Abstract
Objective
This longitudinal study aimed to identify the predictors of leaving during the first year of employment from the cotton spinning mill environment in newly hired workers.
Methods
One hundred and ninety eight consecutively appointed new employees were investigated by questionnaire, lung function test, and skin test. They were examined before employment and at the end of the 1st week, and the 1st, 3rd, 6th, and 12th month after starting work and when possible before leaving their job. 572 personal dust sampling and 191 endotoxin measurements were performed to assess the environmental exposure. For the univariate analysis χ2, Student t tests, ANOVA, and Kruskall Wallis tests were used. Cox proportional hazards analysis was used to identify factors associated with leaving the job.
Results
Fifty three per cent of workers left the mill environment during their first working year. Work related lower respiratory tract symptoms reported at the third month were associated with an increase rate of leaving the industry compared to those remaining in the industry (25% v 4.8%; p<0.005). Having respiratory symptoms at the first month of work predicted those leaving the industry at some point in the next 11 months. According to the Cox model, increasing age and having work related lower respiratory tract symptoms were found to be predictors for leaving job at the first working year. Atopic status, dust and endotoxin levels, and lung function changes were not consistently predictive of workers who left the industry in the follow up period.
Conclusion
This study demonstrated that work related respiratory symptoms can predict workers likely to leave the cotton mill environment during the first year of employment, but atopy or acute lung function changes do not.
Keywords: byssinosis, cotton dust, healthy worker effect, respiratory symptoms, textile workers
There are a variety of respiratory disorders recognised in workers exposed to organic dusts including cotton. The classical descriptions of chronic byssinosis were first studied epidemiologically by Richard Schilling and colleagues.1 They described the frequent presence of a feeling of chest tightness and shortness of breath, experienced on the first day of the working week.2 Besides the chronic symptoms and baseline lung function decline among the cotton workers after long term exposure, acute airway responses such as cough, wheeze, shortness of breath, and acute lung function decline are observed following short term exposure.3 Chronic byssinosis has since been separated in terminology from the immediate experience of respiratory decline seen in naïve cotton workers (acute byssinosis). Cross shift changes in lung function and symptoms have been characterised by the World Health Organization and led to a new classification of byssinosis.4
It has been suggested that the acute responses to cotton dust explain the frequently recognised high labour turnover in new cotton workers and the subsequent finding of low levels of atopic status seen in many cross sectional studies of cotton workers.5 The assumption is that healthy workers survive in the industry and those susceptible to acute responses leave in the first few weeks or months of exposure as they find the environment too challenging. The impact on exposure to cotton dust and its contaminants within the first few months has not been fully evaluated.
In Turkey, the cotton textile industry has a high employment level and a high labour turnover compared with the other industries.6 It has been postulated that the most important reasons for such a high labour turnover in this industry are local economic and social conditions.7 Alternatively, the immediate health effects of the environmental exposure could also be the explanation.
This study was designed to investigate in detail the association between exposure to cotton dust and health related responses. The health outcomes and potential risk factors were respiratory symptoms experienced and related to the work environment, cross shift and cross week changes in lung function, baseline atopic status, and the level of exposure to cotton dust and its contaminants. Specifically we wished to ascertain, in a closely monitored population of new workers in a cotton spinning population with a high labour turnover, whether early adverse reactions to the environment were the cause of workers leaving the industry.
Methods
Study population
This longitudinal study was performed on the predictors of termination in the first year of employment among 198 consecutive newly hired workers at three cotton textile mills in Istanbul.
The baseline data were collected in September 1999. During the first year of the study, 198 consecutive newly hired workers were approached and each worker was followed until leaving the cotton mill or the completion of one year of employment.
The baseline examinations were performed before starting the work. Follow up examinations were performed at week 1 and months 1, 3, and 6 and at the end of 12 months of continuous employment. Workers who left during the time period were studied before leaving (when possible) or contacted by letter/phone when they quit work without notice.
