Abstract
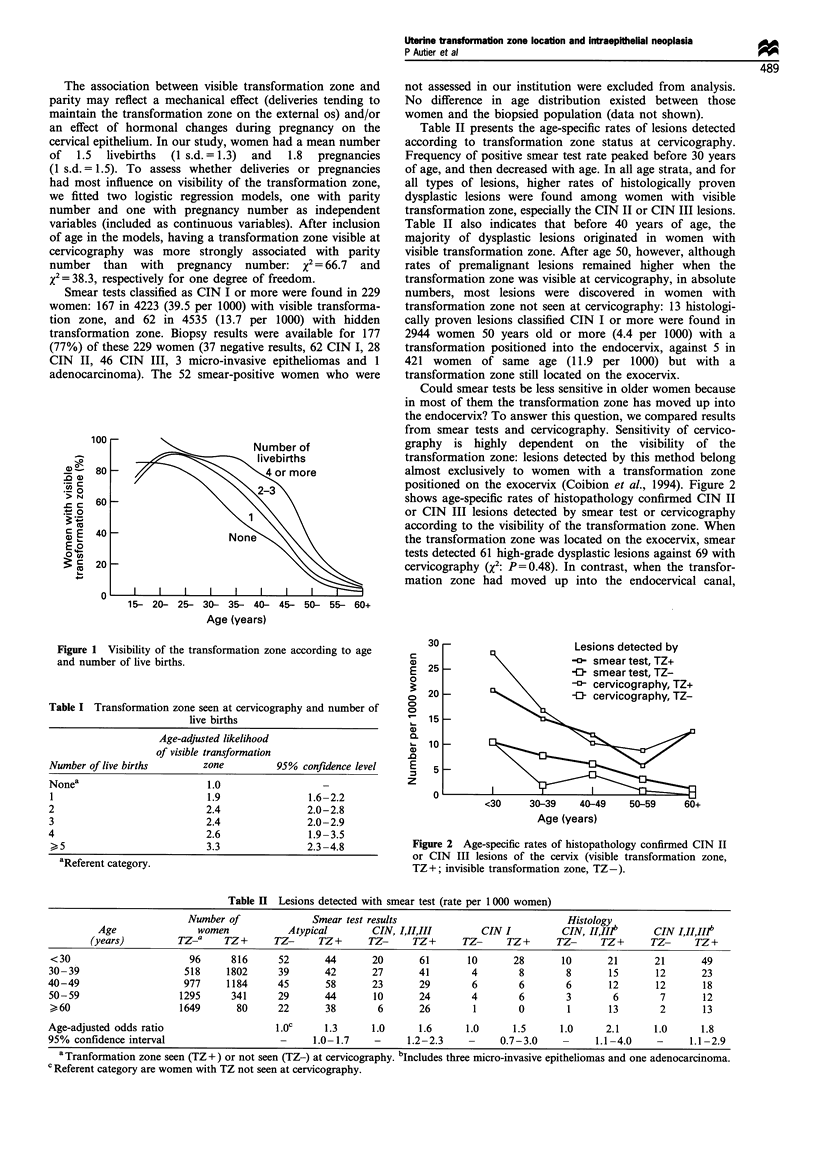
We examined the relationship between the frequency of premalignant lesions of the cervix and location of the transformation zone on the cervix among 8758 women as assessed using cervicography. An endo- and exocervical smear test was performed at the same time. Women with smear test classified CIN I or more were recalled and any abnormal area was biopsied under colposcopy. The transformation zone was located on the exocervix in 94% of women younger than 25 years old; as age increased, the proportion of women with a transformation zone located on the exocervix steadily decreased to reach less than 2% after 64 years old. As compared with women having a transformation zone in the endocervical canal, the age-adjusted likelihood of discovering a histologically proven dysplastic lesion was 1.8 times more frequent among women with a transformation zone located on the exocervix (95% confidence interval 1.1-2.9). This higher frequency seemed not attributable to a lower sensitivity of the smear test when the transformation zone was hidden. The results also showed that deliveries tended significantly to maintain the transformation zone on the exocervix. Parity is a known risk factor for cervix cancer, but the mechanism by which it favours malignant lesions remain unknown. Our results suggest that with increasing numbers of livebirths, the transformation zone is directly exposed for longer periods to external agents involved in dysplastic lesions.
