Short abstract
The BMI is the best available tool for monitoring progress in the campaign against obesity
Keywords: body mass index, children, obesity, overweight, screening
The House of Commons Select Committee on obesity, and two expert groups in the USA, recommend that the body mass index (BMI) of every school child should be measured each year and the result sent home to the parents. The BMI correlates sufficiently well with direct measures of total body fat to support its use, on an anonymous basis, as a public health tool for monitoring progress in dealing with the obesity epidemic. However, the BMI is an imperfect proxy for obesity because there is much individual variability in the relationship between BMI and body fat, cardiovascular risk factors, and long term health outcomes. Whatever BMI cut offs are selected for determining the advice to parents, a high BMI calls for further evaluation and interpretation and the policy proposed by the Select Committee, to send BMI results to parents, is therefore in effect a screening programme. As such, it presents a number of difficulties and should be implemented only as a research study and not as public policy.
The worldwide epidemic of childhood obesity is a public health problem for two reasons. First, it is associated with a variety of adverse health outcomes, including type 2 diabetes and cardiovascular disease. Second, it is perceived in the Western world as unattractive and for many individuals it is, therefore, the cause of much unhappiness. The UK Government has set a target of “halting the rise” in childhood obesity by 2010.1 Concerns about obesity have generated much interest in the body mass index (BMI) as a convenient indicator of body fat and the House of Commons Select Committee on Health2 recommended that:
… throughout their time at school, children should have their Body Mass Index measured annually at school … The results should be sent home in confidence to their parents, together with, where appropriate, advice on lifestyle, follow‐up, and referral to more specialised services … Not only would this system identify children who are already overweight or obese, but it could target those at the top end of the ‘normal' range of BMI to prevent further weight gain.
A USA expert group3 stated that:
Pediatricians … and other clinicians should … routinely track body mass index, and offer relevant evidence‐based counseling and guidance.
The American Academy of Pediatrics4 advised paediatricians to:
Calculate and plot BMI once a year in all children and adolescents … and use change in BMI to identify rate of excessive weight gain relative to linear growth.
In order to implement this advice, decisions have to be made as to what measurement or change in BMI should trigger advice or referral and what investigations and/or interventions should be offered. In this paper, we will argue that the BMI is an essential public health tool for monitoring progress towards the government target, but that its routine use in the ways recommended in these three reports presents a number of difficulties. The use of the BMI in the clinical management of obese children has been discussed elsewhere5 and is not addressed here.
Origins of the BMI
The index weight/height2 was first described by Adolphe Quetelet in the 19th century as an index of weight adjusted for height. Ancel Keys reinvented it in the 1950s and called it the body mass index. Cole first proposed its use in children in 1979, showing that it adjusted weight for both height and age.6 The index weight/height3 adjusts better for height during puberty,7 but the BMI correlates better than this and other related indices with measures of body fat mass (FM).8,9
In the UK, centile charts for BMI are derived from the data used to generate the 1990 growth charts (the “nine centile” charts).10 As children and adolescents are becoming heavier year on year, the BMI charts would need to be updated regularly if the aim was simply to describe the current BMI distribution. This would, however, conceal any population trend and it has therefore been agreed to “freeze” the charts at the position shown on the 1990 charts, so that trends in BMI can be related to that fixed baseline.11
Definitions
There are many definitions of childhood overweight and obesity. Each involves a measure of fatness (usually BMI, but other weight‐for‐height indices are also used12) and a reference centile chart where selected centiles define cut offs for overweight and obesity. As different countries have developed their own BMI charts, and have also selected different centiles for the cut offs, this has led to a plethora of definitions. For example, in the USA overweight and obesity are defined as BMI exceeding the 85th and 95th centiles of the US CDC 2000 reference, while in the UK the definitions use the 91st and 98th centiles of the British 1990 reference. The International Obesity Taskforce (IOTF) definition pooled data from six international BMI references and set the centile cut offs to ensure that at age 18 they matched the adult cut offs of 25 and 30 kg/m2.
Centile based definitions indicate what percentage of the reference population would be “screened in”, for example 9% above the 91st centile (although the continuing rise in obesity means that many more than 9% of children are now above the 91st centile of the UK 1990 reference). The IOTF definition by contrast gives a prevalence rate which is linked to the corresponding adult rate. The IOTF cut offs correspond roughly to the UK 90th and 99th BMI centiles, so the prevalence of IOTF overweight is fairly similar to that for other definitions, whereas the IOTF obesity prevalence rate is much lower.
