Abstract
Objectives
Functional capacity evaluations (FCEs) are commonly used to determine return‐to‐work readiness and guide decision making following work related injury, yet little is known of their validity. The authors examined performance on the Isernhagen Work Systems' FCE as a predictor of timely and sustained recovery in workers' compensation claimants with upper extremity disorders. A secondary objective was to determine whether FCE is more predictive in claimants with specific injuries (that is, fracture) as compared to less specific, pain mediated disorders (that is, myofascial pain).
Methods
The authors performed a longitudinal study of 336 claimants with upper extremity disorders undergoing FCE. FCE indicators were maximum performance during handgrip and lift testing, and the number of tasks where performance was rated below required job demands. Outcomes investigated were days receiving time‐loss benefits (a surrogate of return to work or work readiness) in the year following FCE, days until claim closure, and future recurrence defined as whether benefits restarted, the claim reopened, or a new upper extremity claim was filed. Cox and logistic regression were used to determine the prognostic effect of FCE crudely and after controlling for potential confounders. Analysis was performed separately on claimants with specific and pain mediated disorders.
Results
Most subjects (95%) experienced time‐loss benefit suspension within one year following FCE. The one year recurrence rate was 39%. Higher lifting performance was associated with faster benefit suspension and claim closure, but explained little variation in these outcomes (r2 = 1.2–11%). No FCE indicators were associated with future recurrence after controlling for confounders. Results were similar between specific injury and less specific groups.
Conclusions
Better FCE performance was a weak predictor of faster benefit suspension, and was unrelated to sustained recovery. FCE was no more predictive in claimants with specific pathology and injury than in those with more ambiguous, pain mediated conditions.
Keywords: work capacity evaluation, arm injuries, recurrence, validity and reliability, disability insurance
Upper extremity musculoskeletal disorders, including pain mediated conditions such as lateral epicondylitis and myofascial shoulder pain, have become some of the most burdensome and costly compensable conditions and leading causes of disability among working age adults.1,2 Determining a worker's readiness or safe ability to return to work following injury remains a major challenge for clinicians and claims adjudicators. One clinical tool used internationally for purposes of predicting safe ability to return to work following upper extremity injury is functional capacity evaluation (FCE).3 FCEs are standardised batteries of tests in which a patient's functional ability is determined and compared to required physical job demands, with return to work recommended when abilities equal or exceed required demands.4 FCEs theoretically provide an indication of physical and functional recovery following injury; however, whether FCE performance is associated with future return to work has not been studied in subjects with upper extremity disorders.5
In conjunction with the Alberta Workers' Compensation Board (WCB‐Alberta), our research group has studied the prognostic value of the Isernhagen Work Systems' (Duluth, MN) FCE when administered on workers with low back pain.6,7 Results indicate that the FCE is a modest predictor of timely return to work and a poor predictor of sustained recovery in our sample, made largely of claimants with non‐specific back pain. Whether these results generalise to other conditions, such as those of the upper extremity, is unknown. Also, given the Isernhagen FCE's focus on physiological and biomechanical observation of strength and physical performance, it is possible this tool is more predictive in claimants with specific injuries such as fracture, dislocation, or amputation as compared to primarily pain mediated disability conditions such as low back pain. Reneman et al have reported that maximal ability and effort level can be determined validly by clinicians trained in the Isernhagen method through observation of subjects' physical response to testing.8 However, in non‐specific conditions such as back pain, pain complaints as opposed to physical injury or impairment are typically the most important predictors of recovery.9,10
In workers with specific injuries, physical impairments such as muscle weakness or reduced joint mobility may present as major barriers to return to work that are identifiable during FCE testing.11 For example, a worker with permanently reduced shoulder flexion range of motion following traumatic gleno‐humeral joint dislocation may be unable to perform work duties involving heavy overhead lifting. It is possible that FCE could identify this functional impairment and barrier to performing regular work duties. Evaluation of this hypothesis was not possible in our previous study of claimants with low back pain due to the very small number of claimants undergoing FCE following spinal fracture or dislocation (<5% of our sample). A higher frequency of specific conditions is observed in the upper extremity.
The primary objective of the current study was to determine the prognostic value of the Isernhagen FCE in claimants with upper extremity disorders. A secondary objective was determining whether FCE is more predictive in claimants with clearly identifiable injury such as upper extremity fracture, dislocation, or amputation compared to those with pain mediated conditions with less well defined trauma and pathology, such as repetitive strain injury or myofascial pain syndrome. We hypothesised that better performance on FCE would be associated with faster initial return to work and lower likelihood of recurrence and that FCE would have higher predictive value in claimants with specific injuries.
Methods
Design
A longitudinal cohort design was used.