Workers were identified who left the cotton mills completely (100 workers), or who changed from cotton production exposed to non‐production jobs (five workers), groups we called “leavers”.
Environmental exposure assessment
In order to assess environmental exposure, a total of 572 personal dust sampling and 191 personal endotoxin measurements were performed as part of a weekly hygiene monitoring programme. All occupational groups were identified and sampled wherever practical.
Personal breathing zone cotton dust measurements were performed with the Institute of Occupational Medicine sampling head, 25 mm Whatman GF/A microglass fibre filters, and Casella Vortex Standard personal sampling pumps. Details of the dust sampling techniques used are described in detail elsewhere.8
Endotoxin assays were performed from the personal sampling filters using a quantitative kinetic turbidimetric method (LAL 5000e series) as previously described.9
Ascribing individual exposure
For each worker, personal cotton dust exposure and endotoxin exposure were calculated as the geometric mean of any dust sampling performed specifically on them, if two or more samples were collected during the course of the study. For other workers who had not been individually sampled during the course of the study (22 workers; 11%) or who had only been sampled once (35 workers; 18%), the median values of workers sampled in the same mill with the same occupational classification was calculated and ascribed to that individual. This method of ascribing is similar to that used in previous epidemiological studies of cotton workers, is validated by existing studies demonstrating close relations between exposure and health effects, and led to changes in recommended standards to exposure monitoring for cotton textile workers in the UK.10,11,12
As a result, every worker was given a personalised occupational exposure measurement, based on their individual job allocation at the time or based on their actual exposure measurements during the course of the study.
Questionnaires
All questionnaires were modified from the Medical Research Council (MRC) respiratory questionnaire.13 The MRC respiratory questionnaire was first translated to Turkish and then translated back to English by different translators to verify accuracy. The questionnaires were conducted in face to face interviews by a single trained nurse for all time points in the study. Three different types of questionnaire were used at the follow up surveys. The baseline questionnaire (Q1) was designed to describe the demographics, work history, past exposure, smoking habits, and pre‐employment (baseline) respiratory symptoms. The second type of questionnaire (Q2–6) was used to detect any changes in workroom or occupation of the individual, the development of work related symptoms, and changes in smoking habits in the follow up evaluations. All the active workers attended the questionnaire performances in these five follow up points. A final brief questionnaire (Q7) was developed for workers leaving the study after quitting the job. This questionnaire asked the reasons for leaving the employment in the cotton mills. For those workers who did not attend attempts were made to contact the workers by telephone or letter if up to date contact details were available.
Lung function tests
Lung function tests were performed in all surveys by a trained technician using a Vitalograph Series S dry wedge spirometer based on the criteria of American Thoracic Society.14 Calibration was performed on a daily basis. The tests were conducted at least three times until an acceptable reproducibility was obtained (a minimum of three values with less than 5% variability). The largest forced expiratory volume in the first second (FEV1) was selected and corrected according to the temperature. Each individual observed value was compared with the predicted values using Polgar equations15 and European summary equations.16 For all subjects aged 18 and younger, Polgar equations were used to calculate the predicted values. European summary equations were used for the subjects older than 18 years assuming no change in predicted lung function for workers aged 18–25 (that is, the predicted value was calculated as if for a 25 year old).
Lung function tests were performed before and after the shifts on the first and the last day of the working week at each study time period. A response rate of between 90–100% was obtained for each individual timepoint for ongoing exposed workers.
In order to control for diurnal variation of lung function over the course of the day, all tests were performed on the same shift (8am–4pm shift) as all workers were rotating between morning, afternoon, and night shifts.
In workers who quit work, all were invited to attend again for lung function testing after cessation of cotton dust exposure.
Skin tests
One hundred and forty five workers (73.2%) attended the skin test. A trained nurse performed and assessed the skin tests at the mill. All workers were invited to undergo skin testing to 10 common allergens (cat, dog, house dust mite, cockroach, grass, tree, atemisia, aspergillus, alternaria, cladisporium) to define atopy. Each allergen was assessed separately. Atopy was defined as one or more wheals of up to 3 mm after correcting for negative control.
