Abstract
Objectives
Sick building syndrome (SBS) is described as a group of symptoms attributed to the physical environment of specific buildings. Isolating particular environmental features responsible for the symptoms has proved difficult. This study explores the role and significance of the physical and psychosocial work environment in explaining SBS.
Methods
Cross sectional data on the physical environment of a selection of buildings were added to individual data from the Whitehall II study—an ongoing health survey of office based civil servants. A self‐report questionnaire was used to capture 10 symptoms of the SBS and psychosocial work stress. In total, 4052 participants aged 42–62 years working in 44 buildings were included in this study.
Results
No significant relation was found between most aspects of the physical work environment and symptom prevalence, adjusted for age, sex, and employment grade. Positive (non‐significant) relations were found only with airborne bacteria, inhalable dust, dry bulb temperature, relative humidity, and having some control over the local physical environment. Greater effects were found with features of the psychosocial work environment including high job demands and low support. Only psychosocial work characteristics and control over the physical environment were independently associated with symptoms in the multivariate analysis.
Conclusions
The physical environment of office buildings appears to be less important than features of the psychosocial work environment in explaining differences in the prevalence of symptoms.
Keywords: sick building syndrome, office environment, psychosocial work characteristics
It has been proposed that a cluster of symptoms affecting the eyes, head, upper respiratory tract, and skin is associated with the physical properties of office buildings and costs UK businesses many millions of pounds through low productivity and sickness absence.1 This cluster has been labelled “sick building syndrome” (SBS).2 Although guidelines exist for the investigation and management of SBS,3,4 systematic research has failed to identify consistent associations between particular physical properties of buildings and SBS.5,6,7,8,9,10,11 There is increasing evidence that the psychosocial work environment is related to health12,13,14,15,16,17,18 and that the physical responses to work stress may resemble symptoms that have been attributed to the physical work environment.19 Work overload, lack of support at work, and conflict at work may exacerbate the effects of the physical work environment.20 The design of most existing studies has been such that workers report on problems with their physical work environment, levels of psychosocial work stress, and their perceived health and symptoms. Affect bias (the tendency to report consistently positively or negatively to questionnaire items because of mood) cannot be ruled out as an explanation for associations in such studies.
The Whitehall II study of British civil servants working in various London departments, offered an opportunity to investigate these alternative pathways. This study builds on existing literature by combining objective data on the physical work environment measured by independent field workers with individual reports of psychosocial stress at work and health. Additionally it uses a multilevel framework to consider the possible influence of the physical building environment at one level and individual work characteristics at another level, on workers' health. It avoids the bias that may have affected other studies where SBS is assumed to be a problem since neither participants nor investigators contemplated a study of SBS. Subsequent to collection of data on symptoms and the psychosocial work environment, physical characteristics of the buildings in which the study cohort were working at the time of the survey were measured.
The aim of this study is to examine whether building characteristics or psychosocial work characteristics best explain the rates of symptoms among men and women working in 44 different buildings in and around London.
Methods
The Whitehall II study
This project forms part of the Whitehall II study of civil service office workers, a longitudinal study of 10 308 male and female civil servants, aged 35–55 years at baseline. At the third phase of follow up (1991–93), participants completed a detailed questionnaire that included questions on sociodemographic characteristics, SBS symptoms, the physical nature of the workplace, and psychosocial work characteristics. Details are reported elsewhere.21 Appropriate ethical approval was obtained and all participants consented to take part in the study.
