Abstract
This study examined time trends in the incidence of peptic ulcers and oesophagitis, and the prescription of acid-inhibiting drugs in the period 1994–2003. Data were retrieved from records in general practices in Flanders, Belgium. The incidence of duodenal ulcers decreased by two-thirds and the incidence of gastric ulcers halved, the incidence of oesophagitis initially increased and decreased slowly later on. In 10 years the proportion of patients taking proton-pump inhibitors rose sixfold while the proportion taking H2 antagonists remained stable.
Keywords: anti-ulcer agents, epidemiology, family practice, oesophagitis, peptic ulcer
INTRODUCTION
The incidence of peptic ulcers has fluctuated considerably in the past.1 Most epidemiological studies are performed in hospitals on small numbers of patients hospitalised with complications.2 However, general practice is the appropriate location to investigate the incidence of peptic ulcers in the general population. A gastroscopy can be performed ambulatory at a patient with stomach complaints, to make the exact diagnosis of gastric or duodenal ulcer or oesophagitis. Drug treatment with H2 receptor-antagonists and proton pump inhibitors generally causes no problems with complications being rare. Few data are available for the incidence of peptic ulcers and oesophagitis based on direct information from primary care,3,4 yet this information is necessary for monitoring these diseases. It is unknown whether the increased use of proton-pump inhibitors has influenced the incidence of peptic ulcers.5
This study examined the incidence of duodenal ulcers, gastric ulcers, and oesophagitis in general practice during the period 1994–2003 in Flanders, the northern part of Belgium. The prescription of H2 receptor antagonists and proton-pump inhibitors in the same period was also studied.
METHOD
The Intego database
This study is based on data from the Intego database.6 The database comprises data extracted from the electronic medical records of GPs who work with the medical software Medidoc™. Only practices whose data are of sufficient quality are included in the database. The number of new diagnoses per patient per year has to be greater than one and this relation needed to be stable during the recording period. GPs receive tips about recording data and specific training during workshops on how to note diagnoses with a thesaurus. Data are regularly subjected to internal quality controls. The number of participating practices increased from 26 (34 GPs) in 1999 to 47 (55 GPs) in 2004 and there is almost no omission of cooperating practices. The demographics of the the database population are in concordance with the Flemish population and the practices are spread over the whole of Flanders.
How this fits in
The frequency of peptic ulcers has decreased and the frequency of oesophagus increased during the past decades. This has resulted in fewer hospital admissions for ulcer disease. Environmental factors such as improved medical treatment seem responsible for this. This research was possible due to the use of databases of primary care data.
GPs note diagnoses using software-specific keywords, which they select from a list of 27 000. In the central database these keywords are automatically converted into the International Classification of Primary Care (ICPC-2) classification. The database contains data on diagnoses, drug prescriptions, and laboratory results of 140 000 different patients and 780 000 patient-years.
Case definition
Peptic ulcers and oesophagitis are chronic and recurring diseases and, consequently, counting each flare-up of the disease could produce misleading results about the frequency of the illness. Therefore, each patient was counted uniquely for oesophagitis or duodenal or gastric ulcer.
In Belgium the cost of prescribed H2 antagonists and proton-pump inhibitors is only refunded to the patient with the consent of the Health Insurance Authority. Patients used to need a gastroscopy, from which the diagnosis of oesophagitis or peptic ulcer was made by the endoscopist. This regulation was abolished for H2 antagonists on 1 March 2001 and for generic proton-pump inhibitors on 1 November 2002. Until these dates, new diagnoses were almost always confirmed by endoscopy.
To calculate the proportion of patients who took a H2 antagonist or proton-pump inhibitor, a patient was considered to be taking a drug of a certain class if a prescription was recorded in the year concerned.
RESULTS
From 1994–1995 to 2002–2003 the yearly age-standardised incidence of new patients with a duodenal ulcer decreased from 2.22 to 0.85%, with a significant incidence ratio of 0.38 (95% confidence interval [CI] = 0.31 to 0.48). The incidence of gastric ulcer decreased from 1.75 to 1.01%, with a significant incidence ratio of 0.58 (95% CI = 0.47 to 0.72). The incidence of oesophagitis increased from 7.20 to 10.11% in 1998 and declined back to 8.73% in 2002–2003 with a significant incidence ratio of 1.22 (95% CI 1.11 to 1.33; Table 1).
Table 1.