Definition of endpoints
Symptoms were classified as lower respiratory tract symptoms (cough, phlegm, chest tightness, and shortness of breath) (LRTS) or upper respiratory tract symptoms (ocular and nasal irritation) (URTS). The “work related” symptoms were defined as any symptom that developed after first starting to work in the mill environment, which improved on holidays or on days away from work or that were reported as being worse when working. Workers were classified as current smoker, ex‐smoker, or non‐smoker according to their baseline questionnaire. If the workers started smoking during the follow up period they were reclassified as current smokers.
Acute airway response was categorised by two definitions: cross shift and cross week change. Cross shift change was defined as the difference between before shift and after shift FEV1 values on the first working day (cross shift ΔFEV1). Cross week change was defined as the difference between before shift FEV1 first day and after shift FEV1 values on the fifth working day of the week (cross shift ΔFEV1). The percentages of absolute FEV1 change over a work shift and a work week was used to describe the acute lung function effect. Those with more than a 5% change in lung function and those with 5% or less deterioration of lung function across the time period involved were defined as acute responders or non‐acute responders.
Statistical analysis
At each time point, univariate analysis was performed and current workers were compared with those who had recently left.
Factors predicting subsequent “leaving” at each time point were also investigated by univariate analysis. The significance of univariate differences was assessed by χ2, Student t tests, ANOVA, and Kruskall Wallis depending on the nature of the data.
In order to identify factors associated with leaving the job during the entire follow up period (one year) Cox proportional hazards analysis was used. As the leavers who have left within the first week had no data of work related symptoms and acute lung function change, the “first week leavers” (25 workers) were not included in this model and analysed separately.
The backward elimination method was used. Hazard ratios and 95% confidence intervals were calculated. A p value <0.05 was considered significant.
Results
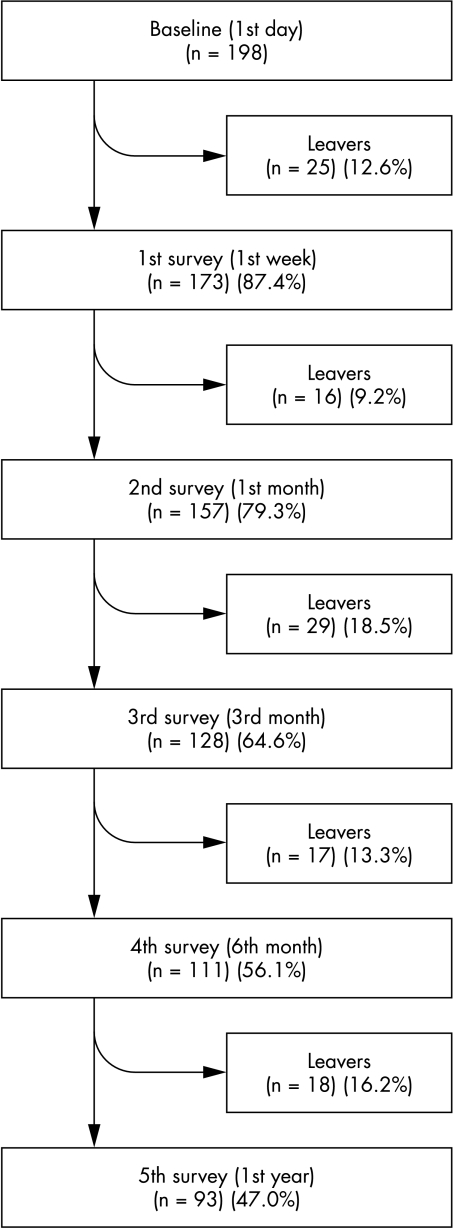
A total of 105 workers (53%) left exposure before the completion of 12 months and 93 newly hired cotton workers (47%) were still employed exposed to cotton spinning processes after 12 months. In figure 1, the numbers of leavers and continuous workers are presented for each stage of follow up.
Figure 1 Number of leavers and active workers at each follow up point.