Definition of SBS
There is no single accepted definition of “sick building syndrome”. The term usually refers to higher than normal prevalence in a particular building of symptoms affecting the eyes, head, upper respiratory tract, and skin. Investigation of SBS has examined office buildings in many countries including the UK,2,22,23,24 Scandinavia,25 and North America.26,27,28,29,30 Studies vary in the symptom description and frequency and whether the symptoms reduce on leaving the building.31,32
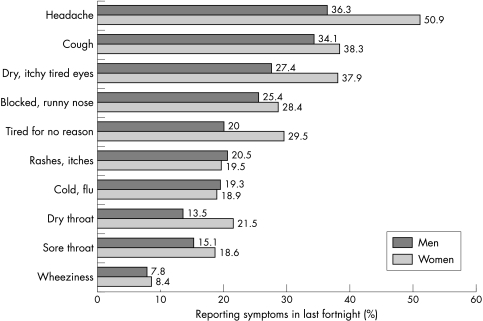
Ten potential SBS symptoms commonly reported in other investigations were included as part of a list of 22 symptoms (see fig 1). Respondents were asked “Have you had any of the following symptoms in the last 14 days?”. The symptoms have some validity as a health measure as they predict future sickness absence gathered from civil service records. Participants with four or more symptoms had an increased risk of sickness absence relative to those without symptoms (short spells: OR = 1.90, 95% CI 1.57 to 2.30; long spells: OR = 1.48, 95% CI 1.11 to 1.98). Psychological distress (a potential confounding factor predicting both reporting of symptoms and reporting of poor psychosocial environment), was measured by the 30‐item General Health Questionnaire.33
Figure 1 Presence of symptoms by sex in the Whitehall II study.
Physical work environment
A participant's physical work environment was assessed in three ways: environmental monitoring, a detailed inspection by three observers, and self‐reported questionnaire. Environmental monitoring was carried out in 29 buildings in which at least 20 participants were working. Access was granted in all buildings approached. In 18 of those buildings a more complete set of measurements was taken by the three observers. Choice of physical environmental exposures to be studied was based on existing studies of the indoor environment and health (reviewed by Burge, for example34). The study design is summarised in table 1. A sample of 10 workstations was selected in each building, stratified to include individual offices, small shared rooms, and open plan offices. Fieldwork and laboratory tests were validated by duplicate samples. Field measurements averaged from three daily readings were matched against the results from data loggers used across the whole day. The validity checks satisfied the team that the methods used to produce the data presented here adequately represented the more detailed pattern of environmental conditions captured by the data loggers.
Table 1 Description of Whitehall II participants and buildings studied.
| 44 buildings studied 4052 participants | |||
|---|---|---|---|
| 29 buildings where environmental monitoring took place | 15 buildings where no monitoring took place | ||
| 18 buildings where more detailed field work took place | 11 buildings where less detailed field work took place | 15 buildings | |
| 180 workstations | 109 workstations | ||
| 2523 participants | 792 participants | 737 participants | |
| Measured by questionnaire | |||
| How close is desk to window? | Y | Y | Y |
| How many people in room? | Y | Y | Y |
| Is room carpeted? | Y | Y | Y |
| Control over lights? | Y | Y | Y |
| Control over heating? | Y | Y | Y |
| Able to open and close windows? | Y | Y | Y |
| Measured by field workers | |||
| Air velocity | Y | Y | |
| CO2 | Y | Y | |
| Lighting level | Y | Y | |
| Radiant temperature | Y | Y | |
| Dry bulb temperature | Y | Y | |
| Relative humidity | Y | Y | |
| Noise level | Y | Y | |
| Airborne fungi | Y | ||
| Airborne bacteria | Y | ||
| Dustmites | Y | ||
| Inhalable dust | Y | ||
| Volatile organic compounds | Y | ||
| Mean (SD) symptom score | 2.50 (0.36) | 2.35 (0.29) | 2.10 (0.39) |
| Mean (SD) age in years | 49.2 (1.5) | 49.1 (1.1) | 49.4 (1.5) |
| % Top employment grades | 42.2 | 38.6 | 34.7 |
| % Bottom employment grades | 15.6 | 21.6 | 17.9 |
| % Male | 71.7 | 61.6 | 67.9 |
Participant's ability to adjust the temperature, adjust artificial light levels, and to open the window was captured by questionnaire. The number of people sharing the same office was also reported by participants. A combined measure of workstation control (ability to adjust heat, artificial light, to open the window, and fewer than 10 people in the room) was created. Respondent answers were validated on site and respondents in four buildings repeated part of the questionnaire to check the reliability of responses over time.
Psychosocial work environment
Decision latitude, job demands, and support at work were measured by self report questionnaire, based on the Karasek Job Content Instrument.35 Employment grade within the civil service was used as a measure of individual socioeconomic position. This is a potential confounding factor, because lower grades command lower salaries, which may lead to greater reporting of symptoms. Participants were categorised into three groups, namely administrative (top grades), professional/executive (middle grades), and clerical/support (lower grades). Other potential confounders, such as time taken to travel to work, problems with housing (such as damp, too small), and exposure to smoke at home and in the workplace were also measured.
