Abstract
Background
The existence of health inequalities between least and most socially deprived areas is now well established.
Aim
To use Quality and Outcomes Framework (QOF) indicators to explore the characteristics of primary care in deprived communities.
Design of study
Two-year study.
Setting
Primary care in England.
Method
QOF data were obtained for each practice in England in 2004–2005 and 2005–2006 and linked with census derived social deprivation data (Index of Multiple Deprivation scores 2004), national urbanicity scores and a database of practice characteristics. Data were available for 8480 practices in 2004–2005 and 8264 practices in 2005–2006. Comparisons were made between practices in the least and most deprived quintiles.
Results
The difference in mean total QOF score between practices in least and most deprived quintiles was 64.5 points in 2004–2005 (mean score, all practices, 959.9) and 30.4 in 2005–2006 (mean, 1012.6). In 2005–2006, the QOF indicators displaying the largest differences between least and most deprived quintiles were: recall of patients not attending appointments for injectable neuroleptics (79 versus 58%, respectively), practices opening ≥45 hours/week (90 versus 74%), practices conducting ≥12 significant event audits in previous 3 years (93 versus 81 %), proportion of epileptics who were seizure free ≥12 months (77 versus 65%) and proportion of patients taking lithium with serum lithium within therapeutic range (90 versus 78%). Geographical differences were less in group and training practices.
Conclusions
Overall differences between primary care quality indicators in deprived and prosperous communities were small. However, shortfalls in specific indicators, both clinical and non-clinical, suggest that focused interventions could be applied to improve the quality of primary care in deprived areas.
Keywords: primary care, quality indicators, social deprivation
INTRODUCTION
International studies of primary care have provided evidence that more prosperous communities within a country experience higher quality care.1 Publicly-funded primary healthcare systems, which are free at the point of use, are likely to minimise the social gradient in the quality of care, when compared to insurance-based systems.2 Nevertheless, inequalities in the quality of care also remain in publicly-funded systems, especially when faced by high levels of disease prevalence and other forms of deprivation. Failure to align the delivery of health care to the needs of the community may result in the classic mismatch described by Tudor Hart in which the most socially deprived communities receive the poorest quality healthcare services, and yet have the highest prevalence of chronic disease.3
The wealth of descriptive information now available for primary care in the UK under the Quality and Outcomes Framework (QOF) is unique in international terms.4 Using QOF data, the aim of the study was to examine the extent to which the performance of primary care varies by deprived area, whether this is changing and what particular aspects of care are compromised. Although QOF data have already been used to demonstrate the association between social deprivation and reduced quality of primary care in general terms,5 no study has yet reported information about individual QOF indicators and longitudinal QOF data.
How this fits in
Shortcomings in the delivery of health care in deprived areas have been well documented. Differences in total QOF scores between practices in the most and the least deprived areas were small in the first year of QOF and smaller still in the second year. Larger shortfalls in the achievement of a few specific QOF indicators in deprived areas have been identified; improvement in these specific indicators may be achievable by focused interventions.
METHOD
QOF data were obtained for each practice in England in the years 2004–2005 and 2005–2006.6 QOF data combine practice-based variables (categorical variables describing whether or not the practices achieve a desired standard) and patient-based variables (continuous variables describing the proportion of patients achieving a given quality standard). Variables within the QOF dataset are grouped into several domains: clinical (76 indicators related to the clinical management of 11 chronic diseases); organisational (56 indicators covering managerial criteria); patient experience (four indicators related to consultation length and a patient survey); additional services (10 indicators relating to services offered by the practice such as cervical smears, child health surveillance and maternity care); and an access domain (a single indicator relating to access to the GPs and nurses).
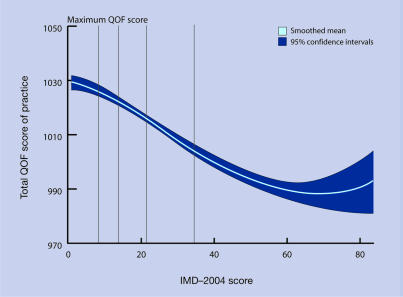
Figure 1.
