Abstract
A prospective study of 246 patients who received multimodal intraoperative monitoring during cervical spine surgery between March 2000 and December 2005. To determine the sensitivity and specificity of MIOM techniques used to monitor spinal cord and nerve root function during cervical spine surgery. It is appreciated that complication rate of cervical spine surgery is low, however, there is a significant risk of neurological injury. The combination of monitoring of ascending and descending pathways may provide more sensitive and specific results giving immediate feedback information and/or alert regarding any neurological changes during the operation to the surgeon. Intraoperative somatosensory spinal and cerebral evoked potentials combined with continuous EMG and motor-evoked potentials of the spinal cord and muscles were evaluated and compared with postoperative clinical neurological changes. A total of 246 consecutive patients with cervical pathologies, majority spinal stenosis due to degenerative changes of cervical spine were monitored by means of MIOM during the surgical procedure. About 232 patients presented true negative while 2 patients false negative responses. About ten patients presented true positive responses where neurological deficit after the operation was predicted and two patients presented false positive findings. The sensitivity of MIOM applied during cervical spine procedure (anterior and/or posterior) was 83.3% and specificity of 99.2%. MIOM is an effective method of monitoring the spinal cord functional integrity during cervical spine surgery and can help to reduce the risk of neurological deficit by alerting the surgeon when monitoring changes are observed.
Keywords: Cervical spine surgery, Intraoperative monitoring, Sensitivity, Specificity
Introduction
Anterior cervical discectomy followed by fusion is a safe procedure with low rate of neurological complication. Intraoperative SEP monitoring is not helpful when performing routine anterior cervical discectomy and fusion [11]. In a mixed population of patients with radiculopathy due to cervical disc herniation, myelopathy, tumors and traumatic dislocation of vertebras a potential utility of intraoperative SEPs and the transcranially elicited MEPs for detection changes in spinal cord functional integrity during anterior cervical fusion has been illustrated [1]. In 6 out of 119 patients operated anteriorly on the cervical spine based upon the monitoring results, true positive findings for neurophysiological alerts that prompted surgeon’s and/or anaesthesiologist’s intervention. Two alerts were related to sudden decreases in blood pressure, two as a result of hyperextension of the neck and one observed as a result of arm positioning during surgery. One alert occurred during single-level discectomy and five occurred during multilevel decompression.
Epstein [3] established the efficacy of SEP monitoring for more complex cervical spine surgery comparing in a historical study 218 unmonitored with 100 monitored patients. In the unmonitored group 8 patients (5%) became quadriplegic and 1 patient died. In the monitored group no quadriplegia or death occurred. The incidence of postoperative radicular deficit was not different between the groups.
Epstein’s observations document the potential high risk of neurological deficit including quadriplegia during complex surgical procedures. A recent report by Khan [5] analyzed 508 patients where SEP monitorings were performed during cervical spine corpectomy. The overall incidence of new postoperative neurological deficit in this series was 2.4%, About 11 with nerve root injury, and 1 with quadriplegia. The calculated sensitivity and specificity of intraoperative SEP monitoring for detecting impending or resultant intraoperative iatrogenic neurologic injury were 77 and 100%, respectively. From the nerve root injuries the C5 injury was the most common. In a prospective cohort study 161 patients with anterior surgery were monitored including in 116 procedures continuous C5 EMG from the deltoid muscle. In cases in which spontaneous C5 activity occurred an appropriate change in operative procedure was made. A historical control group consisted of retrospective review of 55 procedures that were monitored using conventional SEP techniques. The incidence of postoperative C5 palsies was reduced from 7.3 to 0.9% due to intraoperative continuous EMG monitoring. No patients suffered a postoperative C5 palsy when intraoperative evidence of root irritation was absent [4]. Also intraoperative evoked EMG monitoring was shown as a valuable tool in posterior cervical instrumentation using pedicle screws [2]. The intraoperative electrical stimulation was accurate in verifying screw position with 99% of positive predictive value. Patients with skeletal congenital malformations or dysplasia who are positioned for the surgical procedure in anaesthesia can lead to disappearance of evoked potentials simply by positioning of the head [6] while correction of the position lead immediately to the occurrence of the potentials. In this respect alteration in the surgical plan resulted in successful spinal surgery.
