Abstract
Aim
To investigate the relationship between ratings of depressive symptoms and in vivo cortical acetylcholinesterase (AChE) activity in subjects with Parkinson's disease (PD) and parkinsonian dementia (PDem).
Methods
Subjects (with PD, n = 18, including subjects with PDem, n = 6, and normal controls, n = 10) underwent [11C]methyl‐4‐piperidinyl propionate AChE positron emission tomography imaging and clinical assessment including the Cornell Scale for Depression in Dementia (CSDD).
Results
Subjects with PD and PDem had higher scores on the CSDD compared with normal controls: 7.3 (5.4) and 2.8 (2.6), respectively (F = 6.9, p = 0.01). Pooled analysis demonstrated a significant inverse correlation between cortical AChE activity and CSDD scores: R = −0.5, p = 0.007. This correlation remained significant after controlling for Mini‐Mental State Examination scores.
Conclusion
Depressive symptomatology is associated with cortical cholinergic denervation in PD that tends to be more prominent when dementia is present.
Depression is a frequent non‐motor manifestation of Parkinson's disease.1 The pathophysiology of depression in PD is complex and probably related to the dysfunction of several neurotransmitter systems, including serotonin, dopamine and norepinephrine.2 However, a recent meta‐analysis of depression treatment studies in PD found less benefit from typical antidepressant treatment, particularly selective serotonin reuptake inhibitors, than seen in elderly patients without PD.3 A recent study on acute tryptophan depletion also failed to identify a specific serotonergic vulnerability for depression in PD.4 Dopaminergic denervation is unlikely to play a major role in depression, as antidepressant effects of levodopa treatment in PD are generally modest.5
A relatively unique feature of depression in PD is that mood disturbance is associated with a quantitative but not qualitative worsening of cognitive deficits.6 This modulatory effect of depression on cognitive impairment in PD suggests that a common mechanism might underlie both types of symptoms. We recently reported in vivo findings of more severe cholinergic denervation in parkinsonian dementia (PDem) compared with Alzheimer's disease,7 and cholinergic degeneration may play a significant role in the cognitive decline in PD.8 This raises the question of whether depression in PD is, at least in part, associated with cholinergic hypofunction.
Methods
Subjects
The study involved 28 male subjects: 12 with PD, 6 with PDem and 10 normal controls. There were no significant differences in age among the groups (PDem 73.5 (9.2) years, PD 71.2 (7.7) years and normal controls 69.2 (8.8) years; F = 0.5, NS). Subjects were diagnosed as having dementia if they met Diagnostic and statistical manual for mental disorders—4th edition (DMS‐IV) criteria for dementia.9 The PDem group consisted of subjects classified as having idiopathic PD with incident dementia or dementia with Lewy bodies. Previously, we found no significant difference in cortical acetylcholinesterase (AChE) activity between subjects having PD with incident dementia compared with those having dementia with Lewy bodies.7 Subjects with PDem had significantly lower Mini‐Mental State Examination (MMSE) scores than those with PD and normal controls (PDem 24.7 (4.3), PD 27.9 (1.3) and normal controls 29.4 (0.8), F = 9.1, p = 0.001).10 The Unified Parkinson's Disease Rating Scale (UPDRS) motor scores were not significantly different between the PDem (33.8 (8.6)) and PD (26.2 (12.5)) groups but differed as expected from the control subjects (1.8 (1.5)) (F = 27.5, p<0.001).11 The mean (SD) duration of motor symptoms was 5.7 (4.1) years in the PD and 3.8 (2.3) years in the PDem groups. The mean (SD) duration of dementia was 1.8 (2.6) years in the PDem group. None of the subjects was taking antidepressants, anticholinergic or cholinesterase inhibitor drugs. Dopaminergic drugs were withheld for 12–18 h before positron emission tomography (PET) imaging and the UPDRS motor examination in the patients. The Cornell Scale for Depression in Dementia (CSDD) was used to assess depressive symptomatology.12 The Neuropsychiatric Inventory Questionnaire (NPI‐Q), the brief form of the Neuropsychiatric Inventory, was also administered to the patients.13
Patients were recruited from the neurology clinics at the VA Medical Center and University of Pittsburgh, Pittsburgh, Pennsylvania, USA. The study was approved by the institutional review boards, and informed consent was obtained from all subjects.