Statistical analysis
A personal SBS symptom score was created for each respondent by summing the number of symptoms from the list of 10. Where a participant completed only nine items, the mean of available items was used instead. Participants who completed eight or fewer items were excluded from the analyses.
Investigation of the contribution of physical and psychosocial work environments on symptoms was complicated by the fact that varying numbers of observations were obtained for different characteristics. In particular, psychosocial data were available for more participants than were data on physical conditions. Rather than limiting this analysis to the smaller sample with complete observations for all characteristics, we chose to aggregate measures of physical characteristics up to the building level. Where the physical characteristic was measured at 10 sample workstations in a building, a mean was calculated for the building, weighted according to the proportion sampled in each office type (individual offices, small shared rooms, and open plan offices). Each building average provided information on the physical environment for all participants working in that building. Multilevel analysis36 was used to investigate the relations between physical environment in the building and an individual's psychosocial environment and their health. The standard errors are adjusted in multilevel models to allow for the possible non‐independence of observations from participants working in the same building.
Environmental variables were dichotomised according to exposure limits chosen on the basis of official guidance (from Building Services Research and Information Association and the International Standards Organisation) or on generally accepted standards (advised by Thomson MTS Ltd and two of the authors (AM and JE, qualified architects)). Building averages were classified according to whether they were within or outside acceptable limits.
In the first stage of analysis, associations between each exposure (physical environmental variable or psychosocial work characteristic) and reporting of symptoms was investigated, adjusting for age, sex, and grade of employment. The exposure was included in the full model if univariate analyses indicated a difference in the hypothesised direction (for example if symptom scores were higher for buildings averages outside acceptable limits).
Results
Symptom prevalence
The prevalence of the 10 SBS symptoms is shown in figure 1. The mean symptom score was 2.2 for men and 2.7 for women (t test p<0.001) and was lower for older participants (2.5 for 39–44 year olds, 2.4 for 45–49 year olds, 2.2 for 50–54 year olds, and 2.1 for 55–62 year olds, ANOVA p<0.001). Twenty five per cent of men and 15% of women reported no symptoms; 14% of men and 19% of women reported five or more. The mean number of symptoms reported varied by building from 1.2 in the buildings with the fewest symptoms to 3.2 in the buildings with the most symptoms. Table 1 shows the symptom scores and age, sex, and employment grade distribution of participants in buildings grouped by level of assessment. There were no significant differences in SBS scores between participants in the 18 buildings in which the most detailed environmental measures were collected and those in other buildings (p = 0.4). Neither did participants in the 18 buildings with detailed assessment differ in age (p = 0.6), employment grade (p = 0.3), or sex (p = 0.4) from participants in buildings with less detailed assessment (table 1).
Physical environmental characteristics of the workstation
Physical characteristics were investigated for the subset of participants who had data on the physical environment (table 2). None of the characteristics investigated was significantly associated with symptoms. There was a suggestion that high symptom scores were associated with temperature outside the recommended range, poor relative humidity (either too damp or too dry), airborne bacteria, and the presence of inhalable dust. Unexpectedly, lower symptom scores were found in buildings with unacceptable levels of air movement, carbon dioxide, noise, airborne fungi, and volatile organic compounds, although these differences were not statistically significant.
Table 2 Symptom reporting by physical characteristics of buildings.
