Abstract
Mild cognitive impairment (MCI) was proposed as a nosological entity referring to elderly people with mild cognitive deficit but no dementia. MCI is a heterogeneous clinical entity with multiple sources of heterogeneity. The concept of MCI was reviewed and a diagnostic procedure with three different stages was proposed by the European Consortium on Alzheimer's Disease Working Group on MCI. Firstly, MCI should correspond to cognitive complaints coming from the patients or their families; the reporting of a relative decline in cognitive functioning during the past year by a patient or informant; cognitive disorders as evidenced by clinical evaluation; absence of major repercussions on daily life; and absence of dementia. These criteria, similar to those defined during an international workshop in Stockholm, make it possible to identify an MCI syndrome, which is the first stage of the diagnostic procedure. Secondly, subtypes of MCI had to be recognised. Finally, the aetiopathogenic subtype could be identified. Identifying patients at a high risk for progression to dementia and establishing more specific and adapted therapeutic strategies at an early stage, together with more structured overall management, is made possible by the diagnostic procedure proposed.
The concept of mild cognitive impairment (MCI), developed by Petersen et al1 at the end of the 1990s, covers the discipline of cognitive ageing. Numerous attempts have been made in recent decades to classify the boundaries between normal and pathological ageing.2 A common denominator may be isolated for all the different definitions that fall within the context of the cognitive evaluation of physiological or normal ageing. Cognitive disorders, whether about the memory domain or, more broadly, about other cognitive functions, are perceived to be related to or associated with ageing. The potential causal disorders, whether or not they correspond to dementia in nature, are dismissed. The concept of MCI was proposed to fill the gap between normal and dementia‐type pathological ageing.1,2 The concept of MCI assumes that a cognitive continuum exists between normality and Alzheimer's disease, the main cause of dementia. The criteria for MCI, as defined by Petersen et al in 1997, include the following: (1) memory problems, (2) objective memory disorder, (3) absence of other cognitive disorders or repercussions on daily life, (4) normal general cognitive function and (5) absence of dementia. In 1997, the emphasis was on the compulsory presence of memory problems and memory disorder. In 1999 these criteria were clarified, with MCI defined solely in clinical terms.3 The absence of impaired cognitive function in a domain other than memory is also required. The tests are not specified. Memory tests claim 1.5 standard deviation (SD) below normative values. It is important to emphasise that the 1.5 SD proposed was for a group of people considered to be a whole. The 1.5 SD limit was strictly not to be applied on an individual basis. MCI corresponds to stage 0.5 on the Clinical Dementia Rating Scale.4 The concept of MCI made it possible to define a group of patients at a high risk of developing dementia, particularly Alzheimer‐type dementia. The definition by Petersen, however, has been criticised for being tautological. When the concept of MCI is restricted to only memory disorder, defined on the basis of tests generally used for the early diagnosis of Alzheimer's disease, it leads to the identification of people at a high risk of progression to Alzheimer's disease. The diverse presentations of a patient's symptoms encountered in a clinical context led Petersen et al3 to propose an extension of the concept. Petersen5 then repeated the detailed breakdown in MCI. This syndrome‐type classification, based on the clinical evaluation, is associated with different categories of progression. The neuropsychological profile allows three subtypes of MCI to be distinguished: (1) amnestic MCI, which is said to progress preferentially to Alzheimer's disease; (2) MCI characterised by a slight impairment of multiple cognitive domains (“multiple‐domain slightly impaired”), which may progress to Alzheimer's disease and also to vascular dementia, or may even represent a cognitive ageing process qualified as normal; and (3) MCI corresponding to isolated impairment of a cognitive domain other than of memory (“single‐domain non‐memory MCI”), which may progress to non‐Alzheimer‐type dementia. Although a high proportion of people fulfilling MCI criteria progress to Alzheimer‐type dementia, other types of progression, such as mixed dementia, vascular dementia, Lewy body dementia and focal atrophy, are possible. Moreover, the strict application of the initial definition of MCI was soon shown to be heterogeneous and unstable in terms of progression.6 The heterogeneity aspect includes the clinical presentation, progressive profile and aetiological factors, such as type of degenerative lesions, vascular factors, psychiatric disorders and non‐neurological concomitant diseases. Additionally, the diagnosis of MCI should be made by a specific neuropsychological evaluation, which may be consolidated by paraclinical investigations, laboratory tests and brain imaging.7 The identification of a group of people at risk of developing dementia, and Alzheimer's disease in particular, is of major economic importance, particularly if preventive strategies or therapeutic action are to be developed. This challenge explains the popularity of the concept of MCI and its wide application in the epidemiological, clinical, paraclinical and therapeutic domains.