Relationship between total Quality and Outcomes Framework (QOF) 2005–2006 scores and Index of Multiple Deprivation (IMD-2004) scores. Note: vertical lines represent cut-off points for each quintile of deprivation
Index of Multiple Deprivation scores (IMD–2004) were obtained for all lower layer Super Output Areas (SOAs) in England.7 SOAs are geographical ‘socially homogenous’ areas with a population of around 1500 and arguably, present a more focused estimate of social variables than politically defined geographical units such as local government wards. The Office of National Statistics publishes postcode-based, 9-point urbanicity ratings ranging from more densely populated areas to rural areas.8 Because each SOA consists of many postcodes, an urbanicity rating was derived for each SOA based on the least urban rating of its component postcodes. Practice characteristics were provided by the Manchester Primary Care Research and Development Centre, University of Manchester.
Practices were excluded if they had a list size of under 750 patients or under 500 patients per full-time equivalent (fte) GP, on the assumption that these practices were newly formed or about to be closed.
A longitudinal database of all practices in England was constructed, matching practice data with an index of multiple deprivation [IMD]–2004 data based on the practice postcode. QOF and demographic data were available for 8515 practices in 2004–2005 and 8264 practices in 2005–2006. Urbanicity ratings were available for 8480 of these practices in 2004–2005 and for 8264 practices in 2005–2006. Quintiles of deprivation were derived from the IMD–2004 scores for all SOAs in England and practices located in the most and least deprived SOA quintiles were compared.
The process of exception reporting may alter the interpretation of QOF data.9,10 This is the process by which patients are excluded from the chronic disease indicators for a variety of reasons such as failure to attend a clinic appointment in spite of three reminders, or sub-optimal treatment targets in spite of the patient being prescribed maximum tolerated therapy. Discrepancies (shortfalls) between the numbers of patients submitted as eligible for each indicator and the numbers on the specific disease register were assumed to have arisen because the practice had exception reported those patients. Even though practices may have used the process of exception reporting, the QOF dataset only allows the calculation of an exception report rate for 30 of the 76 clinical indicators.10 The data were analysed for each of the chronic disease indicators using both raw data and, where possible, data adjusted for exception reporting following the method of Doran et al.10
Data analysis methods
Univariate associations between variables were explored using parametric tests. Given the size of the database containing information on more than 8000 practices, the central limit theorem ensures that parametric tests are valid. Therefore, where appropriate, t-tests were used to compare the mean QOF scores and its components. Differences between most and least deprived quintiles were compared using means and 95% confidence intervals (CIs) of the mean. Multivariate associations were explored using linear or logistic regression techniques as appropriate.
All data refer to the year 2005–2006, unless otherwise stated. Statistical significance was taken at P = 0.05. As this is essentially an exploratory investigation of a new research area, no adjustment was made for multiple testing.11
Postgraduate training practices and group practices are known to perform better at QOF-related activity.12 To determine the extent to which these practice characteristics may be important determinants of poorer performance in deprived areas, the QOF scores of practices in the least and most deprived quintiles were compared, only for training and group practices.
RESULTS
Most and least deprived quintiles
IMD–2004 scores for the 32 482 SOAs in England range from 0.59 to 86.36. SOAs with an IMD–2004 score >33.53 represent the most deprived geographical quintile in England; SOAs with scores below 9.01 represent the least deprived quintile. In 2005–2006, there were 2373 general practices located in the most deprived quintile of SOAs and 1228 practices in the least deprived quintile of SOAs.
Characteristics of practices and social deprivation
The total registered population of practices in the least deprived area quintile was 9 140 027 compared to 12 967 781 in the most deprived quintile. About one-third more fte GPs were located in the most deprived quintile and their list size was about 10% larger than their counterparts in the least deprived quintile (Table 1). Single-handed and non-training practices were both more commonly represented in the most deprived quintile.
Table 1.
Characteristics of general practices in lowest and highest deprivation quintiles, 2005–2006.
| Least deprived quintile | Most deprived quintile | |
|---|---|---|
| Number of practices | 1228 | 2373 |
| Fte GPs | 4660 | 6342 |
| List size per fte GP | 2063 | 2284 |
| Single-handed practice | 13.4% | 35.1% |
| Training practice | 38.2% | 19.1% |
Fte = full-time equivalent.
