Abstract
Background
Shift work, noise, and physical workload are very common occupational exposures and they tend to cluster in the same groups of workers.
Objectives
To study the short and long term effects of these exposures on risk of coronary heart disease (CHD) and to estimate the joint effects of these factors.
Methods
The study population in this prospective 13 year follow up study of 1804 middle aged industrially employed men was collected at the first screening for the Helsinki Heart Study. The CHD end points (ICD‐9 codes 410–414 and ICD‐10 codes I20–I25) were obtained from official Finnish registers. The Finnish job‐exposure matrix FINJEM provided information on occupational exposures. Relative risks (RR) of CHD for the exposures were estimated using Cox's proportional hazard models adjusting for classical risk factors of CHD.
Results
The RR in the five year follow up for continuous noise combined with impulse noise was 1.28; for shift work it was 1.59, and for physical workload 1.18, while in the 13 year follow up the RRs were 1.58, 1.34, and 1.31, respectively. When adjusted for white‐collar/blue‐collar status the RRs decreased markedly. The RR in the 13 year follow up for those exposed to two risk factors was close to 1.7 and for those exposed to all three, 1.87.
Conclusion
Shift work and continuous noise entailed an excess risk for CHD in the shortest follow up with only a few retired workers but a decreasing risk during the longer follow up. For physical workload and impulse noise the trend was opposite: the CHD risk was increasing with increasing follow up time despite increasing numbers of retired workers.
Keywords: job exposure matrix, longitudinal study, register linkage
Night work and shift work are unavoidable in industrialised societies. Among workers in the European Community, the average number who worked night and shift was 17% in 2000.1 In Finland, where 23% worked in shifts,1 the frequency of 2‐ and 3‐shift work has increased, especially in industry, from 26% in 1984 to 36% in 2003.2 Different kinds of work schedules and irregular working hours have various effects on an individual's health, performance, and wellbeing.3 Shift work may also be related to increased mortality.4,5 It has been estimated that approximately 10–20% of shift workers fail to adjust.6
The coronary heart disease (CHD) risk due to shift work has been extensively studied for decades with both positive and negative findings.7,8,9,10 In their review, Boggild and Knutsson concluded that on balance shift workers were found to have a 40% increase in CHD risk.7 Meanwhile, a somewhat later 22 year follow up study found no excess risk of CHD associated with shift work.8 In a later paper on the work environment of Danish shift and day workers, Boggild and colleagues9 elaborate on the issue. They found that shift work was commonly associated with other work environment factors shown to be related to CHD, and they raised the question whether shift work could be acting as proxy for other work environment exposures. Indeed, shift work, occupational exposure to noise, and physical workload constitute a triad of factors that tend to cluster in the same groups of workers; they have all been identified as CHD risk factors,10 but none of them uniformly in all studies, leaving the true culprit's identity open.
Like shift work, occupational noise is also a very common exposure—it has been estimated that in 2002 about 18% of the Finnish work force was exposed to noise level >80 dB and about 8% to noise level >85 dB.11 In a recent Danish study on noise exposure in some high risk industries, Kock et al found that about 50% of the workers were exposed to more than 85 dB(A).12 The associations of both environmental and occupational noise exposure with CHD risk factors have been studied for decades, yielding both positive and negative findings. In their meta‐analysis, van Kempen and colleagues13 concluded that this relation between noise exposure and ischaemic heart disease is still inconclusive. However, after this meta‐analysis Davies et al performed a large CHD mortality follow up of Canadian lumber mill workers with different levels of exposure to noise.14 They found an exposure‐response trend with an RR of 1.5 in the highest exposure group. In our previous study based on a larger population than the present one, we found a significant excess risk of CHD, ranging from 25% to 60%, depending on the length of follow up time and reference group used.15 The CHD risk of the workers exposed to noise, especially impulse noise, persisted even when most of the cohort was retired and thus no longer exposed to occupational noise.
Physical activity is a well known protective factor in cardiovascular diseases (CVD) and in all‐cause mortality.16 Not only leisure time but also occupational physical activity were found to reduce CVD and all‐cause mortality.17 On the other hand, high physical workload was found to be a risk factor in all‐cause and CVD mortality.18 In a register and job exposure matrix based study on cardiovascular mortality among Finnish males, it was found that the most influential job exposures were high workload, low control, noise, and shift work.19
In contrast to psychosocial factors, physical workload, noise, and shift work form a true triad of “hard” occupational risk factors. For preventive purposes it would be important to know not only their independent effects—if any—but also their joint effects. As far we know, there are no studies exploring the joint effects on CHD risk inside this triad. In addition, does the increased risk persist, even when there is no more exposure, or will it disappear as in case of smoking and CHD risk, where the considerable excess risk decreases when a person stops smoking?20 This is a new and pragmatic view when evaluating occupational risks, and will be relevant for a growing number of older workers.
The aim of the present study was to compare the short term and long term effects of occupational exposures to noise, physical workload, and shift work on risk of CHD among industrially employed men. Secondly, we evaluated the joint effect of these exposures and also studied the persistence of this effect with increasing follow up time—that is, increasing age of the worker.
Methods
Study population and follow up via linkage to population registers
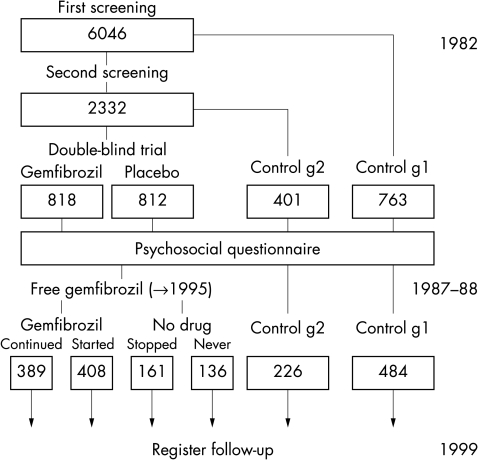
The subjects were selected from among the participants of the first screening visit for the Helsinki Heart Study (HHS), a five year randomised, double blind, placebo controlled primary prevention trial of gemfibrozil, a lipid lowering drug, in middle aged men (aged 40–55 years at entry).21 The participants for the trial were selected via two successive screenings at two government agencies (n = 12 893) and five industrial companies (n = 6046). All those with non‐HDL cholesterol below 5.2 mmol/l were excluded, as were those who had CHD or any other major illness. However, a low cholesterol control group was formed by randomly selecting every seventh participant from those not fulfilling the inclusion criteria. A second control group was formed from those participants with non‐HDL cholesterol above 5.2 mmol/l at the first screening, but below 5.2 mmol/l at the second screening. Those who fulfilled the lipid criterion at both screenings, but had evidence of CHD, were included in a secondary prevention trial. After the double blind trial all trial participants were offered free gemfibrozil until the end of 1995.
