Abstract
The case of a 23‐year‐old mountaineer who was hit by a lightning strike to the occiput causing a large central visual field defect and bilateral tympanic membrane ruptures is described. Owing to extreme agitation, the patient was set to a drug‐induced coma for 3 days. After extubation, she experienced simple and complex visual hallucinations for several days, but otherwise recovered largely. Neuropsychological tests revealed deficits in fast visual detection tasks and non‐verbal learning, and indicated a right temporal lobe dysfunction, consistent with a right temporal focus on electroencephalography. Four months after the accident, she developed a psychological reaction consisting of nightmares with reappearance of the complex visual hallucinations and a depressive syndrome. Using the European Cooperation for Lightning Detection network, a meteorological system for lightning surveillance, the exact geographical location and nature of the lightning flash were retrospectively retraced.
Central nervous system injuries caused by a direct lightning strike to the head are rare but exceedingly harmful.1,2 Electrical current passing through the brain can lead to coagulation of brain tissue, intracranial haemorrhage and damage to the medullary respiratory centre. Secondary ischaemic brain injury may occur after cardiopulmonary arrest.
Visual hallucinations often accompany a defective field of vision, which may be caused by a lesion anywhere in the visual pathway from the retina to the striate cortex.3 Simple hallucinations usually consist of monochrome or coloured flashes (phosphenes), and are differentiated from complex, also known as formed, hallucinations. The latter typically develop with a latent period after acute lesions and persist for some days to weeks.4,5 Unlike patients with mental disorders or substance withdrawal, patients with visual field defects have full insight into the unreality of their perception.
We describe a patient who survived a lightning strike to the head, leaving a focal visual cortex defect with simple and complex visual hallucinations. After a clinically asymptomatic interval, serious psychopathological sequelae occurred.
Case report
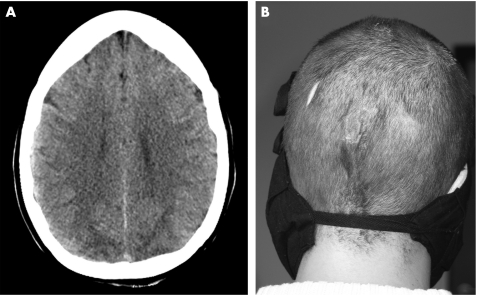
On 3 September 2004, a 23‐year‐old healthy woman was hit by a “bolt from the blue” while climbing on a ridge at 2750 m shortly before reaching the Latemar Peak in the Alps from a southern direction. The accompanying climber was about 50 m from the casualty, and reported that at the time of the incident (about 15:00 Central European Time (CET)), the sky was clear and sunny. He heard cracking thunder and was thrown to the ground by a massive shock wave. The patient was also thrown to the ground, lost consciousness for a few seconds and was confused afterwards. She had no vision, dazzled by a bright light. On arrival of the air rescue team, her Glasgow Coma Scale was 9. She was hospitalised and because of extreme agitation, set to a drug‐induced coma for 3 days. The initial CT scan showed bilateral occipital oedema, but no intracerebral or subarachnoid haemorrhages or skull fractures (fig 1A). Except for bilateral pleural effusions, her cardiopulmonary function was unremarkable. Burns at the occiput (fig 1B), at the right axilla, breast and trunk, and at the right lateral ankle were noted. She had bilateral tympanic membrane ruptures.
Figure 1 (A) Axial CT scan of the head 3 h after the lightning strike showing diffuse occipital oedema. (B) Occipital burn injury 11 days after the lightning strike. Informed consent was obtained for publication of this figure.
After weaning from the respirator, she was initially alert and fully orientated. She complained of blurred vision and a large central bilateral visual field defect. Paroxysmal golden flashes were moving in her whole visual field. She was not able to read, but was able to recognise familiar faces. During artificial ventilation she had received midazolam, sufentanil, morphine, and prior to extubation ketamine and propofol; she did not have a history of illicit drug use.
In the evening, still awake and 6 h after extubation, strange phenomena occurred. These exclusively visual sensations consisted of unknown people, animals and objects acting in different scenes, like a movie. None of the persons or scenes was familiar to her and she was severely frightened by their occurrence. For example, an old lady was sitting on a ribbed radiator, then becoming thinner and thinner, and finally vanishing through the slots of the radiator. Later, on her left side a cowboy riding on a horse came from the distance. As he approached her, he tried to shoot her, making her feel defenceless because she could not move or shout for help. In another scene, two male doctors, one fair and one dark haired, and a woman, all with strange metal glasses and unnatural brownish‐red faces, were tanning in front of a sunbed, then having sexual intercourse and afterwards trying to draw blood from her. These formed hallucinations, partially with delusional character, were in the whole visual field and constantly present for approximately 20 h. At the time of appearance, the patient was not sure whether they were real or unreal, but did not report them for fear that she might be considered insane. However, as she was still frightened after cessation of the hallucinations, she insisted on being transferred to her hometown hospital. In the next days, she had increasingly better insight and later forgot about this episode.
