Abstract
Interest in airborne smallpox transmission has been renewed because of concerns regarding the potential use of smallpox virus as a biothreat agent. Air disinfection via upper-room 254-nm germicidal UV (UVC) light in public buildings may reduce the impact of primary agent releases, prevent secondary airborne transmission, and be effective prior to the time when public health authorities are aware of a smallpox outbreak. We characterized the susceptibility of vaccinia virus aerosols, as a surrogate for smallpox, to UVC light by using a benchtop, one-pass aerosol chamber. We evaluated virus susceptibility to UVC doses ranging from 0.1 to 3.2 J/m2, three relative humidity (RH) levels (20%, 60%, and 80%), and suspensions of virus in either water or synthetic respiratory fluid. Dose-response plots show that vaccinia virus susceptibility increased with decreasing RH. These plots also show a significant nonlinear component and a poor fit when using a first-order decay model but show a reasonable fit when we assume that virus susceptibility follows a log-normal distribution. The overall effects of RH (P < 0.0001) and the suspending medium (P = 0.014) were statistically significant. When controlling for the suspending medium, the RH remained a significant factor (P < 0.0001) and the effect of the suspending medium was significant overall (P < 0.0001) after controlling for RH. Virus susceptibility did not appear to be a function of virus particle size. This work provides an essential scientific basis for the design of effective upper-room UVC installations for the prevention of airborne infection transmission of smallpox virus by characterizing the susceptibility of an important orthopoxvirus to UVC exposure.
Due in part to the 11 September 2001 terrorist attacks, the subsequent mailing of letters containing weaponized Bacillus anthracis in the United States, and the ongoing terrorist attacks and wars in Iraq and Afghanistan, the perceived threat of an intentional release of biothreat agents has increased dramatically over the last 6 years. Smallpox, because of its high case fatality rate and transmissibility, is a serious bioterrorist threat listed by the Centers for Disease Control and Prevention as a category A agent (http://www.bt.cdc.gov/agent/agentlist-category.asp). At present, our defense against smallpox relies on early identification, emergency vaccination, and quarantine. Recent mathematical models suggest that vaccination campaigns alone may have difficulty containing a smallpox outbreak until after many people become infected (3, 5, 6, 15, 16). Estimates from these studies vary widely because of uncertainties associated with model parameters such as the reproductive number, level of immunity in the community, and availability of vaccines. Furthermore, the protection afforded by vaccines can be evaded through manipulations of the viral genome (9). Therefore, innovative methods are needed for limiting the spread of disease that would be effective during the especially critical interval between the occurrence of the first cases and the start of vaccination campaigns. Because an aerosol release of smallpox virus is a strong possibility for introducing the virus into a susceptible population and because the consensus of the Working Group on Civilian Biodefense concluded that “Smallpox spreads from person to person, primarily by droplet nuclei or aerosols expelled from the oropharynx of infected persons and by direct contact” (8, 21), air disinfection in public buildings, especially hospitals and schools, may be able to reduce the effectiveness of primary agent releases, may prevent a portion of secondary transmission of smallpox that occurs via aerosols, and may be effective prior to the time when public health authorities are aware of the outbreak.
Upper-room 254-nm germicidal UV (UVC) light, often referred to as UV germicidal irradiation, has been shown to be an efficient and economical means of air disinfection for tuberculosis and other airborne infections (1, 11, 18, 22, 23). If organisms circulate from the lower room to the upper room (i.e., if there is adequate mixing of room air) and receive an adequate dose of UVC, upper-room UVC can potentially lower the concentration of infective organisms in the lower part of the room and thereby control the spread of airborne infections among room occupants without exposing the occupants to a significant amount of UV radiation (1, 4, 23).