In the present follow up cohort, only participants employed in industry were included (fig 1). At the end of the trial in 1986–87, a psychosocial questionnaire was sent to all those who participated in the primary and the secondary trials, and also to those in both control groups. The response rate was 70% (n = 1947) for the industrial group. After the exclusion of those with missing information on occupation or shift work status and a small group of part‐time and night workers, the study group comprised 1804 men. Of these, 46.9% had never been on gemfibrozil, 31.5% had been on gemfibrozil either during the double blind trial or thereafter, and 21.6% continued medication after the double blind trial.
Figure 1 Numbers of industrially employed participants in different phases of the Helsinki Heart Study.
Among the participants were 344 men who were already retired when completing the questionnaire. However, we decided to include all subjects in the study because of examining the long term effects. The average age of retirement in Finland is 59 years,22 and at the end of 1999 there were, if alive, 91.0% of men 59 years or older.
The cardiac end points were obtained from the Hospital Discharge Register (kept by the National Research and Development Centre for Welfare and Health) and the Register of Deaths (kept by Statistics Finland). Several studies have found these registers to be accurate enough for epidemiological purposes in studies on CHD.23,24 Because of the long follow up, definition of CHD was based on codes 410–414 of the International Classification of Diseases (ICD), 8th and 9th version for the years 1982–95 and I20–I25 of the ICD, 10th version for the years 1996–99.
The cohort was followed up from 1987–88 to the end of 1999 with a mean follow up time of 10.6 years. Due to the long follow up time we present results with progressively longer follow ups: to the end of 1991, 1995, and 1999. Until the end of 1999 there were 344 cases of coronary events, of which 45 were fatal.
Shift work status and occupation
Shift work was recorded in the questionnaire on the following 6‐point item: day work, part‐time work, 2‐shift work, 3‐shift work, irregular work, and night work. In the analyses a dichotomised variable was used (day work, shift work—all combined). Irregular shift systems, with variation in the number and sometimes also the length of the consecutive morning, evening, and night shifts, were a minority in this sample. The 14 men working part‐time, 2 men working nights, and 117 men without shift work information were excluded.
Occupational information was based on the 3‐digit occupational code used in the 1980 census—a Finnish version of the Nordic Classification of Occupations of 1965.25 This information was obtained by record linkage with Statistics Finland. The linkage was based on Personal Identification Numbers. There are 10 major occupational classes. We considered classes 0, 1, and 2 as white‐collar work and classes 3 to 9 as blue‐collar work. The four largest blue‐collar occupational categories were paper and board mill workers, sawyers, forestry supervisors, and forklift operators etc. Forty four per cent of the white‐collar workers were technicians in chemical or mechanical engineering or technicians working in other branches of engineering. The 10 men without an occupational code were excluded.
In this industrial study population, 71.0% of the participants were blue‐collar workers. Among the blue‐collar workers, 48.2% were shift workers, compared with only 9.0% of the white‐collar workers. Most of the participants in the shift work groups (93.8%) had held their jobs for more than five years.
Linkage to FINJEM to obtain estimates of exposure to noise or perceived physical workload
FINJEM is a multipurpose information system which covers major occupational exposures occurring in Finland since 1945.26 Agents, occupations, and calendar periods are the basic dimensions by which exposure is assessed. Exposure is characterised by the proportion of exposed (P) and the mean level of exposure among the exposed (L) by occupation and period. The exposure estimates are based on the judgement of about 20 experts at the Finnish Institute of Occupational Health. The grounds for estimates, definitions of agents, and measurement/survey data are documented in the FINJEM database.
In this study exposures of continuous and impulse noise are used for the period 1985–94. The latter is occupational exposure to noise entailing such impulse that the equivalent dose in dB underestimates the risk of noise induced hearing loss. The proportion of exposed and the mean level of exposure were linked to the data using 3‐digit occupational code. The proportion of exposed in both noise exposures was either 0% or 100%, so in the analyses only the mean level of exposure was used. The mean level of noise exposure among 864 (47.9%) of the men exposed ranged from 80 to 100 dBA. Of these, 184 (10.2% of all) were also assigned as exposed to impulse noise. All men exposed to impulse noise worked in manufacturing and related work (table 1). None of the white‐collar workers was exposed to noise.
Table 1 Prevalence of noise exposure, shift work, and physical workload exposure by occupational category.
| Occupational category | n | Prevalence of noise exposure (%) | Prevalence of shift work (%) | Prevalence of physical workload§ (%) | |||||
|---|---|---|---|---|---|---|---|---|---|
| Un‐exposed | Continuous noise | Both types of noises | Un‐exposed | 2 tertile | 3 tertile | ||||
| 0–2 | White‐collar* | 524 | 100 | 9.0 | 98.3 | 1.5 | 0.2 | ||
| 3 | Agriculture, forestry, commercial fishing | 95 | 85.3 | 14.7 | 3.2 | 84.2 | 15.8 | ||
| 5 | Transport and communications work | 65 | 47.7 | 52.3 | 33.8 | 80.0 | 20.0 | ||
| 6 | Manufacturing and related work† | 513 | 23.2 | 41.1 | 35.7 | 32.2 | 1.9 | 10.5 | 87.5 |
| 7 | Manufacturing and related work‡ | 561 | 26.7 | 73.1 | 0.2 | 70.9 | 23.2 | 54.7 | 22.1 |
| Other | 46 | 76.1 | 23.9 | 63.0 | 58.7 | 41.3 | |||
| Total | 1804 | 52.1 | 37.7 | 10.2 | 36.8 | 43.6 | 22.7 | 33.7 | |
*0 = technical, physical, science, social science, humanistic, and artistic work; 1 = administrative, managerial, and clerical work; 2 = sales work.
†Fine mechanical work; iron and metalware work; electrical work; wood work.
‡Graphic work; glass, ceramic and clay work; chemical processing and related work.
§Product of proportion of exposed (prevalence P) and the mean level of exposure among the exposed (level L).
In the analyses both continuous and impulse noise were divided into two classes: 0, ⩾80 dB, and unexposed and exposed respectively. If a man was exposed to impulse noise he was also exposed to continuous noise. The combined noise variable consisted of three classes (no noise, continuous noise, continuous and impulse noises).