Three days after extubation, she was in a euphoric mood. She reported persistently reduced vision with paroxysmal bright flashes surrounding a large scotoma in the right lower quadrant. The ophthalmological examination revealed a visual acuity of 20/125 in the right eye and 20/200 in the left eye. There were no signs of corneal or retinal lesions. Neurological examination was otherwise normal. The EEG disclosed mild diffuse slowing without a focus or discharges, the ECG showed a bigeminus. MRI of the brain demonstrated mild bilateral occipital subarachnoid haemorrhages without affecting temporal structures.
Ten days later, visual disturbances had improved, leaving a small inferior homonymous paracentral scotoma measuring approximately 5° immediately adjacent to the area of central vision on Amsler grid examination and tangent screen perimetry (Humphrey field analyser, Carl Zeiss Meditec, Jena, Germany). Ophthalmological examination was otherwise unremarkable and her visual acuity was 20/20 in both eyes. Pattern shift visual evoked potentials (30′ checkerboard) from both eyes were persistently deformed and reduced in amplitude for the next 18 months (P2 N3; 3.6–5.4 µV; normal >5 µV). EEG now showed diffuse abnormalities and a right temporal focus (T6 according to the international 10–20 system), with intermittent slowing and spikes. When discharged, she was emotionally stable and optimistic.
The patient was examined with a neuropsychological test battery 7 weeks, 20 weeks and 18 months after the lightning strike. Verbal and non‐verbal cognition were measured with a short form of the German version of the Wechsler Intelligence Scale for Adults Revised.6 Verbal and non‐verbal learning were measured with the California Verbal Learning Test and the Rey Visual Design Learning Test, respectively.7,8 The Ruff 2 and 7 Test was used to quantify differences between automatic and controlled visual searches.9
Seven weeks after the injury, a reduction in fast visual detection tasks and a decrease in non‐verbal learning were found, whereas verbal learning measures and general level were within the normal range (table 1). This difference indicated an intact left temporal function and a right temporal lobe dysfunction, congruent with the persistent right temporal focus on EEG. At 20 weeks, non‐verbal learning proficiency showed considerable improvement to results slightly below her general level of cognitive function. Impairment in visual detection tasks was constant. No significant differences from the population mean in non‐verbal learning and in visual detection were found 18 months after the lightning strike; EEG remained pathological. Brain contrast‐enhanced MRI 4 months after the lightning strike was normal.
Table 1 Improvement of neuropsychological function after the lightning strike.
| Test results in z scores | |||
|---|---|---|---|
| 7 weeks after injury | 20 weeks after injury | 18 months after injury | |
| Ruff 2 and 7 | −1.1 | −0.8 | −0.4 |
| CVLT | 0.9 | 1.4 | 2.4 |
| RVDLT | −0.7 | 0.4 | 0.2 |
| Full‐scale IQ (WAIS‐R) | 0.8 | 0.9 | 1.3 |
CVLT, California Verbal Learning Test; RVDLT, Rey Visual Design Learning Test; WAIS‐R, Wechsler Intelligence Scale for Adults—Revised.
Results of the Ruff 2 and 7 (visual detection), CVLT (verbal memory), RVDLT (non‐verbal learning) and the full‐scale IQ, all transformed into z scores, are shown. A z score between –1 and 1 means that the performance of an individual is within 1 SD from the performance of a normal control of the same age and education. A z score smaller than –1 or bigger than 1 is interpreted as a significant difference.
Twenty weeks after the accident, the patient reported mournfulness, lack of energy and frequent nightmares with “strange flashbacks” for the last month. These nocturnal “flashbacks” were exactly replicating the complex visual hallucinations and paranoid delusions she had experienced the day after weaning from the respirator. She had difficulties in initiating and maintaining sleep, and her sleep was severely disrupted due to awakening from nightmares. She was treated with 20 mg paroxetine and was referred to a specialist in trauma therapy. Her nightmares vanished after approximately 2 weeks. During the next few months, she experienced several depressive episodes with suicidal ideation, but ultimately recovered.
Later, the patient only once re‐experienced the complex hallucinations in the night after her grandmother's house was on fire. On interview, even 24 months after the first occurrence, she remembered the different scenes very well and was able to describe every detail.
Discussion
Owing to an increase in outdoor recreational activities, the number of casualties caused by lightning strikes in the mountains has grown in recent years.10 During lightning weather conditions, hikers and climbers at any location, not only in exposed areas such as ridges or near the summit, are at high risk of injury from lightning. Sometimes, thunderclouds may be overlooked in mountainous surroundings, and a clear sky may give a wrong feeling of security.1 Therefore, anticipation and avoidance of lightning is one of the most important precautions for outdoor activities in the mountains.
