Abstract
Objectives
The research was designed to describe the care and communication processes during weaning from long-term mechanical ventilation (LTMV). A portion of those findings, specifically, how family members interact with the patient and respond to the ventilator and associated ICU bedside equipment during LTMV weaning, are reported here.
Methods
Ethnography conducted in a medical intensive care unit (MICU) and step-down MICU following 30 adults who were weaning from LTMV (> 4 days). Data collection involved field observations conducted from November 2001 to July 2003, interviews with patients, family members, and MICU clinicians, and clinical record review.
Results
Family members were present at the LTMV patients’ bedside during 46% of weaning trials and interacted with patients through touch, talking, and surveillance. Families’ bedside surveillance activities were interpretive of numerical monitor displays and laboratory values, protective of patient safety and comfort, and often focused exclusively on weaning. Interpretive language and surveillance were learned from and imitative of clinician behaviors. Clinicians characterized the family’s presence as helpful, a hindrance, or having no effect on the weaning process. Quantitative analysis using random coefficient modeling examining the effect of family presence on length of weaning trials showed significantly longer daily weaning trials when families were present (p < .0001).
Conclusion
Critical care clinicians influence families’ acquisition of interpretive surveillance skills at the bedside of patients who are weaning from LTMV. This study provides a potentially useful conceptual framework of family behaviors with long-term critically ill patients that could enhance the dialogue about family-centered care and guide future research on family presence in the ICU.
Keywords: prolonged mechanical ventilation, long-term mechanical ventilation, critical care, family presence, ICU visitation
Introduction
During critical illness, mechanical ventilation imposes physical and communication barriers between family members and their critically ill loved ones. Although numerous studies have been conducted of patient experiences with short and long-term mechanical ventilation, research has not focused on family interactions with patients during weaning from mechanical ventilation. Moreover, the importance of family members’ bedside presence and clinicians’ interpretation of family behaviors at the bedside have not been critically examined. As part of a larger study of the care and communication processes in weaning patients from long-term mechanical ventilation (LTMV), we sought to describe how family members interacted with the patient and responded to the ventilator and associated equipment during weaning trials.
Background/Significance
Most studies of family members in the ICU have focused on families’ needs for information, access to the patient, and participation in decisions to withdraw or withhold life sustaining treatment 1–17. Recently, patients’ perspectives of family presence and participation in the ICU have been investigated. Patients who survived critical illness and successfully weaned from mechanical ventilation reported that inclusion of family members in the weaning process was important to them 18–21. Patients rated family visitation as a nonstressful experience, identifying benefits such as reassurance, comfort, and calming from visitors22. Although psychosocial factors, such as anxiety, depression, and sleep deprivation are widely recognized to influence progress in weaning from LTMV 23, there have been no investigations of the effect of family presence on the weaning process.
In a study of spouses’ caregiving roles in the ICU, most participants reported wanting to take an active caregiving role with their critically ill spouse 24. Spouses felt positive about the ability to be close and helpful to their critically ill partner, reporting primarily non-technical caregiving activities such as talking and touching 24. In a recent British study, emotional support, presence, and normalizing talk were the primary patient care contributions of family members in the ICU25. An ethnographic study of 10 families’ experiences at the bedside in a Canadian neurological ICU described information seeking behaviors and efforts by families to assimilate into the culture of the ICU and to maintain connections with the brain-injured patient.26 Exploration of family members’ experiences and actions is timely. More patients are requiring prolonged mechanical ventilation.27, 28 Flexible, longer family visitation in ICU’s has become accepted practice and family-centered, culturally-sensitive care in the ICU continues to be a goal8, 29–32. Yet, little empirical data are available to guide families to an optimal bedside presence. Using data from an ethnographic study of the care and communication processes during weaning from long-term mechanical ventilation (LTMV), we sought to describe how family members interact with the patient and respond to the ventilator and associated ICU bedside equipment during LTMV weaning.
Design/Methods
A focused ethnography was conducted in an urban, tertiary care MICU and step-down MICU from November, 2001 to July, 2003. The study was approved by the University of Pittsburgh Institutional Review Board.
Setting
The MICU was a 20 bed unit with an adjacent 8 bed step down unit. All patient rooms were private, with the exception of one semi-private room. Most LTMV patients were transferred to the step-down MICU for progressive weaning, i.e., reduction of ventilatory support. Care in the step-down unit was managed by an acute care nurse practitioner, critical care medicine, or pulmonary medicine fellow in collaboration with an attending physician. Nurses and respiratory therapists rotated between the more acute MICU and the step-down unit. Both units followed a structured, restrictive visitation policy (6am–7am,10am–12pm, 2pm–3pm,6pm–7pm). Families were required to call into the unit from the waiting room to before visiting. Exceptions to scheduled visitation were made on an individual basis for patients and families in consultation with the nurse manager or care coordinator nurses.
Sample
Thirty adult patients who were weaning from LTMV (≥4 days) were purposively selected for variation in age, gender, ethnicity, neurocognitive status (by clinical record description), severity of illness (APACHE III), primary diagnosis, and likelihood to wean as predicted by critical care clinicians. Potential patient participants were identified by ICU clinicians and during rounds with attending physicians and acute care nurse practitioner. Informed consent for participation was obtained from patients, if decisionally capable, or their proxies. Family members, (n=41) were enrolled as participants and signed informed consents usually in conjunction with patient enrollment. Thirty-one enrolled family members, 27 to 74 years of age, participated in interviews. Clinicians received written and verbal information about the study; 31 clinicians were selected and signed informed consents to participate in interviews based on their involvement in the care of study patients. Patient characteristics are displayed on Table 1.
Table 1.
