Abstract
This report describes an apparent case of femoral nerve mononeuropathy in a 58-year-old equestrian due to mechanical stress. A woman presented at a chiropractic office complaining of right buttock pain radiating to the right groin and knee. A treatment plan, consisting of chiropractic adjustments in addition to stretching and myofascial therapy, was initiated. The goal was to reduce pain and inflammation in the sacroiliac articulation by restoring normal biomechanical function. A rehabilitation program to alleviate tension in the musculature was initiated to reduce mechanical stresses exerted on the femoral nerve. The patient received five treatments over a period of three weeks and became asymptomatic. Even though peripheral nerve entrapment is an uncommon condition, clinicians must not overlook the possibility of a femoral mononeuropathy as it can produce a complex presentation and lead to ineffective patient management.
Keywords: femoral nerve entrapment, mononeuropathy, chiropractic, peripheral nerve compression, iliopsoas muscle
Abstract
Cet article illustre la présentation clinique d’un cas de mononeuropathie fémorale d’origine mécanique chez une femme de 58 ans adepte d’équitation. Une femme ayant des douleurs à la fesse droite irradiant vers l’aine et le genou droit s’est présentée à une clinique chiropratique. Des traitements chiropratiques comprenant des ajustements, un programme d’étirements et une thérapie myofasciale ont été initiés dans le but de réduire les douleurs, l’inflammation et la dysfonction sacro-iliaque. Le traitement choisi visait aussi à réduire les tensions musculaires potentiellement responsables de la compression du nerf fémoral dans la région inguinale.
Les symptômes initialement présents se sont résorbés suite à une série de cinq traitements prodigués sur une période de trois semaines. Même si les compressions nerveuses périphériques au membre inférieur ne sont pas courantes, un clinicien devrait toujours considérer la possibilité d’une mononeuropathie du nerf fémoral puisque cette condition peut entraîner une série de signes et symptômes complexes et mener à une gestion clinique inadéquate de la condition.
Introduction
Although femoral mononeuropathy is considered a rare condition,1–3 the femoral nerve can be injured by several mechanisms: mechanical, pathological, traumatic and metabolic. The child delivery process can, in some cases, elicit a mechanically-induced femoral mononeuropathy. The lithotomy position2,4,5 causes compression and/or stretching of the nerve brought on by excessive flexion, abduction and external rotation of the hip.5 Mechanical stressors, such as impingement between muscles in athletes1,4 and traumatic hyperextension of the hip joint during a fall, have been documented in the literature.5,6 Space-occupying lesions from expanding or lacerative traumatic conditions, for example, hematomas,6–8 enlarged iliopsoas bursa,9 tumors, metastasis8, hip synovial cyst,10 iliopsoas anatomical variant11 and surgery,3,12,13 have also been described as potential causes of femoral mononeuropathy. Metabolic disorders can also, through biochemical interaction, alter nerve function and result in neuropathies. Among them, diabetes,4,8 hypotension, drug abuse, paraproteinemic diseases and herpes zoster infections4 have been associated with neuropathies.
The following report describes an apparent case of femoral nerve mononeuropathy potentially due to mechanical stress induced by horseback riding.
Case report
A 58-year-old retired woman presented to the chiropractic clinic in Trois-Rivières with sharp right buttock pain radiating to the right groin and knee. She also reported a “loss of sensation” over the superior and anterior part of the right knee. The constant pain, which was rated as 6 on a 10-cm visual analogue scale, appeared suddenly ten days before she decided to consult. The patient considered her condition as stable since its beginning, with a slight improvement in the first days. The pain was worst at night and kept her from working and doing her daily chores. The patient also reported muscle weaknesses during stair climbing. Sitting and standing positions aggravated the pain whereas non-weight bearing hip flexion relieved it. The patient did not mention any lumbar pain and had no prior existing condition or trauma. According to the conducted history no other health professional was consulted and the patient had never experienced a similar problem before. The patient was not on any medication and considered herself active and healthy even though she is a smoker. She mentioned that she did a lot of physical work and horseback riding, but had stopped for the last 10 days because of the pain.