QOF scores and social deprivation
The mean total QOF score in 2005–2006 was 1012.6 (median 1035.0), a 53-point improvement on the 2004–2005 figure of 959.9 (median 999.3). In 2004–2005, the difference in total QOF score between top and bottom quintiles was 64.5 points (95% CI = 57.6 to 71.3) but by 2005–2006 this gap had narrowed to 30.4 (95% CI = 26.4 to 34.4).
To examine whether the narrowing gap in QOF scores between high and low deprivation areas was primarily due to improvements in the achievement of practices in deprived areas or whether it arose simply because all lower scoring practices were catching up with higher achieving practices, the ability of practices below a given threshold in the first year of QOF were considered to improve performance in the following year. Thus, of those practices failing to achieve 750 points in 2004–2005, 77% had met this target in 2005–2006, irrespective of deprivation quintile, as confirmed by logistic regression. However, where the threshold was 1040 points, practices in deprived areas did less well. The odds of a practice newly achieving 1040 QOF points were more than halved if the practice was located in the highest deprivation quintile (odds ratio [OR]= 0.47) or if it was single-handed (OR = 0.48), whereas the odds for a training practice were more than doubled (OR = 2.47). Similar ORs were obtained by setting thresholds at 1000, 1020 and 1050 QOF points (results not presented).
Individual QOF indicators and social deprivation
Total 2005–2006 QOF scores and achievements for each of the QOF domains for practices located in the least and most deprived quintiles are presented in Table 2. These indices are further broken down in Tables 3 and 4, which show respectively practice and patient-based (clinical) variables for which there was the largest difference between areas of deprivation. All indicators for which there was a difference of at least 5% between the achievement of practices in least and most deprived quintiles are displayed. In all, this level of achievement difference between least and most deprived quintiles was observed for 22 out of the 147, 2005–2006 QOF indicators.
Table 2.
Differences between least and most deprived quintiles in mean QOF scores: clinical and non-clinical domains, 2005–2006.
| QOF points (%) | |||
|---|---|---|---|
| QOF domain | Least deprived quintile | Most deprived quintile | Difference between quintiles |
| Total QOF score (maximum = 1050) | 1026.9 (97.8) | 996.5 (94.9) | 30.4 (2.9) |
| Total disease domain (maximum = 550) | 541.1 (98.4) | 528.7 (96.1) | 12.4 (2.2) |
| Organisation domain (maximum = 184) | 175.6 (95.5) | 168.7 (91.7) | 6.9 (3.8) |
| Patient experience domain (maximum = 100) | 98.2 (98.2) | 95.2 (95.3) | 2.9 (2.9) |
| Additional services domain (maximum = 36) | 35.6 (98.9) | 34.3 (95.4) | 1.3 (3.6) |
| Access bonus (maximum = 50) | 49.5 (99.0) | 48.1 (96.2) | 1.4 (2.9) |
QOF = Quality and Outcomes Framework.
Table 3.
Differences between least and most deprived quintiles: proportion of practices achieving 2005–2006 practice based QOF indicators.
| QOF indicator | Least deprived quintile, % | Most deprived quintile, % | Difference, % (95% CI) |
|---|---|---|---|
| Medicines 7: identify and follow up SMI patients who do not attend their injectable neuroleptic appointment | 78.5 | 58.0 | 20.5 (17.5 to 23.6) |
| Information 7: surgery open ≥45 hours/week | 90.3 | 74.1 | 16.2 (13.8 to 18.6) |
| Education 7: practice has conducted ≥12 significant event audits in last 3 years | 93.2 | 80.7 | 12.5 (10.3 to 14.6) |
| Patient experience 4: practice has discussed patient survey with patient group or non-executive director of PCT; changes proposed and some evidence that changes enacted | 95.2 | 87.6 | 7.6 (5.8 to 9.4) |
| Records 18: case notes have clinical summary in ≥80% | 80.6 | 73.1 | 7.6 (4.7 to 10.4) |
| Records 15: case notes have clinical summary in ≥60% | 92.0 | 85.6 | 6.4 (4.3 to 8.5) |
| Child health surveillance 1: practice offers child health surveillance checks | 98.0 | 92.0 | 5.9 (4.6 to 7.3) |
| Education 8: practice nurses have personal learning plan | 96.1 | 90.2 | 5.9 (4.3 to 7.5) |
| Education 2: practice has conducted ≥6 significant event audits in last 3 years | 97.4 | 91.9 | 5.5 (4.1 to 6.9) |
| Education 3: all practice nurses have annual appraisal | 96.7 | 91.5 | 5.2 (3.7 to 6.7) |
| Medicines 9: medication review in last 15 months for all patients on repeat medication | 95.4 | 90.4 | 5.1 (3.4 to 6.7) |
PCT = primary care trust. QOF = Quality and Outcomes Framework. SMI = severe mental illness.
