Abstract
Objective
To evaluate the effects of tertiary centres for amyotrophic lateral sclerosis (ALS) on ALS outcome and the use of hospital facilities.
Methods
The study was based on the data of an epidemiological, prospective, population‐based register on ALS (Piemonte and Valle d'Aosta Register for amyotrophic lateral sclerosis, PARALS). The 221 patients recruited between 1995 and 1996 were prospectively followed up for outcome and use of hospital‐based services.
Results
In all, 97 patients were followed up by tertiary ALS centres and 124 by general neurological clinics. Patients followed up by tertiary ALS centres were found to be 4 years younger and underwent percutaneous endoscopic gastronomy and non‐invasive positive‐pressure ventilation more often. Patients followed up by tertiary ALS centres were found to have a considerably longer median survival time (1080 v 775 days), even when stratifying by age, site of onset and respiratory function at diagnosis. In Cox multivariate analysis, attending a tertiary ALS centre was observed to be an independent positive prognostic factor. Moreover, patients attending a tertiary ALS centre were admitted to hospital less often (1.2 v 3.3) and were more frequently admitted for planned interventions. Conversely, patients followed up by general neurological clinics were more frequently admitted for acute events. Also, the hospital stay was considerably shorter for patients attending tertiary ALS centres (5.8 v 12.4 days).
Conclusions
Improved survival was seen in patients with ALS attending tertiary ALS centres, independently from all other known prognostic factors, possibly through a better implementation of supportive treatments. Moreover, because of these centres, the hospitalisation rate was markedly reduced, thus offering a cost‐effective service to patients with ALS and to the community as a whole.
Amyotrophic lateral sclerosis (ALS) is a degenerative disorder of the CNS, characterised by progressive impairment of motor functions at the spinal and bulbar level. Although no cure for ALS is known, palliative care, including symptomatic drugs, percutaneous endoscopic gastrostomy (PEG) and non‐invasive ventilation (NIV), can modify outcome in patients.1 Increasingly, patients with ALS are referred to tertiary ALS clinics, where practice is based on the interdisciplinary care paradigm.2 In contrast with studies on other neurological disorders,3,4,5 only one paper6 has explored the effect of tertiary ALS centres on patients with ALS, reporting that patients with ALS who were followed up by a multidisciplinary clinic had a better prognosis.
This study aims at assessing the effect of tertiary ALS centres on outcome in patients and on the use of hospital facilities.
Methods
Piemonte and Valle d'Aosta Register for ALS
The Piemonte and Valle d'Aosta Register for amyotrophic lateral sclerosis (PARALS) was established in 1995 as a multicentre, prospective and epidemiological register for ALS in two Italian regions.7,8 This study refers to the patients diagnosed with ALS in the 2‐year period between 1995 and 1996, prospectively followed up until 31 December 2003.
Tertiary ALS centres
At the time of the study, two tertiary ALS centres were operational in Piemonte, Torino, and in Veruno. No location in Piemonte and Valle d'Aosta was more than 80 miles from one of the two centres. Both ALS centres had interdisciplinary teams. Patients were seen roughly every 8 weeks. The management of symptoms was based on the best available evidence.1,9 PEG was proposed for a weight loss >10% or episodes of severe choking. NIV was offered for respiratory symptoms, when forced vital capacity (FVC) was <50% of that predicted or when nocturnal pulse oximetry showed marked desaturations.10,11 Riluzole was available free of charge from 1996 and was offered to all patients. All visits and services were provided free of cost to the patients.
Patients were considered to be attending a tertiary ALS centre if they were followed up for at least two visits by one of the two ALS centres.
General neurology clinics
Piemonte and Valle d'Aosta had 26 general neurology departments during the study period. According to the PARALS protocol, the patients attending these clinics were seen at least every 6 months, but they did not undergo regular evaluations of nutritional or respiratory status, and therefore received less attention towards the early introduction of PEG, NIV and palliative care.
Data on admissions to hospital and hospital stay
Data were prospectively collected by the PARALS, and were compared and integrated with data obtained from the Piemonte Hospital Discharge Database, which includes data on all discharges from public and private hospitals in the Piemonte region. An excellent correspondence between two sources has been shown.12
Data analysis
Survival analysis was carried out with Kaplan–Meier tables, and the differences were evaluated with the log rank test.13 Multivariate analysis was carried out with the Cox stepwise proportional hazard model.14 Riluzole, PEG and NIV were included as time‐dependent variables.13 Patients who had a tracheostomy were considered to be deceased at the date of ventilation. Multivariate analyses on hospital admissions were carried out with a stepwise linear regression model. Values of p<0.05 were considered to be significant. All tests were two sided. Data were statistically analysed with the SAS or STAT Software.15
Results
A total of 221 patients were diagnosed as having ALS between 1995 and 1996, 97 (43.9%) were followed up by the two tertiary ALS centres (70 in Torino and 27 in Veruno) and 124 (56.1%) by the general neurology clinics. Patients attending general neurology clinics were significantly older (65.0 (SD 10.3) v 60.8 (SD 11.7) years; p = 0.03) and underwent major interventions less often—that is, PEG (8.8 v 32.0%; p = 0.01) and NIV (6.5 v 15.4; p = 0.04), but we found no differences for sex, type of onset, delay in mean diagnosis, riluzole use or tracheostomy.
