Familial transmissible spongiform encephalopathies comprise about 14% of all cases of transmissible spongiform encephalopathy in humans. We report on a patient with a definite diagnosis of familial Creutzfeldt–Jakob disease with an insertional mutation consisting of seven extra octapeptide repeats between codons 51 and 91 in the PRNP gene, associated with a genotype homozygotic for methionine at codon 129 and a novel coding change of the inserted octapeptide region.
Case report
A Chinese woman developed forgetfulness at the age of 44 years, which progressed into memory deterioration 2 years later. At age 48 years, she developed gait disturbance and was admitted to hospital. On neurological examination she presented with mild dysarthria, intellectual deterioration and cognitive dysfunction. All her extremities showed hypertonia and ataxia, and no pathological reflexes were elicited. Her general health condition was good, except for the narrowed interpalpebral fissure dimension in her left eye and poor visual acuity since childhood.
A general brain magnetic resonance image showed no remarkable changes. The first electroencephalogram showed slow wave activity. The second electroencephalogram taken 13 days after admission, showed periodic sharp and slow wave complexes. Haematoxylin and eosin stain of a brain biopsy specimen taken from the left frontal lobe showed diffuse spongiform degeneration, with obvious vacuoles predominanting in the deep layers of the cortex and astrocytosis and neuronal loss in the cortical ribbon. Electron microscopy showed neurone degeneration, astrocytosis and membrane‐bound vacuole. The patient's mental impairment and other neurological symptoms rapidly worsened after admission. She subsequently developed visual hallucination, urine incontinence and myoclonus 3 weeks after hospitalisation. Creutzfeldt–Jakob disease (CJD) was suspected on clinical diagnosis. She died 46 days after admission. The total illness duration was 50 months.
The patient's mother developed involuntary movements and progressive dementia at age 58 years. She was diagnosed with suspected cerebellar atrophy clinically and died 6 months after onset of symptoms. The patient's grandfather developed dementia and paralysis at age 58 years and died approximately 6 months after onset. The patient's father and four siblings were still healthy, and her only son was healthy at age 20 years.
Proteinase K resistant PrP (PrPres) signals were observed on western blotting assays of 10% brain homogenate. On electrophoresis, the pattern of PrPres was similar to that of PrPres type 1, with predominance of monoglycosylated PrPres. After deglycosylation, two prominent PrP peptides of 27 and 20–21 kDa were detected, corresponding to full‐length PrPwt and a C‐terminal PrP fragment.
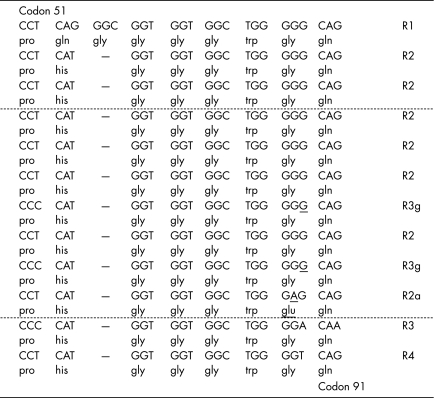
PRNP was analysed using genomic DNA extracted from the frozen brain tissue of the patient. Analysis of the polymerase chain reaction products showed that in addition to the fragment representing the full‐length PRNP, there was an extra band approximately at position 1000 bp. Sequencing tests confirmed that the shorter polymerase chain reaction fragment was the normal human PRNP sequence without any mutation, and that the longer fragment contained a 168‐bp insertion within the octarepeat region of PRNP. The 168‐bp insertion was identified as a seven‐extra‐octarepeat sequence, composed of R2‐R2‐R2‐R3g‐R2‐R3g‐R2a (fig 1), in which R3g differed from wild‐type R3 for a single synonymous change (A→G) at its 21st position without inducing amino acid exchange and R2a had a G→A exchange at the seventh triplet (from GGG→GAG), leading to a conversion from glycine to glutamic acid. The octarepeat region was R1‐R2‐R2‐R2‐R2‐R2‐R3g‐R2‐R3g‐R2a‐R3‐R4 (insertions are shown italicised). No other mutations were detected in the PRNP open reading frame. The codon 129 genotype was homozygotic for methionine.
Figure 1 Nucleotide sequence of the mutant allele in the region between codons 51 and 91 of the PRNP of the patient. The seven extra octapeptide repeats are inserted after the second R2 cycle. The mutated nucleotide and amino acid are shown underlined. –, no amino acid in this position.
Comment
The patient described in this article is the first case of genetic CJD identified in China and represents the fifth reported family with a 168 bp nucleotide insertion1,2,3; however, the octarepeat sequence and gene arrangement differ from those described previously. The patient showed typical clinical features such as sporadic CJD characterised by cerebellar sign, myoclonus and dementia, but had longer illness duration than sporadic CJD. Unlike previously reported patients with familial Creutzfeldt–Jakob disease with seven‐octapeptide repeat insertion, whose ages of onset ranged from 23 to 32 years and illness durations were 7–16 years,1,4 the patient reported here presented with relatively late‐onset dementia and rapid progression of clinical symptoms. It is not clear whether this is due to the novelty of the octapeptide repeat sequence, the associated mutation or some other factors, but this report indicates that the phenotype associated with seven‐repeat inserts can vary.
Acknowledgements
We thank Dr R Will from Edinburgh University, UK, for helpful discussion.
Footnotes
Funding: This work was supported by Chinese National Natural Science Foundation Grants 30130070, 30571672 and 30500018, National Science and Technology Task Force Project (2003BA712A04‐02) and EU Project QLRT 2000 01441.
Competing interests: None declared.
References
- 1.Lewis V, Collins S, Hill A F.et al Novel prion protein insert mutation associated with prolonged neurodegenerative illness. Neurology 2003601620–1624. [DOI] [PubMed] [Google Scholar]
- 2.Origin of extra prion repeat units [online] Available at: http://www.mad‐cow.org/prion_repeat_insertions.html
- 3.Goldfarb L G, Brown P, McCombie W R.et al Transmissible familial Creutzfeldt‐Jakob disease associated with five, seven, and eight extra octapeptide coding repeats in the PRNP gene. Proc Natl Acad Sci US A 19918810926–10930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Croes E A, Theuns J, Houwing‐Duistermaat J J.et al Octapeptide repeat insertions in the prion protein gene and early onset dementia. J Neurol Neurosurg Psychiatry 2004751166–1170. [DOI] [PMC free article] [PubMed] [Google Scholar]