Body of evidence
The prevalence of MCI and its subtypes varies greatly from one study to another, ranging from 3% to around 17% of elderly people (> 65 years).8 These data largely depend on the diagnostic criteria used and on the type of cohort studied (longitudinal follow‐up of cohorts or memory clinic cohorts). Early studies included amnestic MCI, whereas the more recent studies refer to the wider concept of MCI. Epidemiological studies suggest that the progression of MCI is heterogeneous, and may be reversible, stable or progress to dementia.8,9,10,11,12 Dementia thus usually corresponds to the Alzheimer type.13,14,15 Studies also maintain the heterogeneity of the associated factors. Cerebrovascular factors or psychiatric disorders in particular are commonly observed.
The criteria corresponding to memory problems and absence of repercussions on daily life may be too restrictive, resulting in the underestimation of the prevalence of MCI.16 Lastly, a low positive predictive value of the subtypes of MCI has been recently reported, suggesting that the subtype classification of MCI is of limited clinical relevance.17 The diagnosis of MCI and its subtypes, however, was based on psychometric definitions and not in combination with clinical judgement.
Neuropsychological aspects of the classification of MCI are currently the most poorly defined. Objective cognitive impairment must be diagnosed on the basis of evidence, but no limits have been proposed or should be strictly applied on an individual basis. The diagnosis is made by the doctor. Evaluation by a neuropsychological expert may complete the clinical procedure. Emphasis has recently been placed on the importance of both the doctor's role and clinical judgement.5 The choice of evaluation method varies greatly from one study to another, depending on the type of population analysed (patients originating from specialist consultations or cohorts) and also on the objectives of the study. “All‐purpose” consensus‐based or reference batteries currently do not exist. Measures that were used previously, although imperfect, are those with which neuropsychologists and physicians are more familiar, and the ones most commonly used. The absence of a cut‐off gives rise to a possible overlap between the scores obtained by the so‐called normal people and those obtained by people with MCI. Longitudinal follow‐up of cognitive performance may be more effective and may sometimes prove vital in defining the cognitive status of a person. Some people will regain normal cognitive function, some will remain stable and some will undergo a more or less rapid progression of symptoms (fast and slow decliners). The following predictive criteria have been isolated: age > 77 years, initial Mini Mental State Examination (MMS) < 28, increased impairment of free recall, gradual decline in improvement by indexing, poor performance on the clock test, decline in mental flexibility and sensitivity to interference, and presence of the apolipoprotein E, e4 allele.5,18 The predictive importance of memory decline seen during tests repeated over 2 years, rather than an isolated measurement, has been emphasised.19 The recently described concept of both cognitive and functional decline may be vital in identifying people with MCI at high risk of progression to dementia.20
The concept of MCI was described relatively recently and neuropathological data are still limited. The information provided by cohort studies such as the Religious Order Study will perhaps be the most important findings over the next few years.21 In this study, postmortem examination is systematically carried out, irrespective of cognitive status or cause of death. Neuropathological findings are correlated with results of periodic cognitive evaluation. The clinical and neuropathological criteria distinguishing normal elderly people from those with Alzheimer's disease are, however, still debated. Where should the limit be in terms of neuropathology: should it be qualitative or purely quantitative?22 Most neuropathological data support the concept of a continuum between normal ageing and dementia. MCI may represent a transitional neuropathological condition. Degenerative lesions are also observed in so‐called normal people. Moreover, despite the limited number of published cases, aetiological heterogeneity with respect to vascular lesions and other neurodegenerative disease is apparent.23