Lightning harms humans by its electrical effects, heat and concussive forces. The skin is highly resistant to electrical current, and often only superficial flashover burn injuries occur.11 If the current exceeds the breakdown strength of the skin, it preferably travels with structures of least resistance—that is, the vascular and the nervous systems.11 Direct lightning strikes to the head have a high degree of fatality or result in severe neurological sequelae.2,11 Our patient survived without major brain damage. The persisting scotoma was probably caused by direct electrical or thermal effects of the current at the occipital visual cortex, as depicted by transient focal oedema and abnormal visual evoked potentials. Given that the calcarine cortex is a highly vascularised structure, it should be particularly vulnerable to lightning damage.
The representation of the central visual field is located at the convexity of the occipital lobe, the occipital pole. Simple visual hallucinations such as phosphenes often accompany a defective field of vision, and occur rapidly. Complex visual hallucinations can arise from lesions of the entire visual pathway. They are located within the field of reduced vision and usually evolve after hours or days.4 Manford and Andermann3 observed that smaller rather than larger occipital lesions are associated with hallucinations, whereas lesions in the more anterior association cortex cause a loss of visual imagery. Hence, they speculated that hallucinations are generated as a release phenomenon in the association cortex when input from the primary visual cortex is missing and/or the cortical activity is altered by diminished input from the ascending reticular activation system, in particular serotonergic projections that exert an inhibitory action. Evidence for the involvement of the reticular activation system and its connections to the thalamus comes from patients with peduncular hallucinosis, where rostral brainstem lesions, most commonly of vascular origin, cause vivid, usually formed, colourful hallucinations.3
Although in this patient the clinical, radiographic and neurophysiological findings suggest causality between the initial simple and complex visual hallucinations and the visual cortex defect, additional factors might have contributed to the formed hallucinations and paranoid delusions. First, visual hallucinations are known to occur during or after application of a wide range of sedative and anaesthetic drugs, in particular midazolam and propofol, both of which can also elicit sexual hallucinations.12 Second, in a delirium with an altered level of consciousness—for example, after withdrawal of sedatives—visual and tactile hallucinations may occur, typically fragmentary in nature and frightening the patient.13 Finally, as is common in organic disease and similar to hypnagogic hallucinations,3 drowsiness could have triggered the long‐lasting visual sensations with various, complete scenes. Unlike hallucinations caused by release phenomena of the visual association cortex, hallucinations due to epileptic discharges in these areas are not associated with the state of arousal and are usually brief, stereotyped and fragmentary in nature.3
After recovering from acute injuries, our patient developed depression, sleep disturbances and nightmares with an exact recall of the visual hallucinations. Traumatic events, especially in combination with an intensive care unit (ICU) stay, often lead individuals to form highly detailed, vivid and enduring memories that are called flashbulb memories.14 It was hypothesised that ICU patients are specifically prone to memories of nightmares, frightening hallucinations and paranoid delusions, because during an ICU stay memory formation might be reduced for external events and enhanced for internal events.14 Flashbulb memories have great emotional importance to the patient and later can be replayed as daytime recollections or nightmares in post‐traumatic stress disorder. The reappearance of complex visual hallucinations on emotional stress was described before in two patients with occipital lobe lesions.4 It is unclear, however, whether these patients suffered from symptoms of post‐traumatic stress disorder as well. Interestingly, in our patient, the recurring visual memories stopped under treatment with a selective serotonin reuptake inhibitor, supporting a role of perturbed serotonergic transmission in release phenomena of the visual association cortex.
Meteorological conditions
At 15:00 CET, images of a weather radar station located at Patscherkofel south of Innsbruck, Austria, depicted a small, isolated thunderstorm cell just south‐east from Latemar Peak. Within a 15 min period (15:00–15:15 CET), the European Cooperation for Lightning Detection (EUCLID) lightning location network located three flashes in the region south‐east of the summit at distances of approximately 3–4 km from the summit. Peak currents of these flashes were between –8 and –12 kA, typical of negative flashes caused by a current exchange from the negatively charged thunder cloud to the positively charged ground.
On average, the EUCLID network has a location accuracy of about 500 m (50% probability error ellipse) and a distance of 3–4 km is outside this range. Potential reasons for enhanced location errors could be a heavily tilted lightning channel at this high altitude of about 3000 m above sea level or propagation effects of the lightning radiated fields in the poorly conducting mountainous region. Whether the flash that struck the woman was completely missed by the location system or whether it was misplaced is unclear. On the other hand, the positions of the located lightning flashes are in good agreement with the weather radar echoes. For further details on the function and accuracy of lightning detection systems, the reader might consult the EUCLID homepage (http://www.euclid.org/) or Cherington et al1 and references therein.