Subjects
The study cohort included workers' compensation claimants receiving time loss benefits for upper extremity disorders undergoing FCE at the major WCB‐Alberta outpatient rehabilitation facility between 1 January 2000 and 31 March 2002. The main diagnosis was coded according to the International Classification of Diseases, Ninth Revision (ICD‐9) at time of admission to Millard Health and used to identify claimants with upper extremity disorders. Each subject's diagnosis was identified using ICD‐9 coding and verified through medical file review.
Specific inclusion criteria included: compensated injuries with diagnostic codes indicative of injury to the upper extremity; FCE conducted at least six weeks after the date of accident; and no further medical investigations or treatment recommended. Claimants undergoing FCE within the Alberta workers' compensation environment are usually those who have met or surpassed expected injury healing times and have plateaued with medical and rehabilitative interventions, yet report ongoing difficulties related to their compensable condition. Such claimants are evaluated with FCE for purposes of determining fitness to return‐to‐work and administrative decisions are made, in part, based on results. We excluded claimants with explicit physical restrictions at time of FCE testing, such as those being managed with stringent post‐surgical protocols.
Of the 394 claimants meeting inclusion criteria, 336 (85%) had complete data and were included in subsequent analyses. Subjects with missing data were more likely to be female (43% v 29%), younger (45 v 48 years), and perform worse on FCE (7 v 5 failed tasks) but were similar on the other 13 factors listed in table 1. Subjects were predominantly employed males reporting moderate levels of pain and disability. Only 12 subjects in the entire cohort (4%) were rated as meeting or exceeding job requirements on all FCE tasks.
Table 2 Items in the Isernhagen work systems' upper extremity functional capacity evaluation.
| Floor‐to‐waist lift | Sustained elevated work |
| Waist‐to‐overhead lift | Crawling |
| Horizontal lift | Ladder climbing |
| Isometric/dynamic pushing | Right hand coordination |
| Isometric/dynamic pulling | Left hand coordination |
| Right hand carrying | Right hand dynamometric grip strength |
| Left hand carrying | Left hand dynamometric grip strength |
| Front carrying |
Subjects were classified according to the nature of their diagnosis with clearly identifiable injuries (that is, fractures, dislocations, amputations, tendon ruptures, burns, etc) categorised as “specific” injuries and more pain mediated disability conditions (that is, non‐specific upper extremity pain, myofascial pain, sprain/strain, etc) categorised as “less specific” injuries. 185 subjects were categorised into the specific group and 151 were classified as less specific. Dramatic statistically significant differences were observed between these groups, as displayed in table 1. Subjects classified as having specific diagnoses were more likely to be males (84% v 55%) with unilateral injuries (96% v 80%), more prior upper extremity injury claims (2.4 v 1.9), more previous health care (65 v 41 health visits), longer durations of injury (611 v 292 days), and not have jobs to return to (44% unemployed v 23%). Those with specific injuries also performed worse on FCE (eight v six failed tasks) and were more likely rated “fit to work” (61% v 49%); however no significant differences were seen between the groups on any recovery outcome.
Measures
Data on variables of interest were extracted from clinical and administrative databases of the WCB‐Alberta and were merged using a common unique identifier. Claimants undergoing FCE at the rehabilitation facility sign informed consent forms enabling data release for programme evaluation or research purposes. The University of Alberta's Health Research Ethics Board approved the study.
Functional capacity evaluation
The Isernhagen Work Systems' FCE protocol is used at the WCB‐Alberta rehabilitation facility. During this FCE, the administering clinician relies on observation of biomechanical and physiological signs of effort to determine safe, maximum performance levels. The protocol includes activities representing the physical demands of work outlined in the Dictionary of occupational titles, such as gripping, lifting, carrying, pushing, pulling, and other tasks.12 When used on individuals with upper extremity injuries, the protocol is limited to those tasks that require use of the upper extremity (see table 2). Acceptable interrater and test‐retest reliability have been reported for the handgrip and hand coordination tasks in the protocol and for determinations of maximum performance on the lifting and carrying tasks when used on subjects with back pain.13,14,15,16,17
Table 1 Subject characteristics.
