INTRODUCTION
The enactment of the Human Tissue Act (2004) has had a significant impact. In this commentary, we look at the legislation in terms of anatomical teaching and in doing so raise awareness of the importance of body bequeathal to medical teaching.
Following events at Alder Hey and the Bristol Royal Infirmary, in which it was revealed that there had been violations of the Human Tissue Act 19611, the UK government responded by initiating the so-called Kennedy2 and Redfern3 enquiries at the Bristol Royal Infirmary and Royal Liverpool Children's Hospital and the Northern Ireland equivalent O'Hara Inquiry4. All three enquiries found that the current law was not comprehensive or internally consistent for either professionals or families involved5.
September 1st 2006 marked the enactment of the new Human Tissue Act (2004) legislation. This Act has far reaching implications for Clinical researchers, Pathologists, Anatomists and Surgeons. Many saw the bureaucratic burden that the new legislation imposed as both unhelpful and unwieldy. For example, the Human Tissue Authority (HTA) has stipulated that all activities are documented and followed within the framework of Standard Operating Procedures (SOPs) and Service Level Agreements (SLAs).
Perhaps the most significant change in the legislation concerned obtained consent for examination and retention of human tissue for scheduled purposes (research, transplantation, education and training). This was because removal, storage and use of organs and tissues from adults and children without proper consent were the issues that created the most public concern. The Act clearly defines appropriate consent as well as who may give it and makes it unlawful to use bodies or human material for purposes other than that for which they were consented.
HUMAN TISSUE AUTHORITY (HTA)
The HTA was established as the regulatory authority to oversee all activities which fall within the scheduled purposes. The removal, storage, use and disposal of human material have been codified by the HTA in terms of both Codes of Practice and Standard Operating Procedures (SOPs). It is hoped that this regulatory authority, by making consent the fundamental principle in the use of human tissue, will provide the necessary reassurance to the public. The HTA has issued specific codes of practice for all scheduled purposes, anatomical examination falling within the remit of education and training. This is somewhat paradoxical: anatomical examination comes under this regulatory authority for obvious reasons, but has been stringently regulated since the 1800s when grave-robbing was used as a way of supplying cadavers to medical schools6.
ANATOMICAL LEGISLATION
The Anatomy Acts of 1832, 1871 and 1984
The part of the Act dealing with the activities associated with the traditional dissecting room, so-called ‘anatomical examination’, dates back over 170 years when it was argued that “a knowledge of the causes and nature of sundry diseases which affect the body and of the best methods of treating and curing such diseases and the healing and repairing diverse wounds and injuries to which the human frame is liable cannot be acquired without the aid of anatomical examination” The Anatomy Act, 1832. Whilst this assertion is still widely accepted, particularly by medical schools in Great Britain and Ireland where the majority still continue with cadaveric dissection, there are some who argue that there are alternative ways to obtain the necessary knowledge7.
THE ANATOMY ORDER (NORTHERN IRELAND) 1992
In England and Wales the 2004 Human Tissue Act replaced the Anatomy Act of 1984, whilst in Northern Ireland it superseded the Anatomy (Northern Ireland) Order 1992. Why the 1984 legislation was not extended to Northern Ireland is something of a mystery, as there was an eight year period in which legislatively the Anatomists in Northern Ireland continued to work under the Anatomy Act of 1832 and 1871 (this later amendment of the 1832 Act was simply to make it lawful “for one of Her Majesty's Principal Secretaries of State in that part of the United Kingdom called Great Britain, and for the Chief Secretary for Ireland in that part of the United Kingdom called Ireland, from time to time, by order, to vary the period limited by section thirteen of the recited Act as the time within which certificates of interment are to be transmitted to the inspectors of districts” (copy of the Anatomy Act (1832) Amendment Chapter 16 generously provided by Parliamentary Archives, Houses of Parliament, London). Comparison of the Anatomy (Northern Ireland) Order 1992 with the Anatomy Act (1984) reveals that they were essentially the same: the criterion for accepting a bequest of a body was simply “if a person, either in writing at any time or orally in the presence of two or more witnesses during his last illness, has expressed a request that his body be used after death for anatomical examination". Similarly, the retention of parts of the body after the anatomical examination had been concluded was the same - there was a ‘statutory period’ of three years from the date of the donor's death. In both the Anatomy (Northern Ireland) Order 1992 and the Anatomy Act (1984) there was provision for the “surviving spouse or any other surviving relative of the deceased” to object to either the body being used for anatomical examination or the retention of body parts after the three year statutory period. The vagueness of this legislation led to problems for Medical Schools governed by the 1984 Act in terms of receiving bodies when there was only oral instruction on the part of the donor and disagreement within a family (in one instance the donor's wife expressed different views from those of his daughter from the first marriage). In the Human Tissue Act (2004) there is a hierarchy of qualifying relationships ranked with regard to provision of consent, so that the primacy of wishes can be determined. For example, a spouse or partner is ranked higher than a parent or child, who in turn is ranked higher than a brother or sister. The 1992 Order required written donor and witness signatures for both donation and wishes concerning retention after the statutory period.