Patient Characteristics
| Mean ± SD (range) | |
|---|---|
| Age: | 59.5 ± 17.64 (25–87 years) |
| Hospital LOS: | 35.6 ± 25.2 (9–876 days)* |
| Days on MV: | 29.5 ± 30.8 (5–875 days)* |
| Number (%) | |
| Female Gender: | 16 (53) |
| Ethnicity: | |
| African-American | 4 (13) |
| Caucasian | 26 (84) |
| Primary Medical Dx: | |
| Cardio-pulmonary | 17 (57) |
| Surgical complication | 5 (17) |
| Cancer | 3 (10) |
| Neuromuscular | 5 (17) |
| Disposition | |
| Died in Hospital | 5 (17) |
| Home | 8 (27) |
| LTC/LTAC/rehab | 14 (47) |
| Other hospital | 3 (10) |
| Alive at 12 mos. | 12 (40) |
Two outliers excluded from analysis of mean
LTC = long term care, LTAC= long term acute care, rehab = rehabilitation hospital
Observations
Data collection involved field observations, interviews, and clinical record review (Table 2). Patients were followed longitudinally from the start of weaning trials to discharge from the step-down MICU. A “weaning trial” was defined as some period < 24 hours in length off full ventilatory support in the assist control mode. Typically patients weaned on CPAP settings < 12 or tracheostomy mask/T-piece oxygen trials.
Table 2.
Data Sources and Data Collection
| Data Sources | Data Collection Strategy | ||
|---|---|---|---|
| Interview (number) | Observation | Clinical Record Review | |
| Clinicians | yes | yes (progress notes) | |
| Physicians* | 11 | ||
| Respiratory Therapists | 7 | ||
| Nurses# | 10 | ||
| Social Worker | 1 | ||
| Physical Therapist | 1 | ||
| Nutritionist | 1 | ||
| Subtotal | 31 | ||
| Patients (n=30) | 18 | yes | yes (clinical data) |
| Family Members (n=41) | yes | yes (visitation) | |
| Spouse | 15 | ||
| Adult Child** | 8 | ||
| Parent | 6 | ||
| Sibling (sister) | 2 | ||
| Subtotal | 31 | ||
| Family Meetings (n=11) | yes | ||
includes attending physicians, critical care medicine & pulmonary medicine fellows.
includes acute care nurse practitioner and nurse case manager.
includes son-in-law.
Observations were conducted by one of two researchers (JT, MBH) in the clinical setting 4–5 days/week including evenings and weekends with a focus on observing weaning trials. Observations were recorded by dictated or handwritten fieldnotes which were expanded and transcribed verbatim into Microsoft Word. Researchers used an observation guide adapted from previous work33, 34 and the literature. Families’ talk, touch, physical stance, proximity to the patient, movement in the room, attention to electronic monitors and technological devices, and talk were documented.
Interviews
Audiotaped, semi-structured interviews, lasting 30–90 minutes, were conducted with family members. The family member interview guide included questions about perceptions of LTMV, the weaning process, and their role at the patient’s bedside. Patient interviews lasted 10–40 minutes and were audiotaped when possible. Patients were asked to identify actions by others, including family members, which were helpful or unhelpful to them during weaning from LTMV. Audiotaped, semi-structured interviews with clinicians, lasting 30–90 minutes, included open-ended questions about their views of family bedside presence during LTMV weaning.
Clinical record review
To describe the sample, demographic data were collected from the clinical record: age, diagnosis, severity of illness at study enrollment (APACHE III), length of stay, and discharge disposition. Retrospective review of clinical records and observer field notes were used to collect categorical (yes/no) data about family presence during weaning trials (n=437) and daily weaning time which were entered into an Excel version 10 (Microsoft Corp., 2002) spreadsheet.
Data management and analysis
Demographic data were analyzed and displayed descriptively (frequency, mean, standard deviation) (Table 1). Numerical data on family presence during weaning trials and time off full ventilatory support were analyzed by descriptive (frequency, percentage) and correlational statistics. Random coefficient modeling using PROC MIXED in SAS (version 8.2, SAS Institute, Cary NC) was used to investigate the relationship between the duration of the daily weaning trial and family presence. Family presence was entered into the model as a time-dependent indicator variable coded as 0 when the family was not present during the trial and 1 when family members were present.
Field notes and interviews were transcribed verbatim and reviewed for accuracy. Textual files were transferred into ATLAS.TI version 5.0 (Scientific Software Development, 2004) for organization and data management. Files were labeled with unique (patient) case identifiers as well as data type (e.g., interview, observation, clinical record note) and source (e.g., nurse, physician, patient, family member, etc). Interviews were purposefully integrated with other data sources to provide a comprehensive description of the phenomenon of interest – family bedside presence during weaning from LTMV.
Qualitative data analysis began with the first observation and continued throughout the study. Data were coded, or labeled, by comparing new data with previous data and by questioning within and across cases. 35 The coding schema was created by team consensus on coding definitions and grouping codes into categories. Behavioral sequences were mapped for common or recurring behavioral interactions during weaning.36 Each textual passage labeled as family presence was further reviewed to identify the co-occurring codes, dimensions, and context of family presence with patients during weaning. New concepts, describing the behavior of family members as they attended their critically ill relative became evident. For example, the concept ‘surveillance’ linked family presence with the critical care technology. Surveillance was examined within and across cases using matrix construction 37. To further qualify “family presence,” typologies (helpful, neutral, or hindrance) were developed directly from the language of the participants.
Monthly multi-disciplinary team analysis provided additional critique of the credibility of codes and oversight of the analytic process (MBH, VS, JT, RA). Dual coding (MBH, VS) with negotiated consensus was performed on approximately 40% of the data to add rigor to the analysis of this large dataset. A log of theoretical insights and methodological choices documents analysis and research decisions.