| Exposure based on field work data | Acceptable limits | Number of buildings with average inside/outside limits | Mean (SE) difference in symptom score for buildings' outside/inside limits* | Test of significance for mean difference in symptom score* |
|---|---|---|---|---|
| Based on 3315 participants in buildings with full/partial assessment | ||||
| Air velocity | 0.05–0.15 m/s | 9/20 | −0.03 (0.13) | p = 0.8 |
| CO2 | ⩽500 ppm | 25/4 | −0.22 (0.16) | p = 0.2 |
| Lighting level | 250–1000lux | 29/0 | All within limits | |
| Radiant temperature | 19–22°C | 8/21 | −0.02 (0.13) | p = 0.9 |
| Dry bulb temperature | 19–24°C | 23/6 | 0.16 (0.15) | p = 0.3 |
| Relative humidity | 35–65% | 22/7 | 0.09 (0.14) | p = 0.5 |
| Noise level | ⩽55Dba | 26/3 | −0.24 (0.18) | p = 0.2 |
| Based on 2523 participants in fully assessed buildings | ||||
| Airborne fungi | ⩽500 cfu/m3 | 13/5 | −0.10 (0.14) | p = 0.5 |
| Airborne bacteria | ⩽1000 cfu/m3 | 12/6 | 0.09 (0.14) | p = 0.5 |
| Inhalable dust | ⩽0.10 mg/m3 | 12/6 | 0.08 (0.14) | p = 0.6 |
| Volatile organic compounds | ⩽0.3 mg/m3 | 10/8 | −0.10 (0.13) | p = 0.4 |
| Exposure based on questionnaire data | Acceptable limits | Number of participants | Mean (SE) symptom score for participants in each category* | |
| Control over workstation | 0 (no control) | 116 | 2.67 (0.19) | p = 0.1 |
| 1 | 328 | 2.30 (0.12) | ||
| 2 | 955 | 2.30 (0.07) | ||
| 3 | 1103 | 2.20 (0.06) | ||
| 4 (most control) | 1550 | 2.34 (0.05) | ||
*Estimates are adjusted for age, sex, and employment grade using a regression model.
Based on questionnaire data, workstation control was found to be inversely related to symptoms—that is, the more control people have the fewer symptoms they report (table 2).
Ventilation systems
Overall, air conditioning was found to be associated with slightly higher symptom scores compared with other ventilation systems (table 3). Our results are consistent with previous findings,37,38 namely that fewest symptoms are associated with mechanical ventilation, followed by all air and natural ventilation, then air conditioning systems although differences across the types of ventilation system were not statistically significant. The results are clearer when the seasonal effect is removed by examining a subset of four symptoms that are constant throughout the year (headache, tired for no reason, rashes/itches and dry throat; data not shown).
Table 3 Symptom reporting by ventilation system.
| Ventilation system | Number of buildings | Mean (SE) symptom score in the building* |
|---|---|---|
| Mechanical ventilation | 2 | 1.74 (0.26) |
| Natural ventilation | 23 | 2.12 (0.09) |
| All air system | 10 | 2.07 (0.11) |
| Central induction | 6 | 2.21 (0.09) |
| Local induction | 3 | 2.20 (0.24) |
| p = 0.8 |
*Estimates are adjusted for age, sex, and employment grade using a regression model.
Psychosocial work characteristics
High job demands and low support at work were associated with higher mean symptom scores after adjusting for age, sex, and grade (table 4, model 1). Symptom levels tended to be higher for participants with low decision latitude although this association was not statistically significant.
Table 4 Relation between symptom reporting and physical and psychosocial environment: mutually adjusted models.
| Model 1: Adjusted for sex, age, and grade and all work characteristics listed in table | Model 2: Adjusted for sex, age, and grade and all physical characteristics listed in table | Model 3: Physical and work characteristics included together | Model 4: Model 3 + GHQ | |
|---|---|---|---|---|
| Work characteristics | ||||
| Job demands tertile | ||||
| Middle | 0.13 (0.12) | 0.12 (0.12) | 0.04 (0.12) | |
| High | 0.45 (0.13)** | 0.44 (0.13)** | 0.26 (0.13)* | |
| Decision latitude tertile | ||||
| Low | 0.11 (0.12) | 0.10 (0.12) | 0.07 (0.10) | |
| Middle | 0.12 (0.12) | 0.12 (0.10) | 0.04 (0.12) | |
| Support tertile | ||||
| Low | 0.43 (0.11)** | 0.43 (0.11)** | 0.31 (0.10)** | |
| Middle | 0.19 (0.10) | 0.19 (0.10) | 0.15 (0.10) | |
| Physical characteristics | ||||
| Dry bulb temperature 19–24°C v (<19°C or >24°C) | 0.15 (0.17) | 0.11 (0.17) | 0.12 (0.15) | |
| Relative humidity <35% or >65% (v 35–65%) | 0.07 (0.16) | 0.03 (0.16) | −0.01 (0.14) | |
| Airborne bacteria >1000 cfu/m3 (v ⩽1000 cfu/m3) | 0.10 (0.16) | 0.08 (0.15) | 0.11 (0.14) | |
| Inhalable dust >0.1 mg/m3 (⩽0.1 mg/m3) | −0.03 (0.18) | −0.03 (0.18) | −0.02 (0.16) | |
| Control over workstation: no control (v some control) | 0.55 (0.23)* | 0.50 (0.23)* | 0.47 (0.22)* |
Values are difference in mean symptom score from reference group for 2523 participants with complete data.
