Abstract
Background and purpose:
Monoamine oxidase inhibitors (MAOI) are known to cause serotonin toxicity (ST) when administered with selective serotonin reuptake inhibitors (SSRI). Methylene blue (methylthionium chloride, MB), a redox dye in clinical use, has been reported to precipitate ST in patients using SSRI. MB was assessed for MAO inhibition and so for its potential to precipitate ST.
Experimental approach:
Inhibition of purified human MAO was quantified using kinetic assays and visible spectral changes to study the interactions of MB with MAO A.
Key results:
MB was a potent (tight binding) inhibitor for MAO A. It also inhibited MAO B but at much higher concentration. Interactions of MB with the active site of MAO A were confirmed by its action both as an oxidising substrate and as a one-electron reductant.
Conclusions and implications:
MB is a potent reversible inhibitor of MAO A with implications for gut uptake of amines when administered orally. At concentrations reported in the literature after intravenous administration, MAO B would be partially inhibited but MAO A would be completely inhibited. This inhibition of MAO A would be expected to lead to perturbations of 5-hydroxytryptamine metabolism and hence account for ST occurring when administered to patients on SSRI treatment.
Keywords: methylene blue, methylthionium chloride, serotonin toxicity, monoamine oxidase A, MAOI, tight binding
Introduction
Serotonin toxicity (ST), formerly referred to as serotonin syndrome, is one of very few drug–drug interactions involving usual therapeutic doses of commonly used drugs that are capable of developing rapidly and causing death within 24 h. A mixture of therapeutic doses of any drug with significant monoamine oxidase (MAO) inhibitor (MAOI) properties with another drug that has potency as a selective serotonin reuptake inhibitor (SSRI) produces a high risk of precipitating this rapidly worsening interaction (reviewed in Gillman, 2006a). The typical clinical features of ST are (i) neuromuscular hyperactivity: tremor, clonus, myoclonus and hyperreflexia, and, in the advanced stage, pyramidal rigidity; (ii) autonomic hyperactivity: diaphoresis, fever, tachycardia, tachypnoea and mydriasis; and (iii) altered mental status: agitation, excitement, with confusion in the advanced stage. There have been several deaths or near deaths, reported recently where a single dose of a SSRI has been inadvertently added to a MAOI (Otte et al., 2003; Cassens et al., 2006; Zonneveld et al., 2006).
In the past the only drugs recognised as possessing these properties were antidepressants used by specialists so that the risk of them being combined inadvertently was small. However, there are now many drugs on the market that act as 5-hydroxytryptaminergic agents (mostly SSRIs), or MAOIs, which are neither advertised, nor generally recognised, as 5-hydroxytryptaminergic drugs (for example, sibutramine and linezolid). Despite the clear understanding of ST interactions that has developed over the past decade, there is still misinformation in standard texts, such as the British National Formulary, and in pharmaceutical company product information (Gillman, 2005). Recent reviews deal with this complex topic in detail (Gillman, 1998, 2006a, 2006b, 2006c; Dunkley et al., 2003; Whyte et al., 2003; Whyte, 2004; Isbister and Buckley, 2005).
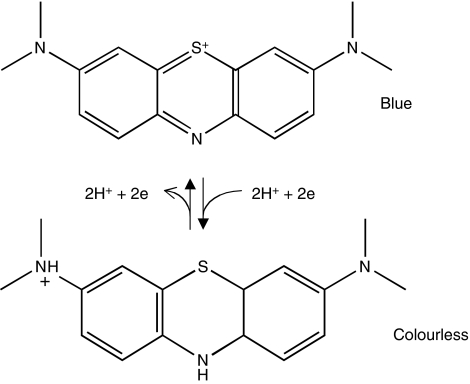
The spectrum concept of ST predicts clearly that severe, life-threatening, degrees of toxicity are likely to develop only after the co-administration of SSRIs and MAOIs. A case report of neurological toxicity associated with the administration of methylene blue (methylthionium chloride, MB), which precipitated the work in this article (Rosenbaum, 2006) seemed an exception. However, the patients in that and subsequently uncovered reports (Gillman, 2006c) had all been taking an SSRI antidepressant before surgery involving the intravenous infusion of MB. All these patients experienced severe toxicity of the degree expected to result only from a combination of MAOI and SSRI, and too severe to be the result of an SSRI alone. A search of the literature revealed no report of such toxicity from MB alone. This led to the prediction that MB (Figure 1) must possess significant MAOI potency.
Figure 1.
Oxidised and reduced forms of methylene blue.