Survival analysis
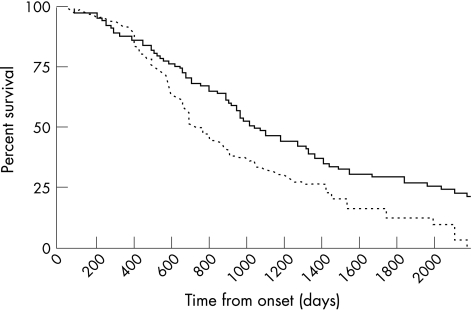
The median survival from onset was 10 months longer among the patients attending a tertiary ALS centre (1080 v 775 days; p = 0.008; fig 1). A marked difference was also found after stratification by age at onset (⩽60 v >60 years), site of onset (bulbar v spinal) and respiratory impairment at diagnosis (FVC% ⩾80 v FVC% <80). In Cox multivariate analysis, not attending a tertiary ALS centre had a 1.61‐fold increased risk of death (p = 0.006; table 1).
Figure 1 Survival curves of patients with amyotrophic lateral sclerosis (ALS) followed up by tertiary ALS centres (continuous line) and general neurology clinics (dotted line; p = 0.0008).
Table 1 Prognostic factors according to Cox multivariate analysis.
| Increased risk of death | p Value | ||
|---|---|---|---|
| FVC <80% at diagnosis | No | 1 | 0.0004 |
| Yes | 4.11 | ||
| PEG | Yes | 1 | 0.0006 |
| No | 3.38 | ||
| Age groups (years) | ⩽50 | 1 | 0.004 |
| 51–60 | 1.40 | ||
| 61–70 | 1.95 | ||
| >70 | 2.72 | ||
| Attending a tertiary centre for ALS | Yes | 1 | 0.006 |
| No | 1.61 | ||
| Bulbar onset | No | 1 | 0.009 |
| Yes | 1.45 | ||
| Riluzole treatment | Yes | 1 | 0.05 |
| No | 1.31 |
The other variables that were included, but did not show significant results, were sex, delay in diagnosis and non‐invasive positive‐pressure ventilation. Riluzole treatment, percutaneous endoscopic gastronomy (PEG) and non‐invasive ventilation were included as time‐dependent variables.
ALS, amyotrophic lateral sclerosis; FVC, forced vital capacity.
Use of hospital‐based services
During the study period, 464 hospital admissions were recorded, corresponding to a mean of 2.2 (SD 1.0) admissions per patient, with a significant difference between tertiary ALS centres (mean 1.2 (SD 0.9)) and general neurology clinics (mean 3.3 (SD 1.8); p = 0.0003). Of them, 30 patients were never admitted to hospital during the course of the disease (19 (19.6%) were followed up by tertiary ALS centres and 11 (8.9%) by general neurology clinics; p = 0.03). The reasons for admission were classified as follows: confirmation of diagnosis, planned interventions (PEG, NIV, tracheostomy), acute events (acute respiratory failure, pneumonia, malnutrition and dehydration) and other reasons (fractures, interventions not related to ALS and admissions for social reasons). Patients followed up by tertiary ALS centres were more frequently admitted for planned interventions, whereas those seen by general neurology clinics were mostly admitted for acute events and other (mainly social) reasons. In multivariate analysis, a higher rate of admission was related to not attending a tertiary ALS centre (p = 0.0003), age >70 years (p = 0.003) and to being unmarried or widowed (p = 0.006).
The mean duration of hospital stay was 10.3 (SD 27.6) days shorter in tertiary ALS centres (mean 5.8, SD 9.5) than in general neurology clinics (mean 12.4, SD 31.6; p = 0.001). In multivariate analysis, longer hospital stay was related to unplanned admissions (p<0.0001), complications during the stay (p = 0.004), not attending a tertiary ALS centre (p = 0.001), age >70 years (p = 0.006) and to being unmarried or widowed (p = 0.01).