Results
Overview: Family Member Bedside Presence
Family members were present at some time during 201 (46.0%) of the 437 days in which weaning trials occurred. Family presence refers to a family member’s attendance at the critically ill patient’s bedside and was characterized by physical, psychological, or social connection or intimacy. Family members interacted with LTMV patients through affectionate and caring touch (hand holding, stroking hair or extremities, hugging, kissing, foot massage, adjusting the patient’s position), talking to the patient, and surveillance activities. Talk directed to the patient included verbal encouragement, coaching, “normalizing” social talk, and interpretations of clinical information. Surveillance was defined as family members’ active engagement in the observation and interpretation of the patient’s physiological or psychological status or numerical displays from the technological devices monitoring the patient. Figure 1 shows the primary behaviors defining family presence at the bedside and the dimensions of those behaviors.
Figure 1.
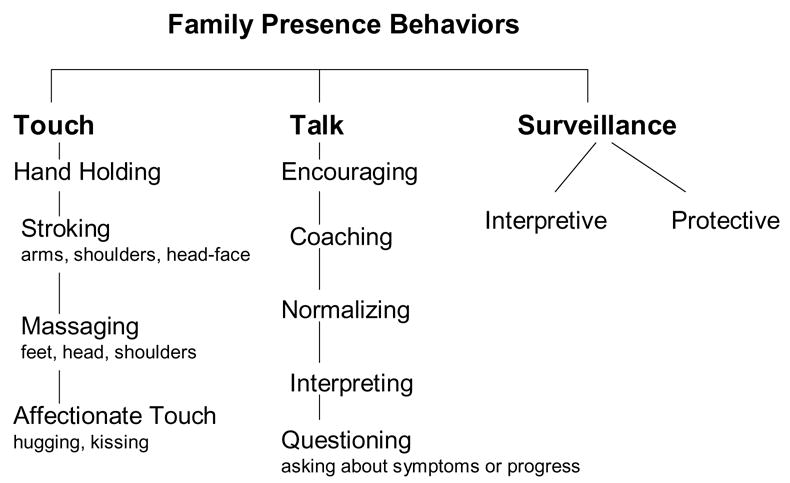
Family Presence at the Bedside of LTMV Patient
The family’s presence was characterized by the clinicians as either a) calming and helpful, b) a hindrance, or c) having no effect (neutral) on the weaning process.
(The family) would just hold her hand sometimes. You know they were really good. And that’s the kind of people that really help out. [respiratory therapist]
versus
(The family’s) pawing and annoyance almost hinders the wean… [respiratory therapist]
The nearly simultaneous actions of talking, touching, and surveillance are illustrated in the Textbox exemplar which presents a typical sequence of behaviors when family arrived at the patient’s bedside during weaning trials. A family member’s verbal greeting was often accompanied by touching the patient’s hand or shoulder, lifting the covers to inspect the patient’s extremities, and a surveying glance to the monitors or machinery. The behaviors and dimensions of family member’s bedside presence are described and analyzed in more detail below.
Touch
While touch is typically considered a natural or untaught act, in the context of serious illness and the high tech environment of the ICU, nurses played a significant role in advising family members, coaching, and modeling “appropriate” touch. One nurse deliberately positioned family members near the patient’s head and encouraged “soothing” touch of the hair and forehead during weaning trials.
Usually when I stand there, I am either holding his hand or stroking his arm. Somebody, the nursing staff, had mentioned when he was very, very sick, that touch is very important. [wife]
In fact, family members acknowledged that some of their responses or actions toward the patient were modeled after the clinicians’ words and actions.
Whenever I hear the doctors or nurses say what she should be doing, I tried to continue that…the (physical therapy) exercises and things like that…so I watched and I paid a lot of attention to the nurses and made sure I wasn’t overdoing it. [husband]
The human and physical connection through touch was extremely important to families as evidenced by the immediacy and regularity of touch when families arrived at bedside and the frequent occurrence of affectionate touch. For example, the mother of CL, a 53 year old man with newly diagnosed multiple myeloma and aspiration pneumonia, described using water-based aromatherapy as a vehicle for touching her critically ill son.
(I brought) some orange water, and I would bathe his face and his neck with that. And his palms and wrists. And, it did seem to relax him… And it was a way of me being able to touch him. [mother]
Talk
Encouraging and Coaching Talk
Verbal encouragement and coaching by family members helped the patient to achieve anxiety reduction or effective breathing patterns. CL’s mother described coaching her son during an episode of ventilator asynchrony by using talk and touch (i.e., hand holding).
I just grabbed hold of both of his hands with all my strength and I kept trying to get him to breathe evenly, you know. I said, “Breathe with me. We did this before, a long time ago, when I was having you…Let’s breathe together.” And he eventually did slow down somewhat. [mother]
JJ, a 58 year old patient with polymyositis, multi-organ failure, and colon cancer, described how his wife’s presence and words provided the necessary encouragement for him to work toward successful weaning despite overwhelming discouragement and fatigue.
My wife came in here and preached to me…She dogged me out about giving up. She said,…Why am I lacking faith now? Why am I all of a sudden giving up? …She renewed my faith. [patient]
Like touch, families were guided by clinicians to use talk when present at the bedside during LTMV weaning trials. The field note in Textbox 1 illustrates interactions in which a patient’s sister was instructed by the respiratory therapist to use encouraging talk with caring touch during weaning. Note that this instruction occurred simultaneously with the therapist’s explanations of lung physiology, laboratory results, and electronic monitor displays.