Upon examination, fine touch, vibration and pain abnormalities were noted at the anterior aspect of the right thigh and medial to the knee. A diminished patellar reflex (see Table 1) was apparent with weakness of knee extension (4/5) and hip flexion (4/5). The sartorius muscle also showed decreased resistance force (4/5).14 Muscle testing was performed with a hand-held dynamometer (micro-FET 2, Hoggan health industries, Utah). Wadsworth and colleagues5 obtained reliability coefficients ranging from 63% to 98% with statistical significance (p < 0.05) on muscle testing with a hand-held dynamometer. Compression of the inguinal region reproduced pain in her knee. Tinel’s test over the inguinal ligament increased pain in the femoral nerve territory. Orthopedic examination including Gaenslen’s test, Yeoman’s test, Faber-Patrick test and thigh thrust test was negative.
Table 1.
Clinical outcomes throughout the treatment.
| Muscle | Side | Initial evaluation | After 3 treatments (10 days) | After 5 treatments (21 days) | |
|---|---|---|---|---|---|
| *Strength measure (kg) | Quadriceps | Left | 19,5 | 22,7 | 27,3 |
| Right | 15,9 | 18,2 | 20,5 | ||
| Sartorius | Left | 21,8 | 22,3 | 21,8 | |
| Right | 15,9 | 17,3 | 22,7 | ||
| Psoas | Left | 25,0 | 26,4 | 26,4 | |
| Right | 23,6 | 25,0 | 27,3 | ||
| Patellar reflex | Left | +2 | +2 | +2 | |
| Right | +1 | +1 | +2 | ||
| Sensory loss | Anterior aspect of the thigh and medial aspect of the knee | Improvement of sensation at the medial aspect of the knee | General improvement of sensation around the knee | ||
| Pain | 6/10 | No pain | No pain | ||
A manual dynamometer was use to measure the strength of the different muscles.
A treatment plan was initiated. Chiropractic palpation revealed pain and articular restriction at right L5/S1 and right sacroiliac joints. The patient received five treatments in a period of three weeks. Chiropractic adjustments consisting of diversified side-posture manipulations were administered on the right sacroiliac joint and L5–S1 segments. The patient also received myofascial therapy through ischemic compression over trigger points and during passive stretching of the involved muscles (rectus femoris and psoas muscles).
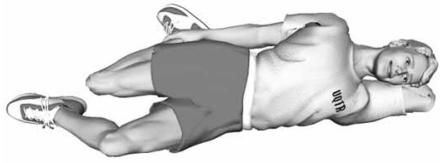
The rectus femoris muscle was stretched in lateral decubitus, and the psoas muscle in dorsal decubitus. The patient was also told to perform 30 seconds stretching exercises twice a day during the treatment period. These stretching exercises are illustrated in Figures 1 and 2.
Figure 1.
Stretching the rectus femoris muscle performed in side posture position by extending the ipsilateral hip, flexing the knee and maintaining the position for 30 seconds.
Figure 2.
Stretching the psoas muscle performed in supine position by flexing the contralateral hip and knee, extending the ipsilateral leg and holding the position for 30 seconds.
Ten days after the beginning of treatment, the patient considered that her general condition improved by 70%, and she was able to resume her daily activities without any problem. Her patellar reflex was still diminished. Seventeen days later, fine touch over the right knee was recovered, and general lower limb strengthening exercises were prescribed. After three weeks, both force and the patellar reflex returned to normal and were similar to those of the opposite lower limb. Clinical outcomes throughout the treatment plan are reported in Table 1.
Discussion
To document femoral nerve pathologies, a literature search of PubMed and Mantis databases was completed, using the following indexing terms: femoral mononeuropathy, compression mononeuropathy, femoral compression, spinal manipulation, neurophysiological effects, sensorimotor control AND spine, nerve compression syndrome.