Does it matter which definition is preferred? The decision does not affect the clinician's management of severely obese children. Data for public health reports can be presented using any or all of the various definitions and comparisons can be made with national and international data, so long as the same cut offs are used consistently. If however the aim is to identify within the whole population a group of children who are at increased risk of obesity and its complications, as proposed by the Select Committee, the choice of definition matters a great deal, because it will affect the advice given, the cost, and the potential benefits and/or harms of the whole exercise.
What does BMI measure?
BMI is currently the best available anthropometric estimate of fatness for public health purposes. The validity of anthropometric data as a proxy for body fat is assessed by direct measurement. There are two main approaches: physicochemical methods and imaging. The first of these measures the amount of body water, by dilution using deuterium oxide, or electrically using bioelectrical impedance or total body electrical conductivity. Imaging using CT or, more recently, MR, can provide precise and reliable measures of FM and lean body or fat free mass (FFM) both overall and in various body compartments. These studies show that BMI has limitations as a measure of the fatness of individual children because:
Body composition, that is the ratio between FFM and FM, varies according to age and gender. There are also significant ethnic differences, for example, between Singaporean, Chinese, Dutch, and American Black children.13,14
Body composition can change while weight and therefore BMI stay the same. For example, dieting and physical exercise fitness training could reduce FM and increase muscle mass.15
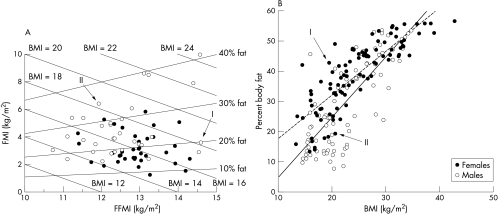
BMI and FM are strongly correlated, but not strongly enough to make useful deductions in individuals. Figure 1A,B16,17,18 illustrates the wide variation in body fat that can occur in subjects with the same BMI.
The extent of the health risks does not relate solely to total FM and is more closely correlated with intra‐abdominal or visceral fat mass (VFM)19 which influences metabolic activity in the liver via the portal venous system. However, neither BMI nor FM correlate well with VFM or with cardiovascular risk factors.20,21,22
Figure 1 Illustrations from two studies of the variability between individuals in the relationship of BMI to body fat. (A) BMI is made up of two components, the fat mass index (FMI) and the fat‐free or lean mass index (FFMI). On this chart, the FFMI (FFM/height2) is plotted on the x axis and the FMI (FM/height2) on the y axis. The sloping lines labelled “BMI = 18, 20” etc. represent points of equal BMI, for example, a BMI of 18 could be made up of an FMI of 6 and an FFMI of 12 or an FMI of 4 and an FFMI of 14. The lines labelled for the value for percentage body fat similarly link points of identical percentage body fat. Each data point represents one child. Note that subjects I and II both have a BMI of 18, between the 75th and 91st centiles for their age, but FMI of II is equivalent to 35% body fat whereas that of I is around 20%. (Reproduced with modification by permission of the author JCK Wells and The Proceedings of the Nutrition Society) (B) BMI is shown on the x axis and percent body fat on the y axis. The regression line is dotted for girls and solid for boys. The filled circles represent girls and the open circles boys. Each data point represents one child. Although there is a close correlation between BMI and percent body fat, there is wide individual variation. For example, child I has approximately twice the percent body fat of child II but they have a similar BMI. (Reproduced with modification by permission of Pietrobelli et al and The Journal of Pediatrics)
The ideal definitions of obesity and overweight would be based either on a close correlation with indicators of future cardiovascular and metabolic disease or on their ability to predict adverse future health outcomes. When considering a whole population, BMI performs moderately well as a proxy for these indicators, particularly at the upper end of the distribution curve, but there is wide variation among individuals. This means that, if BMI is used to identify children at risk, it is in effect a screening test; whatever statistical cut‐off points are chosen, they are inherently arbitrary and must be followed up by a more detailed evaluation to assess risk and plan intervention.