*p<0.05; **p<0.01.
Full model incorporating psychosocial and physical environmental characteristics
The associations between the psychosocial work stress scales and symptoms were unchanged on inclusion of physical environmental characteristics (table 4, model 3) and attenuated somewhat on inclusion of GHQ scores, indicating that some of the association between work characteristics and symptoms was due to negative affect (table 4, model 4). Those with no control over the workstation had higher symptom scores, even after adjustment for age, sex, employment grade, and other physical characteristics (table 4, model 2). Adjustments for work characteristics and GHQ score did not substantially alter this association (models 3 and 4). These results were essentially unchanged when adjustment was made for time taken to travel to work, exposure to smoking in the workplace or in the home, and problems with housing (data not shown). For participants who experienced low decision latitude, high job demands, or low support at work there was no evidence that physical environmental factors were more strongly related to symptoms than the psychosocial variables.
Discussion
These results emphasise the potentially confounding effects of age, sex, socioeconomic position, and psychosocial aspects of work in explaining the prevalence of symptoms. They suggest that “sick building syndrome” may be wrongly named—raised symptom reporting appears to be due less to poor physical conditions than to a working environment characterised by poor psychosocial conditions. A model incorporating physical and psychosocial hazards in the work environment and health has been proposed39 and more recently the interplay between the indoor environment and characteristics of the building's occupants has been recognised.40,41 Control over work, job demands and work overload, job category, social stressors, mental stress at work, and personality traits have all been related to a similar set of symptoms16,18,40,42,43,44,45,46,47,48,49,50 and a study in Africa also found that psychosocial factors were more important than physical exposures.51 Our findings suggest that, in this sample of office based workers, physical attributes of buildings have a small influence on symptoms.
The effects of control over the physical environment and control over work have rarely been investigated simultaneously. Our findings demonstrate that both are associated with higher symptom prevalence. Other studies have suggested that the ability to control one's environment is important and our findings confirm that, even when recommended levels are achieved, employees' ability to control light levels and temperature is associated with fewer symptoms.42,52
An important aspect of the study design was that objective measures of the physical environment were obtained by independent field workers. Many studies have obtained information on the physical office environment by questionnaire. As the same set of respondents report on perceptions of their environment and their health, this could induce spurious associations. The Whitehall II study has the additional advantage of covering a number of buildings and a large sample of respondents who have answered a wide range of questions, including potential confounding factors. Almost every study of SBS reports that women record more symptoms than men and younger people report more symptoms than older people34,50,53 but not all control for these differences. Furthermore, participants and buildings were not selected on the basis of explicit concern with sick building symptoms and responses did not arise from leading questions about whether symptoms were building related. The methods used in this paper differ from previous studies in other ways. An enquiry into questionnaires on SBS indicated that responses alter according to the list of symptoms and the format in which they are asked, and called for standard questions to be used in further studies.31,32 The phrasing of our questions on symptoms has a shorter length of recall, assisting accuracy of response. The techniques used to model the hierarchical structure of the data have not previously been used in studies investigating SBS. Future studies of SBS should ask for recent recall of symptoms, avoid leading questions, and adjust for age, sex, and socioeconomic position.
The lack of association between symptoms and the physical environment could be because the quality of Whitehall buildings is above a threshold for affecting symptoms. If this is the case then claims that SBS affects most buildings and most office workers and causes great financial losses are unfounded, and the search for the cause of SBS is less important in terms of public health. If it is not the case, then it is important to study typical conditions in places representative of most office buildings. This study contains a sample of buildings selected as housing people already participating in a health study rather than ones where SBS was suspected and is therefore more useful in studying the public health implications of the physical environment at work.
