Abstract
Background
Requests for troponin T, a biomarker for myocardial infarction, may be sent in a variety of clinical situations. In most cases, a single sample 12 hours or more after symptom onset should be sufficient for diagnosis. We chose to investigate how troponin T testing is used in our hospital with emphasis on those who had serial rather than single troponin measurements during their hospital stay.
Methods
Prospective survey of 50 patients with serial troponin T requests out of a total of 321 patients who had troponin T levels measured during the same time period.
Results
The time of symptom onset could be clearly identified in 40/50 patients. In 22 of these the first troponin was taken prior to 12 hours after symptom onset. For the 18 patients whose first troponin was taken after 12 hours, the second result remained in the same category (normal or high) as the first in all cases. This was not the case for 3/10 patients whose first troponin was sent within 12 hours and was normal. Early troponin results rarely affected immediate patient management and did not inform decisions about fibrinolytic therapy.
Conclusions
Serial troponin testing was most commonly due to a sample being sent within 12 hours of symptom onset or to unnecessary repetition of an appropriately timed sample. Patient management was rarely enhanced by early troponin testing.
Keywords: Troponin T usage, Myocardial Infarction
INTRODUCTION
Recent years have seen increasing use of troponin testing in the setting of acute chest pain. The sensitivity and specificity of troponin release as a marker of myocardial necrosis are such that the definition of acute myocardial infarction (AMI) has been rewritten to include troponin levels1. There has also been debate about diagnostic cut-off values and the clinical relevance of “borderline” troponin elevations2,3, which may be found in the absence of classical symptoms of cardiac ischaemia or electrocardiographic (ECG) changes in patients who are unwell for some other reason. Guidelines emphasise that a troponin result should be interpreted in the clinical context and should be timed1. Troponin may not start to rise for several hours after symptom onset and although a raised troponin when the patient is first seen can be used to “rule in” AMI, there is some disparity in the recommended protocols for optimal timing of further samples if the initial one is negative4. However, both European and American guidelines agree that a normal troponin 12 hours after symptom onset excludes AMI5,6.
On the basis of anecdotal observations of repeated troponin samples in the same patients, and reports of delay in some results becoming available, we chose to investigate how troponin is used in clinical practice in our hospital. A preliminary analysis showed that during a single month (October 2004) 501 patients had a single troponin T request and 167 had two or more. We decided to investigate prospectively the group of patients who had multiple requests during the same admission to answer the following questions:
In patients who have serial troponin requests, how are they timed in relation to patient presentation?
If an early measurement taken at presentation is normal is a second 12-hour test arranged?
How long is the average period of time between venepuncture and a clinician seeing the result?
Do early troponin results influence immediate clinical management?
METHODS
During the first 18 days of May 2005, on each weekday morning all troponin T requests from the previous 48 hours were reviewed and any patient having two or more tests were identified. Each of these patients was visited by one of the clinicians participating in the study (BL, JM or RS) and their medical notes were reviewed with a data collection sheet designed to answer the questions above. The time taken to transport the samples to the laboratory, time between laboratory receipt of the sample and report of the result, and time to look-up were obtained from the data trail on the laboratory computer system. Troponin T is measured using the Elecsys assay (Roche Diagnostics) and is available as a stat test 24 hours a day. The upper reference limit is 0.03 μg/L.
RESULTS
During the survey period, 68 patients were identified who had at least two troponin T samples sent during a single hospital admission. Complete clinical data were available for 50 and these form the study population. The total number of patients for whom troponin T requests were processed during the survey was 321.
The majority (33/50) of those who had serial troponin requests were new patients presenting via the Emergency Department (ED). First assessment of these patients was split evenly between the hospital's team of specialist chest pain nurses who are called to the ED to see any patient with acute chest pain, and ED senior house officers who tended to see patients with alternative presenting symptoms such as dyspnoea. Presenting symptoms are detailed in Table I. The remainder were inpatients on a variety of wards throughout the hospital and were assessed first by junior doctors on those wards. Out of the 50 patients with serial requests, we noted one with a working diagnosis of ruptured abdominal aortic aneurysm and another of status epilepticus. Forty-eight had ECG's recorded on initial presentation.
Table I.