Monitoring BMI in populations
Data gathered over many years in the UK23 and throughout the world show that BMI is increasing, and it is reasonable to conclude that child and adolescent populations are getting fatter. The increase in BMI probably underestimates the rise in VFM.24,25
Changes over time in the prevalence of overweight and obesity in a population could be monitored in all children and young people, or by sampling. The height and weight data would be anonymised, entered in a database, and converted to BMI, analysed (including classification by social class using post code), and compared with results of previous years. Although quite large errors, particularly in height,26 are likely when very large numbers of children are weighed and measured by many different observers, these are likely to be random rather than systematic and should not invalidate the data. A potentially more troublesome source of error would arise if some children, particularly those who are already overweight or obese, opt out. Sensitive handling of anxious children could perhaps reduce this risk, but children must not be measured and weighed against their will.
Rudolf et al have shown that, in order to demonstrate that the target of “halting the rise” in obesity had been achieved, samples of between several hundred and several thousand would be needed, depending on which definition is adopted.27 The impact of interventions would, therefore, have to be dramatic in order to be demonstrable with reasonable statistical confidence at the level of small communities such as primary schools. The use of more extreme cut offs such as the 99.6th centile would be very susceptible to sampling variation in samples of this size, and could result in dramatic fluctuations in the rate of obesity from year to year.
An alternative approach would be to monitor mean BMI, expressed as the mean SD score adjusted for age and sex, rather than rates of overweight and obesity. This reflects the whole population, not just the fattest children, and is better at detecting small changes in fatness over time as it is based on larger numbers. It does, however, include a proportion of thin children who are not of concern, and their inclusion blunts mean BMI as an indicator.
Sampling from across the country could give a reasonable snapshot of overall progress in tackling obesity, but measuring all children would probably be more useful in formulating and monitoring local public health policy. It would not be necessary to measure every child every year as trend data could be obtained by measuring each child's BMI on two or three occasions during their school career.
Using BMI measurements for identifying and advising individual children
The Select Committee advocated that regular BMI measurements could be used to identify individual children who are at risk of becoming obese. The process would involve several steps:
Defining one or more cut‐off points on the BMI chart which would determine the advice included in a communication to parents.
Defining what annual changes in BMI would determine that advice. This is more difficult because at least 5% of children are likely to change BMI by at least one centile channel width (0.67 SDS) up or down each year28 (based on year‐on‐year r = 0.94, SD of change = √2(1−r)). If children were to be measured each year, many parents would be informed at least once that their child was at increased (or decreased) risk of overweight or obesity.
Suitable software could generate a standardised report for parents on the significance of their child's BMI, taking into account age, gender, changes in BMI from previous measures, the possible margin of error, and ideally also ethnicity and stage of puberty.29 Parents would need instructions as to where and from whom to seek further professional advice. This report should preferably be in the parents' own language. The magnitude of the task and the cost of setting up such a system and maintaining quality should not be underestimated.
Which cut‐off points should be used?
The choice depends on defining the aims. If the aim is only to identify the most severely obese, the cut off could be set at the 98th or 99.6th centile. Most such children identified by this cut off would probably be aware of their obesity and would be candidates for intervention. There would be little risk of over‐including children who were not in fact at risk of significant obesity.
Parents probably recognise extreme degrees of obesity but many parents are not aware that their child is overweight,30 so it could be helpful to identify children who are at risk of becoming overweight or obese, at a stage when intervention might be easier. In order to achieve this the cut off would need to be set at the 85th or 90th centile. A large number of parents (at least 25% of the current population) would need an interpretation of their child's BMI and assessment of their child's health risks. It would be important to stress the need for lifestyle changes while not causing unnecessary anxiety, for example by exaggerating the risks of future obesity and cardiovascular disease.31,32
What interventions would be offered?
Whole‐school and whole‐community approaches to issues of diet and exercise are not easy, and even well funded intensive programmes have yielded only modest improvement.33 Nevertheless, this approach is probably the best way of tackling the obesity epidemic.34,35 Rudolf's data show that it will be difficult to detect a meaningful reduction in BMI measures at the level of individual schools; indeed, a rise could easily occur by chance alone and unless staff are aware of this risk it could demoralise a school that was actually running a good programme.