Another feature of the 1992 Order was that it was interpreted to allow for the use of cadavers for surgical training purposes. This facility, although not extensively used, was important in that it allowed surgeons to research different approaches to procedures without putting patients at risk.
BODY DONATION IN NORTHERN IRELAND
Over the years, Anatomy in The Queen's University of Belfast has observed wide fluctuations in the number of bodies received for anatomical examination. Preliminary analysis of the numbers of bequeathals grouped in 5 year periods has revealed that between 1957 and 1962 only 55 were accepted from Northern Ireland whereas in the period 1977-1982, 196 bequeathals were accepted. The average student numbers annually (medical and dental combined) for these periods were 95 and 191 respectively.
The academic year 2005/2006 marked the first of the expanded medical student numbers with the intake of medical and dental students rising to 313 Whilst student numbers have increased, the number of bequeathals over recent months has declined. This prompted a press release from the then Inspector of Anatomy at the behest of the University to inform the public of the shortage of bodies for undergraduate teaching. She stated that “the successful training of doctors and dentists depended on body donation”8. By increasing the awareness of the importance of dissection for the successful training of doctors and dentists it is hoped that this will encourage individuals to consider making such a bequeathal. This issue is not new nor is it just a regional problem.
Records in the Department have revealed that in the early 1970s, the issue of body donation for dissection was discussed in the local press by the Professor of Anatomy at the time, Professor Jack Pritchard, who stated “The body is extremely useful for medical research and teaching. We can't teach our medical students without bodies”. Medical Schools in England and Wales have also witnessed a reduction in the number of bodies available for undergraduate and postgraduate teaching9.
As anatomists, we consider it essential that medical and dental students develop a sound knowledge and understanding of anatomy and anatomical relations, and the most successful way of achieving this is to dissect (fig 1). However, it is recognised that such an assertion regarding the value of dissection as a teaching method in gross anatomy lacks objective evidence10. Dissection also gives students the opportunity to observe pathological conditions, anatomical abnormalities and variations11. This need has become even greater since the General Medical Council's document Tomorrow's Doctors (1993) led to a reduction in anatomy teaching time in many medical schools. At Queen's, the difference between the old and new curricula (pre and post 1996) saw a reduction from 384 hours in the old course to 183 hours of anatomy in the new integrated course12. As a consequence, the authors found that the knowledge of surface anatomy of graduating doctors' was reduced. The knock-on effect of this has been increased demand for access to cadaveric specimens for postgraduate trainees. To meet these demands the Royal College of Surgeons of England is currently exploring the feasibility of establishing generic core skills courses throughout the UK.
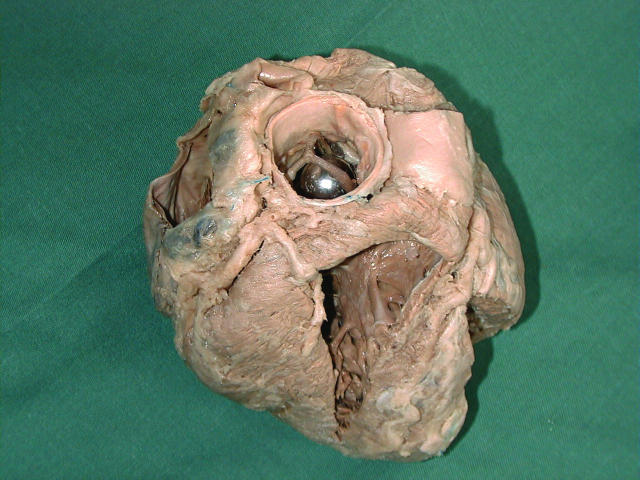
Fig 1.