Normalizing Talk
Normalizing talk by family members, e.g., talking about everyday, non-illness related events, to the patient during visitation in the ICU has been previously described25. In our study, clinicians recognized the importance of normalizing talk characterizing it as a helpful family behavior that can distract patients from the work and worry of weaning.
It can be very wonderful, you know…Talking about other things. Sometimes just sitting there and being quiet, reading whatever mail came today. “What’s going on with Johnny today? Oh my gosh, the Bucs are playing today” That kind of stuff….. Normal and every day kinds of things. [respiratory therapist]
Interpretive Talk
Interpretive talk was a two-way process in which families served as a conduit between clinicians and patients, repeating or rephrasing information from clinicians and interpreting the experience to patients. Conversely, family members also interpreted patient responses, nonvocal communication, and clinical course to clinicians. The following field note illustrates the interplay between touch, coaching and encouraging talk from family members and the reciprocal sharing of technical-numerical information between clinician and family during a weaning trial. The daughter (DTR) models her words to the patient after the respiratory therapist (RT) while also interpreting the experience and the meaning of the patient’s restlessness as shoulder pain.
RT: You’re doing great. The best thing you can do is not to waste energy. Concentrate on your breathing in and out.
DTR Relax, mom. Good job.
The daughter stroked the patient’s hair out of her eyes. RT made more ventilator adjustments. The patient turned her head side to side and lifted her right shoulder…The daughter stroked the patient’s left shoulder. It was a very light touch with just her finger tips.
DTR: Relax, just relax mom. You’re doing fine. (in a whisper). I know your shoulder hurts. You’re doing good.
RT: (to the daughter) You’re doing good.
The daughter stood up and walked to the end of the bed as RT walked over to wash his hands.
DTR: Do you think she’ll be okay?
Then she looked at the monitor.
RT: She’s a little calmer now. You know she was on those (ventilator) settings yesterday. I don’t know what her blood pressure was.
DTR: About 160s, 170s.
RT: Good. She went 8 hours.
DTR: Yeah. She had dialysis and [plasma] pheresis in between. [field note]
In this exemplar, the daughter is a conduit of information between patient and clinician, repeating and translating the respiratory therapist’s information (you’re doing fine, relax) and providing historical clinical information to the respiratory therapist about the previous day’s blood pressure readings and therapies. These actions were accomplished because the daughter had a consistent bedside presence over time and because she had acquired interpretive surveillance skills.
Surveillance
Interpretive Surveillance
By observing clinicians and asking questions, family members learned to “read the monitors” and to interpret device alarms and monitor displays for themselves. Interpretation of numerical and graphical displays by family members extended to other associated critical care technologies, such as the cardiac, blood pressure, and pulse oximetry monitors. Surveillance activities, then, became common ground between family members and clinicians both linguistically and behaviorally.
We could read the gauges (on the ventilator). We learned how to read the dials. [wife]
(The) respiratory therapist…You know, we talk about PEEP and we talk about pressure support…and I said, “Now I get it!” [sister]
I watch the numbers and he (respiratory therapist) explained the numbers for me…how much (the patient) was breathing and stuff and I liked that. [wife]
Clinicians routinely reported objective data, such as hours off full ventilatory support, ventilator settings, oxygen saturation, and blood pressure, to family members. Clinicians helped family members to interpret the numerical displays and patients’ responses to the ventilator. The clinician’s role in explaining the equipment served several purposes – reassuring family members, reinforcing information to patients, and preparing families for surveillance activities.
A lot of times, you have to explain all this stuff to the family and I like to do that because then I’m kind of telling that to the patient again, you know, and reassuring the family. If you get (families) on your side, I’ll have them watch certain things.[respiratory therapist]
Family members were motivated to acquire the language as well as the skills of interpretive surveillance to share common ground with clinicians.
You know how they say “When in Rome..?” Okay, well, I’m in Rome. And I learn to speak your language basically. I don’t say “medicine;” I say “meds.” I don’t call it “carbon dioxide;” I call it “CO2.” …and I try to speak your language because I want to sound a little bit intelligent. I want you to understand that I am trying to understand you… I don’t know everything, but I’m trying. [daughter]
Interpretive surveillance extended from the monitoring equipment to the alarm features of the ventilator which were used by family members to interpret the patient’s condition or experience. As such, the alarm technology was treated as a communicative extension of the patient. The following field note illustrates such a technologically mediated interaction between an elderly patient and her adult daughter.
The patient’s daughter was holding and stroking the patient’s hand. She was responding enthusiastically to the patient’s eyes opening. It was difficult to determine if the patient recognized the daughter. An alarm sounded which was interpreted by the daughter as recognition, “She knows I’m here.” [field note]
Armed with new knowledge to “make sense” of the numbers, family members interpreted minute daily changes as evidence of progress or a setback. This required regular communication between family members and clinical staff, particularly respiratory therapists and nurses. Through their surveillance work, some family members became reliable informants about the patient’s clinical condition or progress. A physician commented,
Actually, sometimes (the patient’s sister) gets me more updated than the nurses. If you asked her, she probably knows what his secretions were 2.5 weeks ago and sometimes that kind of detail is useful. I enjoy talking to her ’cause I get more data out of her. From that point of view, …it helps me take care of him. [critical care fellow]
Protective Surveillance
Family surveillance also involved detecting changes, raising concerns, and asking questions of clinicians. Family members viewed this type of surveillance and questioning as their protective duty.