Main presenting symptoms (patients may have had more than one symptom)
| Symptom | Number of patients (n/50) |
|---|---|
| Chest pain | 30 |
| Dyspnoea | 10 |
| Dizziness / collapse | 8 |
| Abdominal / back pain | 6 |
| Vomiting | 2 |
| None of these | 5 |
In 10 of 50 patients with serial samples the time of symptom onset could not be clearly identified. Of the remaining 40, 22 had their first sample taken within 12 hours of symptom onset and 18 had it performed after 12 hours (figure 1). Of these 18, eight were patients with chest pain who did not present until after 12 hours.
Fig 1.
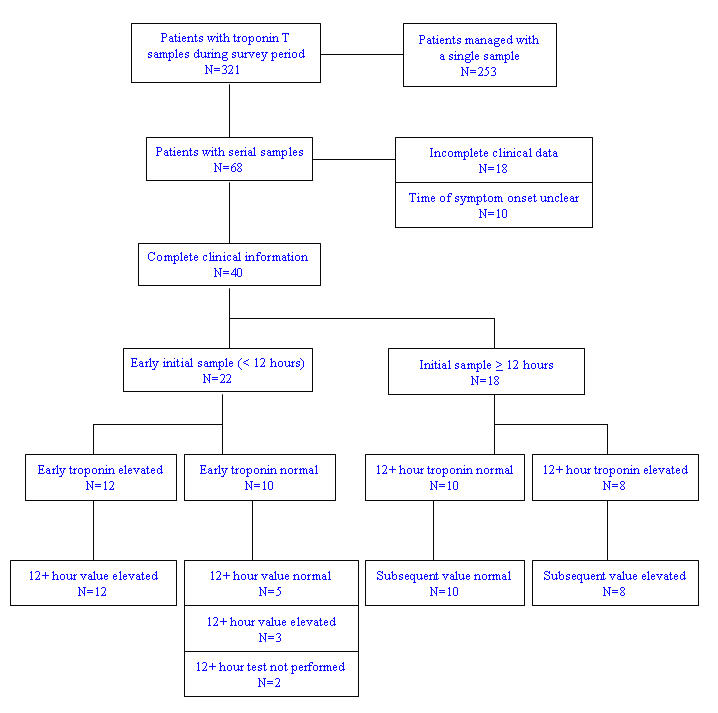
Flowchart illustrating usage of troponin T during survey period
Of the 22 patients whose first troponin was taken early (within 12 hours of symptom onset), 12 had elevated results. Eight of these were assessed by or discussed with the cardiology team and three were admitted to monitored cardiac beds. Two patients received fibrinolytic therapy, in both cases before the troponin T result had been seen.
In the 18 patients whose first sample was sent 12 hours or more after symptom onset, 10 had values below the reference limit and eight were high. In all 18 cases the second troponin result was in the same category (normal or high) as the first.
Seventeen of the hundred samples included in this audit were not labelled with the time of venepuncture. Those samples that were timed took a median time of 57 minutes to be transported to the laboratory (interquartile range 36-73 minutes). The median time taken for the laboratory to process a sample and release the result was 50 minutes (interquartile range 41-67 minutes), and the subsequent median time taken for non-laboratory staff to view the result on the computer system was 81 minutes (interquartile range 16-184 minutes). This excludes one telephoned result and ten results which were not looked up within 12 hours of becoming available. If these results and the untimed samples are excluded, the median total time between venepuncture and non-laboratory staff viewing the result was 221 minutes (interquartile range 118-306 minutes).
DISCUSSION
This survey provides an overview of how one of the most high profile and high-growth tests of recent years is used in clinical practice. Most patients for whom the test is requested are managed with a single sample. However a substantial minority (68/321; 21%) had two or more samples sent during a single hospital admission and these patients were the focus of the current survey to determine the clinical value of serial troponin sampling.