| Entire sample | Specific Injury | Less specific Injury | |
|---|---|---|---|
| (n = 336) | (n = 185) | (n = 151) | |
| Mean (SD) or % | |||
| Age (years) | 45 (11.2) | 45 (12.1) | 44 (9.9) |
| Days between injury and admission* | 468 (720) | 611† (897) | 292† (335) |
| Functional capacity evaluation* (out of 15) | 7.1 (3.2) | 7.6 (3.3) | 6.4 (3.1) |
| Waist‐to‐overhead lift (kg) | 10.1 (6.8) | 10.1 (7.2) | 10.0 (6.2) |
| % Pain Disability Index | 46.6 (20.5) | 46.6 (21.6) | 46.6 (19.1) |
| Pain visual analogue scale (out of 10) | 4.9 (2.3) | 4.7 (2.4) | 5.1 (2.1) |
| Previous WCB upper extremity claims* | 2.1 (2.1) | 2.4 (2.1) | 1.9 (2.1) |
| Number of previous health visits* | 54 (48.7) | 65 (55.2) | 41 (35.1) |
| Gross annual salary ($ thousands) | 35.0 (19.6) | 36 (21.7) | 33 (16.6) |
| Male* | 71 | 84 | 55 |
| Right hand dominant | 92 | 90 | 95 |
| Side of injury* | |||
| Right | 53 | 51 | 56 |
| Left | 35 | 45 | 24 |
| Bilateral | 11 | 4 | 21 |
| Employed* | 66 | 56 | 77 |
| English primary language | 92 | 93 | 91 |
| Physical job demands | |||
| Limited (<5 kg) | 8 | 8 | 9 |
| Light (5–9 kg) | 22 | 21 | 24 |
| Medium (10–20 kg) | 41 | 38 | 44 |
| Heavy (>20 kg) | 29 | 33 | 23 |
| FCE clinician recommended fit to work* | 55 | 61 | 49 |
*Statistically significant difference between specific and less specific groups (p<0.05).
†Median 307.
‡Median 160.
Front carrying
At the rehabilitation facility, claimant performance on the 15 activities in the upper extremity FCE protocol is compared to required physical job demands for related work tasks. Physical job demands are determined through employer report and direct work site measurement or, when these are unavailable, worker self‐report with a standardised questionnaire. After FCE testing, each item in the protocol is given either a pass or fail rating depending on whether or not the subject's functional performance matched or exceeded required job demand levels. For example, a claimant would be rated as failing the waist‐to‐overhead lift if he/she demonstrated the ability to lift 10 kg overhead yet required the ability to lift 25 kg in a labourer job.
We used the total number of tasks rated as failed by the administering clinician and performance on the floor‐to‐waist lift task as indicators of FCE performance, as these measures have previously been found associated with return‐to‐work outcomes in subjects off work due to low back pain or reported functional limitation.6,18 Additionally, maximum performance on the dynamometric right and left handgrip tests and the horizontal and waist‐to‐overhead lifting tests were also available and used as FCE performance indicators.
Potential confounding variables
Other variables were extracted for analysis based on their potential for a confounding influence on the relation between FCE and outcomes. We selected variables from the administrative databases that have been reported as predictive of recovery in previously published studies of claimants with upper extremity disorders19,20,21 or where a sound theoretical rationale existed for considering the variable. Variables extracted included gender; age; employment status; days from injury to FCE; scores on self‐report pain and disability questionnaires including the Pain Disability Index (a reliable and valid measure of self‐reported disability)22,23 and a pain visual analogue scale completed by subjects at time of FCE, clinician return‐to‐work recommendation made immediately following FCE; physical job demands rating from the Human Resources Development Canada's National Occupational Classification;24 pre‐injury annual salary; number of healthcare visits (medical, physical therapy, and chiropractic visits) preceding the FCE for the compensable condition; total number of previous WCB claims; and number of previous WCB upper extremity injury claims.
Outcomes
Our goal was to examine indicators of timely and sustained recovery following FCE. Days until suspension of time‐loss benefits and claim closure following FCE served as surrogate indicators of timely return to work (or readiness to return to work) and recovery. These outcomes are often used as recovery indicators within compensation contexts,25,26 however, they may underestimate the true duration of disability.27,28 Therefore, we also examined the rate of recurrence in subjects experiencing benefit suspension or claim closure (defined as whether time‐loss benefits resumed, the claim was reopened, or a new upper extremity injury claim was filed).
Analysis
Descriptive statistics were calculated including Kaplan‐Meier curves for time receiving time‐loss benefits and until claim closure. Ongoing benefit reception and open claims were censored at one year. Significant differences between subjects with specific versus less specific injuries were determined using χ2, log rank, and t tests. A 0.05 alpha level was chosen to judge significance.
To determine relationships between FCE and days to suspension of time‐loss benefits and claim closure, Cox regression was used.29 Initially, a univariate screen of the relation between all predictor variables and outcomes was performed. The adjusted effect of the FCE indicators was then determined by entering them into multivariable Cox regression models along with the potential confounding measures found significant in the univariate screen. Tests of confounding were also undertaken to determine if any other predictor variable altered regression coefficients by more than 20%.30 These analyses were performed for each FCE variable separately. The partial and marginal amount of variation explained by the FCE variables was calculated using the technique described by Schemper.31 The unique contribution to prediction of the individual FCE lift and handgrip variables was also determined by entering each simultaneously into a multivariable regression model. Logistic regression was used to evaluate the relation between FCE and future recurrence.32 The normality, linearity, and proportional hazard assumptions were evaluated.