AChE PET and brain MRI
The [11C]methyl‐4‐piperidinyl propionate (PMP) radioligand, a selective substrate for AChE hydrolysis, was prepared as described previously.14 Dynamic PET scanning was performed for 80 min immediately after a bolus intravenous injection of 555 MBq (15 mCi) of [11C]PMP. A volumetric spoiled gradient recall MRI was obtained using a 1.5 T scanner. Registration of the PET and magnetic resonance datasets, magnetic resonance‐based region of interest analysis and kinetic analysis has been reported previously.7 Mean neocortical [11C]PMP k3 activity was calculated as a composite score from bilateral frontal, parietal and lateral temporal cortices.
Statistical analysis
Multiple regression analysis was used to analyse depression and MMSE Scores in relation to cerebral AChE levels. Normative cognitive, mood and PET data were collected from normal controls. Unitailed analysis was used for the patient groups in accordance with our a priori hypothesis of an inverse relationship between the CSDD Scores and cortical AChE activity in the subjects with PD and PDem. Scores of the single‐item depression and apathy questions of the NPI‐Q were used for a post hoc analysis.
Results
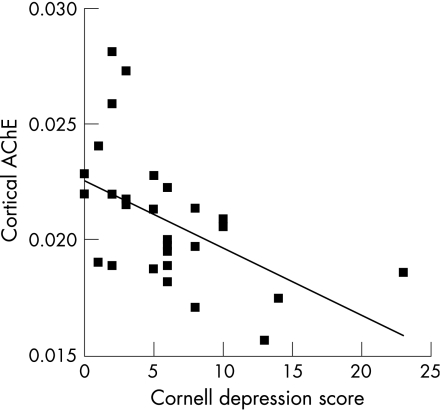
Subjects with PD and PDem had higher scores on the CSDD than normal controls: 7.3 (5.4) and 2.8 (2.6), respectively, F = 6.9, p = 0.01. CSDD scores tended to be higher in PDem (9.7 (3.4)) than in those with PD (6.1 (5.9)), but were not significantly different (t = 1.4, NS). Mean cortical AChE activity was decreased in both subjects with PDem (−18.8%) and PD (−11.4%) compared with normal controls (F = 6.2, p<0.01), but did not differ significantly between the PDem and PD groups (F = 1.8, NS). Pooled group analysis demonstrated a significant inverse correlation between cortical AChE activity and scores on the CSDD rating scale: R = −0.5, p = 0.007 (fig 1).
Figure 1 Cortical acetylcholinesterase (AChE) activity (k3 hydrolysis rate, per min) is plotted against Cornell Scale for Depression in Dementia scores in the combined subjects (R = 0.5, p = 0.007).
A significant inverse correlation was observed between CSDD and MMSE Scores in the combined groups (R = −0.42, p<0.05). Therefore, multiple regression analysis with cortical AChE activity as the dependent variable and MMSE and CSDD scores as independent regressors was performed. A significant overall effect was observed for cortical AChE activity (F = 9.4, p<0.001), with significant partial regressor effects for both the CSDD (F = 5.8, p<0.05) and the MMSE scores (F = 7.8, p<0.01) in the combined patient and control groups.
Analysis limited to the patients with PD and PDem confirmed an inverse correlation between cortical AChE activity and CSDD Score (R = −0.43, p<0.05). Regression analysis in the patients with PD and PDem also demonstrated an overall significant model (F = 3.7, p<0.05), with significant partial regressor effects for both the CSDD rating (F = 3.6, p<0.05) and the MMSE Scores (F = 3.2, p<0.05; table 1). There was no significant correlation between UPDRS motor scores and cortical AChE activity in the patients (R = 0.15, NS). There were also no significant correlations between CSDD and MMSE Scores (R = −0.16, NS), or between CSDD and UPDRS motor scores in the patients (R = 0.22, NS).
