Abstract
A 47 year old woman with pure autonomic failure complained of dizziness during emotional stress. Emotional stimuli have not previously been reported to cause hypotension in patients with autonomic failure. In the patient, ambulatory blood pressure recording revealed severe hypotension (50/30 mm Hg) after a stressful event. During a tilt table test, hyperventilation was shown to cause a significant fall of blood pressure. This suggests that emotional stress can induce hypotension, probably through hyperventilation, in subjects with autonomic failure.
Keywords: autonomic failure, orthostatic hypotension, hyperventilation, emotional stress, hypocapnia
An important feature of autonomic failure is orthostatic hypotension, giving rise to sensations of light headedness or frank syncope following standing up or during prolonged standing.1 Post‐exercise hypotension is another important feature, causing similar complaints immediately following the cessation of physical exercise.1 Emotional stress is not known to provoke hypotensive complaints in autonomic failure. Here we report stress induced hypotension in a patient with pure autonomic failure, probably mediated through hyperventilation.
Case report
A 47 year old woman complained of light headedness provoked by prolonged standing and cessation of exercise, typically after climbing stairs. Light headedness was also triggered by emotional upsets, such as confrontations with an adolescent child. She had never lost consciousness during such episodes. The patient had a medical history of Gilles de la Tourette syndrome. Physical examination revealed severe orthostatic hypotension (blood pressure 160/75 mm Hg supine, 70/45 mm Hg after standing for three minutes). Neurological examination showed no abnormalities. Basic laboratory tests (blood count, electrolytes, glucose, renal and liver function tests) were normal. Magnetic resonance imaging of the brain was also normal. Autonomic function testing revealed normal heart rate variability during rest and deep breathing but a reduced heart rate response to standing (ratio = 0.98) and to the Valsalva manoeuvre (ratio = 1.28). Further analysis showed decreased plasma catecholamine concentrations (noradrenaline, 0.41 nmol/l supine and 0.47 nmol/l upright; adrenaline, not detectable supine and 0.07 nmol/l upright; dopamine, 0.10 nmol/l supine and 0.12 nmol/l upright). There was a complete absence of 123I –metaiodobenzylguanidine (MIBG) uptake on cardiac scintigraphy. A diagnosis of pure autonomic failure was made.
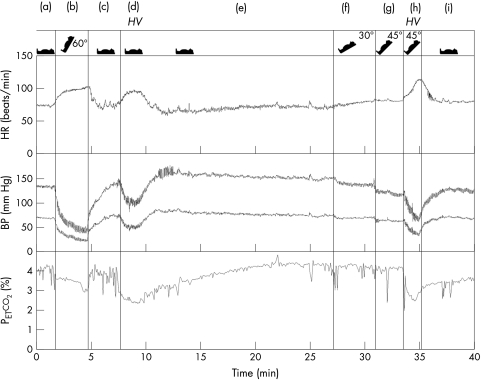
The patient was educated in physical countermanoeuvres, such as leg crossing and squatting, to combat hypotension.2 Despite the beneficial effects of these manoeuvres, she required pharmacological treatment as her complaints progressed over the next two years. Midodrine 10 mg three times daily produced a satisfactory reduction in her hypotensive episodes without serious supine hypertension. However, despite this improvement emotional stimuli continued to trigger her complaints. Ambulatory blood pressure monitoring confirmed the hypotensive nature of these complaints, with one recording of 50/30 mm Hg when her symptoms were provoked by a row. In view of the consistent provocation of complaints by emotional stress, a suspicion of hyperventilation related hypotension was raised. During a tilt table test the patient was asked to hyperventilate while ECG, blood pressure (Finometer, finger photoplethysmography), and end tidal CO2 tension (Petco2) were continuously monitored (fig 1). Hyperventilation in a supine position induced hypotension. Tilting induced enough hypotension to cause the typical complaints, but supine hyperventilation did not. However, when blood pressure was first reduced by a moderate degree of tilting, hyperventilation caused an additional fall in pressure and light headedness. The patient did not experience paraesthesiae during hyperventilation.
Figure 1 During the tilt table test the patient subsequently underwent the following conditions: supine rest (a), 60° tilt (b), supine rest (c), hyperventilation (d), supine rest (e), 30° tilt (f), 45° tilt (g), 45° tilt + hyperventilation (h), and supine rest (i). Both tilting and hyperventilation caused a significant fall of blood pressure. The vasodepressive effect of hyperventilation added to the hypotensive effect of tilting (condition (h)). BP, finger blood pressure; HR, heart rate; HV, hyperventilation; Petco2, end tidal CO2 tension.