To test our hypothesis that FCE is more predictive in claimants with specific pathology or injury, analyses were performed separately for subjects in the specific and less specific groups. This stratification of the sample according to nature of diagnosis also enabled a confirmation of the prognostic value of the FCE indicators. Point estimates and 95% confidence intervals were determined. Calculations were performed using the computer application SPSS (Chicago, IL, USA).
Results
Characteristics
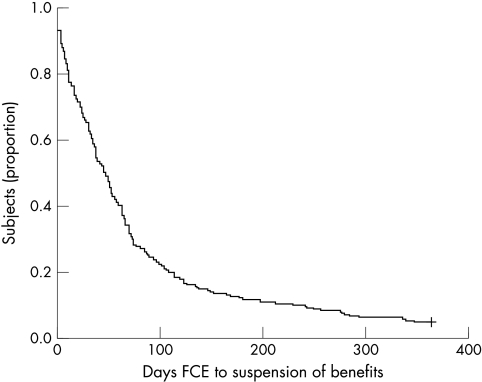
The median time between FCE and time‐loss benefit suspension was 47 days and only 17 (5%) subjects received benefits continuously for the entire year following FCE (fig 1). Of subjects experiencing benefit suspension or claim closure, 79 subjects (24%) resumed time‐loss benefits after initial suspension and 74 (23%) had their claim reopened or filed a new upper extremity injury claim in the year following FCE. Twenty six subjects experienced both forms of recurrence giving an overall rate of 39%. No significant differences were observed between the specific and less specific groups on any of the outcome measures.
Figure 1 Kaplan‐Meier curve showing days to suspension of time‐loss benefits after functional capacity evaluation (n = 336).
Timely recovery
Higher weight lifted on the waist‐to‐overhead (hazard ratio (HR) 1.5 to 1.7) and floor‐to‐waist lift (HR 1.2 to 1.3) tests were modestly associated with faster suspension of benefits (table 3). Comparable predictive ability was seen in the specific (r2 for Cox regression 2–8%) and less specific groups (r2 for Cox regression 2–5%). Compared to the other two lift tests, horizontal lifting was less strongly associated with faster benefit suspension. Higher right handgrip strength was weakly associated with faster benefit suspension but only in subjects with a specific diagnosis, whereas the number of failed FCE tasks and left handgrip strength were not clearly associated with this outcome. Limiting the analysis to those with left or right sided injuries only did not meaningfully alter the prognostic value of right or left handgrip strength. When each of the FCE lift and handgrip variables were entered simultaneously into a multivariable regression equation, waist‐to‐overhead lift was the only FCE indicator independently associated with benefit suspension (specific injury subjects HR 1.82 (95% CI 1.22 to 2.72), less specific HR 1.64 (95% CI 0.99 to 2.74).
Table 3 Results of Cox proportional hazards regression modeling days to suspension of time‐loss benefits.
| Entire sample (n = 336) | PVE† | Specific injury (n = 185) | PVE | Less‐specific injury (n = 151) | PVE | |
|---|---|---|---|---|---|---|
| Hazard ratio (95% CI) | Hazard ratio (95% CI) | Hazard ratio (95% CI) | ||||
| Number of failed FCE items (out of 15) | 0.96 (0.93–0.99) | 1.9 | 0.95 (0.90–0.99) | 3.1 | 0.97 (0.92–1.02) | 1.0 |
| Adjusted* | 0.97 (0.94–1.00) | 0.8 | 0.96 (0.92–1.00) | 1.7 | 0.98 (0.93–1.04) | 0.3 |
| Waist‐to‐overhead (10 kg units) | 1.51 (1.28–1.78) | 6.4 | 1.53 (1.24–1.90) | 7.4 | 1.50 (1.15–1.94) | 5.3 |
| Adjusted* | 1.55 (1.29–1.87) | 5.7 | 1.69 (1.31–2.19) | 7.7 | 1.45 (1.09–1.93) | 4.9 |
| Floor‐to‐waist (10 kg units) | 1.23 (1.10–1.38) | 3.6 | 1.28 (1.09–1.49) | 4.7 | 1.20 (1.01–1.42) | 2.7 |
| Adjusted* | 1.21 (1.06–1.38) | 2.2 | 1.26 (1.05–1.52) | 3.2 | 1.17 (1.96–1.42) | 1.6 |
| Horizontal lift (10 kg units) | 1.19 (1.07–1.32) | 2.7 | 1.20 (1.04–1.39) | 3.1 | 1.18 (1.00–1.39) | 2.5 |
| Adjusted* | 1.14 (1.01–1.29) | 1.3 | 1.14 (0.97–1.35) | 1.3 | 1.15 (0.96–1.37) | 1.5 |
| Right handgrip (10 kg units) | 1.07 (1.00–1.15) | 1.2 | 1.09 (1.00–1.19) | 2.1 | 1.04 (0.94–1.16) | 0.4 |
| Adjusted* | 1.08 (1.01–1.16) | 1.5 | 1.09 (1.00–1.19) | 1.7 | 1.07 (0.95–1.21) | 0.9 |
| Left handgrip (10 kg units) | 0.99 (0.93–1.05) | 0 | 0.98 (0.91–1.07) | 0 | 1.00 (0.90–1.11) | 0 |
| Adjusted* | 0.98 (0.92–1.05) | 0 | 0.98 (0.90–1.06) | 0 | 1.00 (0.89–1.13) | 0 |
*All FCE items adjusted for gross annual salary and pain visual analogue scale.