Table 4.
Differences between least and most deprived quintiles: proportion of patients achieving 2005–2006 clinical QOF indicators.
| QOF indicator | Least deprived quintile, % | Most deprived quintile, % | Difference, % (95% CI) |
|---|---|---|---|
| Epilepsy 4: seizure free for ≥12 months | 77.3 | 65.1 | 12.2 (11.1 to 13.3) |
| Mental health 5: on lithium and serum level in therapeutic range | 90.1 | 78.0 | 12.0 (10.3 to 13.8) |
| Mental health 3: on lithium and serum level checked | 94.0 | 84.4 | 9.6 (7.9 to 11.2) |
| Mental health 4: on lithium and creatinine level and thyroid function checked | 94.3 | 85.4 | 8.9 (7.3 to 10.5) |
| CHD 2: % new angina diagnosis confirmed by exercise test | 92.7 | 85.2 | 7.5 (6.3 to 8.8) |
| LVD 2: % left ventricular disease patients with diagnosis confirmed by ECHO test | 92.9 | 85.6 | 7.3 (5.7 to 8.9) |
| COPD 2: % new cases with diagnosis confirmed by spirometry | 91.3 | 84.5 | 6.8 (5.6 to 8.0) |
| COPD 6: FEV1.0 in all patients diagnosed with COPD | 86.7 | 80.7 | 6.0 (4.8 to 7.1) |
| Stroke 2: % new cases referred for confirmation of diagnosis by CT/MRI scan | 88.4 | 82.5 | 5.9 (4.1 to 7.0) |
| COPD 3: % all cases who have had spirometry testing | 92.2 | 86.6 | 5.6 (4.6 to 6.6) |
| Cervical screening 1: % women aged 25–65 years who have had a smear in the last 5 years | 85.0 | 79.5 | 5.5 (4.5 to 7.3) |
CHD = coronary heart disease. COPD = chronic obstructive pulmonary disease. CT/MRI = computerised axial/tomography/magnetic resonance imaging. ECHO = echocardiogram. FEV1 = forced expiratory volume in 1 second. LVD = left ventricular disease. QOF = Quality and Outcomes Framework.
The reported achievement of each clinical indicator increased following adjustment for exception reporting but for some indicators, the gap between least and most deprived quintiles widened such that three new indicators exceeded the 5% difference and would have appeared in Table 4. These indicators were: chronic obstructive pulmonary disease9 (% given flu vaccination) for which the adjusted difference became 5.5%; diabetes11 (% with record of neuropathy testing) with an adjusted difference of 5.3%; and diabetes8 (% with HbA1c ≤10 mmol/L) with an adjusted difference of 5.0%.
Finally, the differences between first year (2004–2005) QOF achievements in least and most deprived quintiles were obtained. A total of 50 QOF indicators differed by more than 5%, including each one of the indicators appearing in Tables 3 and 4. In other words, for the remaining 28 indicators, the gap between quintiles narrowed to less than 5% by the end of the second year of the QOF. Full results are available from the authors.
The effect of urbanicity
The most urban area of the 9-point urbanicity rating applies to SOAs within urban settlements with a population of 10 000 or more8 and in 2005–2006 was found to contain 83.3% of general practices (and 81.9% of fte GPs) in England. Mean total 2005–2006 QOF scores were 18.5 points lower (95% CI = 15.9 to 21.2) in these urban practices than in rural or less urban practices. Deprivation compounded the effect of urbanicity: for those practices in the most deprived quintile, the mean total QOF score in non-urban practices was 1022.2 (95% CI = 1011.9 to 1032.4) but in urban practices was 995.9 (95% CI = 992.8 to 999.0), a difference of 26 points. The effect of urbanicity as a predictor of total QOF score was not explained by social deprivation alone: together, the two variables explained 4.0% of the variation in the total QOF score, compared to 3.7% for social deprivation alone and 1.2% for urbanicity alone (standardised coefficients, β, for IMD score = −0.18; for urbanicity = −0.06). The total QOF score was not normally distributed and, therefore, the regression equation was re-run using a logit transformation to normalise the dependent variable, resulting in a slightly higher predictive power of the model (5.6%), but with similar regression coefficients (−0.21 and −0.07, respectively).