The FINJEM estimates from the period 1985–94 were used to assess perceived physical workload, referring to tasks where the whole body is exerted by dynamic muscular work. Exposure estimates were based on data of the 1990 survey of working conditions by Statistics Finland. About 4000 salaried workers were interviewed in this survey. Those who considered their work to be physically rather heavy or very heavy were considered to be exposed. The level of exposure was derived from the distribution of responses between rather heavy and very heavy work (score between zero and one). If the number of respondents in an occupation was small, data from a suitable proxy occupation were used. The exposure metric used in the analyses was the product of the proportion of the exposed and the mean level of exposure in that occupation. In the analyses this variable was categorised into tertiles.
Blood pressure, serum lipids, and some lifestyle factors
Blood pressure, height, and weight were measured at the first screening visit by experienced nurses at the workplace clinics of the participants. The lipid measurements in this lipid modulation trial have been described in detail elsewhere.21 Smoking habits were also recorded by questionnaire at the first screening visit (daily consumption of cigarettes), and a dichotomous variable (current smokers, non‐smokers) was used in the analyses. Ex‐smokers were coded as non‐smokers.
Treatment with gemfibrozil
As shown in fig 1, some of the subjects in the present study had participated in the clinical trial, and during our follow up 44.2% of the present study population were on gemfibrozil.
The triad of occupational exposures: shift work, noise, and physical workload
There was a high degree of clustering among the three exposures: among those with manufacturing and related work (occupational category 7), 73.3% were exposed to noise, 70.9% to shift work, and 76.8% to physical workload, while among white‐collar workers, none were exposed to noise, only 9.0% to shift work, and only 1.7% to physical workload (table 1).
The Spearman correlation coefficient between combined noise and physical workload (tertiles) was 0.58. A high percentage of those exposed to noise were simultaneously exposed to a higher level of physical workload (34.8%) or to both physical workload and shift work (21.6%). All subjects exposed to impulse noise were also exposed to physical workload.
Noise, shift work, physical workload, and levels of some classical risk factors for CHD
An overview of the mean body mass index (BMI), systolic blood pressure (SBP), diastolic blood pressure (DBP), and serum total cholesterol as well as the percentage of smokers and use of gemfibrozil by different occupational exposures is given in table 2. Continuous noise exposed blue‐collar workers had the highest BMI, but other factors were highest for blue‐collar workers exposed to both types of noises. Among unexposed white‐collar workers the mean SBP was 137.1 mm Hg compared with 142.2 mm Hg in blue‐collar workers exposed to both noises. There were no substantial differences between blue‐collar day and shift workers, but differences between white‐collar and blue‐collar day and shift workers were more obvious. The greatest difference for smoking was found between white‐collar day workers and shift workers: 28.2% of day workers smoked compared with 46.8% of shift workers. Almost all (98.3%) white‐collar workers were unexposed to physical workload. However, mean levels of SBP and DBP were considerably lower than in unexposed blue‐collar workers. The mean ages for different occupational exposure groups varied between 52.3 and 53.0 years.
Table 2 Means and standard deviations (SD) of body mass index (BMI), systolic and diastolic blood pressure (SBP, DBP), and total serum cholesterol (TotC) and percentages of smoking among industrially employed white‐collar and blue‐collar (W/B) workers by noise, shift work, and physical workload exposures.
| n | BMI (kg/m2) | SBP (mm Hg) | DBP (mm Hg) | TotC (mmol/l) | Use of gemfibrozil (%) | Smoking | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Never | Sometimes | Always | (%) | |||
| Noise | ||||||||||
| W | No noise | 524 | 26.0 (2.9) | 137.1 (15.8) | 89.3 (9.0) | 6.8 (1.1) | 42.9 | 36.5 | 20.6 | 29.8 |
| B | No noise | 416 | 26.6 (3.1) | 141.6 (16.3) | 91.1 (10.0) | 6.9 (1.1) | 40.9 | 40.4 | 18.8 | 32.2 |
| B | Continuous noise | 680 | 26.7 (2.8) | 141.4 (16.7) | 90.6 (10.0) | 6.9 (1.1) | 42.1 | 34.7 | 23.2 | 33.9 |
| B | Continuous and impulse noise | 184 | 26.5 (2.8) | 142.2 (16.6) | 91.4 (10.0) | 7.0 (1.1) | 38.6 | 37.0 | 24.5 | 34.8 |
| Day or shift work | ||||||||||
| W | Day work | 477 | 26.0 (2.9) | 137.0 (15.9) | 89.3 (9.0) | 6.8 (1.1) | 43.2 | 36.5 | 20.3 | 28.2 |
| W | Shift work | 47 | 26.2 (2.6) | 138.0 (14.9) | 89.6 (8.9) | 7.2 (1.3) | 40.4 | 36.2 | 23.4 | 46.8 |
| B | Day work | 663 | 26.6 (2.9) | 141.5 (16.3) | 91.1 (9.7) | 6.9 (1.1) | 41.5 | 37.1 | 21.4 | 32.3 |
| B | Shift work | 617 | 26.6 (2.9) | 141.7 (16.7) | 90.6 (10.3) | 6.9 (1.1) | 40.8 | 36.6 | 22.5 | 34.7 |
| Physical workload* | ||||||||||
| W | 1 tertile | 515 | 26.0 (2.9) | 137.1 (15.9) | 89.3 (9.0) | 6.8 (1.1) | 43.1 | 36.1 | 20.8 | 30.0 |
| B | 1 tertile | 272 | 26.8 (3.1) | 141.5 (16.3) | 90.6 (10.4) | 7.0 (1.0) | 39.0 | 40.8 | 20.2 | 33.2 |
| B | 2 tertile | 401 | 26.8 (2.9) | 141.0 (15.8) | 90.7 (10.0) | 6.9 (1.1) | 42.4 | 35.9 | 21.7 | 31.4 |
| B | 3 tertile | 607 | 26.5 (2.8) | 141.9 (17.1) | 91.1 (9.8) | 6.9 (1.1) | 41.4 | 35.7 | 22.9 | 34.9 |
*Product of proportion of exposed (prevalence P) and mean level of exposure (level L).
Statistical analysis
Means of SBP, DBP, BMI, and total serum cholesterol, and percentages of smoking were used to compare possible differences in the groups formed by occupational exposures.
To study the effect of the three occupational exposures on risk of CHD, Cox's proportional hazards models were used. Noise exposure was studied as a combined variable of three categories: no noise, continuous only, and both continuous and impulse noise. Shift work was treated as a dichotomous variable, and physical workload was categorised into tertiles. To evaluate the possible mediating or confounding effect of other CHD risk factors we added them into the model. For joint effects we formed a new variable on the basis of the dummy variables to represent different combinations of the risk factor levels, as is usual in experimental design. In the case of shift work (SW) and combined noise exposure (NO), for instance, the study population was divided into the following groups using a grouping variable: SW−&NO−, SW−&NO+, SW+&NO−, SW+&NO+.