Full text
PDF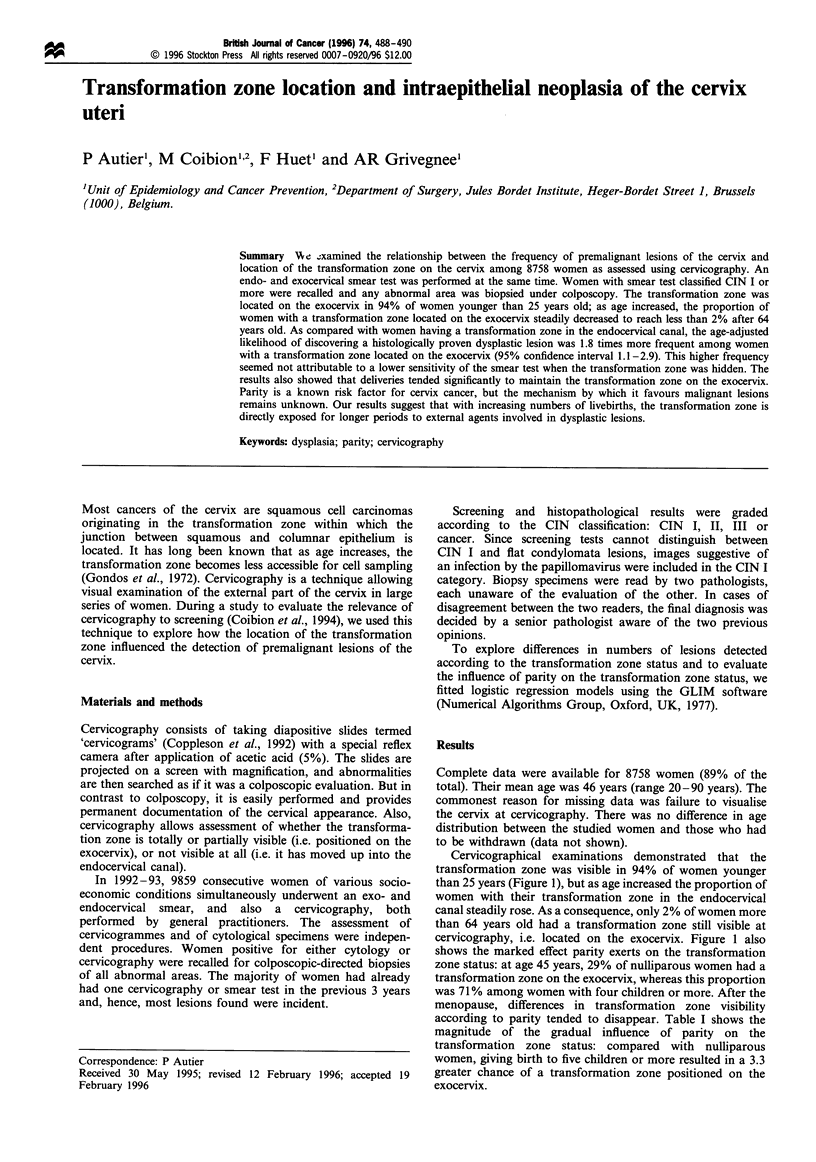

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brinton L. A., Reeves W. C., Brenes M. M., Herrero R., de Britton R. C., Gaitan E., Tenorio F., Garcia M., Rawls W. E. Parity as a risk factor for cervical cancer. Am J Epidemiol. 1989 Sep;130(3):486–496. doi: 10.1093/oxfordjournals.aje.a115362. [DOI] [PubMed] [Google Scholar]
- Cecchini S., Piazzesi G., Carli S. Sensitivity of the screening program for cervical cancer in the Florence District. Gynecol Oncol. 1989 May;33(2):182–184. doi: 10.1016/0090-8258(89)90547-7. [DOI] [PubMed] [Google Scholar]
- Coibion M., Autier P., Vandam P., Delobelle A., Huet F., Hertens D., Vosse M., Andry M., De Sutter P., Heimann R. Is there a role for cervicography in the detection of premalignant lesions of the cervix uteri? Br J Cancer. 1994 Jul;70(1):125–128. doi: 10.1038/bjc.1994.260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuzick J., Singer A., De Stavola B. L., Chomet J. Case-control study of risk factors for cervical intraepithelial neoplasia in young women. Eur J Cancer. 1990;26(6):684–690. doi: 10.1016/0277-5379(90)90117-c. [DOI] [PubMed] [Google Scholar]
- Cuzick J., Szarewski A., Terry G., Ho L., Hanby A., Maddox P., Anderson M., Kocjan G., Steele S. T., Guillebaud J. Human papillomavirus testing in primary cervical screening. Lancet. 1995 Jun 17;345(8964):1533–1536. doi: 10.1016/s0140-6736(95)91086-7. [DOI] [PubMed] [Google Scholar]
- Gondos B., Marshall D., Ostergard D. R. Endocervical cells in cervical smears. Am J Obstet Gynecol. 1972 Nov 15;114(6):833–834. doi: 10.1016/0002-9378(72)90912-x. [DOI] [PubMed] [Google Scholar]
- Mitchell H., Medley G., Giles G. Cervical cancers diagnosed after negative results on cervical cytology: perspective in the 1980s. BMJ. 1990 Jun 23;300(6740):1622–1626. doi: 10.1136/bmj.300.6740.1622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parazzini F., La Vecchia C., Negri E., Fedele L., Franceschi S., Gallotta L. Risk factors for cervical intraepithelial neoplasia. Cancer. 1992 May 1;69(9):2276–2282. doi: 10.1002/1097-0142(19920501)69:9<2276::aid-cncr2820690912>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]