Biomarkers are the most widely studied indicators of the existence of specific lesions found in Alzheimer's disease. The essential component of senile plaque is the β amyloid protein and that of neurofibrillary degeneration is hyperphosphorylated τ protein. Numerous studies have been carried out on these pathological proteins, which are potential markers owing to their relationship with the characteristic lesions. Identification of potential biomarkers was focused primarily on analysis of CSF, access to which is limited in standard medical practice with patients with MCI. Nevertheless, three markers (total τ protein, hyperphosphorylated τ protein and amyloid β42 protein) make it possible to distinguish, with adequate sensitivity, patients with incipient Alzheimer's disease or symptomatic Alzheimer's disease in the initial stages from patients undergoing normal ageing or those with depression or Parkinson's disease. Specificity is much lower with regard to other degenerative forms of dementia, such as Lewy body dementia or frontotemporal dementia.24 Moreover, the combination of variables, including genetic data (eg, apolipoprotein E), could accurately predict Alzheimer's disease in people with MCI better than each of the variables individually.25
Although morphological brain imaging is part of the systematic diagnostic procedure for dementia, it is not currently essential for MCI. The diagnostic criteria for MCI are based solely on clinical evaluation. The difficulties in defining the limits of this concept and the need to characterise its different subtypes may necessitate the wider use of imaging in the future.
Brain imaging essentially makes it possible to identify the early stages of Alzheimer's disease, characterising one of the aetiopathogenic subgroups of MCI. This stage of progression is diagnosed by the different localisation of abnormalities in morphological and functional imaging. Different regions may be selected as targets. The entorhinal and hippocampo‐amygdala regions are of greater interest in volumetric analysis, whereas the temporoparietal cortical and posterior cingulate regions are more important in functional imaging.25,26,27,28,29,30 This separation of the morphological and metabolic effects of the lesions may be explained by the existence of compensatory mechanisms that are particularly active in the hippocampus. These compensate for loss of neurones and maintain relative metabolism in this region. The early changes observed in the posterior association cortex are related to a deafferentation mechanism.31 Moreover, positron emission tomography may, in the future, prove to be the most effective tool in detecting microglial activation, regional deposition of β amyloid protein and neurofibrillary tangles.32,33
Discussion
The European Consortium on Alzheimer's Disease Working Group on MCI has recently proposed a novel diagnostic procedure with different stages. Application of the clinical criteria for diagnosis of MCI, as proposed by Petersen et al, varied considerably from one study to another.20 This heterogeneity is related to the actual interpretation of the concept and also to the extensive variations in the methods used. The different studies, nevertheless, made it possible to underline the limitations of the current criteria, which do not allow homogeneous populations to be defined, both in terms of subtypes of MCI and their mode of progression. The diagnostic accuracy of MCI criteria used in drug trials was low to moderate.34 It is none the less essential, above all, to be able to identify patients at a high risk for progression to dementia.5,20 A critical review was recently conducted in Stockholm and then in Montreal, to define a new consensus on MCI.20,35 A modification of Petersen's criteria was proposed during the conference in Montreal. The European Consortium on Alzheimer's Disease Working Group on MCI presented the elements for review; MCI may henceforth correspond to the criteria listed in box 1.
These criteria underline the importance of the clinical evaluation, which combines neuropsychological evaluation and family interview to detect mild cognitive impairment at the earliest possible stage, but above all to identify a decline in cognitive function. The diagnosis is therefore based primarily on the clinical impression and no longer focuses on the memory domain. The cognitive complaint itself has an important role, both in quantitative and qualitative terms. Its prognostic value is, moreover, regularly emphasised. Furthermore, cognitive disorders may have repercussions on complex day‐to‐day activities. Although the concept of slight repercussions is now recognised, the working group acknowledges the absence of adequate tools for its evaluation. Questionnaires evaluating function in the course of the past year or a battery of cognitive tests repeated at 6‐month intervals may be necessary to evidence this decline.
The new criteria make it possible to identify the MCI syndrome in a manner suited to standard medical practice. The following two points may then be reviewed: (1) Which MCI syndrome subtype is involved? (2) Is the underlying aetiopathogenic subtype identifiable?