The effect of group practices and training practices
Group and postgraduate training practices were found to perform well in deprived areas, on the basis of QOF scores. By excluding all single-handed practices (n = 2035) from the analysis, the difference in the mean total 2005–2006 QOF score between practices in most and least deprived quintiles diminished from 30.4 to 21.2 points (1032.0 and 1010.8, respectively). When non-training practices (n = 6030) were excluded from the analysis, the difference between practices in both areas was 10.9 points (1041.1 and 1030.2, respectively).
Training practices appear to achieve higher QOF scores in more deprived areas. This could be a function of their training status or have arisen because training practices tend to be larger group practices. Total scores were therefore calculated according to practice size and training status. Regardless of size, training practices achieved higher QOF scores than non-training practices in deprived areas. For example, training practices located in the most deprived quintile with four or more fte GPs achieved a mean total QOF score of 1032.8 (95% CI = 1029.9 to 1035.7) whereas the mean score of their non-training counterparts was 1020.5 (95% CI = 016.9 to 1024.1).
The effect of group and training practice status was further explored for individual QOF indicators. Table 5 displays the five QOF indicators which differ the most between most and least deprived areas. For each indicator, the difference was re-analysed according to practice status. Although differences were smaller, group and training practices still performed less well in the most deprived areas.
Table 5.
Differences between least and most deprived quintiles: performance of training and group practices, selected QOF indicators, 2005–2006.
| Difference between quintiles, % | |||
|---|---|---|---|
| QOF indicator | All practices | Group practices | Training practices |
| Medicines 7: identify and follow up SMI patients who do not attend their injectable neuroleptic appointment | 20.5 | 16.8 | 11.9 |
| Information 7: surgery open ≥45 hours/week | 16.2 | 11.0 | 9.2 |
| Education 7: practice has conducted ≥12 significant event audits in last 3 years | 12.5 | 9.4 | 4.2 |
| Epilepsy 4: seizure free for ≥12 months | 12.2 | 11.5 | 10.2 |
| Mental health 5: on lithium and serum level in therapeutic range | 12.0 | 7.4 | 3.3 |
QOF = Quality and Outcomes Framework. SMI = severe mental illness.
DISCUSSION
Summary of main findings
While there are differences in the achievement of objective performance measures of primary care in the UK across areas of social deprivation, overall the differences are not large and seem to be closing. In 2005–2006, practices in the most deprived quintile of SOAs could expect to achieve 30 QOF points less (out of a total of 1050) than practices in the most affluent quintile. This achievement may partly be accounted for by the relatively good distribution of full-time equivalent GPs across areas of deprivation in the UK, albeit with large list sizes, and, in part, by the effect of the performance incentives embodied in the system of rewarding GPs for the quality of care they deliver. Of course, the role of financial incentives has a controversial history in primary care, and there is evidence that many performance improvements of primary care pre-dated the introduction of the QOF in 2004.13 However, the spur to achieve higher QOF scores may not have solely been financial and other factors may have motivated practices, such as the perceived ‘standing’ of high scoring practices.
The relatively small difference in total QOF achievements between geographical areas of deprivation, however, masks some larger differences in the achievement of individual indicators between practices. In particular, differences of over 10% were found for three of the practice-based indicators: practices which recalled patients with a psychotic illness failing to attend their appointment for a depot injection; practices open for at least 45 hours per week; and practices which conducted ≤12 significant event audits. Relatively poor achievement rates for these three practice-based indicators characterised practices in the most deprived quintile.
The greatest shortfall (over 10%) in clinical achievement between patients registered at practices in the least and most deprived quintiles was found for the achievement of fit control in epileptics and the monitoring and control of lithium levels in patients on the Serious Mental Illness register.
