Dissections of intracranial arteries are rare and occur most commonly in the vertebrobasilar system.1 Isolated dissecting aneurysms of the posterior cerebral artery (PCA) are very uncommon. We report a case of subarachnoid haemorrhage (SAH) heralded by a 3‐month history of diplopia due to dissection of the right PCA documented with digital subtraction angiography (DSA), magnetic resonance imaging (MRI) and angiography (MRA). The patient was treated conservatively, with a good outcome.
Case report
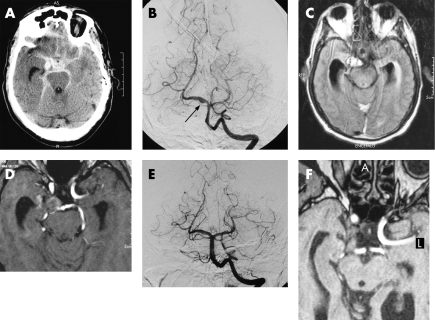
A 58‐year‐old male farm worker was found unconscious in the countryside and admitted to hospital. His medical history was unremarkable except for treated arterial hypertension and diplopia for 3 months. On admission, he had a Glasgow Coma Scale (GCS) score of 14 and a complete right third‐nerve palsy. Vision and corneal reflexes were normal. A computed tomography scan showed diffuse SAH and intraventricular haemorrhage with hydrocephalus (fig 1A). Soon after arrival, he became less responsive and underwent temporary external ventricular drainage. DSA disclosed a fusiform dilatation of the P1–P2 segment of the right PCA with a focal “blister”, suggesting a dissecting aneurysm (fig 1B).
Figure 1 Computed tomography scan at admission showing extensive subarachnoid haemorrhage (SAH) (A). Digital subtraction angiography (DSA; anteroposterior projection) showing a fusiform ectasia of the P1–P2 segment of the right posterior cerebral artery (PCA) with a focal “blister” (arrow) (B). Twenty days later, axial fluid‐attenuated inversion recovery magnetic resonance (FLAIR MR) image (C) and axial T1‐weighted source image of three‐dimensional time‐of‐flight magnetic resonance angiography (3D TOF MRA) (D) show an area of abnormal signal intensity in the right portion of the ambiens cistern surrounding the P1–P2 segment of the right PCA, consistent with intramural haematoma in the subacute phase. DSA (E) and source image of 3D TOF MRA (F) 4 months after SAH showing a near normalisation of the right PCA calibre without focal blister (E) and a decrease in the size of the intramural haematoma (F).
Twenty days later, his GCS score was 15. MRI showed an area of hyperintensity in fluid‐attenuated inversion recovery images in the right portion of the ambiens cistern and iso‐hyperintensity in T1‐weighted images and in axial source images of 3D time‐of‐flight MRA consistent with intramural haematoma in the subacute phase (fig 1C, D). The haematoma surrounded the P1–P2 segment of the PCA. We found no evidence of ischaemic brain lesions. The patient was transferred to a rehabilitation centre.
Four months later, the patient returned to his normal activities. Neurological examination showed partial third‐nerve palsy with ptosis, impaired adduction and a right mydriatic pupil with no reaction to light. A follow‐up DSA showed a reduction of the right PCA fusiform dilatation, with disappearance of the focal blister (fig 1E). MRI and MRA showed a decrease in size of the intramural haematoma (fig 1F).
Discussion
We found a description of 26 cases with isolated PCA dissection in the English literature. The clinical presentation is usually with ischaemic symptoms in the PCA territory (17 patients) whereas SAH was described in 9 patients.1,2,3
Our case has some peculiarities, which include the clinical presentation, the findings on diagnostic imaging and the clinical evolution.
In patients with PCA dissection, third‐nerve palsy was reported in one, which was related to ischaemic lesion in the mid‐brain.1 In our patient, diplopia appeared 3 months before admission and was probably due to progressive enlargement of intramural haematoma with compression of the third‐nerve trunk before rupture in the subarachnoid space.