First thing, I came in (to the room) …There was…the mucus jar. I said “hmm, two days ago when I was here it was clear” …Yesterday I noticed it’s a little red and like little dark pieces of whatever. I called the nurse. I said, “Yesterday it was clear, why is it like that now?” So she explained…If I notice something one day and change in something else, I’ll ask questions…They got so many things to do per patient. It’s important that you come when you’re supposed to and follow the rules, you know. Make sure that you tell them whatever’s wrong or if you notice something wrong with (the patient), have questions about it, ask. [sister]
In an extreme example of interpretive and protective surveillance, one family member searched the wastebasket for clues about nursing care and treatment from discarded cardiac monitoring strips, noticing heart rate elevations and time intervals before treatment was initiated. Thus, protective surveillance behaviors were intertwined with issues of trust, interpretive surveillance and interpretative talk.
As part of their surveillance and protective presence at the bedside, families were instrumental in providing restraint free care by offering alternatives to physical restraint, objecting to physical restraint, and/or supervising time out of restraints. For example, the wife of a brain injured patient with left-sided hemiplegia brought in small bean bag toys - a leprechaun for St. Patrick’s Day, a bunny at Easter – to be placed in his right hand to prevent accidental dislodgement of the tracheostomy.
Protective surveillance behaviors were often interpreted by clinicians as family “anxiety,” “craziness,” or being “difficult.” A family member’s faulty or over-interpretation of patient response, or anxiety about weaning progress was viewed negatively by ICU staff.
(The patient) can go a long time (on a weaning trial) as long as I can keep her psycho daughter out of there. [Imitating daughter] “Mom, mom. Are you anxious? Are you breathing okay? Are you having pain?” She’s right in (the patient’s) face. I took her off (a weaning trial) last week because the daughter said to. She could have gone longer. [Respiratory therapist]
Thus, families’ enactment of protective surveillance impacted how they were viewed by the ICU staff.
The effects of family presence and surveillance
Although patients generally appreciated the presence of family members, some were not as positive in their evaluation. For example, OC a 56-year old patient with ARDS, told an interviewer that her children were “no help” during weaning, and that their visits “made her tired”. Family members also showed insight, albeit retrospective, about possible negative effects of their presence during weaning.
We were there at her bedside and my daughter was on one side and I was on the other. And I would say to her, “Are you short of breath?” and she’d squeeze my hand, “Yes.” The respiratory therapist was there and my daughter asked (the patient) if she wanted to be put back on (the ventilator). She squeezed my hand again for “Yes”, and the respiratory therapist put her right back on (full ventilatory support). I wonder if it’s maybe better if we weren’t there. We held her hand and we tried to give her support. But the next day we weren’t there when they put her on her wean and she went for two hours. And then the next day, she went for four hours. So we thought that maybe that our presence maybe made her a little more anxious. [husband]
Most clinicians recognized emotional support and encouragement as a positive and natural role for family members of patients who were experiencing prolonged critical illness. However, that view was tempered with negative comments and conditional statements indicating that clinicians perceived families as helpful as long as they were supportive of the clinicians’ actions, not upsetting the patient, and not adversarial.
A lot of times (pause), you’d want to hope that they [family members] would be supportive, but a lot of times even though they want what’s best, they want [the patient] off the ventilator, their pawing and annoyance almost hinders the wean…The way they like paw at them. (Raises voice in imitation) “You okay? You breathing? Do you need suctioned?” Just constant…That hinders the patient. Most families are pretty okay. [respiratory therapist.]
A lot of families though, all they seem to accomplish is to agitate the patient and keep them from sleeping. [attending physician]
If (families) are calm, (they can help the patient). It depends on what relationship they had before because relationships don’t change in the hospital. They just get exaggerated. …(Some) patients get real tachypneic, tachycardic, blood pressure will go up and it happens almost immediately when family comes in the room. Sometimes I’ll have the family step out and talk to them and watch (the patient). And the (vital signs) will go back down. [nurse]
Clinicians characterized family presence as helpful, a hindrance, or having no effect (neutral) on weaning based on their evaluation of actions supporting treatment goals. In general, quietly sitting next to the patient, hand-holding and soothing talk were consistently described as helpful, whereas a tense demeanor, hovering, being overly close, and asking the patient about symptoms, activity tolerance, or weaning progress were considered a hindrance. Finally, experienced clinicians evaluated the abilities and effects that individual family members had on LTMV patients to deliberatively include or exclude them from weaning trials.
When we weaned (the patient), her family just stayed by her and they were quiet. You know she was working. I would talk to her and just try to keep reassuring…and just keep her peaceful. They’d just hold her hand sometimes. You know they were really good. And that’s the kind of people that really help out. [respiratory therapist]
If the family member is a “Nervous Nellie, I will limit the patient’s or family’s access during weans. [nurse]
You can kind of gauge if this family member is going to hurt or help. And if, if they’re someone that’s going to help, I’ll kind of include them in with everything I’m doing, but if not, I’ll kind of just say “I’m just checking everything.” [respiratory therapist]
We further explored the effect that family member presence may have on LTMV weaning trials by quantitatively examining the relationship between family presence and length of daily weaning trial (in hours) using random coefficient modeling. Daily weaning trials for LTMV patients in this sample were significantly longer when families were present (mean = 9.80 hours) during the weaning trial than when families were not present (mean = 7.62 hours) (F 1, 395) = 18.15, p <.0001).
Limitations
The relationship between family presence and longer daily weaning trials is exciting but requires cautious interpretation due to the small sample size and categorical nature of the family presence variable. The percentage of weaning time for which families were present was not measured. Moreover, we do not know to what extent families were aware that weaning trials were underway during their visits and how that may or may not have altered their behaviors and interactions at the bedside.