Discussion
The last decade has witnessed a trend towards the development of ALS clinics, based on the assumption that such organisations improve patients' care and quality of life. Our data show that tertiary ALS centres have a positive effect on all outcome measures and optimise the use of hospital‐based health services, with a consequent reduction in costs to the healthcare system.
The two cohorts evaluated in the study showed some differences, partly confirming previous reports.6,16 The patients who attended tertiary ALS centres were slightly younger, indicating that older patients are less motivated to search for specialised care. No other demographic and clinical differences were found. In particular, in contrast with the Irish study,6 we observed no difference in the use of riluzole, probably because the neurologists participating in the PARALS were made aware of the possibility of using this drug during the periodical register meetings. Patients attending tertiary ALS centres underwent PEG and NIV more frequently.
The tertiary ALS centres cohort had a markedly better overall survival than the general neurology clinic cohort, with a 10‐month longer median survival time, paralleling the findings from the Irish study.6 Even after stratifying for the major prognostic factors (in particular for age and site of onset), there was a significant advantage in all groups. Interestingly, the greatest difference between the two cohorts was observed in cases of spinal onset, implying that the positive effect of tertiary ALS centres cannot be totally ascribed to the more widespread use of PEG in their patients.6
Attending tertiary ALS centres remained a major independent prognostic factor in multivariate analysis. Therefore, the positive effect of tertiary ALS centres on patient outcome is probably related to factors other than PEG and NIV, such as the better provision of supportive care and of psychological support, and the emphasis on nutritional and respiratory status.1
The positive effect of tertiary ALS clinics is confirmed by the analysis of hospital admissions. To our knowledge, this is the first paper to analyse prospectively the use of hospital services in ALS. Our data show that the patients attending a tertiary ALS centre had a considerably lower number of hospital admissions and a 50% reduction in mean length of hospital stay than the patients who were followed up by general neurology clinics. Moreover, nearly 75% of hospitalisations of the tertiary ALS centre cohort were planned admissions, whereas acute admissions via the emergency room were more frequent in the general neurology clinics cohort. Therefore, attending a tertiary ALS centre either markedly decreases the risk of acute events or improves the home care of these events, thus reducing emergency hospital admissions.
We found that two independent reasons for a higher number of admissions to and a longer hospital stay were (a) age >70 years and (b) being unmarried or widowed, conditions that can be considered to be surrogate markers of a lack of an adequate social network. This is strong evidence that the support of a patient's family should be a major focus of the ALS team interventions.
In conclusion, tertiary ALS centres improve outcome in patients with ALS, independently from all other known prognostic factors, possibly through a better implementation of supportive treatments. Furthermore, according to the data on hospital admissions, the tertiary ALS centres succeeded in following up their patients, mainly through clinic‐based visits and reducing unplanned admissions due to acute events. This resulted in a remarkable decrease in costs to the health system without worsening the positive effects on patient outcome.
Acknowledgements
This study was partly supported by Regione Piemonte, Ricerca Sanitaria Finalizzata, anni 2003 e 2004 and by Compagnia San Paolo, Torino, Italy.
Abbreviations
ALS - amyotrophic lateral sclerosis
FVC - forced vital capacity
NIV - non‐invasive ventilation
PARALS - Piemonte and Valle d'Aosta Register for amyotrophic lateral sclerosis
PEG - percutaneous endoscopic gastronomy
Footnotes
Competing interests: None declared.
Piemonte and Valle d'Aosta Register for ALS (PARALS): Coordinating centre: 2nd Division of Neurology, Department of Neuroscience, University of Torino, Italy; Project coordinators: A Chiò; Study monitors: A Calvo, N Di Vito and P Ghiglione; Scientific Committee: E Bottacchi, A Chiò, D Cocito, MT Giordana, M Leone, L Mazzini and G Mora; Collaborating centres: A Chiò, AA Terreni, D Schiffer, R Mutani, D Cocito, B Bergamasco and I Rainero (Department of Neuroscience, Section of Neurology, University of Torino, and Azienda Ospedaliera San Giovanni Battista, Torino); A Bertolotto, A Tribolo, R Sciolla, F Mondino and MT Giordana (Department of Neuroscience, Section of Neurology, University of Torino, and Azienda Ospedaliera San Luigi Gonzaga, Orbassano); M Leone, P Gaviani, L Mazzini and F Monaco (Department of Neurology, Amedeo Avogadro University, Novara); R Comitangelo (Department of Neurology, Azienda Ospedaliera San Giovanni, Torino); L Sosso and M Gionco (Department of Neurology, Ospedale Mauriziano, Torino); U Morino and M Nobili (Department of Neurology, Ospedale Martini, Torino); L Appendino and C Buffa (Department of Neurology, Ospedale Maria Vittoria, Torino); D Piazza and C Ravetti (Department of Neurology, Ospedale S Giovanni Bosco, Torino); E Oddenino and W Liboni (Department of Neurology, Ospedale Gradenigo, Torino); G Ferrari (Department of Neurology, Ivrea); M Favero and C Doriguzzi Bozzo (Department of Neurology, Pinerolo); P Santamaria (Department of Neurology, Vercelli); U Massazza (Department of Neurology, Biella); A Villani and R Conti (Department of Neurology, Domodossola), G Mora, C Balzarini (Department of Neurological Rehabilitation, Fondazione S. Maugeri, Clinica del Lavoro e della Riabilitazione, IRCCS, Scientific Institute of Veruno and Pavia); M Palermo (Department of Neurology, Alessandria); F Vergnano,(Department of Neurology, Casale Monferrato); M Aguggia (Department of Neurology, Novi Ligure); MT Penza (Department of Neurology, Tortona); F Fassio, N Di Vito and W Troni (Department of Neurology, Asti); P Meineri (Department of Neurology, Azienda Ospedaliera Santa Croce e Carle, Cuneo); A Dutto and D Seliak (Department of Neurology, Savigliano); G Asteggiano and M Dutto (Department of Neurology, Alba); and G Corso nad E Bottacchi (Department of Neurology, Aosta).