†Proportion of variation explained (out of 100).
Higher weight lifted on the waist‐to‐overhead and floor‐to‐waist lifts were also consistently associated with faster claim closure (table 4), and again comparable predictive ability was seen in specific (r2 for Cox regression 3–9%) and less specific (r 2 for Cox regression 5–11%) groups. Again, horizontal lift performance was less closely associated with faster claim closure. Higher right and left handgrip strength were associated with faster claim closure but only in subjects with less specific disorders whereas the number of failed FCE tasks was not clearly associated with faster claim closure. When the FCE lift and handgrip variables were entered simultaneously into a multivariable regression equation, waist‐to‐overhead lift was the only FCE indicator independently associated with claim closure (specific injury HR 2.32 (95% CI 1.49 to 3.61), less specific HR 2.06 (95% CI 1.24 to 3.43)). As can be seen in table 4, some hazard ratios increased after controlling for confounders. The increase was consistently observed after salary was added to the models (similar to the time to benefit suspension outcome).
Table 4 Results of Cox proportional hazards regression modeling days to claim closure.
| Entire sample (n = 336) | PVE† | Specific injury (n = 185) | PVE | Less specific injury (n = 151) | PVE | |
|---|---|---|---|---|---|---|
| Hazard ratio (95% CI) | Hazard ratio (95% CI) | Hazard ratio (95% CI) | ||||
| Number of failed FCE items (out of 15) | 0.96 (0.93–0.99) | 1.6 | 0.96 (0.92–1.01) | 1.3 | 0.95 (0.90–1.01) | 2.0 |
| Adjusted* | 0.98 (0.94–1.02) | 0.4 | 0.98 (0.93–1.03) | 0.4 | 0.97 (0.92–1.03) | 0.1 |
| Waist‐to‐overhead (10 kg units) | 1.70 (1.43–2.04) | 9.2 | 1.65 (1.31–2.06) | 9.0 | 1.81 (1.36–2.41) | 9.3 |
| Adjusted* | 1.81 (1.49–2.20) | 9.1 | 1.79 (1.38–2.33) | 8.9 | 1.96 (1.46–2.64) | 10.9 |
| Floor‐to‐waist (10 kg units) | 1.29 (1.14–1.47) | 4.5 | 1.26 (1.06–1.50) | 3.7 | 1.31 (1.10–1.57) | 5.2 |
| Adjusted* | 1.29 (1.13–1.49) | 3.7 | 1.26 (1.03–1.53) | 2.7 | 1.37 (1.12–1.67) | 5.8 |
| Horizontal lift (10 kg units) | 1.22 (1.09–1.38) | 3.1 | 1.17 (1.00–1.37) | 2.1 | 1.27 (1.07–1.52) | 4.3 |
| Adjusted* | 1.21 (1.06–1.37) | 2.3 | 1.14 (0.96–1.37) | 1.2 | 1.32 (1.09–1.59) | 5.0 |
| Right handgrip (10 kg units) | 1.08 (1.01–1.16) | 1.4 | 1.06 (0.98–1.16) | 1.1 | 1.11 (0.99–1.25) | 0.2 |
| Adjusted* | 1.09 (1.02–1.18) | 1.8 | 1.06 (0.97–1.15) | 0.6 | 1.22 (1.07–1.39) | 5.4 |
| Left handgrip (10 kg units) | 1.03 (0.96–1.10) | 0.2 | 0.99 (0.91–1.07) | 0.5 | 1.11 (0.98–1.25) | 1.8 |
| Adjusted* | 1.05 (0.98–1.12) | 0.5 | 0.96 (0.88–1.04) | 0.2 | 1.18 (1.04–1.34) | 4.1 |
*All FCE items adjusted for gross annual salary and percent Pain Disability Index.
†Proportion of variation explained (out of 100).
Sustained recovery
Right hand grip strength was the only FCE indicator significantly associated with future recurrence but only within subjects with specific injuries (table 5). Odds of experiencing a future recurrent event increased about 20% for each additional 10 kg in right grip strength. However, this association diminished and became non‐significant (odds ratio 1.17 (95% CI 0.96 to 1.43) after controlling for age, gender, number of previous upper extremity claims, and annual salary.