Average readings over 10 workstations were used to describe the environmental characteristics for each building. This introduces the potential for misclassification and, although this is common practice in studies of building environment and health, it would have strengthened the study if more workstations had been sampled. It should be noted that building characteristics are measured less precisely than psychosocial characteristics. Hodgson also notes that our relative lack of knowledge about specific physical exposures and how best to measure them may be an explanation for the finding that work stress seems to be strongly related to symptoms.17 However, the lack of association between the physical environment and symptoms was consistent across all the analyses performed. Other studies have found similar lack of association between measured contaminants and symptoms.46 The self‐reported nature of the psychosocial work characteristics and symptoms is a potential limitation. A tendency to report always positively (or negatively) may be driving the associations seen here. However, adjustment for GHQ (an indicator of positive or negative affect) was made in our study and some associations between work characteristics and symptom reporting remained.
Questionnaire and fieldwork data were collected at different times of the year. Season affects some measures of the physical environment within buildings and may bias the results. A total of 26 buildings were assessed in the season when central heating is typically in use and 18 buildings were assessed in the non‐heating season. Symptom scores were 0.2 higher in buildings which were assessed in the central heating season compared with those assessed in the non‐heating season (p = 0.09 adjusting for age and sex). Analyses were repeated using a subset of four symptoms that are invariant across the year. The same pattern of findings was found and the conclusions remain unchanged using seasonally invariant symptoms.
These findings should not be interpreted as justification for assuming that the quality of the physical environment of the workplace is unimportant. Comfort and perceived satisfaction with environmental conditions within buildings should not be ignored. Compared to current standards, the results showed that some features are generally acceptable (carbon dioxide, lighting levels, and noise) but that many workstations were too hot, with too little air movement. These conditions can and should be improved even if health outcomes are unchanged.
In this study, the physical environment of workstations and office buildings appears to have less effect on symptom prevalence than features of the psychosocial environment. SBS symptoms are more about the jobs people do, their psychosocial environment, and their ability to control conditions in their office than about the physical environment of the building or workstation where the job is performed. The results imply that if SBS is reported in a building, management should consider causes beyond the physical design and operation of the workplace and should widen their investigation to include the organisation of work roles and the autonomy of the workforce.
Main messages
The physical environment of workstations and office buildings had less effect on symptoms than features of the psychosocial work environment.
Having some control over the local workstation was related to lower reporting of symptoms.
“Sick building syndrome” may be a misnomer—raised symptom levels appear to be largely due to a working environment characterised by poor psychosocial conditions.
Policy implications
Management should consider causes beyond the physical design and operation of the workplace in places where “sick building syndrome” is reported. Investigation of the organisation of work roles and the autonomy of the workforce should be undertaken.
Acknowledgements
The Whitehall II study has been supported by grants from the Medical Research Council; British Heart Foundation; Health and Safety Executive; Department of Health; US, NIH: National Heart Lung and Blood Institute (RO1‐HL36310); US, NIH: National Institute on Aging (RO1‐AG13196); US, NIH: Agency for Health Care Policy Research (RO1‐HS06516); and the John D and Catherine T MacArthur Foundation Research Networks on Successful Midlife Development and Socio‐economic Status and Health. MM is supported by an MRC Research Professorship.
We thank all participating civil service departments and their welfare, personnel, and establishment officers; the Occupational Health and Safety Agency; the Council of Civil Service Unions; all participating civil servants in the Whitehall II study; and all members of the Whitehall II study team.
Footnotes
Competing interests: none.