Strengths and limitations of the study
The association between practices and deprivation was examined by identifying the practice's postcode within IMD deprivation scores. This assumes that the community that the practice serves and the practice buildings themselves are located in the same geographical area. The interpretation of findings at an individual level when data was obtained at practice level may lead to the ‘ecological fallacy’14 and it is clear from this data that general practices are not evenly distributed throughout the country, being more likely to be sited in areas of higher deprivation. Although this data apply to practices located in the most deprived areas rather than to patients living in the most deprived areas, the social gradient in practice performance is likely to apply at a patient level since practice postcode-linked IMD scores have been found to provide a valid proxy for patient-level deprivation scores.15
QOF data may reflect true achievement within a practice or may underestimate achievement (by under-recording of coded data) or overestimate achievement (for example, by high levels of exception reporting). Differential reporting rates may account for some of the differences in observed QOF scores and these findings could represent less well organised data-collection systems or a lower value placed on the importance of gathering QOF data in deprived areas.16 However, little evidence that differences between least and most deprived areas may have been disguised by higher exception reporting rates in poorer areas was found,9 although adjustment for exception reporting did result in three more clinical indicators appearing in this list of indicators for which there was the greatest shortfall in deprived areas. Primary care trusts (PCTs) monitor the reporting of QOF indicators and may interpret satisfactory achievement in different ways. Some indicators are more open to interpretation than others and the indicator describing recall of patients missing their depot neuroleptic medication is an example. Achievement was disallowed by some PCTs if the community psychiatric nurse, rather than the practice nurse, ran the depot clinic. Differential interpretation of some indicators may have contributed to these findings.
The urbanicity data were insufficiently detailed to enable identification of practices in the most densely populated areas of inner cities. It is possible therefore, that larger inequalities in primary care in inner city areas were not detected by this study.
Comparison with existing literature
The existence of health inequalities between least and most socially deprived areas is now well established.17–20 The availability of QOF data enables a much more precise categorisation of primary care inequalities based on an analysis of 147 indicators. The type of practices located in more deprived areas have already been defined21 and just as in the current study, it is known that there are more single-handed GPs, larger practice list sizes per GP and fewer training practices. These structural differences between practices may account for some differences in the achievement of primary care and these findings, particularly the better performance of training practices, suggest that certain types of practice are able to offer a higher standard of care in deprived areas. Characteristics of a socially-deprived population may also account for some of the differences. Patients living in deprived communities may be less likely to engage with long-term management of chronic illnesses and in preventative health care and also less responsive to written invitations to attend appointments.22
Most of the shortfalls in specific performance indicators of primary care have not been described before. Shortfalls in the provision of primary care assume a greater significance when the population needs are correspondingly high and each of the clinical indicators identified in this study relate directly to diseases known to have a higher prevalence in deprived areas.
The finding of high proportions of patients with poorly controlled epilepsy was unexpected. There are currently no reports of increased fit frequency in epileptic patients in deprived areas, although new cases of epilepsy are known to be more common in deprived areas.23 A number of factors could have contributed to this finding such as poor medication adherence, poor access to primary care, sporadic monitoring of serum levels of anti-epileptic medication, difficulties attending specialist neurology centres, or increased comorbidity, particularly with alcohol-related problems.
These findings emphasise the importance of individual indicators as markers of the performance of primary care. Rather than examining global performance in terms of total QOF scores, some of the differences between types of practice only emerge on analysis of individual indicators or domains. For example, lower total QOF scores in smaller practices were found to be attributable to lower attainment of organisational domain indicators whereas clinical care, as measured by the clinical indicators, was equally well delivered by small practices.24
Implications for future research and clinical practice
While the overall findings are reassuring, several of the specific factors contributing to health inequalities identified in this study are readily amenable to improvement. Firstly, the mismatch between higher morbidity in more deprived areas and restricted opening hours of general practices may contribute to health inequalities and policy could be directed at promoting longer opening hours in poorer areas. Smaller practices in particular may find it hard to meet the requirements of longer opening hours. Secondly, training practices were found to perform consistently better in deprived areas than their non-training counterparts and the promotion of training practices in deprived areas, where they are currently under-represented, may translate into improved quality of care for the local communities. Thirdly, there was a pattern of lack of referral for investigations in more deprived areas which may indicate lack of direct access to secondary care services (for example, for exercise electrocardiograms or echocardiograms) or lack of practice-based equipment (such as spirometry). Smaller practices, which typify deprived areas, may not have found it cost-effective to purchase expensive diagnostic equipment. Addressing these obstacles should be possible if health services were able to offer specific support for practices. Finally, specific shortfalls could be addressed such as recall systems for patients on anti-psychotic medication, low cervical smear rates and lack of child health surveillance (even though these latter two indicators have been incentivised for GPs since 1990, long before the beginning of QOF, and yet the social divide remains).