Table 5 Results of logistic regression modeling future recurrence.
| Entire sample | Specific injury | Less specific injury | |
|---|---|---|---|
| (n = 326, 39% recurred*) | (n = 180, 39% recurred*) | (n = 146, 39% recurred*) | |
| Odds ratio (95% CI) | Odds ratio (95% CI) | Odds ratio (95% CI) | |
| Number of failed FCE items (out of 15) | 0.98 (0.92–1.05) | 0.96 (0.87–1.05) | 1.01 (0.91–1.13) |
| Adjusted† | 0.97 (0.90–1.04) | 0.95 (0.86–1.04) | 1.00 (0.89–1.12) |
| Waist‐to‐overhead (10 kg units) | 1.10 (0.79–1.52) | 1.21 (0.80–1.84) | 0.93 (0.54–1.59) |
| Adjusted† | 0.87 (0.60–1.27) | 0.95 (0.60–1.52) | 0.75 (0.38–1.47) |
| Floor‐to‐waist (10 kg units) | 1.04 (0.83–1.31) | 1.06 (0.78–1.44) | 1.02 (0.72–1.43) |
| Adjusted† | 1.05 (0.70–1.17) | 0.89 (0.63–1.24) | 0.95 (0.63–1.46) |
| Horizontal lift (10 kg units) | 1.05 (0.84–1.30) | 1.10 (0.83–1.47) | 0.98 (0.70–1.36) |
| Adjusted† | 0.93 (0.73–1.19) | 0.97 (0.71–1.33) | 0.88 (0.59–1.33) |
| Right handgrip (10 kg units) | 1.15 (1.00–1.32) | 1.26 (1.04–1.51) | 1.00 (0.81–1.25) |
| Adjusted† | 1.08 (0.92–1.27) | 1.17 (0.96–1.43) | 0.89 (0.66–1.19) |
| Left handgrip (10 kg units) | 1.03 (0.90–1.18) | 1.05 (0.88–1.24) | 1.00 (0.80–1.26) |
| Adjusted† | 0.95 (0.81–1.12) | 0.98 (0.81–1.18) | 0.90 (0.65–1.24) |
*Defined as whether a subject restarted time‐loss benefits, reopened their claim, or filed a new upper extremity claim within the year following FCE.
†All FCE indicators adjusted for age, gender, number of previous upper extremity WCB claims, and annual salary.
A more detailed investigation of the 12 subjects rated as meeting or exceeding job requirements on all FCE items revealed these subjects did not have a lower likelihood of recurrence. All 12 subsequently experienced suspension of benefits or claim closure; however, four (33%) of these subjects experienced a future recurrence with three resuming time‐loss benefits and one filing a new upper extremity claim.
Discussion
Better FCE lift performance was modestly associated with faster suspension of time loss benefits and claim closure in this sample of subjects off work due to upper extremity disorders, with waist‐to‐overhead lift being the most predictive FCE indicator. Whether subjects demonstrated performance on FCE that was rated as meeting or exceeding physical job demand levels was not clearly associated with any recovery outcome. The number of failed FCE tasks was unrelated to any recovery outcome and examination of the 12 subjects who were rated as meeting all required job demands indicated they were not at a substantially lower risk of recurrence. In fact, no FCE variable was clearly associated with future recurrence after controlling for potential confounders, indicating FCE does not provide important information regarding a claimant's likelihood of safe return‐to‐work or future reinjury. This is consistent with findings related to FCE in the low back pain population.7,33
Not supported was our hypothesis that FCE would be more predictive of outcomes in subjects with specific injuries due to its ability to detect physical impairment barriers to return to work, such as reduced muscle strength or joint mobility restricting work ability. FCE predictive ability was not clearly better in subjects with distinct pathology such as amputation, fracture, dislocation, or tendon rupture compared to subjects with less specific diagnoses such as non‐specific pain, myofascial pain, or lateral epicondylitis. In fact, better FCE performance was slightly more predictive of faster claim closure in subjects with more ambiguous, pain mediated disorders. This may indicate that physical impairments are not the most important barriers to return to work in claimants with distinct pathology or injury once the condition has become chronic in nature. Additionally, this observation provides support for the conceptualisation of performance based functional tests as behavioural assessments as opposed to strict physical capacity tests.
Regarding FCE's modest overall predictive value and the fact that some items in the protocol appeared to provide meaningless information for purposes of prediction, it may be possible to obtain all or most of the important information using a condensed protocol. When all of the lift and handgrip variables were entered simultaneously into a multivariable regression model, the waist‐to‐overhead lift remained the only factor independently associated with benefit suspension and claim closure indicating the FCE likely contains redundant items. This observation is comparable to previous findings that identified the floor‐to‐waist lift task as the most important item in the Isernhagen protocol for claimants with back pain.6 Potentially, testing only the waist‐to‐overhead lift would provide sufficient information for determining likelihood of future recovery outcomes, such as those examined in this study, in claimants with upper extremity disorders.