None of the workers had respiratory symptoms at the time of employment, but 28 (14%), had either nasal (2%) or ocular irritation (13%). There was no significant relation between these baseline symptoms and age, sex, or current smoking. Twenty nine workers (20.4%) were defined as atopic based on their positive skin test results. Atopy was not associated with age, sex, past exposure, pre‐employment symptoms, or lung function test results.
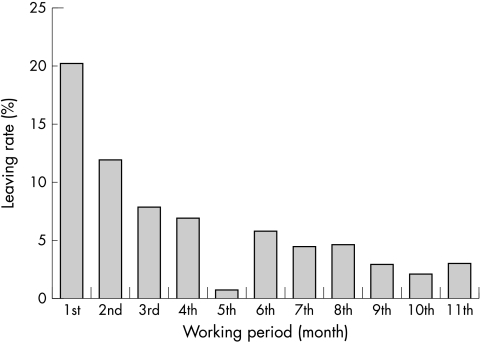
After being hired to the job, 13% of workers quit the job through the first working week, 20% in the first month, 12% in the second month, 8% in the third month, and about 5% in every month between the fourth and the 12th month (fig 2). By the end of the first 12 months a total of 105 workers (53%) had left the work environment in the cotton mill.
Figure 2 Leaving rate in each working month.
Only 69 leavers out of 105 were reached for the final interview (Q7) after quitting the job. Four of them reported health reasons (6%) and six (9%) reported unhealthy work environment as the reasons for leaving. The other self reported quitting reasons were about changing their life (33%), friction in workplace or dismissal, (37%) and work strain (15%). None of the workers who quit work had an FEV1 of less than 80% of predicted normal (data not shown).
Table 1 demonstrates the main characteristics and environmental exposure levels of all “leavers” and active workers. The leavers were older than the active workers. There were more smokers among leavers than active workers in this univariate analysis. However this significance disappeared in the Cox analyses.
Table 1 Comparison of baseline characteristics and environmental exposure among leavers and active workers.
| Leavers (n = 105) | Active workers (n = 93) | p Value | |
|---|---|---|---|
| Mean (SD) age (years) | 18.9 (3.6) | 17.9 (2.2) | 0.02 |
| Male, n (%) | 54 (51.4) | 46 (49.5) | 0.78 |
| Mill, n (%) | |||
| 1 | 51 (48.6) | 41 (44.1) | 0.40 |
| 2 | 13 (12.4) | 18 (19.4) | |
| 3 | 41 (39.0) | 34 (36.5) | |
| Cotton type*, n (%) | |||
| 100% cotton | 92 (92.9) | 83 (91.2) | 0.66 |
| Blend | 7 (7.1) | 8 (8.8) | |
| Current smoker, n (%) | 44 (41.9) | 22 (23.7) | 0.007 |
| Past exposure, n (%) | 7 (6.7) | 8 (8.6) | 0.61 |
| Dust concentration (median) (mg/m3) | 1.95 | 2.09 | 0.83 |
| Endotoxin concentration (median) (EU/m3) | 254.60 | 213.74 | 0.89 |
| Atopy†, n (%) | 10 (20.4) | 19 (20.4) | 0.99 |
| Baseline lung function test (n = 186) | |||
| Abnormal, n (%) | 2 (2.0) | 1 (1.2) | 0.56 |
| Pre‐employment symptoms, n (%) | 16 (15.2) | 12 (12.9) | 0.64 |
*n = 190.
†n = 142.
Porters in spinning left work more commonly compared to all other occupation groups (88% v 12% respectively). However, bobbin carriers in winding (71% v 29%) and draw/speed frame operatives and combers (65% v 35%) tended to stay in the industry when compared to all other occupation groups.
At each follow up period, “leavers” since the previous study visit and “active workers” were compared according to whether they reported symptoms at their previous study visit and on the basis of their previous lung function. Only at one—the third survey (between the first and third months)—was the prevalence of work related lower respiratory tract symptoms found to be higher in the workers who had left in that time period when compared to active workers (table 2). Lung function was not found to be different in “leavers” at any time point.