Incidence per 1000 patient-years of duodenal ulcers, gastric ulcers, and oesophagitis in the years 1994–1995 and 2002–2003.
| 1994–1995 | 2002–2003 | ||||
|---|---|---|---|---|---|
| Age group, yearsa | n | Incidence (95% CI) | n | Incidence (95% CI) | Incidence ratio (95% CI) |
| Duodenal ulcer | |||||
| 25–44 | 81 | 2.12 (1.68 to 2.63) | 26 | 0.70 (0.46 to 1.02) | 0.33b (0.21 to 0.52) |
| 45–64 | 86 | 3.19 (2.55 to 3.93) | 31 | 0.92 (0.62 to 1.30) | 0.29b (0.19 to 0.43) |
| 65–74 | 42 | 3.92 (2.82 to 5.29) | 33 | 2.49 (1.72 to 3.50) | 0.64 (0.40 to 1.00) |
| ≥75 | 36 | 5.14 (3.60 to 7.12) | 24 | 1.87 (1.20 to 2.78) | 0.36b (0.22 to 0.61) |
| Total (age-standardised) | 251 | 2.22 (1.94 to 2.50) | 119 | 0.85 (0.70 to 1.00) | 0.38b (0.31 to 0.48) |
| Gastric ulcer | |||||
| 25–44 | 54 | 1.41 (1.06 to 1.84) | 25 | 0.67 (0.43 to 0.99) | 0.48b (0.30 to 0.76) |
| 45–64 | 79 | 2.93 (2.32 to 3.65) | 54 | 1.60 (1.20 to 2.08) | 0.55b (0.39 to 0.77) |
| 65–74 | 36 | 3.36 (2.35 to 4.65) | 33 | 2.49 (1.72 to 3.50) | 0.74 (0.46 to 1.19) |
| ≥75 | 26 | 3.71 (2.43 to 5.44) | 30 | 2.34 (1.58 to 3.34) | 0.63 (0.37 to 1.07) |
| Total (age-standardised) | 197 | 1.75 (1.50 to 2.00) | 145 | 1.01 (0.84 to 1.18) | 0.58b (0.47 to 0.72) |
| Oesophagitis | |||||
| 25–44 | 262 | 6.84 (6.04 to 7.72) | 323 | 8.65 (7.73 to 9.64) | 1.26b (1.07 to 1.49) |
| 45–64 | 279 | 10.33 (9.16 to 11.62) | 386 | 11.40 (10.29 to 12.60) | 1.10 (0.95 to 1.29) |
| 65–74 | 121 | 11.28 (9.36 to 13.48) | 178 | 13.46 (11.55 to 15.59) | 1.19 (0.95 to 1.50) |
| ≥75 | 82 | 11.71 (9.31 to 14.53) | 148 | 11.53 (9.75 to 13.55) | 0.98 (0.75 to 1.29) |
| Total (age-standardised) | 829 | 7.20 (6.70 to 7.70) | 1177 | 8.73 (8.23 to 9.23) | 1.22b (1.11 to 1.33) |
Younger age groups are not shown because of the low numbers.
Statistically significant results.
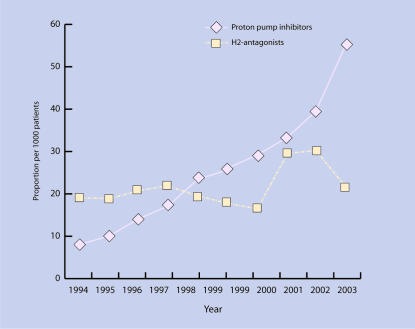
The incidence of duodenal ulcers decreased most sharply in the 25–44 and 45–64 year age groups with a significant incidence ratio of 0.33 and 0.29 respectively. The incidence of gastric ulcer also decreased most sharply in the 25–44 and 45–64 year age groups, with a significant incidence ratio of 0.48 and 0.55. For oesophagitis the increase was only significant in the 25–44 year age group, with an incidence ratio of 1.26 (95% CI = 1.07 to 1.49). The age-standardised proportion of patients who took a proton-pump inhibitor increased in the period 1994–2003 from 8.68% to 50.02%. The proportion of patients who took an H2 antagonist remained stable at around 20% from 1994–2000, increased for 2 years to 30%, and decreased again to the level of 1994 in 2003 (Figure 1).
Figure 1.
The proportion of patients who took a proton-pump inhibitor or an H2-antagonist from 1994 to 2003.