Prior to the introduction of the QOF, GPs in England received a deprivation payment based on the deprivation score of each registered patient,25 but no deprivation component has been included in the QOF payments. Given the relatively small overall deficit in QOF score, this policy seems justified even though the funding differences may be larger than implied by the current study, once higher disease prevalence is taken into account.26 Instead, available financial support to reduce health inequalities could be targeted at the specific indicators identified in this study.
Broadly speaking, there are likely to be two causes of lower performance of primary care in more deprived areas: practice and population factors. Controlling for some practice factors (group and training practices) accounted for two-thirds of the difference, narrowing the gap between least and most deprived quintiles to just 11 QOF points. The remainder of the difference is probably a mix of other practice factors and a patient effect. In other words, well-organised primary care can largely compensate for substantial social disadvantage.
Shortcomings in the effectiveness of primary care to respond to the burden of morbidity in deprived communities have been well documented in the past.27 Yet this study suggests that there have been considerable improvements in primary care in deprived populations over recent years, although there is still room for improvement in specific areas, as described. Quality of care, however, can only partly compensate for the greater health needs in deprived areas that are often refractory to change, so delivering more effective health care remains the key priority as well as addressing the more fundamental causes of deprivation itself.
Acknowledgments
We would like to acknowledge the roles of Andrew Wagner (Manchester Primary Care Research and Development Centre, University of Manchester) and Robin Smith (The Informatics Collaboratory Of the Social Sciences (ICOSS), University of Sheffield).
Funding body
Mark Ashworth has been part funded by the South Thames Research Network (STaRNet), London
Ethics committee
Guy's Research Ethics Committee (Chairman's action, 8/2/06)
Competing interests
The authors have stated that there are none
REFERENCES
- 1.Seddon ME, Marshall MN, Campbell SM, Roland MO. Systematic review of studies of quality of clinical care in general practice in the UK, Australia and New Zealand. Qual Health Care. 2001;10:152–158. doi: 10.1136/qhc.0100152... [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gervas J, Perez Fernandez M, Starfield BH. Primary care, financing and gatekeeping in western Europe. Fam Pract. 1994;11:307–317. doi: 10.1093/fampra/11.3.307. [DOI] [PubMed] [Google Scholar]
- 3.Tudor Hart J. The inverse care law. Lancet. 1971;1:405–412. doi: 10.1016/s0140-6736(71)92410-x. [DOI] [PubMed] [Google Scholar]
- 4.Roland M. Linking physicians' pay to the quality of care — a major experiment in the United Kingdom. N Engl J Med. 2004;351:1448–1454. doi: 10.1056/NEJMhpr041294. [DOI] [PubMed] [Google Scholar]
- 5.Wright J, Martin D, Cockings S, Polack C. Overall quality of outcomes framework scores lower in practices in deprived areas. Br J Gen Pract. 2006;56:277–279. [PMC free article] [PubMed] [Google Scholar]
- 6.NHS. The information centre. Quality and Outcomes Framework. Statistics and data collections. http://www.ic.nhs.uk/statistics-and-data-collections/audits-and-performance/qof (accessed 14 May 2007)
- 7.Beginners' guide to UK geography. Super Output Areas (SOAs) http://www.statistics.gov.uk/geography/soa.asp (accessed 9 May 2007)
- 8.Bibby J, Shepherd J. Developing a new classification of urban and rural areas for policy purposes — the methodology. London: Office for National Statistics; 2004. [Google Scholar]
- 9.McLean G, Sutton M, Guthrie B. Deprivation and quality of primary care services: evidence for persistence of the inverse care law from the UK Quality and Outcomes Framework. J Epidem Comm Health. 2006;60:917–922. doi: 10.1136/jech.2005.044628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Doran T, Fullwood C, Gravelle H, et al. Pay-for-performance programs in family practices in the United Kingdom. N Engl J Med. 2006;355:375–84. doi: 10.1056/NEJMsa055505. [DOI] [PubMed] [Google Scholar]