Existing clinical literature (reviewed in Gillman, 2006c), including a report of antidepressant effect of MB (Naylor et al., 1987), appeared to support the possibility that MB would inhibit MAO, as did the well-known properties of MB as an electron acceptor. Effective inhibition of amine oxidases, including MAO, was reported to play a role in the prevention by MB of ifosfamide encephalopathy (Aeschlimann et al., 1996; Kupfer et al., 1996). However, the only reported Ki for inhibition of MAO B was rather high at 5.6 μM (Bachurin et al., 2001; Shumakovich et al., 2004). This is within the range for whole-blood concentration immediately after a 100 mg oral dose in humans, and intravenous administration gave more than 10-fold higher sustained concentrations (Peter et al., 2000). In another study, the concentration of MB in rat brain was estimated at 0.5 μM from 1 mg kg−1 intraperitoneally (Callaway et al., 2004).
The role of MAO in the brain, its involvement in disease and the therapeutic potential of MAOIs has recently been reviewed in the light of new structural information (Youdim et al., 2006). Crystal structures of MAO A (De Colibus et al., 2005) and MAO B (Binda et al., 2002) have shown that the active site is a long, narrow hydrophobic cavity penetrating deep into the molecule where the substrate is aligned by two tyrosines so that the amine is close to the N-5 of the flavin. The active site of MAO A is wider than that of MAO B (De Colibus et al., 2005) and, in functional studies, MAO A accommodates larger non-flexible ligands (Efange et al., 1993; Medvedev et al., 1998). Structure–function studies have shown that MAO substrates and inhibitors are somewhat lipophilic with an aromatic ring and a nitrogen (or oxygen or sulphur) close to that ring (reviewed in Wouters, 1998; Kalgutkar et al., 2001; Ramsay and Gravestock, 2003). MB fits this description and indeed was an inhibitor and electron acceptor for MAO B (Shumakovich et al., 2004). Other tricyclic heterocycles, such as the β-carbolines (Kim et al., 1997), are also known as effective inhibitors, particularly of MAO A.
The experiments reported below show that MB inhibits both MAO A and MAO B. In particular, it is a tight-binding inhibitor of MAO A that interacts with the active site as shown by its action as an oxidative substrate and by its redox effects on the flavin of MAO A.
Methods
MAO assays
Recombinant human liver MAO A and MAO B were purified as reported previously (Tan and Ramsay, 1993).
MAO A (usually about 50 nM) was assayed spectrophotometrically at 314 nm in 50 mM potassium phosphate, pH 7.2–0.2%, Triton-X100 at 30°C using kynuramine (0.1–0.9 mM) as the substrate (Tan and Ramsay, 1993). The kinetic constants were calculated by the Shimazu kinetic software. Apparent Km values in the presence of MB (30–200 nM) were also determined. This experiment revealed an apparent Ki of 69 nM, only slightly higher than the enzyme concentration, indicating that Michaelis–Menten analysis could not be used because the concentration of free inhibitor would be depleted by binding to the enzyme. To obtain the Ki, the initial rates in the absence and presence of MB were analysed by the equation developed by Morrison (1968) for tight-binding inhibitors.
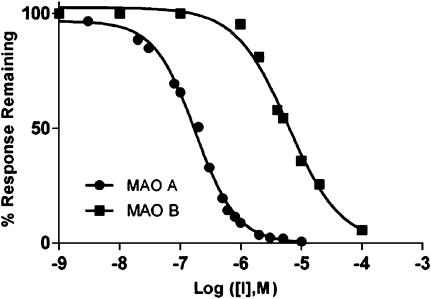
MAO B was assayed polarographically using the same buffer as for MAO A (Tan and Ramsay, 1993). Inhibition was measured for 0–20 μM MB in the presence of 0.6 μM benzylamine (2 × Km) as shown in Figure 2. Further analysis of the kinetics of interaction with MAO B would require varying both the amine and oxygen substrates, because the Km for oxygen is 0.28 μM (Husain et al., 1982; Ramsay et al., 1987).
Figure 2.
Dose–response curves for the inhibition of MAO A (left) and MAO B (right) by methylene blue (MB). MAO A (122 nM) was assayed spectrophotometrically with 0.3 mM (2 × Km) kynuramine, and 25 concentrations of MB (some points omitted for clarity). MAO B was assayed polarographically with 0.6 mM (2 × Km) benzylamine.