Discussion
This study is the first to document and describe how family members interact with patients during weaning from LTMV. The data provide exemplars of family presence as calming and helpful, as well as examples of situations wherein family presence was a potential hindrance to the weaning process. The analysis identified and described characteristics of patient-family interactions that were judged by clinicians to facilitate or interfere with the weaning process; these typologies and descriptions could be the basis for family member education programs. Additionally, expanded understanding and use of the nurses’ and respiratory therapists’ skills in modeling, advising, and coaching helpful family presence during weaning is an important avenue for exploration. This study identified specific aspects of family presence and clinician involvement with family that extend the current conceptualization of patient-focused, family centered care in ICU’s. Moreover, the data validate family presence during weaning as a potentially beneficial strategy as indicated by the finding that LTMV patients weaned for significantly longer periods when family members were present for some portion of the trial.
Surveillance of patients via technology is recognized as central to critical care nursing and competent care 38–42 Findings of this study confirm a human-technology interface occurring between family members, patients, clinicians, and mechanical equipment (ventilators, cardiac monitors, oxygenation monitors) in which family members interpret “signals” and information from technological displays to gauge their loved one’s condition and progress.26 Clinicians, particularly nurses and respiratory therapists, play key roles in explaining the technologies and numerical displays to family visitors. Importantly, families modeled the behaviors of clinicians and actively attempted to acquire the language of clinicians regarding ICU technologies. This specific finding is similar to previous descriptions26, 43 of family bedside presence in the trauma emergency room and neurological ICU where family members “monitor(ed) the monitors,” and modeled their verbal responses to the patient in tone and content after the nurse.43(p. 245) Similarly, Morse and Pooler 43 observed nurses coaching families to “talk to” or touch the patient. The present study illustrates a rather sophisticated acquisition of interpretive skills and language on the part of family members during prolonged critical illness as well as greater comfort with high tech life support equipment and physical touch as they acclimated to and learned about the ICU environment.26
This work is the first to include extensive observations of and interviews with respiratory therapists as well as nurses and physicians. Clearly, the role of respiratory therapists at the bedside is critical in teaching families about the ventilator and associated technologies, interpreting monitor displays, and encouraging and modeling therapeutic talk and touch in ways that assist families to understand how their presence can benefit patients weaning from LTMV.
This study extends previous research by describing family members’ experiences and actions within the context of long-term critical illness. Hupcey and Zimmerman21 interviewed 45 adult patients following 3–30 days in medical or surgical ICUs to describe the psychosocial needs of ICU patients and the behaviors of families, friends, and staff that helped or hindered meeting these needs. Patients identified the presence of family and friends as supportive (e.g., watchful, encouraging) and a positive influence toward meeting their primary need of “feeling safe.” That study, however, also reported negative psychosocial effects of family visitation.21 Patients became distressed when visitors withdrew or hid information and when visitors were upset or crying at the bedside. The conceptualization of family “watchfulness” in the ICU21 has now been extended to specific surveillance activities: inspection of the patient’s extremities, interpretation of monitor displays,26 prevention of device disruption, and questioning changes in condition.
Additionally, these findings suggest a need for better understanding of family behavior in the ICU. Actions or responses by ICU family members that are often perceived as “hypervigilant” by clinicians (i.e., continuously at bedside, requiring detailed information, examining clinical records, and note-taking)44 are essentially forms of surveillance and, for some families, may be required as a protective filial duty or to adequately prepare families to communicate with clinicians. Further research is needed to: a) better characterize such behaviors, b) describe extremes in surveillance behavior, c) measure family caregiver vigilance 45, d) measure time that families spend at the bedside during weaning trials, e) rate the quality of family presence activities, and f) develop and test interventions to guide families toward a positive bedside presence.
This study further conceptualized the surveillance role of family members as a “conduit for clinical information” about the patient. Although the patient’s family has been considered a source of medical history, the observation that families can play an important role in clinical assessment of chronically critically ill patients is conceptually new. Family members who learned to understand the basic characteristics of the patient’s illness and treatment and who were present every day were able to share information about trends in the patient’s physical or psychological signs and treatments. Findings of this study provide a potentially useful conceptual framework of family behaviors in interaction with critically ill patients, machinery, and clinicians (Figure 1) that could enhance the dialogue about family-centered care and guide future research on family needs and presence in the ICU. In summary, family bedside presence during weaning from LTMV represents an important and potentially beneficial interaction that may be influenced by coaching and instruction from nurses, respiratory therapists, and physicians.
Textbox 1. Behavioral Sequence: Surveillance-Talk-Touch
10:05 AM. The patient is lying in bed, tracheostomy connected to trach mask. His sister is talking to the respiratory therapist (RT) who is again explaining “good lung down” for the left lower lobe problem.
RT: Looks like he’s worked up.
He advises the sister to reassure the patient, encourage him.
RT: The nurse last night talked him down. You can do anything, put a cloth on his head, stroke his head. You may be the best person to do that.
RT shows the sister the arterial blood gas results from 5a.m., this morning.
RT: His numbers are great.
Sister: It’s great
RT: Great, yes, it is….
The sister looks under the sheet at his feet. [Surveillance]
Sister (to patient): Good morning, pumpkin. Sleepy? Huh? [Talk]
She is leaning over the right side bed rail, stroking the patient’s head, massaging his hair gently. [Touch]
Sister (to patient): Wanna watch some TV?
RT looks at monitor, then patient, and then to his watch. He is counting the respirations. They are RR=28, HR = 121, SaO2=89–91
10:11AM
RN (concerned look to the monitor): Think he’d do better with his head up a little? She raises head of the bed.
Sister: How long has he been on this side?
RT: We just turned him. His respiratory rate is coming down. That’s correct. Just talk to him.
Sister peeks under the sheet and begins stroking his head again. The patient’s eyes are closed and he is turned away from the TV in a right side lying position.
Acknowledgments
Thanks to Michael P. Donahoe, MD, Dana DiVirgilio-Thomas, BA, Tricia Roesch, MSN, CRNP, Lauren Broyles, BSN, Bridget Coyne, MSN, CRNP.