On entering the study the men were 45–62 years old and at the end of the study they were 57–74 years old. As the follow up was long enough to allow for most of the subjects to be retired before the end‐point, different follow up times were used to study if aging (retirement of subjects) had an effect on CHD risk. The analyses were performed using the statistical packages Egret for Windows and SPSS 12.0.1 for Windows.
Results
Noise, shift work, and physical workload as predictors of CHD risk
We estimated the CHD risks for the three exposures using three follow up times, until the end of 1991, the end of 1995, and the end of 1999 (table 3). At the end of 1991 most of the subjects were still working, while at the end of 1999 most were retired. By comparing the risks obtained using different follow up times, we could see whether the risk persisted even after retirement. For the noise exposure two different trends emerged: “continuous noise only” was a significant risk factor (RR = 1.48, p = 0.05) in the shortest follow up, but no longer when the follow up was extended. In contrast, the risk due to “both noises” increased with increasing follow up time, with an RR = 1.58 (p = 0.01) when the follow up lasted to the end of 1999. A fairly similar pattern was found for physical workload with RR = 1.31 (p = 0.03) in the longest follow up. In the case of shift work the risk clearly decreased when the follow up was extended: those working shifts had RRs of CHD of 1.59, 1.41, and 1.34 (for all, p = 0.01) compared with day workers.
Table 3 Noise, shift work, and physical workload as a predictor of coronary heart disease (CHD) risk among industrially employed men for different follow ups (FU).
| n/CHD cases | Unadjusted | Age adjusted | SBP–TotC–Smo–BMI adjusted | Gemfibrozil adjusted | Adjusted‡ | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | |||
| Continuous and/or impulse noise | ||||||||||||
| FU –91 | No | 940/48 | 1 | 1 | 1 | 1 | 1 | |||||
| Continuous | 680/51 | 1.48 | (1.00–2.19) | 1.47 | (0.99–2.18) | 1.39 | (0.93–2.06) | 1.47 | (0.99–2.18) | 1.29 | (0.85–1.96) | |
| Both | 184/12 | 1.28 | (0.68–2.41) | 1.28 | (0.68–2.40) | 1.16 | (0.61–2.18) | 1.25 | (0.66–2.34) | 1.12 | (0.58–2.14) | |
| FU –95 | No | 940/99 | 1 | 1 | 1 | 1 | 1 | |||||
| Continuous | 680/90 | 1.27 | (0.96–1.70) | 1.27 | (0.95–1.69) | 1.21 | (0.91–1.61) | 1.27 | (0.96–1.69) | 1.16 | (0.86–1.57) | |
| Both | 184/27 | 1.42 | (0.93–2.17) | 1.42 | (0.93–2.17) | 1.29 | (0.84–1.98) | 1.39 | (0.91–2.13) | 1.28 | (0.83–1.99) | |
| FU –99 | No | 940/162 | 1 | 1 | 1 | 1 | 1 | |||||
| Continuous | 680/134 | 1.16 | (0.93–1.46) | 1.16 | (0.92–1.45) | 1.11 | (0.89–1.40) | 1.16 | (0.92–1.46) | 1.07 | (0.84–1.37) | |
| Both | 184/48 | 1.58 | (1.15–2.18)** | 1.59 | (1.15–2.19)** | 1.46 | (1.06–2.02)* | 1.56 | (1.13–2.16)** | 1.45 | (1.04–2.02)* | |
| Day or shift work | ||||||||||||
| FU –91 | Day | 1140/58 | 1 | 1 | 1 | 1 | 1 | |||||
| Shift | 664/53 | 1.59 | (1.10–2.31)* | 1.63 | (1.12–2.37)* | 1.49 | (1.02–2.17)* | 1.57 | (1.08–2.28)* | 1.47 | (0.98–2.19) | |
| FU –95 | Day | 1140/120 | 1 | 1 | 1 | 1 | 1 | |||||
| Shift | 664/96 | 1.41 | (1.08–1.84)* | 1.44 | (1.10–1.88)** | 1.33 | (1.01–1.74)* | 1.39 | (1.07–1.82)* | 1.32 | (0.99–1.76) | |
| FU –99 | Day | 1140/196 | 1 | 1 | 1 | 1 | 1 | |||||
| Shift | 664/148 | 1.34 | (1.08–1.66)** | 1.37 | (1.11–1.70)** | 1.30 | (1.04–1.61)* | 1.33 | (1.08–1.65)** | 1.27 | (1.01–1.60)* | |
| Physical workload† | ||||||||||||
| FU –91 | 1 tertile | 787/45 | 1 | 1 | 1 | 1 | 1 | |||||
| 2 tertile | 409/25 | 1.07 | (0.66–1.74) | 1.07 | (0.66–1.74) | 0.99 | (0.61–1.62) | 1.07 | (0.66–1.74) | 0.85 | (0.50–1.42) | |
| 3 tertile | 608/41 | 1.18 | (0.77–1.80) | 1.17 | (0.76–1.78) | 1.10 | (0.72–1.69) | 1.17 | (0.77–1.79) | 1.10 | (0.71–1.68) | |
| FU –95 | 1 tertile | 787/89 | 1 | 1 | 1 | 1 | 1 | |||||
| 2 tertile | 409/47 | 1.01 | (0.71–1.44) | 1.01 | (0.71–1.44) | 0.95 | (0.67–1.36) | 1.02 | (0.72–1.45) | 0.85 | (0.58–1.24) | |
| 3 tertile | 608/80 | 1.17 | (0.87–1.59) | 1.16 | (0.86–1.57) | 1.11 | (0.82–1.50) | 1.17 | (0.86–1.58) | 1.11 | (0.82–1.50) | |
| FU –99 | 1 tertile | 787/134 | 1 | 1 | 1 | 1 | 1 | |||||
| 2 tertile | 409/77 | 1.11 | (0.83–1.46) | 1.10 | (0.83–1.46) | 1.07 | (0.80–1.41) | 1.12 | (0.84–1.48) | 0.96 | (0.71–1.29) | |
| 3 tertile | 608/133 | 1.31 | (1.03–1.67)* | 1.29 | (1.02–1.64)* | 1.27 | (0.99–1.61) | 1.32 | (1.03–1.67)* | 1.26 | (0.99–1.60) | |
The relative risks (RR) with 95% confidence intervals (95% CI) and p value were derived using Cox proportional hazards models with different covariates.