UVC susceptibility of microorganisms is often assumed to follow a first-order decay with a susceptibility parameter, z, according to the equation CUV/Cno UV = e−zD, where CUV/Cno UV (sometimes referred to as the fraction remaining) is the ratio of the concentration of virus plaques with the UVC on to the concentration with the UVC off, z, defined as UVC susceptibility, is expressed in meters squared per joule, and D is the UVC dose in joules per meter squared. The higher the z value, the more susceptible the organism is to UV light. Two studies have been conducted examining the utility of UVC for disinfecting aerosolized poxvirus. In 1943, Edward et al. established that vaccinia and influenza viruses are highly susceptible to UVC, with greater than 90% viral inactivation with exposure times of as little as 0.5 s for vaccinia virus (2). In 1964, Jensen conducted a similar study, exposing aerosolized vaccinia virus along with other aerosolized viruses to UVC (10). Jensen was able to demonstrate an inactivation rate of greater than 99.99% for vaccinia virus aerosols exposed to UVC for as little as 0.3 s. Rauth (17) studied the UVC sensitivity of a range of viruses in liquid suspension and showed that vaccinia virus is highly susceptible to UVC inactivation, in part because of its large size and adsorption cross-section relative to those of other viruses. Unfortunately, these studies have important limitations. The data on UVC inactivation in liquid may not be relevant to airborne virus wrapped in respiratory secretions. Neither of the aerosol studies characterized the actual delivered dose, altered the dose of UVC to determine the susceptibility of a poxvirus aerosol to inactivation, or determined the effect of relative humidity (RH) on the survival of irradiated poxvirus aerosols. However, the survival of an aerosolized pathogen in the presence of UVC has been shown to be dependent on the RH (7, 12, 14, 19, 20) and the medium used for aerosol suspension (14).
The objective of this investigation was to characterize the susceptibility of vaccinia virus to UVC with respect to UVC dose, RH, and aerosol suspension medium in a laboratory setting by using an environmentally controlled benchtop chamber equipped with a UVC light exposure window and thereby develop a model of susceptibility to UVC. This characterization of susceptibility to UVC is a part of the essential scientific basis for designing effective upper-room UVC installations for the prevention of airborne infection transmission in hospitals and other public buildings.
MATERIALS AND METHODS
Vaccinia virus stock.
Vaccinia virus (strain WR) was kindly provided by Acambis (Cambridge, MA) and was grown in Vero cells (ATCC CCL-81) obtained from the American Type Culture Collection (Manassas, VA) at 37°C with 5% CO2 in growth medium consisting of minimum essential medium with Earl's balanced salts (HyClone, Logan, UT) and 10% heat-deactivated defined fetal bovine serum (HyClone, Logan, UT). Virus stocks were made by inoculating vaccinia virus at a multiplicity of infection of 0.1 into T-150 flasks containing a confluent monolayer of Vero cells and 2 ml of growth medium. The flasks were incubated in 5% CO2 at 37°C for 60 min. The flasks were gently rocked at 15-min intervals. After incubation, 25 ml of growth medium was added to the flask, which was then incubated in 5% CO2 at 37°C for 2 days. Vaccinia virus was harvested by scraping the flask, decanting medium, and centrifuging it at 2,000 × g for 10 min at 4°C. The supernatant was decanted, and the pellet was suspended in 5 ml of growth medium in a 15-ml polypropylene centrifuge tube. Each tube was kept in ice water and sonicated for 1 min with a Branson 450 Sonicator (Emerson Electric, St. Louis, MO) at setting 5 and a 50% duty cycle to disrupt the cells. The tubes were then spun at 2,000 × g for 10 min at 4°C to remove cellular debris. Virus stocks (approximately 108 PFU/ml) were portioned into 1-ml volumes and stored at −80°C until use.
Benchtop UVC exposure chamber.
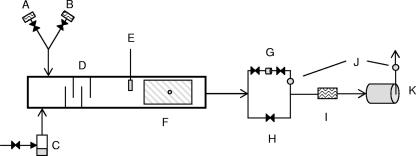
The details of the one-pass, dynamic aerosol test system were described by Ko et al. (12) and Lai et al. (14) and are shown schematically in Fig. 1. Briefly, the chamber is composed of three sections, (i) aerosol generation and RH control, (ii) UVC exposure, and (iii) sampling. The first part of the system contains a six-jet Collison nebulizer (CN-38; BGI, Waltham, MA) filled with a vaccinia virus suspension (described in the section on vaccinia virus survival experimental procedures). The nebulizer output was mixed with makeup air composed of HEPA-filtered room air, filtered humidified air, or filtered desiccated air to achieve the desired RH. For a low RH, the nebulizer output was directed through a diffusion dryer prior to entering the chamber to achieve additional drying. The nebulizer output and makeup air passed through a series of baffles to promote droplet drying and thorough uniform distribution of particles at the appropriate RH (measured via an Omega RH32 temperature and RH meter [Omega Engineering Inc., Stamford, CT]) prior to entry into the UVC exposure section. UVC was generated by six 36-W low-pressure mercury (254-nm wavelength) lamps (Lumalier, Memphis, TN) which were fixed 25 cm above a fused quartz window measuring 279 by 254 mm. Screens placed between the UVC light source and exposure window were used to attenuate the UVC output and dose within the exposure chamber. UVC irradiance in the chamber was measured through a fused quartz port in the bottom of the UVC exposure section of the chamber with an IL 1400A UV light meter (International Light, Peabody, MA) and ranged from 0.1 to 3.2 J/m2. These values were based on initial vaccinia virus dose-response experiments performed with our chamber and the detection limits of our plaque assay system. The UVC dose was determined by multiplying the UVC irradiance by the exposure time (7.6 s). The exposure time was computed on the basis of the cross-sectional area of the chamber and the airflow rate. Air was drawn through the chamber by a pump at 28.3 liters/min through a manifold attached to the sampler. A HEPA filter was connected after the samplers to remove all of the aerosols before the airstream entered the pump. When sampling was not in progress, the aerosol-laden airstream running through the chamber was bypassed around the samplers and the flow was directed to the HEPA filter as shown in Fig. 1. The entire apparatus was set up inside a 6-ft class II biosafety cabinet and maintained under negative pressure with respect to the cabinet interior.