The syndrome subtype may be recognised as early as the initial evaluation. This may include amnestic MCI, characterised by predominant impairment of the memory domain; or non‐amnestic MCI, characterised by slight impairment of multiple cognitive domains (multiple‐domain MCI); or may correspond to predominant impairment of a cognitive domain other than of memory (single‐domain MCI). The following diagnostic criteria were recently proposed for the identification of pre‐Alzheimer's disease (or prodromal Alzheimer's disease) amnestic MCI: (1) criteria for MCI; (2) evidence of objective memory disorder based on a memory test showing the specificity of amnestic syndrome in Alzheimer's disease—namely, hippocampal amnestic syndrome characterised by a drop in free recall.36 None of the tests, however, are obligatory; likewise, the concept of a cut‐off has been dismissed.35 The diagnosis should not be made only based on restrictive psychometric definitions but in combination with clinical judgement. The psychological and behavioural symptoms should also be taken into account and should not systematically be the exclusion criteria for the diagnosis. Patients may have depressive symptoms related to cognitive impairment or to the underlying process.
Box 1: Criteria for identification of mild cognitive impairment (MCI), given by the MCI Working Group of the European Consortium on Alzheimer's Disease, Brescia Meeting, Italy, June 2005
Cognitive complaints coming from the patients or their families
The reporting of a decline in cognitive functioning relative to previous abilities during the past year by the patient or informant
Cognitive disorders as evidenced by clinical evaluation (impairment in memory or in another cognitive domain)
Absence of major repercussions on daily life (the patient may, however, report difficulties concerning complex day‐to‐day activities)
Absence of dementia
The aetiopathogenic approach follows the syndrome stage. A simple classification, corresponding to the subtypes usually encountered during consultations, may be proposed: neurodegenerative disease (pre‐Alzheimer's disease MCI, Lewy body dementia or, more rarely, frontotemporal dementia and focal atrophy); cognitive disorders corresponding to vascular lesions (vascular pre‐dementia MCI, mixed dementia); and dysphoric or dysthymic disorders (anxious or depressive syndrome). Issues such as giving multiple medicinal products, particularly if this includes psychotropic agents or medicinal products with an anticholinergic effect, or multiple disorders in particular must be taken into consideration in the aetiological process.37
Unresolved issues
Functional and morphological imaging methods, such as biological markers, may, in the future, make it possible to clarify the different aetiopathogenic factors. These are currently most effective for “prodromal Alzheimer's disease” MCI.
Conclusion
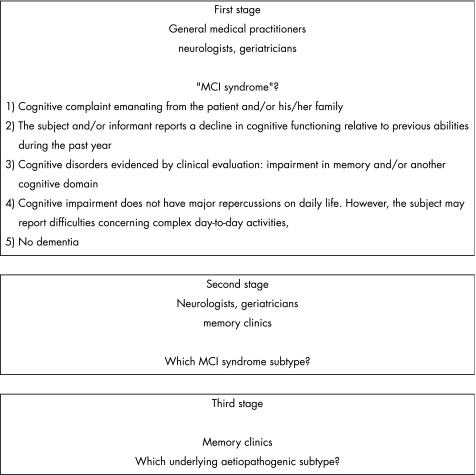
The European Consortium on Alzheimer's Disease MCI group explicitly identifies three separate stages of the diagnostic procedure, and emphasises that different clinicians participate at each stage (fig 1). Firstly, the MCI criteria and procedure will make it possible to identify patients at a high risk for progression to dementia. Secondly, because even with these new MCI criteria there will be a heterogeneous condition, additional tests (such as CSF and neuroimaging) are needed to determine the underlying cause. Future projects, whether corresponding to clinical or therapeutic research, will be able to use more homogeneous populations as a basis and establish more specific and adapted therapeutic strategies at an early stage, if needed, along with more structured overall management. Although the main objective is the early diagnosis of Alzheimer's disease, the other aetiopathogenic subtypes of MCI must not be neglected.
Figure 1 Different stages of the diagnostic procedure for identification of mild cognitive impairment, as given by the European Consortium on Alzheimer's Disease.
Acknowledgements
We thank all members of the EADC working group.