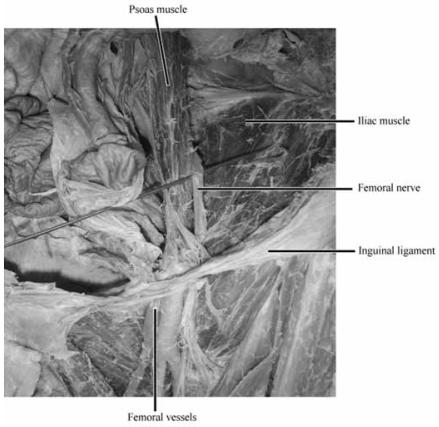
Femoral nerve compression is an uncommon clinical entity when compared with other mononeuropathies.5 It has been reported several times in the literature but its specific prevalence is unknown. The femoral nerve comes from the posterior division of the second, third and fourth roots of the lumbar plexus. It runs through the proximal fibers of the psoas major muscle and courses onwards laterally. Then it runs caudally between the iliacus and psoas muscles, reaching the deep side of the inguinal ligament lateral to the femoral artery. The femoral nerve is separated from the femoral blood vessels by continuous iliopectineal fascia joining the inguinal ligament to the psoas, the iliacus and transversalis fasciae.16 Under the inguinal ligament, the femoral nerve lies on the superficial border of the iliacus muscle. As it leaves the inguinal region, the nerve enters the femoral triangle, limited superiorly by the inguinal ligament, laterally by the sartorius muscle and medially by the long adductor muscle. At this level, the femoral nerve breaks up into several motor and sensory branches. Motor innervation supplies the iliacus, quadriceps, sartorius and pectineal muscles. Sensory innervation supplies the anteromedial aspect of the thighs as well as the medial aspect of the leg and foot down to the hallux.17
Typically, the symptoms of patients with a femoral mononeuropathy will manifest as an acute or subacute onset7 of severe pain in the inguinal region associated with tenderness in the iliac fossa.2 Some patients with femoral neuropathies do not experience any pain.1,5 However, the most striking symptoms are weakness of the quadriceps muscles and a decreased patellar reflex3,5,7 which may result in difficulty ambulating.12,13 Weakness of the quadriceps and sartorius muscles can culminate in reduced hip flexion and external rotation forces as well as diminished knee extension force.2 Patients may describe paresthesia of the anteromedial aspect of the thigh,5,12 possibly extending to sapheneous nerve distribution down to the hallux. The dysesthetic pain can vary from a burning sensation to sharp pain in the distal femoral nerve or more often in the sapheneous nerve territory.2 If the condition is chronic, it may result in wasting or atrophy of the distal quadriceps muscle due to denervation.1,13 Tinel’s sign (pain created by percussion over the area of the femoral nerve) will be positive over the inguinal ligament.6,7 In the presence of pain upon passive extension of the hip and a palpable mass and/or swelling of the iliacus muscle, hematoma must be considered.6 If the iliopsoas is involved, the location of the lesion must be at least 4 cm above the inguinal ligament and will impair hip flexion.5,12 Fasciculations observed in the quadriceps muscle indicate an anterior horn disease or an entrapment mononeuropathy.8 Another technique that may help to diagnose a femoral mononeuropathy is muscle testing using a scale of force14 to evaluate if there is any weakness of the quadriceps, psoas or sartorius muscles.8 Finally, to quantify the muscle atrophy, the circumference of the thighs can be measured by tape and compared to the asymptomatic leg.4
The diagnosis of femoral neuropathies relies upon the following methods. Electromyography (EMG) to detect waves and fibrillation potentials at rest, resulting from muscle denervation.1,4,6,8 To eliminate the possibility of an expanding lesion or swelling due to hematoma, computerized tomography (CT) scan of the pelvic region is indicated.6,7 Magnetic resonance imaging (MRI) also can reveal a mass in the inguinal or pelvic region,6 asymmetry of the quadriceps resulting from an atrophy or any affection of soft tissues.4 Nerve conduction velocity (NCV) study can serve to evaluate nerve integrity.12 The prognosis of femoral mononeuropathy can be accurately predicted by age and the amount of axonal loss.2 Kuntzer et al.,2 showed that older individual presenting with important axonal loss are more likely to have a poor prognosis. Young adults with minimal axonal loss are more likely to recover completely from a femoral mononeuropathy. Depending on the cause, different therapies can be used. If an expanding lesion such as hematoma is suspected, the role of physical therapy is questionable. Surgery would be the most effective approach combined with the cessation of any anticoagulative therapy.7 It is noteworthy that muscle force may be recovered satisfactorily with physical therapy, but the sensory deficit may persist over a year.12 Furthermore, the degree of motor deficit observed during the initial 10 days to a month does not seem to influence the prognosis.2 Rehabilitation is usually satisfactory from 6 to 24 months after the beginning of treatment.2 After two years, no further recovery is normally observed.2