Table 2 Comparisons of leavers and active workers according to their work related symptoms and lung function tests at each follow up period point.
| 2nd survey (first month) | 3rd survey (third month) | 4th survey (sixth month) | 5th survey (first year) | |||||
|---|---|---|---|---|---|---|---|---|
| Leavers | Active workers | Leavers | Active workers | Leavers | Active workers | Leavers | Active workers | |
| WR‐LRTS, n/N | 0/16 | 5/157 | 6/24 | 6/125 | 3/17 | 17/111 | 0/17 | 4/93 |
| (%) | – | (3.2) | (25.0)* | (4.8) | (17.6) | (15.3) | – | (4.3) |
| WR‐URTS, n/N | 4/16 | 50/157 | 12/24 | 49/125 | 7/17 | 49/111 | 4/17 | 32/93 |
| (%) | (25.0) | (31.8) | (50.0) | (39.2) | (41.2) | (44.1) | (23.5) | (34.4) |
| Cross shift ΔFEV1 | 3/16 | 31/146 | 2/23 | 16/123 | 0/17 | 10/111 | 3/17 | 21/92 |
| −5% ⩽, n/N (%) | (18.8) | (21.2) | (8.7) | (13.0) | – | (9.0) | (17.6) | (22.8) |
| Cross week ΔFEV1 | 4/13 | 47/138 | 3/19 | 26/110 | 1/17 | 18/111 | 4/17 | 21/91 |
| −5% ⩽, n/N (%) | (30.8) | (34.1) | (15.8) | (23.6) | (5.9) | (16.2) | (23.5) | (23.1) |
WR‐LRTS, work related lower respiratory tract symptoms; WR‐URTS, work related upper respiratory tract symptoms; Δ, change.
*p<0.005.
An analysis of factors predicting subsequent “leaving” at each time point demonstrated that workers, who had WR‐LRTS at the first month of work, were more likely to leave at some point in the next 11 months than those who did not have symptoms at the first month (66.7% v 36.5%; p<0.05). This analysis demonstrated that the “leavers” who had respiratory symptoms after the first month left work significantly earlier than those who had not (mean working days: 41 v 124).
In addition, workers who had WR‐URTS at the first month were also found to be more likely to quit their job in the next 11 months (49.2% v 31.8%; p<0.05).
Table 3 summarises the results of the Cox proportional hazard analysis. According to this model increasing age (HR = 1.09, CI 1.03 to 1.15) and WR‐LRTS (HR = 2.03, CI 1.01 to 4.07) were found to be predictors for quitting job at the first working year, after correcting for other confounders.
Table 3 Results of Cox proportional hazards model of the factors associated with quitting job during the first year.
| Variables* | β | p value | HR (95% CI) |
|---|---|---|---|
| Age (1 year) | 0.09 | 0.005 | 1.09 (1.03 to 1.15) |
| WR‐LRTS | |||
| No | |||
| Yes | 0.71 | 0.047 | 2.03 (1.01 to 4.07) |
| Cross shift ΔFEV1 | |||
| Non‐decliners | |||
| Decliners | −0.70 | 0.062 | 0.50 (0.24 to 1.05) |
WR‐LRTS, work related lower respiratory tract symptoms; Δ, change.
*Factors included in analyses are age, sex, mill, occupational group, past exposure, dust level, endotoxin level, smoking, cross shift ΔFEV1, cross week ΔFEV1, WR‐LRTS, and WR‐URTS.
Attempts to identify factors that were related to workers leaving within the first week were all unproductive. The data have not been shown for brevity.
Discussion
This longitudinal study of 198 new starters employed in a series of Turkish cotton mills has defined respiratory symptoms lung function, atopic status, and environmental exposure prospectively in a cohort of newly hired cotton workers. It has allowed an investigation of relations between development of symptoms, lung function responses, and leaving the cotton environment within the first 12 months. Little previous work is available on newly hired workers.