FIG. 1.
Benchtop chamber schematic. Components: A, saturated air; B, desiccated air; C, pressurized nebulizer; D, baffles; E, temperature and RH meter; F, quartz UV exposure window; G, sample collector; H, sample bypass; I, HEPA filter; J, flow meters; K, vacuum pump.
Vaccinia virus survival experimental procedures.
The UVC light was turned on with clean air flowing through the chamber at least 30 min prior to aerosolization. Aerosols were generated by adding 1 ml of a vaccinia virus suspension (106 to 107 PFU/ml of medium [enumerated after thawing]), 10 μl of Antifoam A (Sigma, St. Louis, MO), and 49 ml of either water or synthetic respiratory fluid (SRF [phosphate-buffered saline with 10% fetal bovine serum]) into the Collison nebulizer and pressurizing it at 138 kPa. The nebulizer was run for 20 min before sampling to ensure that concentrations within the chamber had reached a steady state and would remain constant during the experiment. Samples were collected by passing the entire chamber airflow through a 37-mm gelatin filter (SKC Inc., Eighty Four, PA) having a 3-μm nominal pore size (retention rates for phages T1 and T3, which are roughly in the same size range as vaccinia virus, are 99.9% and 99.94%, respectively) and housed within a polystyrene air sampling cassette. Samples pairs were collected consisting of a sample with the UVC lights on, followed by a control sample with the UVC lights off for the corresponding conditions and vice versa. Triplicate sample pairs were collected for each combination of UVC dose (approximately 0.1, 0.7, 1.5, and 3.0 J/m2), RH (18 to 23%, 58 to 63%, and 78 to 83%), and aerosol suspending medium (water, SRF) conditions. After sampling, the filters were removed from the cassette and placed in a 50-ml polypropylene centrifuge tube along with 1 ml of sterile water. The tube was vortexed and then incubated at 37°C for 10 min to dissolve the filter. After incubation, the tube was vortexed again prior to the addition of 0.1 ml of the dissolution volume to the plaque assay in triplicate. Two serial 1:10 dilutions of dissolved filter solution in sterile water were also subjected to plaque assay in triplicate. The culturable fraction remaining for each sample pair was calculated by dividing the average number of PFU formed with the UVC lights on by the average number of PFU formed with the UVC lights off. The decay rate constant was then determined by dividing the natural logarithm of the average fraction remaining for the three sample pairs by the UVC dose.
Plaque assay.
Six-well tissue culture plates were seeded with 3 ml of a 2 × 105 cell ml−1 concentration of Vero cells (enumerated by hemacytometer) and incubated overnight in 5% CO2 at 37°C. Two milliliters of growth medium was removed from each well prior to the addition of 0.1 ml of the virus filter sample (described in the section on vaccinia virus survival experimental procedures) to each well. For a subset of samples corresponding to size-selective samples collected on 80-mm filters (described in the section on the evaluation of particle size distribution and survival), 2.4 ml of growth medium was removed and 0.6 ml of virus sample was added to each well. The tissue culture plate containing the virus samples was initially incubated for 1 h in 5% CO2 at 37°C with gentle rocking every 15 min. After the initial incubation, 2 ml of fresh culture medium was added to each well and the plate was incubated in 5% CO2 at 37°C for 2 days. After incubation, the cell culture medium was removed and Vero cells were fixed and stained with 1% crystal violet in 70% methanol for plaque counting.
Evaluation of particle size distribution and survival.