SBP, systolic blood pressure; TotC, total serum cholesterol; Smo, smoking; BMI, body mass index.
*p<0.05; **p<0.01.
†Product of proportion of exposed (prevalence P) and mean level of exposure among the exposed (level L).
‡Noise adjusted for day/shift work, day/shift work adjusted for noise, physical workload adjusted for day/shift work.
By adjusting for some lifestyle related factors we explored what part of the effect of the occupational factors on CHD risk was possibly accounted for by lifestyle factors. The risks associated with all three occupational factors decreased somewhat, suggesting that the effect was partially mediated by lifestyle. We also explored the effect when occupational factors were adjusted for the remaining other factors. In case of noise and shift work, and physical workload and shift work the risks diminished but remained significant. If the adjustment was made for white‐collar/blue‐collar status the CHD risks decreased considerably.
The risk patterns were quite similar after adjusting for age or treatment with gemfibrozil.
Joint effects of shift work, noise, and physical workload
Table 4 shows first the joint effects of shift work and noise. When followed up to the end of 1999, shift workers exposed to both continuous and impulse noise had RR = 1.59 (p = 0.04) compared with unexposed day workers, and shift workers with physical workload in the highest tertile had RR = 1.69 (p < 0.001) compared with day workers with no or lower exposure to physical workload. Similarly, those exposed to both continuous and impulse noise and physical workload in the third tertile had RR = 1.68 (p < 0.001) when compared with those unexposed to noise or greater physical workload. The trends in the patterns of risk with increasing follow up time (−1995 and −1999) mirrored those seen in table 3 in all exposure combinations—that is, the RRs associated with shift work decreased with increasing follow up time (more workers retired), while the RRs associated with physical workload or a combination of continuous and impulse noise increased with increasing follow up time.
Table 4 Joint effects of shift work (SW), noise, and physical workload (PW) on risk of coronary heart disease (CHD) risk among industrially employed men for different follow ups.
| n/CHD cases | Unadjusted | Age adjusted | SBP–TotC–Smo–BMI adjusted | Blue‐/white‐collar adjusted | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| RR | 95% CI | RR | 95% CI | RR | 95% CI | RR | 95% CI | |||
| Shift work + noise | ||||||||||
| Fu –95 | SW−, no | 746/72 | 1 | 1 | 1 | 1 | ||||
| SW−, continuous | 310/34 | 1.13 | (0.75–1.71) | 1.10 | (0.73–1.65) | 1.08 | (0.72–1.63) | 1.05 | (0.65–1.70) | |
| SW−, both | 84/14 | 1.78 | (1.01–3.16)* | 1.72 | (0.97–3.05) | 1.60 | (0.90–2.83) | 1.65 | (0.88–3.09) | |
| SW+, no | 194/27 | 1.47 | (0.94–2.28) | 1.45 | (0.93–2.26) | 1.31 | (0.84–2.04) | 1.40 | (0.87–2.24) | |
| SW+, continuous | 370/56 | 1.62 | (1.14–2.30)** | 1.65 | (1.16–2.34)** | 1.46 | (1.03–2.08)* | 1.50 | (0.97–2.32) | |
| SW+, both | 100/13 | 1.36 | (0.76–2.46) | 1.40 | (0.78–2.53) | 1.21 | (0.67–2.18) | 1.26 | (0.66–2.40) | |
| Fu –99 | SW−, no | 746/121 | 1 | 1 | 1 | 1 | ||||
| SW−, continuous | 310/52 | 1.04 | (0.75–1.43) | 0.99 | (0.72–1.37) | 1.00 | (0.72–1.39) | 0.88 | (0.60–1.28) | |
| SW−, both | 84/23 | 1.82 | (1.16–2.84)** | 1.74 | (1.11–2.72)* | 1.67 | (1.07–2.60)* | 1.54 | (0.95–2.50) | |
| SW+, no | 194/41 | 1.34 | (0.94–1.92) | 1.33 | (0.93–1.89) | 1.23 | (0.87–1.76) | 1.21 | (0.83–1.76) | |
| SW+, continuous | 370/82 | 1.43 | (1.08–1.89)* | 1.45 | (1.10–1.93)** | 1.31 | (0.99–1.74) | 1.21 | (0.86–1.70) | |
| SW+, both | 100/25 | 1.59 | (1.03–2.44)* | 1.65 | (1.07–2.54)* | 1.43 | (0.93–2.21) | 1.35 | (0.84–2.16) | |
| Shift work + physical workload† | ||||||||||
| Fu –95 | SW−, PW− | 748/35 | 1 | 1 | 1 | 1 | ||||
| SW−, PW+ | 392/23 | 1.20 | (0.83–1.73) | 1.17 | (0.81–1.70) | 1.11 | (0.77–1.60) | 1.08 | (0.69–1.68) | |
| SW+, PW− | 448/35 | 1.43 | (1.02–2.01)* | 1.45 | (1.04–2.03)* | 1.26 | (0.90–1.77) | 1.31 | (0.88–1.95) | |
| SW+, PW+ | 216/18 | 1.65 | (1.10–2.47)* | 1.67 | (1.12–2.51)* | 1.50 | (1.00–2.26)* | 1.49 | (0.92–2.39) | |
| Fu –99 | SW−, PW− | 748/117 | 1 | 1 | 1 | 1 | ||||
| SW−, PW+ | 392/79 | 1.32 | (0.99–1.76) | 1.29 | (0.97–1.71) | 1.25 | (0.94–1.67) | 1.18 | (0.83–1.67) | |
| SW+, PW− | 448/94 | 1.39 | (1.06–1.82)* | 1.41 | (1.08–1.85)* | 1.26 | (0.96–1.65) | 1.26 | (0.92–1.73) | |
| SW+, PW+ | 216/54 | 1.69 | (1.22–2.33)** | 1.72 | (1.25–2.38)*** | 1.58 | (1.14–2.18)** | 1.51 | (1.03–2.20)* | |
| Noise + physical workload† | ||||||||||
| Fu –95 | No, PW− | 820/39 | 1 | 1 | 1 | 1 | ||||
| Continuous, PW− | 376/31 | 1.43 | (1.01–2.02)* | 1.43 | (1.01–2.02)* | 1.30 | (0.92–1.83) | 1.29 | (0.84–2.00) | |
| No, PW+ | 120/9 | 1.36 | (0.80–2.32) | 1.34 | (0.78–2.28) | 1.24 | (0.72–2.11) | 1.23 | (0.68–2.23) | |
| Continuous, PW+ | 304/20 | 1.21 | (0.82–1.79) | 1.20 | (0.81–1.76) | 1.18 | (0.80–1.74) | 1.10 | (0.69–1.76) | |
| Both, PW+ | 184/12 | 1.48 | (0.96–2.29) | 1.48 | (0.96–2.28) | 1.33 | (0.86–2.06) | 1.34 | (0.81–2.23) | |
| Fu –99 | No, PW− | 820/134 | 1 | 1 | 1 | 1 | ||||
| Continuous, PW− | 376/77 | 1.29 | (0.98–1.71) | 1.29 | (0.98–1.71) | 1.19 | (0.90–1.58) | 1.11 | (0.79–1.57) | |
| No, PW+ | 120/28 | 1.50 | (1.00–2.25) | 1.47 | (0.98–2.21) | 1.40 | (0.93–2.11) | 1.29 | (0.82–2.03) | |
| Continuous, PW+ | 304/57 | 1.17 | (0.85–1.59) | 1.14 | (0.83–1.55) | 1.15 | (0.84–1.57) | 1.00 | (0.69–1.45) | |
| Both, PW+ | 184/48 | 1.68 | (1.21–2.33)** | 1.68 | (1.21–2.34)** | 1.54 | (1.10–2.14)* | 1.44 | (0.98–2.12) | |
The relative risks (RR) with 95% confidence intervals (95% CI) and p value were derived using Cox proportional hazards models with different covariates.