The aim of the current study was to determine the sensitivity and specificity of multimodal intraoperative monitoring as described by Sutter et al. [9, 10] used to monitor spinal cord and nerve root function during complex cervical spine surgeries.
Patient population and method
About 246 consecutive patients prepared for cervical spine surgical procedure were selected for multimodal intraoperative monitoring from March 2000 to December 2005 due to the potential risk of neurological damage as the result of the complex surgical procedure. The clinical diagnosis are shown in Table 1 and the surgical approach, anterior, posterior 360° approach is summarized in Fig. 1. The patients were informed about the procedure after the neurological examination. There were 112 females and 134 males of mean age 57.9 years (range from 1 to 83 years). The general inclusion and exclusion criteria as well as the method of examination of the multimodal intraoperative neurophysiological monitoring as well as the anaesthesia protocol have been described by Sutter et al. [9, 10]. All MIOM during this period of time were performed by the first two authors, experienced neurophysiologists specially trained in the different methods of MIOM.
Table 1.
Diagnostic groups of patients operated on cervical spine with the aid of MIOM (n = 246)
| Diagnostic characteristics | |
|---|---|
| Congenital anomaly | 16 |
| Degenerative | 176 |
| Disc herniation | 20 |
| Fractures/instability | 7 |
| Rheumatoid arthritis | 17 |
| Miscellaneous | 10 |
| Total | 246 |
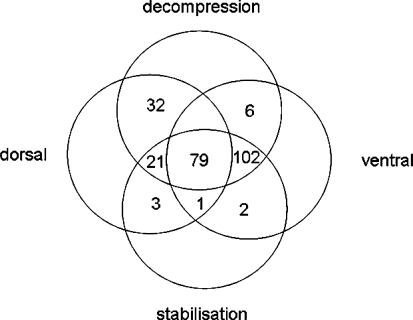
Fig. 1.
Presentation of surgical approaches on 246 patients with cervical spine disorders
Results
The surgical procedure of the 246 patients with cervical spine pathologies mainly resulting in cervical myelopathy were planned and performed according to the pre-existing pathology, by experienced and skilled spine surgeons. The mean time of intraoperative monitoring was 4.3 h ranging from 0.8 to 17 h. During the surgical procedure the tests of the multimodal intraoperative monitoring as described by Sutter [9, 10] were applied according to the actual situation taking the surgical procedure into account in order to assess the functional status of spinal cord, i.e. the motor and sensory pathways. If required, due to the selective nerve root decompression, monitoring of the nerve roots were included. The different tests and their frequency of application during the surgical procedure is summarized in Table 2.
Table 2.
Test applied to the patient population (n = 246) with cervical spinal stenosis
| Monitoring modality | Monitorings applied | Baseline recording | ||
|---|---|---|---|---|
| Out of 246 cases | Mean tests per patient | Normal | Abnormal/No potential | |
| cm-EP | 241 (98.0%) | 2.6 | 58 | 180/3 |
| Sm-EP | 7 (2.8%) | 2.4 | NVM | |
| cs-EP | 104 (42.3%) | 1.0 | 16 | 74/14 |
| ss-EP | 2 (0.8%) | NVM | ||
| nc-EP | 231 (93.9%) | 1.4 | 67 | 163/1 |
| ns-EP | 27 (11.0%) | 1.1 | NVM | |
| F-Wave | 2 (0.8%) | NVM | ||
| EMG | 219 (89.0%) | 2.6 | No Spontaneous Activity | |
Tests: recorded muscle pairs or stimulated nerve pairs in a given modality, NVM normative value missing
cm-EP Cerebro-muscular evoked potentials, cs-EP cerebro-spinal evoked potentials, ns-EP neuro-spinal evoked potentials, nc-EP neuro-cerebral evoked potentials, sm-EP spino-muscular evoked potentials, ss-EP spino-spinal evoked potentials
The surgeon was informed about the changes of the potentials particularly if the trend justified an alert so the surgeon could adapt the procedure accordingly.