Low back pain and pelvic pain are the most common reason why people seek chiropractic care. They occur in 23.6% of the population under chiropractic care.18 Many signs indicated that our patient had an entrapment mononeuropathy. Our patient manifested symptoms highly suggestive of peripheral compression of the femoral nerve. Weakness of the iliacus, quadriceps and sartorius muscles as well as the decreased patellar reflex supported this differential diagnosis. The location of her sensory loss indicated a peripheral nerve lesion. A single nerve root lesion could not account for the specific loss of cutaneous femoral nerve innervation. The presence of Tinel’s sign and painful compression of the inguinal area confirmed femoral nerve involvement. The patient had not suffered from any trauma recently, the intensity of pain decreased a few days after the first episode, and the absence of swelling or a palpable mass in the inguinal region limited the possibility of an expanding lesion such as an hematoma.6,7 Keeping in mind the fact that the patient had a good fitness level, and that there was no indication of a specific pathology either on physical examination or in her medical and familial history, it was postulated from her social history that she had a mechanical femoral mononeuropathy triggered by horseback riding. Although it would have to be confirmed by advanced testing, the femoral nerve might have been compressed and stretched through a combination of mechanisms. Two mechanisms were suspected in the present case.
It is important to mention that implication of the iliopsoas muscle indicates a lesion at least 4 cm above the inguinal ligament.5 The first hypothesis is that the femoral nerve might have been compressed and stretched in the iliopsoas groove under the thick iliac fascia (Figure 3).5,7
Figure 3.
The femoral nerve emerges from the posterior division of the second, third and fourth lumbar roots. It runs through the proximal fibers of the psoas muscle and courses onwards laterally. Then, it passes caudally between the iliacus and psoas muscles to reach the deep side of the inguinal ligament laterally to the femoral artery.
At that location, the nerve segment has a poor blood supply which makes it more susceptible to stretching lesions that can provoke ischemia.5 Repetitive trauma associated with rapid hip flexion and abduction could cause a femoral nerve lesion by stretching the nerve within the psoas muscle.3 This might have occurred repetitively while the patient was horseback riding, because the position of the legs on the “western saddle” forces the lower limbs in abduction and external rotation.
Our patient’s clinical presentation suggested that the lesion involved more than a compressive peripheral mononeuropathy. In fact, overuse or accumulation of micro-trauma of the sacroiliac articulation, that may have occurred during horseback riding, could have led to dysfunction and caused inflammation inside the joint.19 The pattern of pain in the ipsilateral buttock and groin and the sacroiliac dysfunction are signs and symptoms often related to a sacroiliac syndrome, according to Gatterman (1995).20 Inflammation within the joint may directly trigger reflex responses and activate the paravertebral musculature, consequently modifying its electrical activity and creating pain.21 Such dystonic activity of the psoas muscle might result in mechanical impairment of the femoral nerve that runs through its body.
The second hypothesis is that compression of the nerve under the inguinal ligament might have been a secondary cause of the mononeuropathy. It has been reported in the literature that excessive hip abduction, external rotation and flexion might compress the femoral nerve under the inguinal ligament,5 but would not involve the iliopsoas muscle. Inevitably, horseback riding results not only in persistence of an irritating posture but also produces repetitive microtraumas.22 Daily practice of that sport might have been a contributing factor to our patient’s mononeuropathy.