References
- 1.Miller R G, Rosenberg J A, Gelinas D F.et al Practice parameter: the care of the patient with amyotrophic lateral sclerosis (an evidence‐based review): report of the Quality Standards Subcommittee of the American Academy of Neurology: ALS Practice Parameters Task Force. Neurology 1999521311–1323. [DOI] [PubMed] [Google Scholar]
- 2.McCallin A. Interdisciplinary practice – a matter of teamwork: an integrated literature review. J Clin Nursing 200110419–428. [DOI] [PubMed] [Google Scholar]
- 3.Ruhholtz S, Waydhas C, Lewan U.et al A multidisciplinary quality management system for the early treatment of severely injured patients: implementation and results in two trauma centers. Intensive Med Care 2002281395–1404. [DOI] [PubMed] [Google Scholar]
- 4.Pozzilli C, Brunetti M, Amicosante A M V.et al Home‐based management in multiple sclerosis: results of a randomised controlled trial. J Neurol Neurosurg Psychiatry 200273250–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Temkin‐Greener H, Gross D, Kunitz S J.et al Measuring interdisciplinary team performance in a long‐term care setting. Med Care 200442472–481. [DOI] [PubMed] [Google Scholar]
- 6.Raynor B J, Alexander M, Corr B.et al Effect of a multidisciplinary amyotrophic lateral sclerosis (ALS) clinic on ALS survival: a population based study, 1996–2000. J Neurol Neurosurg Psychiatry 2003741258–1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Piemonte, Valle d'Aosta Register for Amyotrophic Lateral Sclerosis ( P A R A L. Amyotrophic lateral sclerosis in Italy, 1995 through 1996: a prospective analysis of incidence. Neurology 200156239–244.11160962 [Google Scholar]
- 8.Chiò A, Mora G, Leone M.et al Early symptom progression rate is related to ALS outcome: a prospective population‐based study. Neurology 20025999–103. [DOI] [PubMed] [Google Scholar]
- 9.Leigh R N, Ray‐Chaudhuri K. Motor neuron disease. J Neurol Neurosurg Psychiatry 199457886–896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bach J R. Amyotrophic lateral sclerosis: predictors for prolongation of life by non‐invasive respiratory aids. Arch Phys Med Rehabil 199576828–832. [DOI] [PubMed] [Google Scholar]
- 11.Aboussouan L S, Kham S U, Meeker D P.et al Effect of noninvasive positive‐pressure ventilation on survival in amyotrophic lateral sclerosis. Ann Intern Med 1997127450–453. [DOI] [PubMed] [Google Scholar]
- 12.Chiò A, Ciccone G, Calvo A.et al Validity of hospital morbidity records for amyotrophic lateral sclerosis. A population‐based study. J Clin Epidemiol 200255723–727. [DOI] [PubMed] [Google Scholar]
- 13.Armar K B, Machin D.Survival analysis: a practical approach. Chichester: Wiley, 1995
- 14.Cox D R. Regression models and life tables. J R Stat Soc (B) 197234187–220. [Google Scholar]
- 15.SAS/STAT Software Changes and enhancements for release 6.12. Cary, NC: SAS Institute, 1996
- 16.Lee J R ‐ J, Annegers J F, Appel S H. Prognosis of amyotrophic lateral sclerosis and the effect of referral selection. J Neurol Sci 1995132207–215. [DOI] [PubMed] [Google Scholar]