DISCUSSION
According to the current results, the incidence of duodenal ulcers decreased by two-thirds, while the incidence of gastric ulcers halved over the period of 10 years, and the incidence of oesophagitis initially increased and slowly decreased later on. The frequency of oesophagitis was about four times that of peptic ulcer. Over 10 years the proportion of patients taking proton-pump inhibitors rose sixfold, while the proportion taking H2 antagonists remained stable.
Different simultaneous trends are probably the cause of the changes in incidence. As these changes in incidences occurred over a relatively short period of time, it is unlikely that the cause was due to biological changes. Causes are likely to be identified in societal influences. There could have been a diagnostic shift from peptic ulcer to oesophagitis, but the reason for such a shift is not obvious. It is possible that the widespread and chronic use of proton-pump inhibitors in patients with oesophagitis protects against the occurrence of peptic ulcers, but this cannot be deduced from this study. Susser and Stein1 described a cohort hypothesis according to which societal influences have affected different generations differently in the past and suggested a decline in the incidence of peptic ulcers. Other factors affecting ulcer aetiology can be sought in the increasing use of non-steroidal anti-inflammatory drugs and lifestyle changes.7 The increase of Helicobacter pylori eradication might play a role, but this information is not available in the database.
The current results are based on data from a continuously recording network of GPs. They aim to examine a large population in primary care and to calculate incidence rates in a direct way. No formal criterion was used for the registration of a peptic ulcer or oesophagitis in the electronic medical records by GPs. However, Belgian social security regulations required a gastroscopy report for the reimbursement of acid secretion inhibiting drugs. Therefore, it can be safely assumed that almost all new diagnoses were confirmed by gastroscopy.
In recent decades the incidences of peptic ulcer and oesophagitis have changed considerably. It is likely that different simultaneous trends in society are responsible for this. Possible explanations are a shift in diagnosis and the increasing use of proton-pump inhibitors; however, the factors responsible for this cannot be determined from this descriptive study.
Acknowledgments
Thanks are expressed to all the GPs who participated. Without their collaboration this work would not have been possible.
Funding body
The Intego project is supported by the Government of Flanders and commissioned by its Minister responsible for Health Policy
Ethics committee
Personal data are encrypted to guarantee protection of privacy. The project was referred to the Privacy Committee which enforces the Belgian legislation on privacy. The Intego project was also approved by the ethical review board of the medical school of the University of Leuven, Belgium
Competing interests
The authors have stated that there are none
REFERENCES
- 1.Susser M, Stein Z. Civilisation and peptic ulcer. Lancet. 1962;1:115–119. [PubMed] [Google Scholar]
- 2.Bardhan K, Williamson M, Royston C, Lyon C. Admission rates for peptic ulcer in the Trent Region, UK, 1972–2000. Changing pattern, a changing disease? Dig Liver Dis. 2004;36(9):577–588. doi: 10.1016/j.dld.2004.04.007. [DOI] [PubMed] [Google Scholar]
- 3.Kang J-Y, Tinto A, Higham J, Majeed A. Peptic ulceration in general practice in England and Wales 1994–1998: period prevalence and drug management. Aliment Pharmacol Ther. 2002;16(6):1067–1074. doi: 10.1046/j.1365-2036.2002.01261.x. [DOI] [PubMed] [Google Scholar]
- 4.Van de Lisdonk EH, van den Bosch WJHM, Lagro-Janssen ALM. Ziekten in de huisartspraktijk. 4th edn. Maarssen: Elsevier gezondheidszorg; 2003. [Google Scholar]
- 5.Post P, Kuipers E, Meijer G. Declining incidence of peptic ulcer but not of its complications: a nation-wide study in the Netherlands. Aliment Pharmacol Ther. 2006;23(11):1587–1593. doi: 10.1111/j.1365-2036.2006.02918.x. [DOI] [PubMed] [Google Scholar]
- 6.Bartholomeeusen S, Chang-Yeon K, Faes C, et al. The denominator in general practice, a new approach from the Intego database. Fam Pract. 2005;22(4):442–447. doi: 10.1093/fampra/cmi054. [DOI] [PubMed] [Google Scholar]
- 7.Levenstein S. Commentary: peptic ulcer and its discontents. Int J Epidemiol. 2003;31(1):29–33. doi: 10.1093/ije/31.1.29. [DOI] [PubMed] [Google Scholar]