The goal of treatment in this case was to reduce inflammation by restoring the normal biomechanical function of the sacroiliac joint with chiropractic adjustments. Spinal manipulation can alter the neuromusculoskeletal system and modulate the pain process by modifying central facilitation of the spinal cord, thereby affecting the motor control system.23 In fact, recent evidences demonstrate that spinal manipulation evokes paraspinal muscle reflexes and alters motoneurone excitability. The effects of spinal manipulation on somatomotor activity may be quite complex, producing excitatory and inhibitory effects. Spinal manipulation can both increase the excitability of motor pathways in the spinal cord and depress the inflow of sensory information from muscle spindles.23 Myofascial and stretching therapies were administered to release tension in the musculature, possibly reducing mechanical stresses exerted on the femoral nerve.
The clinical presentation suggesting involvement of the sacroiliac joint and the surrounding hip musculature oriented the intervention toward chiropractic adjustments of the sacroiliac articulation combined with myofascial and stretching therapy of the involved muscles. The functional improvement and reduction of pain noted after only a few treatments indicated that peripheral nerve entrapment of mechanical origin can be resolved effectively with a conservative approach.
Finally, a number of limitations were identified in the present case study. Based on the patient’s history and exam findings, a differential diagnosis for this condition could have been sacroiliac joint dysfunction with associated myofascial pain syndrome. A gold standard modality such as NCV would have been necessary to confirm the diagnosis of femoral mononeuropathy.
Conclusion
Patients complaining of radiating pain and associated symptoms are commonly seen in chiropractic offices. Even though peripheral lower limb nerve entrapments are uncommon conditions, clinicians should be aware of their existence. Peripheral lower limb nerve mononeuropathy can be associated with confusing clinical manifestations and lead to ineffective patient management. In the event of mechanical nerve compression, such as in the present case, chiropractic treatment including spinal manipulation, myofascial therapy, stretching and strength exercises should be considered.
Footnotes
This study was funded by the Chaire de Recherche en Chiropratique FRCQ-Système Platinum.
References
- 1.Padua L, D’Aloya E, LoMonaco M, Padua R, Gregori B, Tonali P. Mononeuropathy of a distal branch of the femoral nerve in a body building champion. J Neurol Neurosurg Psychiatry. 1997;63(5):669–71. doi: 10.1136/jnnp.63.5.669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kuntzer T, van Melle G, Regli F. Clinical and prognostic features in unilateral femoral neuropathies. Muscle Nerve. 1997;20(2):205–11. doi: 10.1002/(sici)1097-4598(199702)20:2<205::aid-mus11>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 3.Papastefanou SL, Stevens K, Mulholland RC. Femoral nerve palsy. An unusual complication of anterior lumbar interbody fusion. Spine. 1994;19(24):2842–4. [PubMed] [Google Scholar]
- 4.Muellner T, Ganko A, Bugge W, Engebretsen L. Isolated femoral mononeuropathy in the athlete. Anatomic considerations and report of two cases. Am J Sports Med. 2001;29(6):814–7. doi: 10.1177/03635465010290062401. [DOI] [PubMed] [Google Scholar]
- 5.al Hakim M, Katirji B. Femoral mononeuropathy induced by the lithotomy position: a report of 5 cases with a review of literature. Muscle Nerve. 1993;16(9):891–5. doi: 10.1002/mus.880160902. [DOI] [PubMed] [Google Scholar]