Spectrophotometric studies of MAO
Spectral data were obtained using MAO A in 50 μM potassium phosphate, pH 7.2, 0.05% Brij, as in previous work (Ramsay, 1991; Jones et al., 2005). The enzyme was prepared for the experiments by centrifugal gel filtration, diluted to about 15 μM, and its concentration determined from the absorbance at 456 nm (extinction coefficient, 12 300 M−1 cm−1). For anaerobic experiments, oxygen was replaced with argon by cycling the custom-made anaerobic cuvette between vacuum and argon.
Data analysis
Parameters are shown as the values calculated±s.e. from the non-linear regression fit. The calculation of Ki used the equation for tight binding inhibitors (Morrison, 1968) in PRISM (from Graphpad Software, Inc., http://www.graphpad.com/curvefit/). Ki values are the mean±s.d. mean of values from four experiments.
Materials
All chemicals were purchased from Sigma-Aldrich (Poole, Dorset, UK). The purity of the MB was checked by determining the ratio of the absorbance at 664–610 nm using 10 μM MB in water (Fujimoto et al., 1994). The ratio was 2.02 so the MB was used as supplied. It should be noted that the molar absorbance of MB varies with concentration (Lewis et al., 1943). The oxidised and reduced forms of MB are shown in Figure 1.
Results
MAO A and MAO B have very different sensitivity to MB
Figure 2 shows the inhibition of the two forms of MAO by MB, each assayed at subsaturating substrate concentration (2 × Km). The IC50 value for MB inhibition of MAO A was 164±8 nM under this specific condition with 122 nM MAO A. In contrast, no inhibition of MAO B was seen in the spectrophotometric assay at 100 nM. Data from the polarographic assays of MAO B are shown in Figure 2 (the right-hand curve) and the IC50 value for MAO B inhibition by MB was 5.5±1.7 μM.
MB is a tight-binding inhibitor of MAO A
The IC50 value of 164±8 nM (Figure 2) was obtained using 122 nM MAO A in the assays. Clearly, the normal Michaelis–Menten assumption that the inhibitor concentration would not be depleted by the enzyme did not hold. When both kynuramine and MB were varied, the IC50 value increased as the substrate concentration increased (data not shown), consistent with competitive inhibition (Henderson, 1972). Tight-binding analysis of data for MAO A according to Morrison (1968) gave a Ki value of 27±3 nM (mean±s.d.; n=4).
MB binds to the active site of MAO A
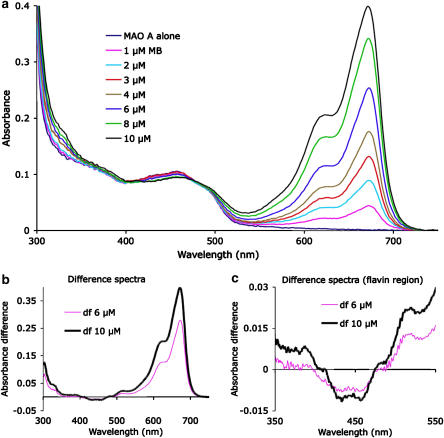
Inhibitors binding in the active site of MAO A influence the visible spectrum of the covalently bound cofactor flavin adenine dinucleotide (FAD) (Hynson et al., 2003). When MAO A was titrated with MB (Figure 3), only a very small and featureless change in the difference spectrum of the MAO A FAD (MAO A with MB—MAO A alone) at around 450 nm was detected (Figure 3b). In previous work, the KD for inhibitor binding was calculated from inhibitor-induced changes in the flavin spectrum (Hynson et al., 2003). However, the influence of MB on the flavin spectrum was too small to analyse accurately, with a maximum decrease of 0.01 that was compromised by the large adjacent absorbance peaks of the MB.
Figure 3.
Titration of MAO A with methylene blue (MB). Increments of MB (1 μM) were added to MAO A (7.6 μM) and the spectra recorded for MAO A with final concentrations of 0–10 μM MB as indicated. Arrows indicate the increase at 665 nm due to MB and the decrease in the flavin region. (a) The difference between the spectrum for MAO A with 6 μM or 10 μM MB and the spectrum for MAO A alone is shown in (b). (c) The difference spectra are the same as (b) but on an expanded scale to show the change in the absorbance of the MAO A flavin.
In contrast, the absorbance of MB was greatly (about 50%) decreased in the presence of enzyme (Figure 3b) compared with the value of 61 500 M−1 cm−1 determined for the conditions used here, an aqueous solution of 50 mM potassium phosphate, pH7.4, containing 0.05% Brij. The molar extinction coefficient for MB is influenced by the concentration at which it is determined (Lewis et al., 1943; Bergmann and O'Konski, 1963), by the salt concentration in aqueous solution (Fujimoto et al., 1994), and by the presence of detergent (Yamamoto et al., 2007). Binding to or association with surfaces or other compounds, such as serum albumin (Hu et al., 2005), also alters the absorption spectrum. Thus, the decrease in absorbance of MB induced by enzyme was likely to be due to nonspecific absorption rather than specific insertion into the hydrophobic active site and was thus not examined further.