As mentioned, none of the FCE variables considered was clearly associated with future recurrence. Thus, FCE has questionable value in determining which claimants are “safe” to return to work or at low risk of future recurrence. The observed rate of recurrence (39%) following FCE in this cohort of workers' compensation claimants with upper extremity disorders was dramatically higher than that observed in a related cohort of claimants with low back pain (20%).7 No other published research could be located indicating administrative or claims recurrence rates in claimants with upper extremity disorders. One report by Pransky and colleagues has been published detailing results of a survey administered on workers one year after reporting a work related upper extremity disorder, which indicated a 26% recurrence rate.34 However, the self‐report of re‐injury data cannot be directly compared with our administrative recurrence rates. More research is needed on the phenomenon of recurrence in upper extremity disorders to determine which factors influence or predict this important outcome. Until more is known, the design of effective interventions for prevention of recurrent disability for these disorders is unlikely.
Limitations of this study include reliance on administrative databases, which influenced our selection of potential prognostic factors and outcomes. Although claim and benefit status are important personal and societal outcomes, they likely only partially depict recovery and return to function. In addition, information on all potentially confounding factors was not available in the databases. Another potential source of bias is measurement error, as the reliability and validity of the methods used for determining job demands for comparison to FCE performance have not been studied. Results are only fully generalisable to the Isernhagen Work Systems' FCE and may not apply to all available FCE protocols.
Conclusions
Higher weight lifted during FCE was consistently, yet modestly, associated with faster time to benefit suspension and claim closure in a sample of claimants with upper extremity disorders. Whether subjects demonstrated FCE performance that met or exceeded physical job demands was unrelated to future return to work or work readiness determinations, and no FCE indicators were associated with future recurrence. FCE was no more predictive in claimants with specific pathology and injury than in those with more ambiguous, pain mediated conditions.
Main messages
Higher weight lifted during FCE was consistently, yet modestly, associated with faster time to benefit suspension and claim closure in a sample of claimants with upper extremity disorders.
Whether subjects demonstrated functional performance that met or exceeded physical job demands was unrelated to future recovery.
The one year recurrence rate, defined as whether benefits restarted, the claim reopened, or a new upper extremity claim was filed, was 39%.
No FCE indicators were associated with future recurrence.
FCE was no more predictive in claimants with specific pathology and injury than in those with more ambiguous, pain mediated conditions.
Policy implications
Lifting performance during FCE may provide some information for predicting time to benefit suspension and claim closure in workers' compensation claimants with upper extremity disorders.
Workers' Compensation Boards and insurers should not rely solely on information from FCE to determine the work readiness of injured workers with upper extremity disorders as ability to return to work is likely to be underestimated.
Recurrence rates in compensable upper extremity disorders appear high and further research is needed in this area.
Acknowledgements
This research was financially supported by a research grant from the Workers' Compensation Board of Alberta.
Footnotes
Competing interests: none.
The University of Alberta Health Research Ethics Board approved this research.
References
- 1.Silverstein B, Welp E, Nelson N.et al Claims incidence of work‐related disorders of the upper extremities: Washington state, 1987 through 1995. Am J Public Health 1998881827–1833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fabrizio A J. Work‐related upper extremity injuries: prevalence, cost and risk factors in military and civilian populations. Work 200218115–121. [PubMed] [Google Scholar]
- 3.Lechner D, Roth D, Straaton K. Functional capacity evaluation in work disability. Work 1991137–47. [Google Scholar]
- 4.Isernhagen S J. Return to work testing: functional capacity and work capacity evaluation. Orthop Phys Ther NA 1992183–98. [Google Scholar]
- 5.Innes E, Straker L. Validity of work‐related assessments. Work 199913125–152. [PubMed] [Google Scholar]
- 6.Gross D P, Battie M C, Cassidy J D. The prognostic value of functional capacity evaluation in patients with chronic low back pain: part 1: timely return to work. Spine 200429914–919. [DOI] [PubMed] [Google Scholar]
- 7.Gross D P, Battie M C. The prognostic value of functional capacity evaluation in patients with chronic low back pain: part 2: sustained recovery. Spine 200429920–924. [DOI] [PubMed] [Google Scholar]