Within the group of 246 patients undergoing the cervical spine surgery 232 presented true negative while 2 patients false negative findings. The two false negative cases are summarized in Table 3: fortunately both patients with postoperative C5 radiculopathy recovered completely within 1, respectively 6 weeks. Both were not monitored by continuous EMG from the deltoid muscle as proposed by Jimenez [4].
Table 3.
MIOM of false negative cases (n = 2) out of 246 Patients operated on cervical spine
| False negative cases of cervical | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Patient | Region | Pathology | Surgery | Duration (h) | IOM modalities | IOM-baseline | IOM-changes | Neurological deterioration | Duration (week) | Recovery |
| F, 55 years | C2–C5 | Spondylotic cervical myelopathy and deformity (SLCT) | Corpectomy C3 + C4, Correction and Fusion, dv | 9.3 | csC8-EPcmBB,ADM-EPnMNc-EPcont EMGBB,ADM | All potentials available, but pathologic | Loss of all potentials after C4/5 distr., recovered after reduction | Radiculopathy C5 left | 6 | Complete |
| F, 70 years | C5–C7 | Spondylotic cervical myelopathy (SLCT) | Dorsal decompression | 3.3 | csT1-EPcmADM,,AH-EPnMNc-EPcont EMGADM,AH | All Potentials available, but pathalogic | None | Radiculopathy C5 left | 1 | Complete |
There were two false positive cases (Table 4) while ten patients presented true positive findings (Table 5).
Table 4.
MIOM of false positive cases (n = 2) out of 246 Patients operated on cervical spine
| False positive cases of cervical | ||||||||
|---|---|---|---|---|---|---|---|---|
| Patient | Region | Pathology | Surgery | Duration | IOM modalities | IOM-baseline | IOM-changes | Expected neurological deficit |
| F, 69 years | C0–T1 | Congen. Malformation with sek. compressive Myelopathy (SLCT) | Dorsal decompression and fusion | 3.8 h | csT5-EPcmEP BR,ADMnMNc-EPEMG BR,ADM | Pathological motor and sensory potentials on both sides | Alteration of cmEP ADM left | Radiculopathy C8 left |
| F, 83 years | C6–C7 | Spondylotic cervical myelopathy (SLCT) | Ventral and dorsal decompression and fusion | 5.3 h | csT12-EPcmEP BR,ADMnc/ns-EP MN, TNEMG BR,ADM | Motor and sensory evoked potentials severely pathological | Alteration of ncEP MN left | Ataxie left Arm |
Table 5.
MIOM of true positive cases (n = 10) out of 246 patients operated on cervical spine
| True positive cases of cervical | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Patient | Region | Pathology | Surgery | Duration (h) | IOM modalities | IOM-baseline | IOM-changes | Neurological deterioration | Duration | Recovery |
| F, 44 years | C0–C7 | Rheumatoid arthritis | Decompression and fusion, ventral and dorsal | 6 | csEP, cmEP BR ADM, nsEP, ncEP MN, TN, cont EMG | All available, but pathologic | Deterioration of pyramidal tract and dorsal tract function left arm | Central paresis left arm | After 2 days reoperation | Complete |
| F, 77 years | C1–C6 | Rheumatoid arthritis | Decompression and fusion C0–T1 | 3.8 | csEP, cmEP BR ADM | All available, but pathologic | Alteration of csEP and cmEP left arm | Central paresis left arm | 3 months | Complete |