Footnotes
Work performed at the University of Pittsburgh and supported by the National Institute for Nursing Research, NIH, U.S. Public Health Service (Grant No. R01 NR007973)
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Auerbach SM, Kiesler DJ, Wartella J, Rausch S, Ward KR, Ivatury R. Optimism, satisfaction with needs met, interpersonal perceptions of the healthcare team, and emotional distress in patients’ family members during critical care hospitalization. Am J Crit Care. 2005;14(3):202–210. [PubMed] [Google Scholar]
- 2.Bouman CC. Identifying priority concerns of families of ICU patients. Dimens Crit Care Nurs. 1984;3(5):313–319. doi: 10.1097/00003465-198409000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Burr G. Contextualizing critical care family needs through triangulation: an Australian study. Intensive Crit Care Nurs. 1998;14(4):161–169. doi: 10.1016/s0964-3397(98)80473-4. [DOI] [PubMed] [Google Scholar]
- 4.Daley L. The perceived immediate needs of families with relatives in the intensive care setting. Heart Lung. 1984;13(3):231–237. [PubMed] [Google Scholar]
- 5.Hickey M. What are the needs of families of critically ill patients? A review of the literature since 1976. Heart Lung. 1990;19(4):401–415. [PubMed] [Google Scholar]
- 6.Jamerson PA, Scheibmeir M, Bott MJ, Crighton F, Hinton RH, Cobb AK. The experiences of families with a relative in the intensive care unit. Heart Lung. 1996;25(6):467–474. doi: 10.1016/s0147-9563(96)80049-5. [DOI] [PubMed] [Google Scholar]
- 7.Kleinpell RM, Powers MJ. Needs of family members of intensive care unit patients. Appl Nurs Res. 1992;5(1):2–8. doi: 10.1016/s0897-1897(05)80076-x. [DOI] [PubMed] [Google Scholar]
- 8.Molter NC. Needs of relatives of critically ill patients: a descriptive study. Heart Lung. 1979;8(2):332–339. [PubMed] [Google Scholar]
- 9.Molter NC. Families are not visitors in the critical care unit. Dimens Crit Care Nurs. 1994;13(1):2–3. doi: 10.1097/00003465-199401000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Takman C, Severinsson E. Comparing Norwegian nurses’ and physicians’ perceptions of the needs of significant others in intensive care units. J Clin Nurs. 2005;14(5):621–631. doi: 10.1111/j.1365-2702.2004.01038.x. [DOI] [PubMed] [Google Scholar]
- 11.Verhaeghe S, Defloor T, Van Zuuren F, Duijnstee M, Grypdonck M. The needs and experiences of family members of adult patients in an intensive care unit: a review of the literature. J Clin Nurs. 2005;14(4):501–509. doi: 10.1111/j.1365-2702.2004.01081.x. [DOI] [PubMed] [Google Scholar]
- 12.Norton SA, Tilden VP, Tolle SW, Nelson CA, Eggman ST. Life support withdrawal: communication and conflict. Am J Crit Care. 2003;12(6):548–555. [PubMed] [Google Scholar]
- 13.Prendergast TJ, Puntillo KA. Withdrawal of life support: intensive caring at the end of life. JAMA. 2002;288(21):2732–2740. doi: 10.1001/jama.288.21.2732. [see comment] [DOI] [PubMed] [Google Scholar]
- 14.Mirr MP. Factors affecting decisions made by family members of patients with severe head injury. Heart Lung. 1991;20(3):228–235. [PubMed] [Google Scholar]
- 15.Swigart V, Lidz C, Butterworth V, Arnold R. Letting go: family willingness to forgo life support. Heart Lung. 1996;25(6):483–494. doi: 10.1016/s0147-9563(96)80051-3. [DOI] [PubMed] [Google Scholar]
- 16.Tilden VP, Tolle SW, Nelson CA, Fields J. Family decision-making to withdraw life-sustaining treatments from hospitalized patients. Nurs Res. 2001;50(2):105–115. doi: 10.1097/00006199-200103000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Engstrom A, Soderberg S. The experiences of partners of critically ill persons in an intensive care unit. Intensive & Critical Care Nursing. 2004;20(5):299–308. doi: 10.1016/j.iccn.2004.05.009. [DOI] [PubMed] [Google Scholar]
- 18.Bertolotti G, Carone M. From mechanical ventilation to home-care: the psychological approach. Monaldi Arch Chest Dis. 1994;49(6):537–540. [PubMed] [Google Scholar]
- 19.Jacavone J, Young J. Use of pulmonary rehabilitation strategies to wean a difficult-to-wean patient: case study. Crit Care Nurse. 1998;18(6):29–37. [PubMed] [Google Scholar]
- 20.Logan J, Jenny J. Qualitative analysis of patients’ work during mechanical ventilation and weaning. Heart Lung. 1997;26(2):140–147. doi: 10.1016/s0147-9563(97)90074-1. [DOI] [PubMed] [Google Scholar]
- 21.Hupcey JE, Zimmerman HE. The need to know: experiences of critically ill patients. Am J Crit Care. 2000;9(3):192–198. [PubMed] [Google Scholar]
- 22.Gonzalez CE, Carroll DL, Elliott JS, Fitzgerald PA, Vallent HJ. Visiting preferences of patients in the intensive care unit and in a complex care medical unit. American Journal of Critical Care. 2004;13(3):194–198. [PubMed] [Google Scholar]