Abbreviations
MCI - mild cognitive impairment
Footnotes
Competing interests: None declared.
References
- 1.Petersen R C, Smith G E, Waring S C.et al Aging, memory, and mild cognitive impairment. Int Psychogeriatr 1997965–69. [DOI] [PubMed] [Google Scholar]
- 2.Ritchie K, Touchon J. Mild cognitive impairment: conceptual basis and current nosological status. Lancet 2000355225–228. [DOI] [PubMed] [Google Scholar]
- 3.Petersen R C, Doody R, Kurz A.et al Current concepts in mild cognitive impairment. Arch Neurol 2001581985–1992. [DOI] [PubMed] [Google Scholar]
- 4.Hughes C P, Berg L, Danziger W L.et al A new clinical scale for the staging of dementia. Br J Psychiatry 1982140566–572. [DOI] [PubMed] [Google Scholar]
- 5.Petersen R C. Mild cognitive impairment as a diagnostic entity. J Intern Med 2004256183–194. [DOI] [PubMed] [Google Scholar]
- 6.Ritchie K, Artero S, Touchon J. Classification criteria for mild cognitive impairment: a population‐based validation study. Neurology 20015637–42. [DOI] [PubMed] [Google Scholar]
- 7.Burns A, Zaudig M. Mild cognitive impairment in older people. Lancet 20023601963–1965. [DOI] [PubMed] [Google Scholar]
- 8.DeCarli C. Mild cognitive impairment: prevalence, prognosis, aetiology, and treatment. Lancet Neurol 2003215–21. [DOI] [PubMed] [Google Scholar]
- 9.Ritchie K, Artero S, Touchon J. Classification criteria for mild cognitive impairment: a population‐based validation study. Neurology 20015637–42. [DOI] [PubMed] [Google Scholar]
- 10.Larrieu S, Letenneur L, Orgogozo J M.et al Incidence and outcome of mild cognitive impairment in a population‐based prospective cohort. Neurology 2002591594–1599. [DOI] [PubMed] [Google Scholar]
- 11.Frisoni G B, Fratiglioni L, Fastbom J.et al Mild cognitive impairment in the population and physical health: data on 1,435 individuals aged 75 to 95. J Gerontol A Biol Sci Med Sci 200055M322–M328. [DOI] [PubMed] [Google Scholar]
- 12.Ganguli M, Dodge H H, Shen C.et al Mild cognitive impairment, amnestic type: an epidemiologic study. Neurology 200463115–121. [DOI] [PubMed] [Google Scholar]
- 13.Wentzel C, Rockwood K, MacKnight C.et al Progression of impairment in patients with vascular cognitive impairment without dementia. Neurology 200157714–716. [DOI] [PubMed] [Google Scholar]
- 14.Bischkopf J, Busse A, Angermeyer M C. Mild cognitive impairment—a review of prevalence, incidence and outcome according to current approaches. Acta Psychiatr Scand 2002106403–414. [DOI] [PubMed] [Google Scholar]
- 15.Palmer K, Wang H X, Backman L.et al Differential evolution of cognitive impairment in nondemented older persons: results from the Kungsholmen Project. Am J Psychiatry 2002159436–442. [DOI] [PubMed] [Google Scholar]
- 16.Rasquin S M, Lodder J, Visser P J.et al Predictive accuracy of MCI subtypes for Alzheimer's disease and vascular dementia in subjects with mild cognitive impairment: a 2‐year follow‐up study. Dement Geriatr Cogn Disord 200519113–119. [DOI] [PubMed] [Google Scholar]
- 17.Fisk J D, Merry H R, Rockwood K. Variations in case definition affect prevalence but not outcomes of mild cognitive impairment. Neurology 2003611179–1184. [DOI] [PubMed] [Google Scholar]
- 18.Morris J C, Storandt M, Miller J P.et al Mild cognitive impairment represents early‐stage Alzheimer disease. Arch Neurol 200158397–405. [DOI] [PubMed] [Google Scholar]
- 19.Collie A, Maruff P, Currie J. Behavioral characterization of mild cognitive impairment. J Clin Exp Neuropsychol 200224720–733. [DOI] [PubMed] [Google Scholar]