The aetiology of PCA dissection and more generally of intracranial dissections remains obscure, although it has been associated with trauma and sport‐related activities, cervical manipulations, arteritis, atherosclerosis, fibromuscular dysplasia, surgery, delivery, hypertension and connective tissue disease.2,3 No definite risk factors were identified in our patient, except for mild hypertension controlled with drugs.
The pathological hallmark of arterial dissection is represented by a separation of layers of the vessel wall usually caused by an intimal tear that connects the arterial lumen with the wall of the artery, forming an intramural haematoma. SAHs are not rare in intracranial artery dissections because they lack an external elastic membrane and have a thinner adventitia and fewer elastic fibres in the media as compared with extracranial vertebral and carotid arteries.2,3
Diagnosis of intracranial artery dissection relies on DSA, but MRI and MRA have found a role in establishing the initial diagnosis and in the follow‐up.1,2,4 DSA signs of arterial dissections include irregular narrowing (“pearl and string sign”), fusiform aneurysm (“pseudoaneurysm” or dissecting aneurysm) and venous mural pooling of contrast medium, although the only pathognomonic DSA finding is the identification of a double lumen—that is, the passage of the contrast medium into a true and false lumen.2,3
MRI is an ideal complement to DSA, as it can directly enable assessment of the vessel wall and demonstration of the intramural haematoma. The intramural haemotoma typically has a crescent shape showing hyperintensity to isointensity in T1‐weighted image and hyperintensity in proton density and T2‐weighted images in the subacute stage.
The variability of MRI appearance of intramural haematoma reflects differences in the techniques used (spatial resolution, pulse sequence) and the time interval between haemorrhage and examination.4 A combination of DSA, MRI and MRA findings strongly supported the diagnosis in our case.
Arterial dissection is a dynamic disease and this justifies the clinical and neuroradiological follow‐up of patients.4 The healing process at the site of mural haematoma is responsible for the change in vessel silhouette with time and can result in a complete or partial recovery of the vessel lumen. Sometimes, however, dissection evolves in vessel occlusion or formation of pseudo‐aneurysm.
The natural history and optimal treatment of PCA dissecting aneurysms are not established, but our and other cases1,2,3 suggest a more benign outcome as compared with dissections of the vertebrobasilar arteries. A favourable outcome was common in patients with ischaemia treated conservatively or with anticoagulation. Among nine patients with SAH, four were treated with surgical or endovascular “trapping” with parent artery occlusion to prevent re‐bleeding and five with a conservative management.2,3,5 We decided to treat our patient conservatively because of the poor clinical conditions at admission and in view of the rich vascular supply to the brain stem that originates from P1 segment which makes occlusion of the parent artery at this level risky.5
Footnotes
Competing interests: None declared.
References
- 1.Caplan L R, Estol C J, Massaro A R. Dissection of the posterior cerebral arteries. Arch Neurol 2005621138–1143. [DOI] [PubMed] [Google Scholar]
- 2.Sherman P, Oka M, Aldrich E.et al Isolated posterior cerebral artery dissection: report of three cases. Am J Neuroradiol 200627648–652. [PMC free article] [PubMed] [Google Scholar]
- 3.Lazinski D, Willinsky R A, TerBrugge K.et al Dissecting aneurysms of the posterior cerebral artery: angioarchitecture and a review of the literature. Neuroradiology 200042128–133. [DOI] [PubMed] [Google Scholar]
- 4.Mascalchi M, Bianchi M C, Mangiafico S.et al MRI and MR angiography of vertebral artery dissection. Neuroradiology 199739329–340. [DOI] [PubMed] [Google Scholar]
- 5.Ciceri E F, Klucnik R P, Grossman R G.et al Aneurysms of the posterior cerebral artery: classification and endovascular treatment. Am J Neuroradiol 20012227–34. [PMC free article] [PubMed] [Google Scholar]