- 23.Burns SM, Clochesy JM, Hanneman SKG, Ingersoll GE, Knebel AR, Shekleton ME. Weaning from long-term mechanical ventilation. Am J Crit Care. 1995;4(1):4–22. [PubMed] [Google Scholar]
- 24.Eldredge D. Helping at the bedside: spouses’ preferences for helping critically ill patients. Res Nurs Health. 2004;27(5):307–321. doi: 10.1002/nur.20033. [DOI] [PubMed] [Google Scholar]
- 25.Williams CM. The identification of family members’ contribution to patients’ care in the intensive care unit: a naturalistic inquiry. Nurs Crit Care. 2005;10(1):6–14. doi: 10.1111/j.1362-1017.2005.00092.x. [DOI] [PubMed] [Google Scholar]
- 26.Lam P, Beaulieu M. Experiences of families in the neurological ICU: a “bedside phenomenon”. J Neurosci Nurs. 2004;36(3):142–146. [PubMed] [Google Scholar]
- 27.Needham DM, Bronskill SE, Calinawan JR, Sibbald WJ, Pronovost PJ, Laupacis A. Projected incidence of mechanical ventilation in Ontario to 2026: Preparing for the aging baby boomers. Crit Care Med. 2005;33(3):574–579. doi: 10.1097/01.ccm.0000155992.21174.31. [see comment] [DOI] [PubMed] [Google Scholar]
- 28.Behrendt CE. Acute respiratory failure in the United States: incidence and 31-day survival. Chest. 2000;118(4):1100–1105. doi: 10.1378/chest.118.4.1100. [DOI] [PubMed] [Google Scholar]
- 29.Wright F, Cohen S, Caroselli C. Diverse decisions. How culture affects ethical decision making. Crit Care Nurs Clin North Am. 1997;9(1):63–74. [PubMed] [Google Scholar]
- 30.Henneman EA, Cardin S. Family-centered critical care: a practical approach to making it happen. Crit Care Nurse. 2002;22(6):12–19. [PubMed] [Google Scholar]
- 31.Azoulay E, Pochard F, Chevret S, et al. Family participation in care to the critically ill: opinions of families and staff. Intensive Care Med. 2003;29(9):1498–1504. doi: 10.1007/s00134-003-1904-y. [DOI] [PubMed] [Google Scholar]
- 32.Gentling SJ, Grady R, Mattox KL. Hospital administrator’s perspective: the Critical Care Family Assistance Program. Chest. 2005;128(3 Suppl) doi: 10.1378/chest.128.3_suppl.103S. [DOI] [PubMed] [Google Scholar]
- 33.Happ MB, Roesch TK, Kagan SH. Patient communication following head and neck cancer surgery: a pilot study using electronic speech-generating devices. Oncol Nurs Forum. 2005;32(6):1179–1187. doi: 10.1188/05.ONF.1179-1187. [DOI] [PubMed] [Google Scholar]
- 34.Happ MB, Roesch TK, Garrett K. Electronic voice-output communication aids for temporarily nonspeaking patients in a medical intensive care unit: a feasibility study. Heart & Lung. 2004;33(2):92–101. doi: 10.1016/j.hrtlng.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 35.Strauss A, Corbin J. Basics of Qualitative Research: techniques and procedures for developing grounded theory. 2. Thousand Oaks, CA: Sage Publishing; 1998. [Google Scholar]
- 36.Happ MB, Swigart V, Tate J, Crighton MH. Event analysis techniques. Advances in Nursing Science. 2004;27(3):239–248. doi: 10.1097/00012272-200407000-00008. [DOI] [PubMed] [Google Scholar]
- 37.Miles MB, Huberman AM. Qualitative Data Analysis: An expanded sourcebook. 2. Thousand Oaks: Sage Publishing; 1994. [Google Scholar]
- 38.Cooper MC. The intersection of technology and care in the ICU. ANS Adv Nurs Sci. 1993;15(3):23–32. doi: 10.1097/00012272-199303000-00005. [DOI] [PubMed] [Google Scholar]
- 39.Ray MA. Technological caring: a new model in critical care. Dimens Crit Care Nurs. 1987;6(3):166–173. [PubMed] [Google Scholar]
- 40.Barnard A, Sandelowski M. Technology and humane nursing care: (ir)reconcilable or invented difference? J Adv Nurs. 2001;34(3):367–375. doi: 10.1046/j.1365-2648.2001.01768.x. [DOI] [PubMed] [Google Scholar]
- 41.Benner P, Hooper-Kyriakidis P, Stannard D. Clinical wisdom and interventions in critical care: A thinking-in-action approach. Philadelphia: WB Saunders Company; 1999. [Google Scholar]
- 42.Wikström AC, Sätterlund US. Patient on display – a study of everyday practice in intensive care. J Adv Nurs. 2003;43(4):376–383. doi: 10.1046/j.1365-2648.2003.02726.x. [DOI] [PubMed] [Google Scholar]
- 43.Morse JM, Pooler C. Patient-family-nurse interactions in the trauma-resuscitation room. Am J Crit Care. 2002;11:240–249. [PubMed] [Google Scholar]
- 44.Slota M, Shearn D, Potersnak K, Haas L. Perspectives on family-centered, flexible visitation in the intensive care unit setting. Crit Care Med. 2003;31(5 Suppl) doi: 10.1097/01.CCM.0000065276.61814.B2. [DOI] [PubMed] [Google Scholar]
- 45.Mahoney DF, Jones RN, Coon DW, Mendelsohn AB, Gitlin LN, Ory M. The Caregiver Vigilance Scale: application and validation in the Resources for Enhancing Alzheimer’s Caregiver Health (REACH) project. Am J Alzheimers Dis Other Demen. 2003;18(1):39–48. doi: 10.1177/153331750301800110. [DOI] [PMC free article] [PubMed] [Google Scholar]