The interventions offered to individual children identified as being above defined BMI cut‐off points are more problematic. Experience in specialist obesity clinics shows that even those obese children who are highly motivated and well supported by their families have great difficulty in controlling their weight. There is no reason to think that obese children newly identified in schools by BMI measurements above the 98th or 99.6th centile are likely to be any more successful, and the same applies to children in the much larger group identified as being above the 85th or 90th centile.
Conclusion
The BMI is the best available tool for monitoring progress in the campaign against obesity. Notwithstanding the pitfalls outlined above, a robust quality assured anonymised data collection and analysis system could provide national and local data that would inform the planning and evaluation of intervention programmes.
The use of BMI in the way proposed by the Select Committee and the USA Expert Reports presents significant challenges and gives rise to several unsubstantiated hypotheses, for example:
That feedback of BMI results to all parents would result in lifestyle changes and a fall in mean BMI across the whole population of school children.
That the use of cut offs to identify children whose BMI exceeds specified levels would result in more overweight and/or obese children taking effective steps to control their weight.
That the benefits of any such programme would substantially exceed any harms.
That sufficient professional expertise can be made available to manage the inevitable increase in referrals for obesity assessment and weight control.
These hypotheses could be tested in a research programme, subjected to the usual scientific, ethical, and governance controls.
Acknowledgements
We thank the referees for constructive comments and suggestions.
Abbreviations
BMI - body mass index
FFM - fat free mass
FFMI - fat‐free mass index
FM - fat mass
FMI - fat mass index
IOTF - International Obesity Taskforce
VFM - visceral fat mass
Footnotes
Research at the UCL Institute of Child Health and Great Ormond Street Hospital for Children NHS Trust benefits from R&D funding received from the NHS Executive
Competing interests: none declared
References
- 1.Department for Education and Skills and Department of Health National service framework for children, young people and maternity services—core standards. London: DfES and DH, 200447
- 2.House of Commons: Health Committee Obesity: third report of session 2003–04. Vol I. London: The Stationery Office, 2004 (paragraphs 368 and 369,
- 3.Koplan J P, Liverman C T, Kraak V A, eds, Committee on Prevention of Obesity in Children and Youth Preventing childhood obesity: health in the balance. Recommendation 8. Washington, DC, The National Academies Press, 2005 ( http://www.nap.edu/catalog/11015.html, accessed 4th Jan 2006) [PubMed]
- 4.Committee on Nutrition of the American Academy of Pediatrics Prevention of pediatric overweight and obesity. Pediatrics 2003112424–430. [DOI] [PubMed] [Google Scholar]
- 5.Cole T J, Faith M S, Pietrobelli A.et al What is the best measure of adiposity change in growing children: BMI, BMI %, BMI z‐score or BMI centile? Eur J Clin Nutr 200559419–425. [DOI] [PubMed] [Google Scholar]
- 6.Cole T J. A method for assessing age‐standardized weight‐for‐height in children seen cross‐sectionally. Ann Hum Biol 19796249–268. [DOI] [PubMed] [Google Scholar]
- 7.Cole T J. Weight/heightp compared to weight/height2 for assessing adiposity in childhood: influence of age and bone age on p during puberty. Ann Hum Biol 198613433–451. [DOI] [PubMed] [Google Scholar]
- 8.Freedman D S, Thornton J C, Mei Z.et al Height and adiposity among children. Obes Res 200412846–853. [DOI] [PubMed] [Google Scholar]
- 9.Freedman D S, Khan L K, Serdula M K.et al Inter‐relationships among childhood BMI, childhood height, and adult obesity: the Bogalusa Heart Study. Int J Obes Relat Metab Disord 20042810–16. [DOI] [PubMed] [Google Scholar]
- 10.Cole T J, Freeman J V, Preece M A. Body mass index reference curves for the UK, 1990. Arch Dis Child 19957325–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Preece M, Cole T, Fry T. Body mass index standards for children. 1990 data will remain available. BMJ 1999319122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chinn S, Rona R J, Gulliford M C.et al Weight‐for‐height in children aged 4–12 years. A new index compared to the normalized body mass index. Eur J Clin Nutr 199246489–500. [PubMed] [Google Scholar]