Experiments were undertaken by using the same procedures as described above to investigate the size distribution of viral aerosols and the corresponding survival of vaccinia virus, with the following changes. (i) Viral aerosols were exposed to a fixed UVC dose of 0.5 J/m2, (ii) RH testing was done at 78 to 83% and 18 to 23% RH only, (iii) one sample pair was collected for each condition, and (iv) samples were collected with the Andersen 2000 ambient particle sizing cascade sampler (BGI Inc., Waltham, MA). Prior to sampling, 80-mm gelatin filters (SKC Inc., Eighty Four, PA) were placed on top of each impactor plate of the Andersen 2000 sampler. A 37-mm gelatin filter cassette was placed in line after the last plate. After sampling, the 80-mm gelatin filters from impactor plates corresponding to stage 4 (2.1 to 3.3 μm), stage 5 (1.1 to 2.1 μm), and stage 6 (0.7 to 1.1) (impactor plates were not loaded for stages 1, 2, and 3 [>3.3 μm] since preliminary data indicated that there were no virus particles collected on these stages) and the cassette were removed and transferred to 50-ml centrifuge tubes. Because of their increased size, the 80-mm filters were cut into quarters prior to transfer into a 50-ml centrifuge tube and 4 ml of water was added for dissolution. The mixture was then vortexed and incubated at 37°C for 10 min, and 0.4 ml of the dissolved filter solution was added to the plaque assay. The 37-mm filters were processed as described above. The numbers of PFU determined from the filters which collected virus aerosols without UVC exposure were used to calculate the particle size distribution in terms of the total biological activity (plaque-forming activity), while the difference between the numbers of PFU with and without UVC exposure was used to calculate vaccinia virus survival for each size range corresponding to respective impactor stages. All data were normalized to account for differences in dissolution and inoculation volumes.
Statistical analysis.
Basic statistical analysis and presentation were performed with Excel 2003 (Microsoft Corporation, Redman, WA) and SigmaPlot (Systat Software, Inc., Richmond, CA). Because of a poor fit with the conventional one-hit model described above, with the assumption that all virus-containing particles have the same UVC sensitivity, we assumed that the distribution of virus UVC susceptibilities follows a log-normal distribution with a geometric mean zg and a geometric standard deviation σg as described by the formula
 |
where CUV/CnoUV is the ratio of the concentration of virus plaques with the UVC on to the concentration of virus plaques with the UVC off, z is the UVC susceptibility (meters squared per joule), and D is the UVC dose in joules per meter squared. The model was fitted in R (version 2.0.1.) by minimizing the sum of squared errors and confidence limits determined from the bootstrap standard error from 500 samples of the residuals. To determine whether RH and suspending medium had significant effects on the sensitivity curves for vaccinia virus aerosols exposed to UVC, we performed likelihood ratio tests consistent with the least-squares procedure, assuming lognormal errors, to determine whether separate models at each level of RH and suspending medium fit the data significantly better than using fewer models to fit only the effects of RH, suspending medium, or all of the data without stratification.
RESULTS
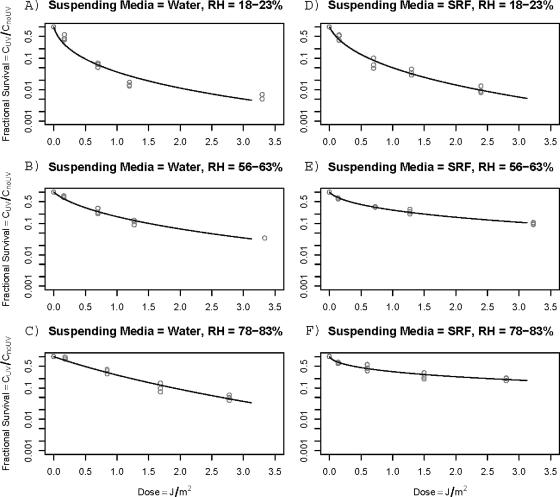
The average airborne concentration of virus in the chamber was 644 plaque-forming viruses per liter of air, which corresponded to 90,860 plaques per filter. With the described bench top chamber, we measured vaccinia virus inactivation levels ranging from 5 to 99.5% by comparing samples with the UV light on to subsequent control samples with the UV light off. The coefficients of variation between triplicate experiments ranged from 0.03 to 0.4, with a median of 0.17. The fractional survival of vaccinia virus suspended in either water or SRF and aerosolized at low (18 to 23%), medium (58 to 63%), and high (78 to 83%) RHs is shown in Fig. 2. Survival decreased with increasing UVC doses under all of the circumstances tested. The z values for vaccinia virus determined by assuming first-order decay rates (data not shown) were in general agreement with the trends seen when using a model assuming a log-normal distribution of z values for susceptibility. However, dose-response plots generally show a significant nonlinear component and a poor fit when using a first-order decay (Fig. 2). When we assumed that virus susceptibility follows a log-normal distribution, we obtained reasonable fits to the data (Fig. 2A to F).