SBP, systolic blood pressure; TotC, total serum cholesterol; Smo, smoking; BMI, body mass index.
*p<0.05; **p<0.01; ***p<0.001.
†PW+ when product of prevalence (P) and level (L) is in 3 tertile.
The RRs of the joint effects of two exposures were mostly higher than the RRs of the separate exposures, but did not show any risk peaks. Adjustment for SBP, BMI, smoking, and total cholesterol decreased the RRs somewhat, indicating one possible lifestyle related pathway for the effect. Adjusting for white‐collar/blue‐collar status considerably decreased the risk estimates. Only the joint effects of shift work and physical workload (RR = 1.5, p = 0.03) and noise and physical workload (RR = 1.44, p = 0.06), remained significant or borderline significant in the follow up until 1999. The risk patterns were quite similar after adjusting for age or treatment with gemfibrozil.
The unadjusted RR of those exposed to all three risk factors was 2.21 (p = 0.01) until the end of 1991 and 1.87 (p < 0.001) until the end of 1999 compared with those unexposed to any of the factors.
Discussion
In our follow up study of industrially employed, middle aged males the common occupational exposures shift work, noise, and physical workload all emerged as significant risk factors of CHD. Their joint effects did not show any high risk peaks; the RR of those with all three risk factors present was about twofold compared with those with none of the factors. Shift work and continuous noise entailed an excess risk for CHD in the shortest follow up with only few retired workers but a reduced risk during the longer follow up times with increasing number of retired workers. For physical workload and impulse noise the trend was opposite: the CHD risk increased with increasing follow up time.
Possible pathways for the short term and long term effects of the risk factors
The finding that occupational risk factors may extend their effect into old age is not new. In a 25 year follow up of mortality in the Whitehall study,27 those in the lowest employment grade compared with the highest had RR 3.12 when not retired and 1.86 when retired. The impact of occupation thus remained considerable. As pointed out by Kasl, there are different steps or transitions in the development of CHD, and different mechanisms may influence these steps.28 It is thus to be expected that a long follow up may reveal different features of the putative risk factors.
Continuous noise involved increased CHD risk mainly during the shortest follow up, when most of the subjects were still employed, but if impulse noise and related workload were present, the excess CHD risk persisted long after the subjects had retired. In the study by Davies et al on CHD risk associated with exposure to noise, much higher relative risks were evident for subjects during their employed years.14 We may speculate that noise has an effect both on short term triggering mechanisms and on long term processes enhancing atherosclerosis. It has been suggested that noise may have direct physiological stress reactions via the hypothalamus‐pituitary‐adrenal axis with secretion of stress hormones followed by an increase of blood pressure and heart rate, strong risk factors of CHD in the long term.29 According to Morrell et al, noise may precipitate complications in susceptible subgroups, for example by triggering arrhythmias—an example of short term effects.30 Noise may also have adverse psychosocial effects, such as problems of sleeping, or stress related behavioural changes, such as alcohol consumption or smoking—all risk factors of CHD with both short and long term effects.13
The estimates of CHD risk due to shift work were higher in the short term than in the long term follow up, although the latter also remained steadily significant, suggesting the presence of both short term and long term risk factors—short term meaning here “during active working life” and long term, “during working life and retirement”. Like noise exposure, shift work also entails adverse psychosocial effects such as lack of social support and possible effort‐reward imbalance at work,31 but shift work can also induce CHD by behavioural and circadian rhythm/sleep related pathways.32 The shift workers in this study smoked more than the day workers, although they were physically more active than the day workers.33 In our earlier study,34 shift work seemed to trigger the effect of other, lifestyle related risk factors of CHD (especially smoking and obesity), and it could thus be hypothesised that after retirement, the disappearance of these behaviour related joint effects would also rapidly decrease the risk of CHD. We did not have information on the possible shift related differences in diet, which could be another mediating factor for the observed higher risk of CHD among shift workers. However, earlier studies among industrial workers indicate that even though 2‐ and 3‐shift work affects the circadian distribution of food intake, there are no significant differences according to type of shifts in the energy intake or in the quality of food.35 Finally, transfer from shift work to day work of subjects with symptoms related to CHD, causing exposure misclassification, could also explain the diminishing CHD risk among the shift workers.
The disruption of circadian rhythms may entail several pathways to CHD, some related to the increases in the frequency of sleep disturbances,30 some due to changes in other circadian rhythms. Many of these changes can trigger short term stress reactions and mechanisms increasing the clinical manifestations of CHD. Only six successive nights of time in bed restricted to four hours per night increased the activity of the sympathetic nervous system, increased evening cortisol concentrations, and decreased glucose tolerance similar to normal aging.36 The frequency of ventricular extrasystoles increased by 49% among shift workers during the first year of shift working in a prospective study of new shift workers, the increase being significantly higher than among the daytime workers.37 Experimental short term sleep deprivation also increased peripheral circulation of leukocytes, interleukins, and C‐reactive protein, the latter being a predictor of the risk of stroke and myocardial infarction.38,39 Recently, shift workers were found to have an increased death risk for stroke, the highest risk being already observed during the first five years after starting work.5
By physical workload the CHD risk became manifest mainly during the longer follow up, when most of the subjects had retired. It is noteworthy that those exposed to impulse noise were all also exposed to physical workload. This high correlation of the two exposures complicates the search for the pathways for their effect on CHD risk and it also complicates the ability of the study to separate their affects on CHD risk.