Table 1 Results of the multiple regression analysis using cortical acetylcholinesterase as a dependent parameter and scores for the Cornell Scale for Depression in Dementia and Mini‐Mental State Examination as regressors.
| Subjects | CSDD Score | MMSE Score | Overall model |
|---|---|---|---|
| Patients and controls | F = 5.8, p<0.05 | F = 7.8, p<0.01 | F = 9.4, p<0.001 |
| Patients only | F = 3.6, p<0.05 | F = 3.2, p<0.05 | F = 3.7, p<0.05 |
CSDD, Cornell Scale for Depression in Dementia; MMSE, Mini‐Mental State Examination.
A post hoc analysis was performed using scores on the single‐item depression and apathy scores of the NPI‐Q scale in the patients. Seven patients scored positive for either depression or apathy and five patients scored positive for both symptoms. Analysis of variance using cortical AChE as the dependent parameter and the depression and apathy items as independent variables demonstrated an overall significant model (F = 3.29, p<0.05); a significant effect of decreased cortical AChE activity and depression was observed in patients who reported depression compared with those who did not (k3 hydrolysis rates 0.0167 (0.0019) vs 0.0184 (0.0028), respectively; F = 3.72, p<0.05). By contrast, there was a non‐significant trend for differences in AChE activity between patients reporting apathy compared with those who did not (k3 hydrolysis rates 0.017 (0.0018) vs 0.0186 (0.0029), respectively; F = 2.86, p<0.1).
Discussion
We found that depressive symptomatology was significantly correlated with the severity of cortical cholinergic denervation. This correlation remained significant after controlling for global cognitive performance. In this study, we studied the combined groups of PD and PDem to better extract information from the spectrum of cognitive and mood non‐motor symptoms in this disorder, thereby eliminating a potentially arbitrary categorical distinction. A recent study reported findings of concomitant mood and cognitive impairments in a large series of patients with PD.15 A significantly higher number of patients with depression who, on testing, were found to have dementia, and a significantly greater proportion of patients with depression who, after 5 years, developed dementia suggested that depression in PD may be a forerunner of dementia.15 Cholinergic hypofunction as a mechanism underlying depression‐modulated cognitive impairment may explain why depression is a risk factor for dementia in PD.16 Previous studies have shown that elderly patients with depression are often impaired on tasks that require executive control processes and that a decrement in cognitive processing resources may be a trait marker of geriatric depression.17 A recent study has found more treatment failures with the selective serotonin reuptake inhibitor citalopram in geriatric patients with depression and concomitant executive cognitive impairment than in patients with geriatric depression alone, emphasising the potential need for non‐serotonergic antidepressant pharmacotherapy in such patients.18
Our study does have some limitations, including the relatively small sample size, the lack of an independent measure of apathy and the study population being restricted to men. Our limited post hoc analysis using NPI‐Q apathy and depression subscale data indicated that depression tended to be more correlated with cortical cholinergic activity than apathy.
In conclusion, our findings provide support for a cholinergic contribution to depressive symptoms in PD that tends to be more prominent when the disease is complicated by dementia. Further research is needed into the overlap with apathy, effects of executive cognitive impairment and how this interacts with the monoamine transmitter alterations in this disorder.
Acknowledgements
This study was supported by the Department of Veterans Affairs, the Pittsburgh Foundation and the NIA (AG‐05133). We thank our PET technologists for their skillful performance in data acquisition, cyclotron operators and chemists for their production of [11C]PMP, and research assistants Larry Ivanco and Tonya Engel for their help.
Abbreviations
AChE - acetylcholinesterase
CSDD - Cornell Scale for Depression in Dementia
MMSE - Mini‐Mental State Examination
NPI‐Q - Neuropsychiatric Inventory Questionnaire
PDem - parkinsonian dementia
PET - positron emission tomography
PMP - methyl‐4‐piperidinyl propionate
UPDRS - Unified Parkinson's Disease Rating Scale
Footnotes
Competing interests: None declared.