FIG. 2.
UVC susceptibilities of vaccinia virus aerosols suspended in either water or SRF at 18 to 23%, 58 to 63%, and 78 to 83% RH.
The geometric mean (Zg), geometric standard deviation (σg), and 95% confidence intervals for log-normally distributed Z values for UVC susceptibility of airborne vaccinia virus are shown in Table 1. The geometric mean Z values ranged from 9.48 to 1.42, with the highest Z values associated with low (18 to 23%) RHs and the lowest Z values associated with high (78 to 83%) RHs. The overall effects of RH (P < 0.0001) and the suspending medium (P = 0.014) were statistically significant. Controlling for the suspending medium, RH remained a significant factor (P < 0.0001), and the effect of the suspending medium was significant overall (P < 0.0001) after controlling for RH. However, the suspending medium did not have a significant effect at low RHs (P = 0.12), although the suspending medium significantly altered the shape (σg) of the curve at moderate and high RHs (both P < 0.0001).
TABLE 1.
Log-normally distributed Z values for UV susceptibility of airborne vaccinia virusa
| Suspending medium (% RH) | Zg | 95% CI
|
σg | 95% CI
|
||
|---|---|---|---|---|---|---|
| Lower | Upper | Lower | Upper | |||
| SRF (18-23) | 6.16 | 4.27 | 8.89 | 2.65 | 2.13 | 3.52 |
| SRF (58-63) | 1.94 | 1.66 | 2.26 | 4.44 | 3.70 | 5.47 |
| SRF (78-83) | 1.63 | 1.14 | 2.32 | 7.23 | 4.45 | 13.78 |
| Water (18-23) | 9.48 | 5.32 | 16.90 | 3.17 | 2.39 | 4.61 |
| Water (58-63) | 2.54 | 2.05 | 3.16 | 2.64 | 2.13 | 3.48 |
| Water (78-83) | 1.42 | 1.15 | 1.75 | 1.65 | 1.11 | 10.12 |
Estimates were fitted to the ratio of on/off plaque counts for each filter pair in each experiment. Confidence intervals (CI) were estimated with 500 bootstrap iterations of sampling from residuals.
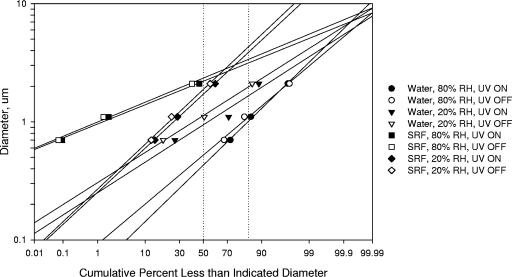
The Andersen sampler was used in conjunction with our UVC testing system to evaluate the influence of particle size on UVC inactivation of vaccinia virus. The UVC dose was delivered at 0.5 J/m2 to ensure that adequate virus numbers would be detected on each stage of the sampler. A comparison of the size distributions of vaccinia virus with the UVC on and off for each RH condition and suspending medium is shown in Fig. 3. If the particle size has an influence on UVC inactivation of virus, the size distribution would be expected to change when UVC was applied. However, The log probability plot shows that the geometric mean (median diameter) and geometric standard deviation (84% diameter divided by the 50% diameter) were very similar for each individual condition, regardless of whether the UV light was on or off.
FIG. 3.
Log probability plot of vaccinia virus aerosol particle size distribution. Vaccinia virus stocks were suspended in either water or SRF and aerosolized, with or without UVC exposure, at low and high RHs. The dotted vertical lines at 50% and 84% are used to determine the median and the geometric standard deviation.
DISCUSSION
We developed a dose-response model for vaccinia virus susceptibility to UVC light and demonstrated that RH significantly affects vaccinia virus susceptibility. This finding confirms that vaccinia virus's sensitivity to UVC is altered in the presence of high RH in a way similar to that of other bioaerosols. This information has not been previously reported for poxviruses and is essential for designing effective interventions with upper-room UVC for reducing exposure to poxviruses as part of a strategy to prevent airborne transmission of smallpox. Both variola virus (the virus which causes smallpox) and vaccinia virus are members of the poxvirus family. These viruses are similar in terms of size, shape, replication, and structure (enveloped, double-stranded DNA, etc.). There is a high degree of conservation of core replication genes for all poxviruses, which makes the molecular details of replication very similar. Vaccinia virus is more closely related to variola virus than to other readily available viruses and poses a reduced risk in the event of inadvertent laboratory exposures compared to other poxviruses.