- 20.Gauthier S, Touchon J. Mild cognitive impairment is not a clinical entity and should not be treated. Arch Neurol 2005621164–1166. [DOI] [PubMed] [Google Scholar]
- 21.Morris J C, Price A L. Pathologic correlates of nondemented aging, mild cognitive impairment, and early‐stage Alzheimer's disease. J Mol Neurosci 200117101–118. [DOI] [PubMed] [Google Scholar]
- 22.Duyckaerts C. Looking for the link between plaques and tangles. Neurobiol Aging 200425735–9 Discussion, 7436. [DOI] [PubMed] [Google Scholar]
- 23.Bennett D A, Schneider J A, Bienias J L.et al Mild cognitive impairment is related to Alzheimer disease pathology and cerebral infarctions. Neurology 200564834–841. [DOI] [PubMed] [Google Scholar]
- 24.Blennow K. CSF biomarkers for mild cognitive impairment. J Intern Med 2004256224–234. [DOI] [PubMed] [Google Scholar]
- 25.Reiman E M, Uecker A, Caselli R J.et al Hippocampal volumes in cognitively normal persons at genetic risk for Alzheimer's disease. Ann Neurol 199844288–291. [DOI] [PubMed] [Google Scholar]
- 26.De Leon M J, Convit A, DeSanti S.et al Contribution of structural neuroimaging to the early diagnosis of Alzheimer's disease. Int Psychogeriatr 199795(Suppl 1)183–9024752. [DOI] [PubMed] [Google Scholar]
- 27.Korf E S, Wahlund L O, Visser P J.et al Medial temporal lobe atrophy on MRI predicts dementia in patients with mild cognitive impairment. Neurology 20046394–100. [DOI] [PubMed] [Google Scholar]
- 28.Jack C R, Jr, Petersen R C, Xu Y.et al Rates of hippocampal atrophy correlate with change in clinical status in aging and AD. Neurology 200055484–489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.DeCarli C, Miller B L, Swan G E.et al Cerebrovascular and brain morphologic correlates of mild cognitive impairment in the National Heart, Lung, and Blood Institute Twin Study. Arch Neurol 200158643–647. [DOI] [PubMed] [Google Scholar]
- 30.Jagust W J, Haan M N, Eberling J L.et al Functional imaging predicts cognitive decline in Alzheimer's disease. J Neuroimaging 19966156–160. [DOI] [PubMed] [Google Scholar]
- 31.Chetelat G, Desgranges B, de la Sayette V.et al Dissociating atrophy and hypometabolism impact on episodic memory in mild cognitive impairment. Brain 2003126(Pt 9)1955–1967. [DOI] [PubMed] [Google Scholar]
- 32.Klunk W E, Engler H, Nordberg A.et al Imaging brain amyloid in Alzheimer's disease with Pittsburgh Compound‐B. Ann Neurol 200455306–319. [DOI] [PubMed] [Google Scholar]
- 33.Mathis C A, Wang Y, Klunk W E. Imaging beta‐amyloid plaques and neurofibrillary tangles in the aging human brain. Curr Pharm Des 2004101469–1492. [DOI] [PubMed] [Google Scholar]
- 34.Visser P J, Scheltens P, Verhey F R. Do MCI criteria in drug trials accurately identify subjects with predementia Alzheimer's disease? J Neurol Neurosurg Psychiatry 2005761348–1354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Winblad B, Palmer K, Kivipelto M.et al Mild cognitive impairment—beyond controversies, towards a consensus: report of the International Working Group on Mild Cognitive Impairment. J Intern Med 2004256240–246. [DOI] [PubMed] [Google Scholar]
- 36.Dubois B, Albert M L. Amnestic MCI or prodromal Alzheimer's disease? Lancet Neurol 20043246–248. [DOI] [PubMed] [Google Scholar]
- 37.Ancelin M L, Artero S, Portet F.et al Non‐degenerative mild cognitive impairment in elderly people and use of anticholinergic drugs: longitudinal cohort study. BMJ 2006332455–459. [DOI] [PMC free article] [PubMed] [Google Scholar]