Discussion
Emotional stress was found to provoke a hypotensive episode in our patient. This is remarkable, as psychological stressors are known to increase sympathetic outflow and thus raise blood pressure in healthy subjects.3 To our knowledge, emotional stimuli have not previously been reported to cause hypotension in patients with autonomic failure.
Both tilting and hyperventilation caused a fall of blood pressure in our patient and evoked complaints similar to those in daily life. However, the question remains as to whether her stress related complaints can be explained by hyperventilation induced hypotension. Thus we should consider the following questions: can stress induce hyperventilation, and can hyperventilation induce hypotension?
It is known that emotional stress evokes part of the fight‐flight‐fright response, associated with a mild degree of hyperventilation. Emotional or mental stressors often cause mild hypocapnia.4 In normal subjects these small fluctuations of Petco2 do not give rise to paraesthesiae or other complaints related to hypocapnia. Hyperventilation causes an increase in heart rate in normal subjects.4,5 The effects of hyperventilation on blood pressure are not unequivocal, but it can be stated that hyperventilation apparently does not cause frank hypotension in healthy subjects.5 However, in our patient even mild decreases in Petco2 resulted in a significant fall of blood pressure. Earlier studies have shown that hyperventilation can in fact cause a fall of blood pressure and only a moderate increase of heart rate in subjects with autonomic failure.6,7 The amount of increase of heart rate during hyperventilation in autonomic failure depends upon the amount of vagal denervation. In our patient, the heart rate increased markedly during hyperventilation, indicating that vagal innervation was relatively spared compared with the marked sympathetic vasoconstrictor failure. In autonomic failure, the fall in blood pressure during hyperventilation is associated with a lowering of peripheral vascular resistance which outweighs an increase in cardiac output.6 It is likely that hyperventilation in autonomic failure lowers blood pressure through hypocapnia, as effects could not be reproduced through other features associated with hyperventilation, such as an increase of pH or Pao2, or by an increase in respiratory movements without hypocapnia.7 A direct peripheral vasodilator effect of hypocapnia seems probable, as hyperventilation causes hypotension in conditions with insufficient sympathetic innervation, as in autonomic failure or in healthy subjects during ganglionic blockade.7,8
Our results suggest that emotional stress can act as a factor inducing hypotension in subjects with autonomic failure, and we recommend an open mind towards this possibility. This may not only help understand events, but may also help the patient: emotional stressors are hard to avoid, and our patient still experiences lightheadedness following such stimuli, even though she is fully aware of the mechanism. However, knowing that the complaints are caused by defective blood pressure regulation rather than by an emotional hypersensitivity offers some reassurance.
Acknowledgements
We are indebted to R H A M Reijntjes for his assistance with the preparation of figure 1.
Abbreviations
Petco2‐ end tidal CO2 tension
Footnotes
Competing interests: none declared
References
- 1.Bannister R, Mathias C J. Clinical features and evaluation of the primary chronic autonomic failure syndromes. In: Mathias CJ, Bannister R, editors. Autonomic failure. A textbook of clinical disorders of the autonomic nervous system. Oxford: Oxford University Press, 1999307–316.
- 2.Wieling W, Colman N, Krediet C T.et al Nonpharmacological treatment of reflex syncope. Clin Auton Res 200414(suppl 1)62–70. [DOI] [PubMed] [Google Scholar]
- 3.Ziegler M G. Psychological stress and the autonomic nervous system. In: Robertson D, Biaggioni I, Burnstock G, et al, editors. Primer on the autonomic nervous system. Amsterdam: Elsevier Academic Press, 2004189–190.
- 4.Gardner W N. The pathophysiology of hyperventilation disorders. Chest 1996109516–534. [DOI] [PubMed] [Google Scholar]
- 5.Fontana F, Bernardi P, Merlo Pich E.et al Opioid peptide modulation of circulatory response to hyperventilation in humans. Peptides 2000211223–1230. [DOI] [PubMed] [Google Scholar]
- 6.Burnum J F, Hickman J B, McIntosh H D. The effect of hypocapnia on arterial blood pressure. Circulation 1954989–95. [DOI] [PubMed] [Google Scholar]
- 7.Onrot J, Bernard G R, Biaggioni I.et al Direct vasodilator effect of hyperventilation‐induced hypocarbia in autonomic failure patients. Am J Med Sci 1991301305–309. [DOI] [PubMed] [Google Scholar]
- 8.Jordan J, Shannon J R, Diedrich A.et al Interaction of carbon dioxide and sympathetic nervous system activity in the regulation of cerebral perfusion in humans. Hypertension 200036383–388. [DOI] [PubMed] [Google Scholar]