Edward et al. and Jensen et al. showed that UVC light effectively inactivated vaccinia virus aerosols and suggested that virus inactivation increased for a given UVC irradiance as exposure times increased (2, 10). However, these studies did not establish a dose-response relationship or evaluate the influence of RH. Harper suggested that vaccinia virus aerosols had decreased survival at 80% RH compared to 50 and 20% RH conditions when monitored in a rotating drum over a period of 23 h and show 1 to 2 log10 reductions in infectious virus concentrations without the use of UVC during this time period (7). In our experiments, a moderate UVC intensity (approximately 3.0 J/m2) produced a dose that resulted in a 1- to 2-log10 reduction of the infectious vaccinia virus concentration (Fig. 1) during a 7.6-s exposure. Thus, the use of UVC reduced the survival time of vaccinia virus by a factor of >10,000 over that observed with natural biological decay. The more rapid biological decay of poxvirus aerosols at high RH may offset somewhat the increased resistance to UVC at high RH. The combined effect of UVC and high RH on potential exposure under real-world conditions needs to be studied.
Microorganisms are thought to follow an exponential decay model of survival (Eq. 1) when exposed to disinfection agents such as UVC, heat, ozonation, or ionizing radiation (13). The sensitivity of the organism is defined by the rate constant Z and is thought to be unique to each microbial species and is independent of UVC irradiance (13). Thus, a Z value determined for a given organism under a given exposure condition may be assumed to apply to any exposure conditions to which that organism is subjected. However, our data for vaccinia virus show that the Z value is dependent on UV irradiance and is also influenced by RH. Our data consistently show that there is a steep slope of log inactivation plotted against the UVC dose at low UVC doses, with a gradual decrease in the slope as the UVC dose increases. The deviation from the simple linear model assuming identical Z values for all aerosolized viral particles, indicated by a σg of >1.0, is most pronounced at high RH for vaccinia virus aerosolized in SRF (σg = 7.23) and is least evident at high RH for vaccinia virus aerosolized in water (σg = 1.65). Other investigators have also noted that microorganisms are not necessarily inactivated by UVC light following uniform first-order kinetics. Riley and Kaufman's study on the inactivation of airborne Serratia marcescens by UVC light showed a nonlinear component (19). They theorized that nonlinearity was due to the presence of two families of organisms with different sensitivities to UVC. Ko et al. noted similar trends in their study of the influence of RH on the UV sensitivity of S. marcescens and Mycobacterium bovis (12). Kowalski et al. also referenced the two-stage survival curve in which a small proportion of the population is resistant to UV (13). However, these investigators do not provide a plausible explanation as to why there are only two populations with differing UV sensitivities. It seems reasonable to inquire why there are only two populations rather than many populations that would exhibit a distribution of sensitivities to UV, as is suggested by our data and analysis.
Since environmental data dealing with aerosols and microorganisms are commonly log-normally distributed, we assumed that the distribution of virus UVC susceptibilities follows a log-normal distribution with a geometric mean Zg and a geometric standard deviation σg and fitted our curves accordingly. UVC susceptibility plots show a superior fit when we assume a log-normal distribution of Z values, compared with a linear fit. The apparent distribution of Z values may be due to either the distribution of actual doses delivered to the viruses or inherent differences in the viruses themselves. The former explanation is reasonable since droplets are likely to have a log-normal size distribution and may not dry to a uniform shape or have a uniform UV absorbance or reflectance. Thus, the distribution of z values will be a result of the actual distribution of the total dose received by the virus.
Optical particle counters or aerodynamic particle counters can characterize aerosols with respect to size and number but do not measure biological activity (i.e., infectivity). Our novel use of the Andersen 2000 allowed us to measure the number and size distribution of the virus aerosol, as well as infectivity. In these experiments, the size distributions of airborne vaccinia virus did not shift when the virus was exposed to UVC, regardless of the RH or suspending medium (Fig. 3). This suggests that differences in virus susceptibility to UVC are not directly a function of particle size in this experimental setting. If UVC were a function of particle size, the median diameter and slope of the line would differ between the on and off conditions. Associations between UV susceptibility and particle size have not been reported for vaccinia virus or other viruses, but studies of bacteria have shown that UVC susceptibility decreases as particle size increases (14).