Early troponin requesting (within 12 hours) was a common reason for duplicate samples being performed. Of 22 patients with early samples sent, we observed three in whom clinical management was potentially affected by the result of the early sample. Early troponins may be used as part of an investigation protocol for chest pain such as the Sheffield protocol7, which recommends a single troponin measurement at 6 hours. This protocol however also involves continual ECG monitoring and exercise stress testing and as such is applicable to specialist chest pain units rather than general medical take-in through the ED. An early level is of value if it rules in AMI in a patient whose clinical findings and ECG are equivocal, thereby facilitating earlier management. However we found that no patient received earlier thrombolytic therapy because of an early troponin T result and that only a minority (3/12) of patients who had a positive early troponin were immediately transferred to monitored cardiac beds. Such observations raise questions about the clinical value of early troponin testing, including in patients in whom it is found to be elevated.
In cases of serial troponin samples another question of interest is whether both are necessary. Guidelines state that in certain equivocal cases it is useful to demonstrate a rise and fall in troponin in order to diagnose an acute episode of cardiac ischaemia1. However this indication for serial testing refers to atypical cases rather than the majority and is unlikely to explain many of the serial troponin samples that we observed. There is always a degree of redundancy in requesting with any diagnostic test but it is a particularly relevant issue where troponin is concerned given that chest pain is a common and important presenting symptom in the ED. Furthermore troponin workload is difficult for laboratories to manage, as it is perceived that troponin measurements cannot be delayed or repeat troponin requests declined by the laboratory without the risk of harmful consequences to patients. However we did find that the problem of repeated troponin samples was less than it had appeared prior to the survey. We also found that although laboratory turnaround time for troponin is higher than ideal, it comprised under a quarter of the median total length of time between venepuncture and a clinician viewing the result.
Among 18 patients with serial troponin samples whose initial sample had been sent at least 12 hours from symptom onset, the subsequent result remained in the same category in every case. This is a reassuring finding and underscores the reliability of the 12 hour troponin sample and the predictive value of this troponin T assay in clinical practice. In contrast among 10 patients whose early troponin level was normal, the 12 hour result was elevated in 3, highlighting the potential for diagnostic error when troponin levels are measured within 12 hours of symptom onset.
The optimal role for troponin T sampling in the assessment of suspected acute ischaemic chest pain is as a single sample 12 hours (or later) from the onset of symptoms. We found that early samples rarely affected immediate patient management and did not inform decisions about fibrinolytic therapy. Samples taken 12 hours or more after symptom onset do not need to be repeated in the absence of further ischaemic symptoms.
The authors have no conflict of interest.
REFERENCES
- 1.Joint European Society of Cardiology/American College of Cardiology Committee. Myocardial infarction redefined – a consensus document for the redefinition of myocardial infarction. Eur Heart J. 2000;21(18):1502–13. doi: 10.1053/euhj.2000.2305. [DOI] [PubMed] [Google Scholar]
- 2.Collinson P. The British Cardiac Society on the redefinition of myocardial infarction: a basis for discussion. Ann Clin Biochem. 2004;41(Pt 4):258–9. doi: 10.1258/0004563041201608. [DOI] [PubMed] [Google Scholar]
- 3.Fox KA, Birkhead J, Wilcox R, et al. British Cardiac Society Working Group on the definition of myocardial infarction. Heart. 2004;90(6):603–9. doi: 10.1136/hrt.2004.038679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hamm CW. Cardiac biomarkers for rapid evaluation of chest pain. Circulation. 2001;104(13):1454–6. [PubMed] [Google Scholar]
- 5.Bertrand ME, Simoons ML, Fox KA, Wallentin LC, Hamm CW, McFadden E, et al. Management of acute coronary syndrome in patients presenting without persistent ST-elevation. Eur Heart J. 2002;23(23):1809–40. doi: 10.1053/euhj.2002.3385. [DOI] [PubMed] [Google Scholar]
- 6.Braunwald E, Antman EM, Beasley JW, Califf RM, Cheitlin MD, Hochman JJ, et al. ACC/AHA guidelines for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction: executive summary and recommendations. Circulation. 2000;102(10):1193–209. doi: 10.1161/01.cir.102.10.1193. [DOI] [PubMed] [Google Scholar]
- 7.Goodacre S, Morris FP, Campbell S, Arnold J, Angelini K. A prospective observational study of a chest pain observation unit in a British hospital. Emerg Med J. 2002;19(2):117–21. doi: 10.1136/emj.19.2.117. [DOI] [PMC free article] [PubMed] [Google Scholar]