In Turkey, there is a higher turnover rate in the textile industry compared with other industries. Korkusuz pointed out the turnover rate was 35% in Turkish textile industry in one year.6 Similarly, the labour turnover was high in this study, with 13% of workers leaving within the first week of employment. Most of these early leavers cited dissatisfaction with the job and problems/friction with supervisors/colleagues as the main reason for leaving.
A few workers reported previous cotton exposure, but were still included in the study. It is of note that a proportion of these previously exposed workers reported pre‐existing URTS, although there were no reports of LRTS in any worker prior to employment. In a subanalysis we investigated the presence of previous employment in the cotton industry for its independent effect on leaving. No influence was found, although the numbers involved are small. We elected to leave these workers in the analysed study population and use past exposure as a possible independent predictor variable in the final Cox regression analysis.
The high participation rate for all workers continuing in the mill enhances the study. The only exception to the high participation rate was the number of workers who failed to respond to follow up questionnaires or phone calls on leaving the mill environment. Despite the permanent presence of the nurse and technician responsible for clinical and hygiene assessments on site, many of the workers who left the cotton exposed environment did so without prior notice. This made it impossible to secure maximum response to lung function and questionnaires at the time of leaving. We investigated if there was any baseline difference between these “leavers” who did not report for follow up and those who did. The baseline demographic characteristics were no different between the groups. In addition it is worth noting that the response rate for targeting “leavers” was much higher in this prospective study than is normally obtained for a retrospective study of ex‐employees.
Previous cross sectional studies have reported a low prevalence of atopic individuals in workers who remain in the cotton industry. It has commonly been suggested that such a low prevalence of atopy in cross sectional studies is caused by atopic workers finding the environmental exposure to dust, endotoxin, and multiple fungal and bacterial allergens too challenging for their allergic status. It has been considered that allergic workers will quit the environment within the first few months, leaving a healthy population. The current study has found no evidence to support this argument. There was no relation between atopy and leaving the cotton industry in the first year of employment and no relation between baseline atopic status and the development of across shift or across working week lung function change. Some recent studies also showed no influence of atopy on the risk of leaving the cotton mill environment for newly employed workers.17,18 Wang and colleagues have shown that the “healthy worker survivor effect” was a possible reason for decreased respiratory symptoms at one year.19
Similarly the study has failed to show a predictive effect of changes in across shift lung function or across week lung function decline in the exposure as predictors of individuals selecting out of the mill environment.
However, the presence or development of respiratory symptoms does predict individuals who subsequently leave the industry. This finding is consistent in both the univariate and Cox regression analysis. Both work related upper and lower respiratory symptoms may have a selection effect.
One of the key questions is whether the relation between the development of symptoms in early periods of exposure (even in the absence of pre‐existing atopy or lung function change) can itself influence the nature of the “surviving population”, has implications both for the cotton industry and other populations where a healthy worker survival effect has been suggested. Bearing in mind that the effect in the first year of employment studied here can only be statistically related to symptoms but not lung function or atopy makes a generalisable extrapolation of the principle tenuous.
The aetiological agent(s) within the cotton mill environment that is/are responsible for the development of respiratory symptoms (that cannot be measurably associated with lung function changes) in this population remains uncertain. Endotoxin and total dust concentrations are theoretically the most likely aetiological factors, but there was no convincing pattern of association between leaving the cotton mills and the level of exposure in this study. It is important to state that this study has only investigated leaving in the first 12 months and a different design is required to investigate mid term or long term workers for reasons for leaving later in the employment history.
In conclusion this study of new starters in a cotton industry has demonstrated that WR‐LRTS detected at the first working month can predict workers likely to leave from cotton mill environment during the first year of employment. However, there is no evidence of the previously held view that atopic individuals are more likely to select out, or that monitoring of lung function across shift or across the working week will predict those unable to tolerate the environment at the first year of employment.
A large scale geographical collaboration in this type of population is urgently needed to verify these findings and their representative nature.