References
- 1.House of Commons Environment Committee Sixth report: indoor pollution. London: Her Majesty's Stationery Office, 1988
- 2.Burge S, Hedge A, Wilson S.et al Sick building syndrome: a study of 4373 office workers. Ann Occup Hyg 198731493–504. [DOI] [PubMed] [Google Scholar]
- 3.Health and Safety Executive How to deal with Sick Building Syndrome. Guidance for employers, building owners and building managers. London: HMSO, 1995
- 4.Tearle P. The sick building syndrome. Comm Dis Public Health 19992303–304. [PubMed] [Google Scholar]
- 5.Appleby P H. ABC of work related disorders. Building related illnesses. BMJ 1996313674–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bourbeau J, Brisson C, Allaire S. Prevalence of the sick building syndrome symptoms in office workers before and six months and three years after being exposed to a building with an improved ventilation system. Occup Environ Med 19975449–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jaakkola M S, Jaakkola J J. Office equipment and supplies: a modern occupational health concern? Am J Epidemiol 19991501223–1228. [DOI] [PubMed] [Google Scholar]
- 8.Sykes J M. Sick building syndrome: a review. London: Health and Safety Executive, 1988
- 9.Leinster P, Mitchell E.A review of indoor air quality and its impact on the health and well‐being of office workers. Commission of the European Communities Luxembourg 1992
- 10.Raw G J.Sick building syndrome: a review of the evidence on causes and solutions. London: HMSO, 1992, (HSE Contract research report No 42 )
- 11.Menzies R, Tamblyn R, Farant J ‐ P.et al The effect of varying levels of outdoor air supply on the symptoms of sick building syndrome. N Engl J Med 1993328821–827. [DOI] [PubMed] [Google Scholar]
- 12.Bosma H, Stansfeld S A, Marmot M G. Job control, personal characteristics, and heart disease. J Occup Health Psychol 19983402–409. [DOI] [PubMed] [Google Scholar]
- 13.Marmot M G, Bosma H, Hemingway H.et al Contribution of job control and other risk factors to social variations in coronary heart disease incidence. Lancet 1997350235–239. [DOI] [PubMed] [Google Scholar]
- 14.Kuper H, Marmot M. Job strain, job demands, decision latitude, and risk of coronary heart disease within the Whitehall II study. J Epidemiol Community Health 200357147–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ooi P L, Goh K T. Sick building syndrome: an emerging stress‐related disorder? Int J Epidemiol 1997261243–1249. [DOI] [PubMed] [Google Scholar]
- 16.Crawford J O, Bolas S M. Sick building syndrome, work factors and occupational stress. Scand J Work Environ Health 199622243–250. [DOI] [PubMed] [Google Scholar]
- 17.Hodgson M. Indoor environmental exposures and symptoms. Environ Health Perspect 2002110663–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mizoue T, Reijula K, Andersson K. Environmental tobacco smoke exposure and overtime work as risk factors for sick building syndrome in Japan. Am J Epidemiol 2001154803–808. [DOI] [PubMed] [Google Scholar]
- 19.Lahtinen M, Sundman‐Digert C, Reijula K. Psychosocial work environment and indoor air problems: a questionnaire as a means of problem diagnosis. Occup Environ Med 200461143–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lahtinen M, Huuhtanen P, Reijula K. Sick building syndrome and psychosocial factors—a review of literature. Indoor Air 1998432–39. [Google Scholar]
- 21.Marmot M G, Smith G D, Stansfeld S.et al Health inequalities among British civil servants: the Whitehall II study. Lancet 19913371387–1393. [DOI] [PubMed] [Google Scholar]
- 22.Jones P J, Vaughan N D, Grajewski T.et al Internal conditions and the response of office workers. Proceedings of the Workplace Comfort Forum. London, March 1995
- 23.Finnegan M J, Pickering C A C, Burge P S. The sick building syndrome: prevalence studies. BMJ 19842891573–1575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wilson S, Hedge A.The office environment survey: a study of building sickness. Building Use Studies Ltd 1987
- 25.Jaakkola J J K, Miettinen P, Tuomaala P.et al The Helsinki office environment study: the type of ventilation system and the sick building syndrome in Proceedings of Indoor Air 19931285–289. [Google Scholar]
- 26.National Institute for Occupational Safety and Health, US Environmental Protection Agency Indoor air quality and work environment study. NIOSH, July 1990
- 27.National Institute for Occupational Safety and Health, US Environmental Protection Agency Indoor air quality and work environment study. NIOSH, Jan 1991