We also considered that the physical layout of the UVC exposure chamber may have resulted in a distribution of UVC doses to the viruses. However, the chamber was designed to provide uniform doses by eliminating shadow-causing overhangs and using a multilamp fixture which was greater in area than the quartz window of the exposure chamber and mounted well above the window. Furthermore, we do not think that edge effects (regions of low flow near walls and corners) affect the log-normal distribution of virus sensitivity to UVC because these effects are constant and would not vary with the RH and suspending medium. Furthermore, the use of sample pairs consisting of a sample with the UV lights on followed by a sample with the UV lights off controlled for losses associated with the chamber design, sampling method, daily nebulizer output, etc. Thus, any changes in virus survival not attributed to UV would be equivalent in both the on and off samples.
Alternatively, if the particles have uniform properties such that each virus in the aerosol receives the same dose, then the distribution of z values may be a function of the makeup of the individual viruses. This is not unreasonable since at the time of harvest the viruses recovered after sonically disrupting cells are likely in various stages of assembly. Furthermore, the assembly process is not perfect and may lead to morphological heterogeneity of the viruses. These differences, in turn, will likely affect the UV absorbance and reflectivity of the virus itself. These morphological differences may also degrade the general fitness of the virus and increase its susceptibility to the effects of UVC such as the formation of photodimers or the ability to be repaired by host repair mechanisms. This is an area where further study is needed. Neither of the two possible explanations for heterogeneous UVC susceptibility, variation of physical particle characteristics and of viral particle assembly, requires genetic variation within the virus strain used for these experiments. Genetic variation in susceptibility, for example, through differences in repair capability, could explain the apparent heterogeneity of z values. However, the large effect of particle composition and RH on the extent of heterogeneity and the relative genetic uniformity of the WR vaccinia virus strain indicates that the physical properties of the particles or random variations in viral assembly are more likely explanations for heterogeneous Z values.
We find that simple first-order models do not account for the decay of poxvirus infectivity in the presence of UV light and that RH plays an important role in modifying the susceptibility of poxvirus to UVC. This finding is especially important for reducing exposures to smallpox by using UVC in the “real world,” where the RH varies as a function of season, temperature, and geographic region. We describe a new model that has a strong biological rationale and gives a good fit to the observed decay curves for vaccinia virus. Models of upper-room UVC air disinfection, such as that described by Brickner et al. (1), are not relevant to our study and are not generally useful because of the many arbitrary assumptions used in these models. We determined the parameters of this model under a range of conditions which showed reduced virus susceptibility at moderate RH levels (40 to 60%) commonly found in climate-controlled indoor settings. Virus susceptibility to UVC will be even greater, and require a correspondingly higher UVC dose, at locations in many parts of the world where the RH is high and RH controls are not available. With these results, designers of air disinfection systems, whether using in-duct or upper-room UVC, will now be able to input our equations into fluid dynamic models to accurately estimate the efficacy of poxvirus inactivation under various RH conditions. Further studies are needed to examine the actual effectiveness of such systems and how well the model parameters provided here serve to predict system performance with respect to the control of exposure to poxviruses used as biothreat agents.
Acknowledgments
We thank Andrew Spielman and Richard Pollack, Harvard School of Public Health, for their expertise and advice regarding virology and cell culture methods and for reviewing the manuscript and Thomas Monath and Acambis, Inc., for generous donation of viral strains and assistance with the production of virus for this work.
This work was supported by National Institute of Allergy and Infectious Diseases grant R21 A1053522 from the National Institutes of Health.
Footnotes
Published ahead of print on 20 July 2007.