- 11.Rothman KJ. No adjustments are needed for multiple comparisons. Epidemiology. 1990;1:43–46. [PubMed] [Google Scholar]
- 12.Ashworth M, Armstrong D. The relationship between general practice characteristics and quality of care: a national survey of indicators used in the UK ‘Quality and Outcomes Framework’. BMC Fam Pract. 2006;7:68. doi: 10.1186/1471-2296-7-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Campbell SM, Roland MO, Middleton E, Reeves D. Improvements in quality of clinical care in English general practice 1998–2003: longitudinal observational study. BMJ. 2005;331:1121–1125. doi: 10.1136/bmj.38632.611123.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Longley PA, Goodchild G, Maguire DJ, Rhind DW. Geographic information systems and science. Chichester: John Wiley and Sons Ltd; 2001. [Google Scholar]
- 15.Strong M, Maheswaran R, Pearson T. A comparison of methods for calculating general practice level socioeconomic deprivation. BMC Int J Health Geographics. 2006;5:29–34. doi: 10.1186/1476-072X-5-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Saxena S, George J, Barber J, et al. Association of population and practice factors with potentially avoidable admission rates for chronic diseases in London: cross sectional analysis. J R Soc Med. 2006;99:81–89. doi: 10.1258/jrsm.99.2.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lipman T. Singing from the same QOF hymn sheet: Stairway to Heaven or Mephisto Waltz. Br J Gen Pract. 2006;56:819–820. [Google Scholar]
- 18.Reeves D, Baker D. Investigating relationships between health need, primary care and social care using routine statistics. Health Place. 2004;10:129–140. doi: 10.1016/S1353-8292(03)00053-4. [DOI] [PubMed] [Google Scholar]
- 19.Syme SL. Social and economic disparities in health: thoughts about intervention. Milbank Q. 1998;76:493–505. 306–307. doi: 10.1111/1468-0009.00100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Adams J, White M. Socio-economic deprivation is associated with increased proximity to general practices in England: an ecological analysis. J Public Health. 2005;27:80–81. doi: 10.1093/pubmed/fdh210. [DOI] [PubMed] [Google Scholar]
- 21.Hippisley-Cox J, Hardy C, et al. The effect of deprivation on variations in general practitioners' referral rates: a cross sectional study of computerised data on new medical and surgical outpatient referrals in Nottinghamshire. BMJ. 1997;314:1458–1461. doi: 10.1136/bmj.314.7092.1458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hippisley-Cox J, O'Hanlon S, Coupland C. Association of deprivation, ethnicity, and sex with quality indicators for diabetes: population based survey of 53,000 patients in primary care. BMJ. 2004;27:1267–1269. doi: 10.1136/bmj.38279.588125.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Heaney DC, MacDonald BK, Everitt A, et al. Socioeconomic variation in incidence of epilepsy: prospective community based study in south east England. BMJ. 2002;325:1013–1016. doi: 10.1136/bmj.325.7371.1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang Y, O'Donnell CA, Mackay DF, Watt GC. Practice size and quality attainment under the new GMS contract: a cross-sectional analysis. Br J Gen Pract. 2006;56:830–835. [PMC free article] [PubMed] [Google Scholar]
- 25.Carr-Hill RA, Sheldon T. Designing a deprivation payment for general practitioners: the UPA(8) wonderland. BMJ. 1991;302:393–396. doi: 10.1136/bmj.302.6773.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Guthrie B, McLean G, Sutton M. Workload and reward in the Quality and Outcomes Framework of the 2004 general practice contract. Br J Gen Pract. 2006;56:836–841. [PMC free article] [PubMed] [Google Scholar]
- 27.Department of Health. Inequalities in health: report of an independent inquiry chaired by Sir Donald Acheson. London: The Stationery Office; 1998. [Google Scholar]