- 28.Tamblyn R M, Menzies R I, Tamblyn R T.et al The feasibility of using a double blind experimental cross‐over design to study interventions for sick building syndrome. J Clin Epidemiol 199245603–612. [DOI] [PubMed] [Google Scholar]
- 29.Fisk W J, Mendell M J, Daisey J M.et al The California healthy building study Phase 1: A summary in Proceedings of Indoor Air 19931279–284. [Google Scholar]
- 30.Middaugh D A, Pinney S M, Linz D H. Sick building syndrome. Medical evaluation of two work forces. J Occup Med 1992341197–1203. [PubMed] [Google Scholar]
- 31.Raw G J, Roys M S, Tong D. Questionnaire design for sick building syndrome, Part II: The effect of symptom list and frequency scale. Healthy Buildings 19941481–486. [Google Scholar]
- 32.Roys M S, Raw G J, Whitehead C. Questionnaire design for sick building syndrome, Part I: Tables vs separate symptom questions and method of determining building‐relatedness. Healthy Buildings 19943183–188. [Google Scholar]
- 33.Goldberg D P.The detection of psychiatric illness by questionnaire: A technique for the identification and assessment of non‐psychotic psychiatric illness. New York: OUP, 1972
- 34.Burge P S. Sick building syndrome. Occup Environ Med 200461185–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Karasek R, Theorell T.Healthy work, stress, productivity and the reconstruction of working life. New York: Basic Books, 1990
- 36.Goldstein H.Multilevel statistical models. London: Edward Arnold, 1995
- 37.Mendell M J, Smith A H. Consistent pattern of elevated symptoms in air‐conditioned office buildings: a re‐analysis of epidemiologic studies. Am J Public Health 1990801193–1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Seppanen O, Fisk W J. Association of ventilation system type with SBS symptoms in office workers. Indoor Air 20021298–112. [DOI] [PubMed] [Google Scholar]
- 39.Cox T, Ferguson E. Measurement of the subjective environment. Work Stress 1994898–109. [Google Scholar]
- 40.Thorn A. The sick building syndrome: a diagnostic dilemma. Soc Sci Med 1998471307–1312. [DOI] [PubMed] [Google Scholar]
- 41.Bass B, Economou V, Lee C K.et al The interaction between physical and social‐psychological factors in indoor environmental health. Environ Monit Asses 200385199–219. [DOI] [PubMed] [Google Scholar]
- 42.Raw G J, Roys M S, Leaman A. Sick building syndrome, productivity and control. Property Journal, August 1993
- 43.Skov P, Valbjorn O, Pedersen B V. Influence of personal characteristics, job related factors and psychosocial factors on the sick building syndrome. Scand J Work Environ Health 198915286–295. [DOI] [PubMed] [Google Scholar]
- 44.Stenberg B, Eriksson N, Hoog J.et al The sick building syndrome (SBS) in office workers. A case‐referent study of personal, psychosocial and building‐related risk indicators. Int J Epidemiology 1994231190–1197. [DOI] [PubMed] [Google Scholar]
- 45.Stolwijk J A J. Sick building syndrome. Environ Health Perspect 19919599–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nelson N A, Kaufman J D, Burt J.et al Health symptoms and the work environment in four nonproblem United States office buildings. Scand J Work Environ Health 19952151–59. [DOI] [PubMed] [Google Scholar]
- 47.Spurgeon A, Gompertz D, Harrington J M. Non‐specific symptoms in response to hazard exposure in the workplace. J Psychosom Res 19974343–49. [DOI] [PubMed] [Google Scholar]
- 48.Ford C V. Somatization and fashionable diagnoses: illness as a way of life. Scand J Work Environ Health 199723(Suppl 3)7–16. [PubMed] [Google Scholar]
- 49.Norback D, Edling C. Environmental, occupational, and personal factors related to the prevalence of sick building syndrome in the general population. Br J Ind Med 199148451–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Runeson R, Norback D, Stattin H. Symptoms and sense of coherence—a follow‐up study of personnel from workplace buildings with indoor air problems. Int Arch Occup Environ Health 20037629–38. [DOI] [PubMed] [Google Scholar]
- 51.Bachmann M O, Myers J E. Influences on sick building syndrome symptoms in three buildings. Soc Sci Med 199540245–251. [DOI] [PubMed] [Google Scholar]
- 52.Bordass W, Leaman A, Willis S. Control strategies for building services: the role of the user. BRE conference Buildings and the environment, May 1994
- 53.Brasche S, Bullinger M, Morfeld M.et al Why do women suffer from sick building syndrome more often than men? Subjective higher sensitivity versus objective causes. Indoor Air 200111217–222. [DOI] [PubMed] [Google Scholar]