REFERENCES
- 1.Brickner, P. W., R. L. Vincent, M. First, E. Nardell, M. Murray, and W. Kaufman. 2003. The application of ultraviolet germicidal irradiation to control transmission of airborne disease: bioterrorism countermeasure. Public Health Rep. 118:99-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Edward, D., W. Elford, and P. Laidlaw. 1943. Studies of air-borne virus infections. J. Hyg. 43:1-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eubank, S., H. Guclu, V. S. Kumar, M. V. Marathe, A. Srinivasan, Z. Toroczkai, and N. Wang. 2004. Modelling disease outbreaks in realistic urban social networks. Nature 429:180-184. [DOI] [PubMed] [Google Scholar]
- 4.First, M. W., R. A. Weker, S. Yasui, and E. A. Nardell. 2005. Monitoring human exposures to upper-room germicidal ultraviolet irradiation. J. Occup. Environ. Hyg. 2:285-292. [DOI] [PubMed] [Google Scholar]
- 5.Gani, R., and S. Leach. 2001. Transmission potential of smallpox in contemporary populations. Nature 414:748-751. [DOI] [PubMed] [Google Scholar]
- 6.Halloran, M. E., I. M. Longini, Jr., A. Nizam, and Y. Yang. 2002. Containing bioterrorist smallpox. Science 298:1428-1432. [DOI] [PubMed] [Google Scholar]
- 7.Harper, G. J. 1961. Airborne micro-organisms: survival tests with four viruses. J. Hyg. 59:479-486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Henderson, D. A., T. V. Inglesby, J. G. Bartlett, M. S. Ascher, E. Eitzen, P. B. Jahrling, J. Hauer, M. Layton, J. McDade, M. T. Osterholm, T. O'Toole, G. Parker, T. Perl, P. K. Russell, and K. Tonat. 1999. Smallpox as a biological weapon: medical and public health management. JAMA 281:2127-2137. [DOI] [PubMed] [Google Scholar]
- 9.Jackson, R. J., A. J. Ramsay, C. D. Christensen, S. Beaton, D. F. Hall, and I. A. Ramshaw. 2001. Expression of mouse interleukin-4 by a recombinant ectromelia virus suppresses cytolytic lymphocyte responses and overcomes genetic resistance to mousepox. J. Virol. 75:1205-1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jensen, M. 1964. Inactivation of airborne viruses by ultraviolet irradiation. Appl. Microbiol. 12:418-420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kethley, T. W., and K. Branch. 1972. Ultraviolet lamps for room air disinfection. Effect of sampling location and particle size of bacterial aerosol. Arch. Environ. Health 25:205-214. [DOI] [PubMed] [Google Scholar]
- 12.Ko, G., M. W. First, and H. A. Burge. 2000. Influence of relative humidity on particle size and UV sensitivity of Serratia marcescens and Mycobacterium bovis BCG aerosols. Tuber. Lung Dis. 80:217-228. [DOI] [PubMed] [Google Scholar]
- 13.Kowalski, W. J., W. P. Bahnfleth, D. L. Witham, B. F. Severin, and T. S. Whittam. 2000. Mathematical modeling of ultraviolet germicidal irradiation for air disinfection. Quant. Microbiol. 2:249-270. [Google Scholar]
- 14.Lai, K. M., H. A. Burge, and M. W. First. 2004. Size and UV germicidal irradiation susceptibility of Serratia marcescens when aerosolized from different suspending media. Appl. Environ. Microbiol. 70:2021-2027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Legrand, J., C. Viboud, P. Y. Boelle, A. J. Valleron, and A. Flahault. 2004. Modelling responses to a smallpox epidemic taking into account uncertainty. Epidemiol. Infect. 132:19-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Meltzer, M. I., I. Damon, J. W. LeDuc, and J. D. Millar. 2001. Modeling potential responses to smallpox as a bioterrorist weapon. Infect. Dis. 7:959-969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rauth, A. M. 1965. The physical state of viral nucleic acid and the sensitivity of viruses to ultraviolet light. Biophys. J. 5:257-273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Riley, R. L. 1974. Airborne infection. Am. J. Med. 57:466-475. [DOI] [PubMed] [Google Scholar]
- 19.Riley, R. L., and J. E. Kaufman. 1972. Effect of relative humidity on the inactivation of airborne Serratia marcescens by ultraviolet radiation. Appl. Microbiol. 23:1113-1120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tseng, C. C., and C. S. Li. 2005. Inactivation of virus containing aerosols by ultraviolet germicidal irradiation. Aerosol Sci. Technol. 39:1136-1142. [Google Scholar]
- 21.Wehrle, P. F., J. Posch, K. H. Richter, and D. A. Henderson. 1970. An airborne outbreak of smallpox in a German hospital and its significance with respect to other recent outbreaks in Europe. Bull. W. H. O. 43:669-679. [PMC free article] [PubMed] [Google Scholar]
- 22.Xu, P., E. Kujundzic, J. Peccia, M. P. Schafer, G. Moss, M. Hernandez, and S. L. Miller. 2005. Impact of environmental factors on efficacy of upper-room air ultraviolet germicidal irradiation for inactivating airborne mycobacteria. Environ. Sci. Technol. 39:9656-9664. [DOI] [PubMed] [Google Scholar]
- 23.Xu, P., J. Peccia, P. Fabian, J. W. Martyny, K. P. Fennelly, M. Hernandez, and S. L. Miller. 2003. Efficacy of ultraviolet germicidal irradiation of upper-room air in inactivating airborne bacterial spores and mycobacteria in full-scale studies. Atmos. Environ. 37:405-419. [Google Scholar]