- 13.Deurenberg P, Yap M, van Staveren W A. Body mass index and percent body fat: a meta analysis among different ethnic groups. Int J Obes Relat Metab Disord 1998221164–1171. [DOI] [PubMed] [Google Scholar]
- 14.Yajnik C S, Yudkin J S. The Y‐Y paradox. Lancet 2004363163. [DOI] [PubMed] [Google Scholar]
- 15.Barbeau P, Gutin B, Litaker M.et al Correlates of individual differences in body‐composition changes resulting from physical training in obese children. Am J Clin Nutr 199969705–711. [DOI] [PubMed] [Google Scholar]
- 16.Wells J C K. A Hattori chart analysis of body mass index in infants and children. Int J Obes Relat Metab Disord 200024325–329. [DOI] [PubMed] [Google Scholar]
- 17.Wells J C. Body composition in childhood: effects of normal growth and disease. Proc Nutr Soc 200362521–528. [DOI] [PubMed] [Google Scholar]
- 18.Pietrobelli A, Faith M S, Allison D B.et al Body mass index as a measure of adiposity among children and adolescents: a validation study. J Pediatr 1998132204–210. [DOI] [PubMed] [Google Scholar]
- 19.Owens S, Gutin B, Ferguson M.et al Visceral adipose tissue and cardiovascular risk factors in obese children. J Pediatr 199813341–45. [DOI] [PubMed] [Google Scholar]
- 20.Savva S C, Tornaritis M, Savva M E.et al Waist circumference and waist‐to‐height ratio are better predictors of cardiovascular disease risk factors in children than body mass index. Int J Obes Relat Metab Disord 2000241453–1458. [DOI] [PubMed] [Google Scholar]
- 21.Goran M I, Nagy T R, Treuth M S.et al Visceral fat in white and African American prepubertal children. Am J Clin Nutr 1997651703–1708. [DOI] [PubMed] [Google Scholar]
- 22.Owens S, Gutin B, Ferguson M.et al Visceral adipose tissue and cardiovascular risk factors in obese children. J Pediatr 199813341–45. [DOI] [PubMed] [Google Scholar]
- 23.Rudolf M C, Sahota P, Barth J H.et al Increasing prevalence of obesity in primary school children: cohort study. BMJ 20013221094–1095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McCarthy H D, Ellis S M, Cole T J. Dramatic increases in central overweight and obesity in British children aged 11–16 years: cross‐sectional surveys of waist circumference. BMJ 2003326624–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moreno L A, Sarría A, Fleta J.et al Secular trends in waist circumference in Spanish adolescents, 1995 to 2000–02. Arch Dis Child 200590818–819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hall D M B. Growth monitoring. Arch Dis Child 20008210–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rudolf M, Levine R, Feltbower R.et al The TRENDS project: development of a methodology to reliably monitor the obesity epidemic in childhood. Arch Dis Child 200691309–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cole T J. Growth monitoring with the British 1990 growth reference. Arch Dis Child 19977647–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fu W P, Lee H C, Ng C J.et al Screening for childhood obesity: international vs population‐specific definitions. Which is more appropriate? Int J Obes Relat Metab Disord 2003271121–1126. [DOI] [PubMed] [Google Scholar]
- 30.Carnell S, Edwards C, Croker H.et al Parental perceptions of overweight in 3–5 y olds. Int J Obesity 200529353–355. [DOI] [PubMed] [Google Scholar]
- 31.Reilly J R, Armstrong J, Ahmad R.et al Early life risk factors for obesity in childhood: cohort study. BMJ 20053301357–1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Viner R M, Cole T J. Adult socioeconomic, educational, social, and psychological outcomes of childhood obesity: a national birth cohort study BMJ20053301354–1357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gortmaker S L, Peterson K, Wiecha J.et al Reducing obesity via a school‐based interdisciplinary intervention among youth. Planet Health. Arch Pediatr Adolesc Med 1999153409–418. [DOI] [PubMed] [Google Scholar]
- 34.Sahota P, Rudolf M C, Dixey R.et al Evaluation of implementation and effect of primary school based intervention to reduce risk factors for obesity. BMJ 20013231027–1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sahota P, Rudolf M C, Dixey R.et al Randomised controlled trial of primary school based intervention to reduce risk factors for obesity. BMJ 20013231029–1032. [DOI] [PMC free article] [PubMed] [Google Scholar]