- 6.Tamai K, Kuramochi T, Sakai H, Iwami N, Saotome K. Complete paralysis of the quadriceps muscle caused by traumatic iliacus hematoma: a case report. J Orthop Sci. 2002;7(6):713–6. doi: 10.1007/s007760200127. [DOI] [PubMed] [Google Scholar]
- 7.Pirouzmand F, Midha R. Subacute femoral compressive neuropathy from iliacus compartment hematoma. Can J Neurol Sci. 2001;28(2):155–8. doi: 10.1017/s0317167100052860. [DOI] [PubMed] [Google Scholar]
- 8.Seijo-Martinez M, Castro del Rio M, Fontoira E, Fontoira M. Acute femoral neuropathy secondary to an iliacus muscle hematoma. J Neurol Sci. 2003;209(1–2):119–22. doi: 10.1016/s0022-510x(03)00005-4. [DOI] [PubMed] [Google Scholar]
- 9.Yoon TR, Song EK, Chung JY, Park CH. Femoral neuropathy caused by enlarged iliopsoas bursa associated with osteonecrosis of femoral head – a case report. Acta Orthop Scand. 2000;71(3):322–4. doi: 10.1080/000164700317411960. [DOI] [PubMed] [Google Scholar]
- 10.Stuplich M, Hottinger AF, Stoupis C, Sturzenegger M. Combined femoral and obturator neuropathy caused by synovial cyst of the hip. Muscle Nerve. 2005;32(4):552–4. doi: 10.1002/mus.20364. [DOI] [PubMed] [Google Scholar]
- 11.Jelev L, Shivarov V, Surchev L. Bilateral variations of the psoas major and the iliacus muscles and presence of an undescribed variant muscle – accessory iliopsoas muscle. Ann Anat. 2005;187(3):281–6. doi: 10.1016/j.aanat.2004.10.006. [DOI] [PubMed] [Google Scholar]
- 12.Brooke JD, Cheng J, Misiaszek JE, Lafferty K. Amplitude modulation of the soleus H reflex in the human during active and passive stepping movements. Journal of Neurophysiology. 1995;73:102–11. doi: 10.1152/jn.1995.73.1.102. [DOI] [PubMed] [Google Scholar]
- 13.Farrow A, Morrison R, Pickersgill T, Currie R, Hammersley N. Transient femoral neuropathy after harvest of bone from the iliac crest. Br J Oral Maxillofac Surg. 2004;42(6):572–4. doi: 10.1016/j.bjoms.2004.06.014. [DOI] [PubMed] [Google Scholar]
- 14.Clarkson HM. Musculoskeletal assessment: joint range of motion and manual muscle strength. 2. Philadelphia: Lippincott Williams & Wilkins; 2000. [Google Scholar]
- 15.Wadsworth CT, Krishnan R, Sear M, Harrold J, Nielsen DH. Intrarater reliability of manual muscle testing and hand-held dynametric muscle testing. Phys Ther. 1987;67(9):1342–7. doi: 10.1093/ptj/67.9.1342. [DOI] [PubMed] [Google Scholar]
- 16.Gray S. Gray’s anatomy. 1. New York: Vintage Books; 1994. [Google Scholar]
- 17.Moore KL, Dalley AF. Clinically oriented anatomy. 4. Philadelphia: Lippincott Williams & Wilkins; 1999. [Google Scholar]
- 18.Christensen M. Job analysis of chiropractic. Colorado: National Boards of chiropractic examiners; 2005. p. 11. [Google Scholar]
- 19.DeMann LE., Jr Sacroiliac dysfunction in dancers with low back pain. Man Ther. 1997;2(1):2–10. doi: 10.1054/math.1997.0280. [DOI] [PubMed] [Google Scholar]
- 20.Gatterman MI. Foundation of Chiropractic Subluxation. st. Louis: Mosby; 1995. pp. 454–5. [Google Scholar]
- 21.Holm S, Indahl A, Solomonow M. Sensorimotor control of the spine. J Electromyogr Kinesiol. 2002;12(3):219–34. doi: 10.1016/s1050-6411(02)00028-7. [DOI] [PubMed] [Google Scholar]
- 22.Robertson C, Saratsiotis J. A review of compressive ulnar neuropathy at the elbow. J Manipulative Physiol Ther. 2005;28(5):345e1–e18. doi: 10.1016/j.jmpt.2005.04.005. [DOI] [PubMed] [Google Scholar]
- 23.Pickar JG. Neurophysiological effects of spinal manipulation. Spine J. 2002;2(5):357–71. doi: 10.1016/s1529-9430(02)00400-x. [DOI] [PubMed] [Google Scholar]