [DOI] [PubMed] [Google Scholar]
- 5.Barker KN, Flynn EA, Pepper GA, Bates DW, Mikeal RL. Medication errors observed in 36 health facilities. Arch Intern Med. 2002;162:1897–903. doi: 10.1001/archinte.162.16.1897. [DOI] [PubMed] [Google Scholar]
- 6.Cornish PN, Knowles SR, Marchesano R, Tam V, Shadowitz S, Juurlink J, Etchells EE. Unintended medication discrepancies at the time of hospital admission. Arch Intern Med. 2005;165:424–9. doi: 10.1001/archinte.165.4.424. [DOI] [PubMed] [Google Scholar]
- 7.Pronovost P, Weast B, Schwarz M, et al. Medication reconciliation: a practical tool to reduce the risk of medication errors. J Crit Care. 2003;18(4):201–5. doi: 10.1016/j.jcrc.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 8.O'Sullivan TA, Wittkowsky AK. Clinical drug monitoring- interviewing the patient. In: Boh EL, Young YL, editors. Pharmacy Practice Manual 2nd ed. Maryland: Lippincott Williams and Wilkins; 2001. pp. 581–7. [Google Scholar]
- 9.Hatoum AT, Hutchinson RA, Witte KW, Newby GP. Evaluation of the contribution of clinical pharmacists: Inpatient care and cost reduction. Drug Intell Clin Pharm. 1988;22:252–9. doi: 10.1177/106002808802200318. [DOI] [PubMed] [Google Scholar]
- 10.Rodehaver C, Fearing D. Medication reconciliation in acute care: ensuring an accurate drug regimen on admission and discharge. Joint Commission J Quality Patient Safety. 2005;July 31(7):406–13. doi: 10.1016/s1553-7250(05)31054-3. [DOI] [PubMed] [Google Scholar]
- 11.Nester TM, Hale LS. Effectiveness of a pharmacist acquired medication history in promoting patient safety. Am J Health-Syst Pharm. 2002;59:2221–5. doi: 10.1093/ajhp/59.22.2221. [DOI] [PubMed] [Google Scholar]
- 12.Gleason KM, Groszek JM, Sullivan C, Rooney D, Barnard C, Noskin GA. Reconciliation of discrepancies in medication histories and admission orders of newly hospitalized patients. Am J Health-Syst Pharm. 2004;61:1689–95. doi: 10.1093/ajhp/61.16.1689. [DOI] [PubMed] [Google Scholar]
- 13.Lessard S, DeYoung J, Vazzana N. Medication discrepancies affecting senior patients at hospital admission. Am J Health- Syst Pharm. 2006;63:740–3. doi: 10.2146/ajhp050291. [DOI] [PubMed] [Google Scholar]
- 14.Anderson RJ, Nykamp D, Miyhara RK. Documentation of pharmaceutical care activities in community pharmacies by doctor of pharmacy students. J Pharm Pract. 1995:83–8. [Google Scholar]