References
- 1.Weintraub D, Moberg P J, Duda J E.et al Effect of psychiatric and other nonmotor symptoms on disability in Parkinson's disease. J Am Geriatr Soc 200452784–788. [DOI] [PubMed] [Google Scholar]
- 2.Remy P, Doder M, Lees A.et al Depression in Parkinson's disease: loss of dopamine and noradrenaline innervation in the limbic system. Brain 20051281314–1322. [DOI] [PubMed] [Google Scholar]
- 3.Weintraub D, Morales K H, Moberg P J.et al Antidepressant studies in Parkinson's disease: a review and meta‐analysis. Mov Disord 2005201161–1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leentjens A F, Scholtissen B, Vreeling F W.et al The serotonergic hypothesis for depression in Parkinson's disease: an experimental approach. Neuropsychopharmacology 2006311009–1015. [DOI] [PubMed] [Google Scholar]
- 5.Growdon J H, Kieburtz K, McDermott M P.et al Levodopa improves motor function without impairing cognition in mild non‐demented Parkinson's disease patients. Parkinson Study Group. Neurology 1998501327–1331. [DOI] [PubMed] [Google Scholar]
- 6.Tröster A I, Stalp L D, Paolo A M.et al Neuropsychological impairment in Parkinson's disease with and without depression. Arch Neurol 1995521164–1169. [DOI] [PubMed] [Google Scholar]
- 7.Bohnen N I, Kaufer D I, Ivanco L.et al Cortical cholinergic function is more severely affected in Parkinsonian dementia than in Alzheimer's disease: an in vivo PET study. Arch Neurol 2003601745–1748. [DOI] [PubMed] [Google Scholar]
- 8.Zarow C, Lyness S A, Mortimer J A.et al Neuronal loss is greater in the locus coeruleus than nucleus basalis and substantia nigra in Alzheimer and Parkinson diseases. Arch Neurol 200360337–341. [DOI] [PubMed] [Google Scholar]
- 9.DSM‐IV Diagnostic and statistical manual of mental disorders. 4th edn. Washington, DC: American Psychiatric Association, 1994
- 10.Folstein M F, Folstein S E, McHugh P R. Mini‐mental state: a practical method for grading the cognitive state of patients for the clinician. J Psychiatry Res 197512189–198. [DOI] [PubMed] [Google Scholar]
- 11.Fahn S, Elton R. Members of the UPDRS development committee. Unified Parkinson's disease rating scale. In: Fahn S, Marsden C, Calne D, Goldstein M, eds. Recent developments in Parkinson's disease. Florham Park, NJ: Macmillan Healthcare Information, 1987153–164.
- 12.Alexopoulos G S, Abrams R C, Young R C.et al Cornell Scale for Depression in Dementia. Biol Psychiatry 198823271–284. [DOI] [PubMed] [Google Scholar]
- 13.Kaufer D I, Cummings J L, Ketchel P.et al Validation of the NPI‐Q, a brief clinical form of the Neuropsychiatric Inventory. J Neuropsychiatry Clin Neurosci 200012233–239. [DOI] [PubMed] [Google Scholar]
- 14.Snyder S E, Tluczek L, Jewett D M.et al Synthesis of 1‐[11C]methylpiperidin‐4‐yl propionate ([11C]PMP) for in vivo measurements of acetylcholinesterase activity. Nucl Med Biol 199825751–754. [DOI] [PubMed] [Google Scholar]
- 15.Lieberman A. Are dementia and depression in Parkinson's disease related? J Neurol Sci 2006248138–142. [DOI] [PubMed] [Google Scholar]
- 16.Marder K, Tang M‐X, Côté L.et al The frequency and associated risk factors for dementia in patients with Parkinson's disease. Arch Neurol 199552695–701. [DOI] [PubMed] [Google Scholar]
- 17.Nebes R D, Butters M A, Houck P R.et al Dual‐task performance in depressed geriatric patients. Psychiatry Res 2001102139–151. [DOI] [PubMed] [Google Scholar]
- 18.Alexopoulos G S, Kiosses D N, Heo M.et al Executive dysfunction and the course of geriatric depression. Biol Psychiatry 200558204–210. [DOI] [PubMed] [Google Scholar]