| M, 40 years | C3–C4 | Spondylotic cervical myelopathy | Decompression and fusion ventral | 2.8 | cmEP BR ADM, ncEP MN, cont EMG | All available, but pathologic | Loss of cmEP BR right | Sensomotor radiculopathy C5 right | 2 months | Complete |
| M, 79 years | C3–C5 | Degenerative stenosis and instability | Decompression and fusion ventral and dorsal | 4.8 | csEP, cmEP BR ADM, ncEP MN, cont EMG | All available, but pathologic | Alteration of ncEP MN right | Proprioceptiv deficits arm right | 1 day | Complete |
| M, 66 years | C3–C5 | Spondylotic cervical myelopathy | Decompression dorsal | 3.5 | csEP, cmEP BR ADM, ncEP MN TN, nsEP, cont EMG | All available but pathologic | Alteration cmEP arm and leg right | Deterioration of preexisting heavy spasticity | 2 months | Complete |
| F, 61 years | C5–C6 | Spondylotic cervical myelopathy | Decompressin and fusion ventral and dorsal | 3.3 | csEP, cmEP BR ADM, ncEP MN, cont EMG | All available but pathologic | Deterioration of cmEP ADM right at end of decompression | Central paresis arm right | 1 day | complete |
| M, 78 years | C3–C7 | Spondylotic cervical myelopathy | Laminoplasty C3–C7 | 3.8 | cmEP BR ADM, ncEP MN, cont EMG | All available but pathologic ncEP | Deterioration of cmEP and ncEP left | Deterioration of central paresis left | 1 day | Complete |
| F, 56 years | C4–6 | Spondylotic myelopathy and radiculopthy C6 bilateral | Decompression and fusion, ventral | 3.5 | cmEP BB TM TA, ncEP MN, cont EMG | All available but pathologic | Deterioration of all cmEP right | Deterioration of preexisting paresis right | 3 months | Complete |
| m, 73 y | C4–C6 | Spondylotic cervical myelopathy | Decompression and fusion ventral | 4.8 | cmEP DM BB TA, cont EMG, ncEP MN TN | All available but pathologic | Deterioration of cmEP DM left | C5 radiculopathy left | 1 month | Complete |
| M, 65 y | C4–C7 | Spondylotic cervical myelopathy | Decompression and fusion ventral | 6 | cmEP DM BR ADM, cont EMG, ncEP MN TN | All available but pathologic | Deterioration of cmEP DM left | C5 radiculopathy left | 5 months | Complete |
Using the standard formula the sensitivity of the MIOM for the cervical spine surgical procedure was calculated to be 83.3% and the specificity 99.2%. It has to be clearly stated that none of the 246 patients who underwent complex cervical spine procedure sustained a permanent deterioration of pre-existing symptoms or any new occurring symptoms.
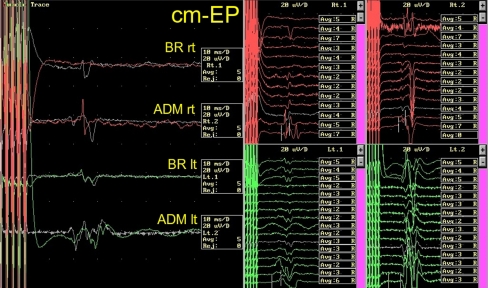
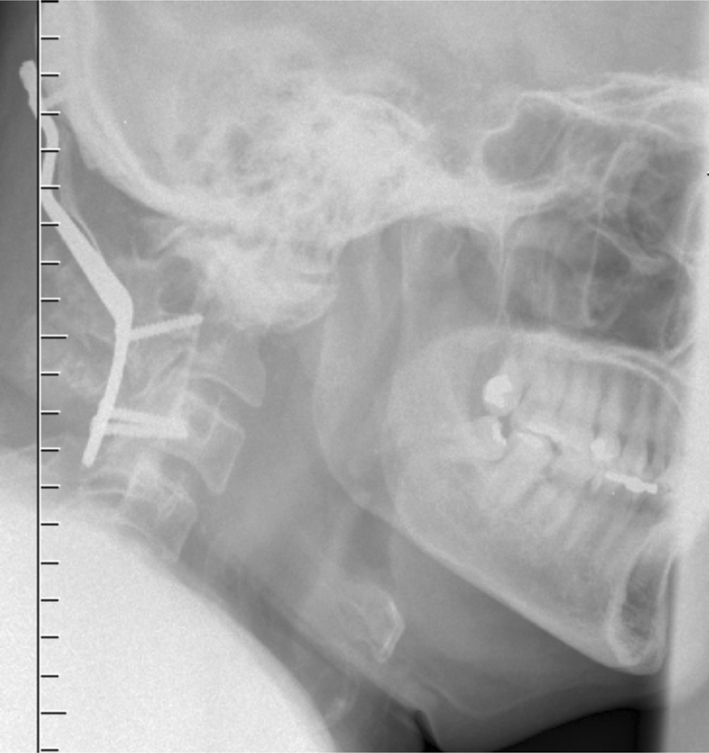
The following short case documents the close collaboration between the spine surgeon and the neurophysiologist resulting in a successful management of impending complications in cervical spine surgery. A 55-year-old male had to undergo ventro-dorsal decompression and stabilisation for compressive myelopathy due to cranio-cervical dyssegmentation (Figs. 2, 3). During reposition of the head we almost lost the motor-evoked potentials (Fig. 4). After release of the reposition the evoked potentials recovered almost to the baseline, so that the surgeon could carry on after adapting the surgical procedure (Fig. 5). The patient had the same neurological deficits postoperatively.