Is there an independent effect on CHD risk of any of the factors?
Firstly, it is questionable to apply the notion of “independent effect” in the present case with a triad of exposures with a high degree of simultaneous occurrence, and with partly similar pathways to disease. Secondly, in the case of noise and physical workload it would be questionable from a statistical point of view to adjust for one of them when studying the risk associated with the other, as they were highly correlated. Thirdly, as the factors of the triad occur mainly among blue‐collar workers, we adjust for them when adjusting for white‐collar/blue‐collar status. After these caveats we consider and compare the effects of the separate factors.
Main messages
The relative risks of CHD associated with shift work or continuous noise decreased with increasing follow up time (more workers retired).
The impulse noise was always combined with physical workload, and this combination entailed increased long term risk of CHD.
Those exposed to all factors of this triad had approximately a twice greater CHD risk than those exposed to none of them.
The information on exposure to noise or workload was obtained by linkage to the FINJEM job exposure matrix that gives job specific and not individual specific information on the exposition. The CHD risk due to noise or workload may thus be underestimated.
There has been some concern about the contradictory findings on the risk factor status of shift work. The 22 year follow up in the Copenhagen Male Study found no association between shift work and risk of CHD mortality, and their study clearly showed that the lack of difference in CHD risk was not due to the length of the study or aging of the study subjects.8 In our study the risk factor status of shift work is obvious, and the only clear difference in the study populations is that we have an industrial study cohort, while the subjects in the Copenhagen Male Study came from various occupational fields. In our study the risk estimates for shift work ranged from 1.62 to 1.22, depending on length of follow up, reference group, or factors adjusted for. In every case it was significant or borderline significant (p = 0.1). It thus seems that shift work even has an independent effect. The CHD risk due to continuous noise was present mainly together with shift work, while the risk due to impulse noise was significantly present in the longer follow up independent of shift work. However, as impulse noise occurred only together with physical workload, it is difficult to separate the effects of these two factors on CHD risk.
Limitations of the study
Our study deals with industrially employed males in late middle age, and most of them were retired at the end of the follow up. It is thus predominantly a study of late effects, and the risk estimates might be different for currently employed subjects, especially in the case of shift work and exposure to continuous noise, where the shorter follow up gave higher estimates of risk than the longer one.
A drawback is that we do not have any information on their job status during the follow up, either on promotions to day work, or retirement. However, because of the high mean age (40–55 years) at the start of the follow up, the cohort can be regarded as a selected group and early drop‐outs due to starting shift work could not occur in this study.
The information on exposure to noise or workload was not obtained through interview, as was the shift work status, but by linkage to the FINJEM job exposure matrix. The risks obtained through job specific information tend to be lower than those based on person specific information.27 The risks associated with exposures to noise or workload may thus be underestimated.
The focus of the present study was on the triad of hard occupational exposures, and although the lifestyle factors and principal risk factors for CHD were taken into account, psychosocial factors were not dealt with. The possibility of effect modification or confounding by such factors remains open.
Policy implications
Shift workers with high cardiovascular risk should be transferred to day work, if possible. Even a later cessation of shift work exposure seems to decrease the risk for CHD.
If workers cannot avoid impulse noise they should protect themselves from it.
Implications for research and prevention
The different trends in the long term risks of shift work, noise, and physical workload after the retirement of most of the workers indicate differences in the pathways from the exposures to CHD. To study the different mechanisms of shift work, noise, and physical workload in relation to cardiovascular health, further studies are needed not only with the regular follow up information of the health outcomes studied, but also exposure, risk factors, and moderators of cardiovascular health.
A recent study of retired monozygotic twins discordant on exposure to night work showed that retired night workers still had an increased risk for poor subjective health and disturbed sleep.40 We are aware of no earlier studies indicating that the increased risk for CHD due to shift work is diminished after cessation of the exposure with retirement from work. Since this was not the case in relation to exposure to physical workload and impulse noise, the observation cannot be regarded as self‐evident. The diminishing risk after leaving shift work seems to support the recommendations originally given by the ILO Night Work Convention 1990,41 that shift workers with high cardiovascular risk should be transferred to day work, if possible. As shown by this study, even a later cessation of shift work exposure seems to decrease the risk for CHD.
Acknowledgements
We thank Virginia Mattila, Language Centre, University of Tampere, for revision of the English language in the manuscript.
Abbreviations
BMI - body mass index
CHD - coronary heart disease
HHS - Helsinki Heart Study
RR - relative risk
Footnotes
Funding: this study was supported by the Kalle Kaihari Heart Research Fund
Competing interests: none declared
References
- 1.European Foundation for the Improvement of Living and Working Conditions Third European Survey on Working Conditions 2000. Luxembourg: Office for Official Publications of the European Communities, 2001
- 2.Lehto A ‐ M, Sutela H.Uhkia ja mahdollisuuksia. Työolotutkimusten tuloksia 1977–2003. Helsinki: Tilastokeskus, 2004 (in Finnish),
- 3.Costa G. Shift work and occupational medicine: an overview. Occup Med (Lond) 20035383–88. [DOI] [PubMed] [Google Scholar]
- 4.Knutsson A, Hammar N, Karlsson B. Shift workers' mortality scrutinized. Chronobiol Int 2004211049–1053. [DOI] [PubMed] [Google Scholar]
- 5.Karlsson B, Alfredsson L, Knutsson A.et al Total mortality and cause‐specific mortality of Swedish shift‐ and dayworkers in the pulp and paper industry in 1952–2001. Scand J Work Environ Health 20053130–35. [DOI] [PubMed] [Google Scholar]