Retained heart specimen, plastinated as per the work of Gunther von Hagens. Of particular interest is the aortic valve replacement.
REGULATORY AUTHORITY FOR TISSUES AND EMBRYOS (RATE)
It seems that the HTA will be a transitory structure as it is to be combined with the Human Fertilisation and Embryo Authority (HFEA, established in 1991) to become the Regulatory Authority for Tissue and Embryos (RATE)13. This single Authority will also take responsibility for the regulation of the supply of blood and blood products, formerly the remit of the Medicines and Healthcare Products Regulatory Agency. The provisional timetable for the formation of this single Authority is suggested as 2008, but will depend on the need for primary legislation. In doing so, the Government argues that it will bring convergence to all regulatory aspects dealing with human biological tissues.
We hope this brief account raises awareness of the important issues – the new regulatory framework imposed by the Human Tissue Act (2004) and secondly, the importance of dissection and thus body bequeathal to the training of future doctors and other health professionals.
Acknowledgments
We would like to thank Dr Tracey Wilkinson for her constructive comments and suggestions to improve this commentary. The authors have no conflict of interest.
REFERENCES
- 1.Bauchner H, Vinci R. What have we learnt from the Alder Hey affair? That monitoring physicians' performance is necessary to ensure good practice. BMJ. 2001;322(7782):309–10. doi: 10.1136/bmj.322.7282.309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kennedy I. Learning from Bristol: the report of the public inquiry into children's heart surgery at the Bristol Royal Infirmary 1984-1995. Bristol: Bristol Royal Infirmary Inquiry; 2001. [DOI] [PubMed] [Google Scholar]
- 3.Redfern M. The report of the Royal Liverpool Children's Inquiry. London: House of Commons; 2001. [Google Scholar]
- 4.O'Hara J. Human organs inquiry report. Belfast: Department of Health, Social Services and Public Safety; 2002. [Google Scholar]
- 5.Explanatory notes to Human Tissue Act 2004: Chapter 30. London: Department of Health; 2004. [Google Scholar]
- 6.Lee K, McDonald SW. Not modern-day body-snatching: the response of the public. Scot Med J. 2002;47(3):66–70. doi: 10.1177/003693300204700307. Available from: http://www.smj.org.uk/0602/organ.htm. Last accessed May 2007. [DOI] [PubMed] [Google Scholar]
- 7.McLachlan JC, Bligh J, Bradley P, Searle J. Teaching anatomy without cadavers. Med Educ. 2004;38(4):418–24. doi: 10.1046/j.1365-2923.2004.01795.x. [DOI] [PubMed] [Google Scholar]
- 8.University ‘wants your body’. BBC News. 2006 Oct 06; Available from: http://news.bbc.co.uk/1/hi/northern_ireland/5410930.stm. Last accessed May 2007.
- 9.More body donations needed to sustain medical education, training and research. London: Department of Health; 2007. [Google Scholar]
- 10.Winkelmann A. Anatomical dissection as a teaching method in medical school: a review of the evidence. Med Educ. 2007;41(1):15–22. doi: 10.1111/j.1365-2929.2006.02625.x. [DOI] [PubMed] [Google Scholar]
- 11.Ellis H. Teaching in the dissecting room. Clin Anat. 2001;14(2):149–51. doi: 10.1002/1098-2353(200103)14:2<149::AID-CA1023>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 12.McKeown PP, Heylings DJ, Stevenson M, McKelvey KJ, Nixon JR, McCluskey DR. The impact of curricular change on medical students' knowledge of anatomy. Med Educ. 2003;37(11):954–61. doi: 10.1046/j.1365-2923.2003.01670.x. [DOI] [PubMed] [Google Scholar]
- 13.Human tissue and embryos bill: key benefits. London: Office of the Leader of the House of Commons; 2007. Government Bills 2006/07 – draft bills. [Google Scholar]