Fig. 2.
Pre-Op X-ray
Fig. 3.
Pre-Op CT-Scan
Fig. 4.
Motor-evoked potentials
Fig. 5.
Post-Op X-ray
Discussion
The true incidence of complications of surgical procedures of cervical spine is unknown. The recently introduced spine tango, a multi-centre study initiated by the Spine Society of Europe, might in future offer reliable information on the outcome of treatment of the different pathologies of cervical spine with incidence of surgically induced complications. However, the data has not been released to date. The study of Epstein in a historical study of 218 unmonitored and 100 monitored patients, as followed by monitoring of SEP, revealed an incidence of 4% of severe neurological complication (quadriplegia) while none in the monitored group. This observation documents the potential high risk of neurological deficit however at that time only SEP was used. Meanwhile it is well established in the literature that SEP alone do not offer reliable information about the function of the descending corticospinal tract nor about the motor pathways of the nerve roots. Therefore the study by Taunt [11] does not really add any new information while using SEPs to monitor patients with radiculopathy due to cervical disc herniation. In our study population only 20 patients were operated on disc herniation however, being accompanied by additional bony degenerative changes at the operated level. In a mixed population of cervical spine surgical procedures Bose [1] presented the sensory and motor-evoked potentials for detection of spinal cord function during anterior cervical fusion and the advantage of having to alert the surgeon when pathological alteration of the potentials suddenly occurs. A very recent report by Khan [5] which analyzed 508 with SEP monitoring during cervical spine corpectomy is in spite of the current body of knowledge [7, 8] of very little value considering the anterior approach in corpectomy the descending pathways are the prime focus for the monitoring techniques. Khan calculated the sensitivity as 77% and specificity 100% only by using SEP. In the presented population of 246 patients with cervical spine surgical procedure of mixed population with majority degenerative changes and cervical spine canal stenosis based upon our findings we found a sensitivity of 83% and specificity of 99%. The application of the available monitoring tests has been constantly adapted according to the procedure the neurophysiologist observed the surgeon and constantly informed him about the development and the trends of the different potentials being monitored. If reproducible pathological finding has been observed the surgeon has been alerted and shared decision has been made whether the procedure had to be adapted. In the entire series of 246 patients only 2 false negative cases were documented. Both of them suffered a postoperative C5 lesion which luckily recovered completely. In this respect it has to be stated that those cases occurred at the beginning of the monitoring activities in the clinic. In a later stage the constant monitoring of the deltoid muscle by the means of motor-evoked potentials have been introduced and no new C5 palsy has occurred as false negative finding. Based upon our observation the MEP of C5 nerve root have an advantage to the continuous EMG monitoring as proposed by Jimenez [4] as being most probably a more sensitive finding. The one case with a false positive result was a patient with severe pathological changes of cervical spine and based upon the pathological findings of SEP of median nerve an expected ataxia of the left arm was documented however, no neurological findings was observed postoperatively after the surgeon performed control in situ without finding any unusual alteration in the surgical environment.
Out of the ten true positive cases six were attributed to a lesion of spinal cord while four to the nerve root. In this respect we could document and foresee in the very complex patient population with severe pathology of the cervical spine a rate of minor neurological complication of 5% and all recovered to the preoperative status. It has to be clearly stated that none of the 246 patients who underwent complex cervical spine procedure sustained a permanent deterioration of pre-existing symptoms or any new occurring symptoms.
Even though we have no historical comparable group and out of obvious reasons a prospective randomized study was not initiated as clearly explained by Sala et al. [7, 8]. We are of the opinion that looking at our results the MIOM is an effective method of monitoring the spinal cord and nerve root function during cervical spine surgery and can help to reduce the risk of neurological deficit by alerting the surgeon when monitoring changes are observed in complex surgical procedures.