- 6.Härmä M. Individual differences in tolerance to shiftwork: a review. Ergonomics 199336101–109. [DOI] [PubMed] [Google Scholar]
- 7.Boggild H, Knutsson A. Shift work, risk factors and cardiovascular disease. Scand J Work Environ Health 19992585–99. [DOI] [PubMed] [Google Scholar]
- 8.Boggild H, Suadicani P, Hein H O.et al Shift work, social class, and ischaemic heart disease in middle aged and elderly men; a 22 year follow up in the Copenhagen Male Study. Occup Environ Med 199956640–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Boggild H, Burr H, Tuchsen F.et al Work environment of Danish shift and day workers. Scand J Work Environ Health 20012797–105. [DOI] [PubMed] [Google Scholar]
- 10.Steenland K, Fine L, Belkic K.et al Research findings linking workplace factors to CVD outcomes. Occup Med 2000157–68. [PubMed] [Google Scholar]
- 11.Kauppinen T, Hanhela R, Heikkilä P.et alTyö ja terveys Suomessa 2003. Helsinki: Työterveyslaitos, 2004 (in Finnish),
- 12.Kock S, Andersen T, Kolstad H A.et al Surveillance of noise exposure in the Danish workplace: a baseline survey. Occup Environ Med 200461838–843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van Kempen E E, Kruize H, Boshuizen H C.et al The association between noise exposure and blood pressure and ischemic heart disease: a meta‐analysis. Environ Health Perspect 2002110307–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Davies H W, Teschke K, Kennedy S M.et al Occupational exposure to noise and mortality from acute myocardial infarction. Epidemiology 20051625–32. [DOI] [PubMed] [Google Scholar]
- 15.Virkkunen H, Kauppinen T, Tenkanen L. Long‐term effect of occupational noise on the risk of coronary heart disease. Scand J Work Environ Health 200531291–299. [DOI] [PubMed] [Google Scholar]
- 16.Lee I M, Paffenbarger R S, Jr, Hennekens C H. Physical activity, physical fitness and longevity. Aging (Milano) 199792–11. [DOI] [PubMed] [Google Scholar]
- 17.Barengo N C, Hu G, Lakka T A.et al Low physical activity as a predictor for total and cardiovascular disease mortality in middle‐aged men and women in Finland. Eur Heart J 2004252204–2211. [DOI] [PubMed] [Google Scholar]
- 18.Kristal‐Boneh E, Harari G, Melamed S.et al Association of physical activity at work with mortality in Israeli industrial employees: the CORDIS study. J Occup Environ Med 200042127–135. [DOI] [PubMed] [Google Scholar]
- 19.Virtanen S V, Notkola V. Socioeconomic inequalities in cardiovascular mortality and the role of work: a register study of Finnish men. Int J Epidemiol 200231614–621. [DOI] [PubMed] [Google Scholar]
- 20.US Department of Health and Human Services The health consequences of smoking: cardiovascular disease. A report of the Surgeon General. Rockville, MD: Public Health Service, Office on Smoking and Health, 1983291–321.
- 21.Frick M H, Elo O, Haapa K.et al The Helsinki Heart Study: primary prevention trial with gemfibrozil middle‐aged men with dyslipidemia: safety of treatment, changes in risk factors, and incidence of coronary heart disease. N Engl J Med 19873171237–1245. [DOI] [PubMed] [Google Scholar]
- 22.Finnish Centre for Pensions, The Social Insurance Institution Statistical yearbook of pensioners in Finland 1996. Finland: Helsinki, 1997
- 23.Palomäki P, Miettinen H, Mustaniemi H.et al Diagnosis of acute myocardial infarction by MONICA and FINMONICA diagnostic criteria in comparison with hospital discharge diagnosis. J Clin Epidemiol 199447659–666. [DOI] [PubMed] [Google Scholar]
- 24.Pietilä K, Tenkanen L, Mänttäri M.et al How to define coronary heart disease in register‐based follow up studies: experience from the Helsinki Heart Study. Ann Med 199729253–259. [DOI] [PubMed] [Google Scholar]
- 25.Central Statistical Office of Finland Classification of occupations 1980. Handbook No. 14. Helsinki: Central Statistical Office of Finland, 1981
- 26.Kauppinen T, Toikkanen J, Pukkala E. From cross‐tabulations to multipurpose exposure information systems: a new job‐exposure matrix. Am J Ind Med 199833409–417. [DOI] [PubMed] [Google Scholar]
- 27.Marmot M G, Bosma H, Hemingway H.et al Contribution of job control and other risk factors to social variations in coronary heart disease incidence. Lancet 1997350235–239. [DOI] [PubMed] [Google Scholar]
- 28.Kasl S V. The influence of the work environment on cardiovascular health: a historical, conceptual, and methodological perspective. J Occup Health Psychol 1996142–56. [DOI] [PubMed] [Google Scholar]
- 29.Stansfeld S, Haines M, Brown B. Noise and health in the urban environment. Rev Environ Health 20001543–82. [DOI] [PubMed] [Google Scholar]
- 30.Morrell S, Taylor R, Lyle D. A review of health effects of aircraft noise. Aust N Z J Public Health 199721221–236. [DOI] [PubMed] [Google Scholar]
- 31.Peter R, Alfredsson L, Knutsson A.et al Does a stressful psychosocial work environment mediate the effects of shift work on cardiovascular risk factors? Scand J Work Environ Health 199925376–381. [DOI] [PubMed] [Google Scholar]
- 32.Knutsson A, Boggild H. Shiftwork and cardiovascular disease: review of disease mechanisms. Rev Environ Health 200015359–372. [DOI] [PubMed] [Google Scholar]
- 33.Harma M, Tenkanen L, Sjoblom T.et al Combined effects of shift work and life‐style on the prevalence of insomnia, sleep deprivation and daytime sleepiness. Scand J Work Environ Health 199824300–307. [DOI] [PubMed] [Google Scholar]
- 34.Tenkanen L, Sjoblom T, Harma M. Joint effect of shift work and adverse life‐style factors on the risk of coronary heart disease. Scand J Work Environ Health 199824351–357. [DOI] [PubMed] [Google Scholar]
- 35.Lennernäs M, Hambraeus L, Åketrstedt T. Shift related dietary intake in day and shift workers. Appetite 199525253–265. [DOI] [PubMed] [Google Scholar]
- 36.Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet 19993541435–1439. [DOI] [PubMed] [Google Scholar]
- 37.van Amelsvoort L, Schouten E, Maan A.et al Changes in frequency of premature complexes and heart rate variability related to shift work. Occup Environ Med 200158678–681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Meier‐Ewert H K, Rdker P M, Rifai N.et al Effect of sleep loss on C‐reactive protein, and inflammatory marker of cardiovascular risk. J Am Coll Cardiol 200443678–683. [DOI] [PubMed] [Google Scholar]
- 39.Danesh J, Whincup P, Walker M.et al Low grade inflammation and coronary heart disease: prospective study and updated meta‐analyses. BMJ 2000321199–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ingre M, Åkekrstedt T. Effect of accumulated night work during the working lifetime, on subjective health and sleep in monozygotic twons. J Sleep Res 20041345–48. [DOI] [PubMed] [Google Scholar]
- 41.ILO Night work contention. Geneva: ILO, 1990171