The pathophysiology of lightning‐related cerebral and neurobehavioural complications is not well understood. Although in some cases, the electrical current of a direct strike to the head is high enough to cause generalised brain oedema, subarachnoid and intracerebral haemorrhages, others show scarce neuropathological abnormalities, mostly in the brain tissue adjacent to blood vessels.15 In this patient, the neuropsychological profile and the EEG findings demonstrated a constant right temporal dysfunction, remote from the apparent occipital lesion. Furthermore, a mild encephalopathy was shown by diffuse abnormalities on EEG, persisting for several months. Follow‐up MRI of the brain failed to show brain atrophy or lesions in the respective regions. Secondary ultrastructural and chemical changes can not be detected using common imaging techniques.
Often, however, regardless of whether the head was injured or not, lightning victims complain of long‐term neuropsychological problems, including memory and attention deficits, and emotional lability.2,11,16 Although the exact origin of these symptoms is unclear, a psychobiological model involving psychological triggers, neurochemical (eg, neurotransmitter) alterations and—in cases such as this one—structural damage appears more plausible as compared with a purely psychogenic explanation.
This case illustrates that a direct lightning strike to the head can be survived with minor clinical deficits. However, delayed and long‐term sequelae should be anticipated. Persistent neuropsychological and behavioural problems are common in lightning strike survivors; therefore, early injury‐appropriate referral and rehabilitation are necessary.2,17
Acknowledgements
We thank Wolfgang Jakob for preparing the photograph, Ulf Reinstadler for providing the CT scans, and Mary Ann Cooper and Andreas Steinbrecher for helpful comments on the manuscript.
Abbreviations
CET - Central European Time
EUCLID - European Cooperation for Lightning Detection
ICU - intensive care unit
Footnotes
Competing interests: None.
Informed consent was obtained for publication of figure 1.
References
- 1.Cherington M, Krider E P, Yarnell P R.et al A bolt from the blue: lightning strike to the head. Neurology 199748683–686. [DOI] [PubMed] [Google Scholar]
- 2.Cherington M. Neurologic manifestations of lightning strikes. Neurology 200360182–185. [DOI] [PubMed] [Google Scholar]
- 3.Manford M, Andermann F. Complex visual hallucinations. Clinical and neurobiological insights. Brain 19981211819–1840. [DOI] [PubMed] [Google Scholar]
- 4.Kölmel H W. Complex visual hallucinations in the hemianopic field. J Neurol Neurosurg Psychiatry 19854829–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lance J W. Simple formed hallucinations confined to the area of a specific visual field defect. Brain 197699719–734. [DOI] [PubMed] [Google Scholar]
- 6.Tewes U.Handbuch und Testanweisung für den Hamburg‐Wechsler Intelligenztest für Erwachsene. Revision 1991. Bern: Hans Huber, 1994
- 7.Delis D C, Kramer J H, Kaplan E.et alCalifornia Verbal Learning Test: adult version. Manual. San Antonio, TX: Psychological Corporation, 1987
- 8.Spreen O, Strauss E.A compendium of neuropsychological tests. New York: Oxford University Press, 1991171–176.
- 9.Ruff R M, Niemann H, Allen C C.et al The Ruff 2 and 7 Selective Attention Test: a neuropsychological application. Percept Mot Skills 1992751311–1319. [DOI] [PubMed] [Google Scholar]
- 10.Holle R L. Lightning‐caused deaths and injuries during hiking and mountain climbing. In: Preprints, International Conference on Lightning and Static Electricity. Paper KMP‐33. September 20–22, 2005. Seattle, WA: Boeing Company, 2005
- 11.Cooper M A. Emergent care of lightning and electrical injuries. Semin Neurol 199515268–278. [DOI] [PubMed] [Google Scholar]
- 12.Balasubramaniam B, Park G R. Sexual hallucinations during and after sedation and anaesthesia. Anaesthesia 200358549–553. [DOI] [PubMed] [Google Scholar]
- 13.Norton J W, Corbett J J. Visual perceptual abnormalities: hallucinations and illusions. Semin Neurol 200020111–121. [DOI] [PubMed] [Google Scholar]
- 14.Jones C, Griffiths R D, Humphris G. Disturbed memory and amnesia related to intensive care. Memory 2000879–94. [DOI] [PubMed] [Google Scholar]
- 15.Kleinschmidt‐DeMasters B K. Neuropathology of lightning‐strike injuries. Semin Neurol 199515323–328. [DOI] [PubMed] [Google Scholar]
- 16.van Zomeren A H, ten Duis H J, Minderhoud J M.et al Lightning stroke and neuropsychological impairment: cases and questions. J Neurol Neurosurg Psychiatry 199864763–769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Primeau M. Neurorehabilitation of behavioral disorders following lightning and electrical trauma. Neurorehabilitation 20052025–33. [PubMed] [Google Scholar]