Acknowledgements
This study was supported by grants from the Cotton Industry War Memorial Trust and from Marmara University Research Foundation. Endotoxin analyses were performed by Dr Gael Tavernier of North West Lung Centre. The authors thank Nurten Bucan and Gaffur Bircan for technical assistance in the mills.
Abbreviations
FEV1 - forced expiratory volume in one second
LRTS - lower respiratory tract symptoms
MRC - Medical Research Council
URTS - upper respiratory tract symptoms
WR - work related
References
- 1.Schilling R S F, Huges J P W, Dingwall‐Fordyce I.et al An epidemiological study of byssinosis among Lancashire cotton workers. Br J Ind Med 195512217–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schilling R S F. Byssinosis in cotton and other textile workers. Lancet 1956ii261–265. [DOI] [PubMed] [Google Scholar]
- 3.Niven R M, Pickering C A C. Byssinosis and related diseases. Eur Res Mon 199911286–300. [Google Scholar]
- 4.World Health Organization Recommended health based occupational exposure limits for selected vegetable dusts. Report of a WHO study group. Technical report series 684 1983 [PubMed]
- 5.Koskela R S, Klockars M, Jarven E. Mortality and disability among cotton mill workers. Br J Ind Med 199047384–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Korkusuz M R. Analyzing of work condition at weaving industry. PhD Thesis, Dokuz Eylul University Institute of Social Science. Izmir 1995
- 7.Binbir S. Analyzing of work condition at textile and confection industry in Turkey and the world. PhD Thesis. Istanbul University Institute of Social Science. Istanbul 2002
- 8.Niven R M, Fishwick D, Pickering C A C.et al A study of the performance and comparability of the sampling response to cotton dust of work area and personal sampling techniques. Ann Occup Hyg 199236349–362. [DOI] [PubMed] [Google Scholar]
- 9.Simpson J C G, Niven R M L, Pickering C A C.et al Comparative personal exposures to organic dusts and endotoxin. Ann Occup Hyg 199943107–115. [PubMed] [Google Scholar]
- 10.Fishwick D, Fletcher A M, Pickering C A C.et al Lung function, bronchial reactivity, atopic status and dust exposure in Lancashire mill operatives. Am Rev Respir Dis 19921451103–1108. [DOI] [PubMed] [Google Scholar]
- 11.Fishwick D, Fletcher A M, Pickering C A C.et al Respiratory symptoms and dust exposure in Lancashire coton and manmade fibre mill operatives. Am J Respir Crit Care Med 1994150441–447. [DOI] [PubMed] [Google Scholar]
- 12.Niven R McL, Fletcher A M, Pickering C A C.et al Chronic bronchitis in textile workers. Thorax 19975222–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.MRC Committee on research into chronic bronchitis 1966. Questionnaire in respiratory symptoms and instruction for its use. London: MRC, 1966
- 14.American Thoracic Society Snowbird workshop on standardization of spirometry. Am Rev Respir Dis 1979119831–838. [DOI] [PubMed] [Google Scholar]
- 15.Polgar G, Promadhat V. Pulmonary function testing in children: techniques and standards. Philadelphia: WB Saunders Co, 1971, 170–80, 254
- 16.Quanjer P. ed. Standardized lung function testing. Report of Working Party on Standardization of Lung Function Tests. Bull Eur Physiopathol Respir 198319(Suppl 5)45–51. [Google Scholar]
- 17.Zhong Y, Li D, Qinyan M A.et al Lung function and symptoms among cotton workers and dropouts three years after the start of work. Int J Occup Environ Healht 20028297–300. [DOI] [PubMed] [Google Scholar]
- 18.Wang X‐R, Pan L‐D, Zhang H‐X.et al A longitudinal observation of early pulmonary responses to cotton dust. Occup Environ Med 200360115–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang X R, Pan L D, Zhang H X.et al Follow‐up study of respiratory health of newly‐hired female cotton textile workers. Am J Ind Med 200241111–118. [DOI] [PubMed] [Google Scholar]