Acknowledgments
Dr. Lote Medicus fund for the financial support of the development of MIOM at the Schulthess Clinic. Dave O’Riordan and Charles McCammon for helping with the manuscript. Anne Mannion PhD for the critical review of the manuscript. A special thanks to professor Arnaldo Benini who supported the study with his patients.
Conflict of interest statement None of the authors has any potential conflict of interest.
References
- 1.Bose B, Sestokas AK, Schwartz DM. Neurophysiological monitoring of spinal cord function during instrumented anterior cervical fusion. Spine J. 2004;4:202–207. doi: 10.1016/j.spinee.2003.06.001. [DOI] [PubMed] [Google Scholar]
- 2.Djurasovic M, Dimar JR, 2nd, Glassman SD, Edmonds HL, Carreon LY. A prospective analysis of intraoperative electromyographic monitoring of posterior cervical screw fixation. J Spinal Disord Tech. 2005;18:515–518. doi: 10.1097/01.bsd.0000173315.06025.c6. [DOI] [PubMed] [Google Scholar]
- 3.Epstein FJ, Farmer JP, Freed D. Adult intramedullary spinal cord ependymomas: the result of surgery in 38 patients. J Neurosurg. 1993;79:204–209. doi: 10.3171/jns.1993.79.2.0204. [DOI] [PubMed] [Google Scholar]
- 4.Jimenez JC, Sani S, Braverman B, Deutsch H, Ratliff JK. Palsies of the fifth cervical nerve root after cervical decompression: prevention using continuous intraoperative electromyography monitoring. J Neurosurg Spine. 2005;3:92–97. doi: 10.3171/spi.2005.3.2.0092. [DOI] [PubMed] [Google Scholar]
- 5.Khan MH, Smith PN, Balzer JR, Crammond D, Welch WC, Gerszten P, Sclabassi RJ, Kang JD, Donaldson WF. Intraoperative somatosensory evoked potential monitoring during cervical spine corpectomy surgery: experience with 508 cases. Spine. 2006;31:E105–E113. doi: 10.1097/01.brs.0000200163.71909.1f. [DOI] [PubMed] [Google Scholar]
- 6.Ofiram E, Lonstein JE, Skinner S, Perra JH. The disappearing evoked potentials: a special problem of positioning patients with skeletal dysplasia: case report. Spine. 2006;31:E464–E470. doi: 10.1097/01.brs.0000222122.37415.4d. [DOI] [PubMed] [Google Scholar]
- 7.Sala F, Lanteri P, Bricolo A. Motor evoked potential monitoring for spinal cord and brain stem surgery. Adv Tech Stand Neurosurg. 2004;29:133–169. doi: 10.1007/978-3-7091-0558-0_4. [DOI] [PubMed] [Google Scholar]
- 8.Sala F, Palandri G, Basso E, Lanteri P, Deletis V, Faccioli F, Bricolo A. Motor evoked potential monitoring improves outcome after surgery for intramedullary spinal cord tumors: a historical control study. Neurosurgery. 2006;58:1129–1143. doi: 10.1227/01.NEU.0000215948.97195.58. [DOI] [PubMed] [Google Scholar]
- 9.Sutter M, Eggspühler A, Grob D, Jeszenszky D, Porchet F, Muller A, Dvorak J (2007) The diagnostic value of Multimodal Intraoperative Monitoring (MIOM) during Spine Surgery: a prospective Study of 1017 cases. Eur Spine J (in preparation) [DOI] [PMC free article] [PubMed]
- 10.Sutter M, Eggspühler A, Muller A, Dvorak J (2007) Multimodal Intraoperative Monitoring: Methodology. Eur Spine J (In preparation) [DOI] [PMC free article] [PubMed]
- 11.Taunt CJ, Jr, Sidhu KS, Andrew SA. Somatosensory evoked potential monitoring during anterior cervical discectomy and fusion. Spine. 2005;30:1970–1972. doi: 10.1097/01.brs.0000176321.02963.72. [DOI] [PubMed] [Google Scholar]