- 8.Reneman M F, Fokkens A S, Dijkstra P U.et al Testing lifting capacity: validity of determining effort level by means of observation. Spine 200530E40–E46. [DOI] [PubMed] [Google Scholar]
- 9.Cutler R B, Fishbain D A, Steele‐Rosomoff R.et al Relationships between functional capacity measures and baseline psychological measures in chronic pain patients. J Occup Rehabil 200313249–258. [DOI] [PubMed] [Google Scholar]
- 10.Hunt D G, Zuberbier O A, Kozlowski A J.et al Are components of a comprehensive medical assessment predictive of work disability after an episode of occupational low back trouble? Spine 2002272715–2719. [DOI] [PubMed] [Google Scholar]
- 11.Isernhagen S J. Functional capacity evaluation: rationale, procedure, utility of the kinesiophysical approach. J Occup Rehab 19922157–168. [DOI] [PubMed] [Google Scholar]
- 12.United States Employment and Training Administration Dictionary of occupational titles. 4th edition. Indianapolis: JIST Works, 1991
- 13.Gross D P, Battié M C. Reliability of safe maximum lifting determinations of a functional capacity evaluation. Phys Ther 200282364–371. [PubMed] [Google Scholar]
- 14.Buddenberg L A, Davis C. Test‐retest reliability of the Purdue Pegboard Test. Am J Occ Ther 200054555–558. [DOI] [PubMed] [Google Scholar]
- 15.Mathiowetz V. Comparison of Rolyn and Jamar dynamometers for measuring grip strength. Occup Ther Int 20029201–209. [DOI] [PubMed] [Google Scholar]
- 16.Reneman M F, Jaegers S, Westmaas M.et al The reliability of determining effort level of lifting and carrying in a functional capacity evaluation. Work 20021823–27. [PubMed] [Google Scholar]
- 17.Brouwer S, Reneman M F, Dijkstra P U.et al Test‐retest reliability of the Isernhagen Work Systems Functional Capacity Evaluation in patients with chronic low back pain. J Occup Rehab 200313207–218. [DOI] [PubMed] [Google Scholar]
- 18.Matheson L N, Isernhagen S J, Hart D L. Relationships among lifting ability, grip force, and return to work. Phys Ther 200282249–256. [PubMed] [Google Scholar]
- 19.Feuerstein M, Shaw W S, Lincoln A E.et al Clinical and workplace factors associated with a return to modified duty in work‐related upper extremity disorders. Pain 200310251–61. [DOI] [PubMed] [Google Scholar]
- 20.Himmelstein J S, Feuerstein M, Stanek E J., 3rdet al Work‐related upper‐extremity disorders and work disability: clinical and psychosocial presentation. J Occup Environ Med 1995371278–1286. [DOI] [PubMed] [Google Scholar]
- 21.Bernard B P, National Institute for Occupational Safety and Health Musculoskeletal disorders and workplace factors: a critical review of epidemiologic evidence for work‐related musculoskeletal disorders of the neck, upper extremity, and low back. Ohio: Cincinnati, 1997
- 22.Tait R C, Chibnall J T, Krause S. The Pain Disability Index: psychometric properties. Pain 199040171–182. [DOI] [PubMed] [Google Scholar]
- 23.Gronblad M, Hupli M, Wennerstrand P.et al Intercorrelation and test‐retest reliability of the Pain Disability Index (PDI) and the Oswestry Disability Questionnaire (ODQ) and their correlation with pain intensity in low back pain patients. Clin J Pain 19939189–195. [DOI] [PubMed] [Google Scholar]
- 24.National occupational classification: occupational descriptions Human Resources Development Canada 2001
- 25.Cole D C, Mondloch M V, Hogg‐Johnson S. Listening to injured workers: how recovery expectations predict outcomes—a prospective study. CMAJ 2002166749–754. [PMC free article] [PubMed] [Google Scholar]
- 26.Cote P, Hogg‐Johnson S, Cassidy J D.et al The association between neck pain intensity, physical functioning, depressive symptomatology and time‐to‐claim‐closure after whiplash. J Clin Epidemiol 200154275–286. [DOI] [PubMed] [Google Scholar]
- 27.Krause N, Dasinger L K, Deegan L J.et al Alternative approaches for measuring duration of work disability after low back injury based on administrative workers' compensation data. Am J Ind Med 199935604–618. [DOI] [PubMed] [Google Scholar]
- 28.Dasinger L K, Krause N, Deegan L J.et al Duration of work disability after low back injury: a comparison of administrative and self‐reported outcomes. Am J Ind Med 199935619–631. [DOI] [PubMed] [Google Scholar]
- 29.Kleinbaum D G.Survival analysis: a self‐learning text. 1st edition. New York: Springer, 1996
- 30.Hosmer D W, Lemeshow S.Applied survival analysis: regression modeling of time to event data. 1st edition. New York: Wiley, 1999
- 31.Schemper M. The relative importance of prognostic factors in studies of survival. Stat Med 1993122377–2382. [DOI] [PubMed] [Google Scholar]
- 32.Hosmer D W, Lemeshow S.Applied logistic regression. 2nd edition. New York: Wiley, 2000
- 33.Gross D P, Battie M C. Functional capacity evaluation performance does not predict sustained return to work in claimants with chronic back pain. J Occup Rehabil 200515285–294. [DOI] [PubMed] [Google Scholar]
- 34.Pransky G, Benjamin K, Hill‐Fotouhi C.et al Occupational upper extremity conditions: a detailed analysis of work‐related outcomes. J Occup Rehabil 200212131–138. [DOI] [PubMed] [Google Scholar]