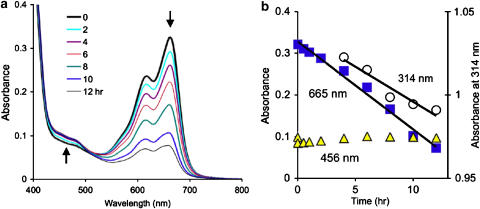
MB acts as an oxidising substrate for MAO A
Proximity of MB to the flavin was confirmed by the reduction of MB by kynuramine in the presence of MAO A under anaerobic conditions (Figure 4). MAO A with 10 μM MB was made anaerobic and excess kynuramine (0.3 mM final concentration) was added from the sidearm. Spectra were collected every 30 min overnight (Figure 4a). The time courses for the absorbance of MB (664 nm) and for the flavin (456 nm) show that the flavin was rapidly reduced by the excess of substrate, then reoxidised until MB reduction reached steady state (Figure 4b). The steady-state rate of reduction of MB over 12 h (Figure 4b) was 0.35 nmol h−1 and the rate of oxidation of kynuramine was 0.39 nmol h−1. To compare this rate with that where oxygen is the electron acceptor, as in Figure 2, the observed velocities were converted to rate constants to normalise for the different enzyme concentrations. The rate constant for the oxidation of kynuramine by MB was 0.045 h−1, extremely slow compared to the rate constant with oxygen at 4950 h−1. Others have previously reported that MB gave a 500-fold slower rate than oxygen with MAO B (Shumakovich et al., 2004).
Figure 4.
Methylene blue (MB) acts as the oxidising substrate for MAO A under anaerobic conditions. (a) MAO A (8 μM) with 10 μM MB was made anaerobic and 0.3 mM kynuramine added at time 0. The absorbance of MB at 665 nm decreased with time as indicated by the arrow. The flavin absorbance at 456 nm decreased during the mixing time but returned to its starting value over 3 h. (b) The steady-state rate of oxidation of kynuramine (314 nm) and of reduction of MB (665 nm) were compared between 4 and 12 h when the flavin absorbance at 456 nm was constant.
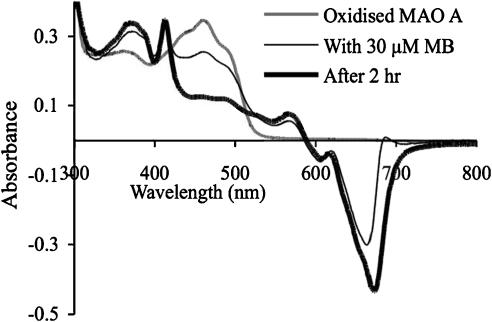
MB in the presence of reducing agents reduces MAO A
MB is commonly used as a photosensitiser. Light excites MB into a triplet state that can extract electrons from amines generating reduced MB (Kim and Scranton, 2004). Thiol-reducing agents are often used to produce reduced MB (for example, Jonnalagadda and Tshabalala, 1992). When MB was added anaerobically to MAO A-containing dithiothreitol (normally present for storage) at about 0.3 mM and the inhibitor amine, D-amphetamine, at 50 μM (Ki for MAO A is 20 μM (Ramsay and Hunter, 2002)), reduction of MAO A was observed. Figure 5 shows the decrease at 456 nm and the appearance of the 412 nm peak typical of the anionic flavosemiquinone in MAO A in the presence of 30 μM MB. After 2 h, the one-electron reduction of MAO A was complete. No further reduction to the dihydroflavin was observed because of the presence of D-amphetamine that stabilises the MAO semiquinone form (Ramsay and Hunter, 2002). Only about 1% radical was generated in the absence of dithiothreitol, so the radical generation requires the thiol reagent.
Figure 5.
Reduction of MAO A by methylene blue (MB) in the presence of D-amphetamine and dithiothreitol (DTT). MAO A was diluted eightfold from stock to 27 μM so that the concentration of D-amphetamine was 60 μM and of DTT about 0.35 mM, was made anaerobic, and 30 μM MB added both to the MAO A cuvette and to the blank cuvette. The spectral change after the addition showed some reduction of MB (decrease at 665 nm) and appearance of the features of the MAO A anionic semiquinone (increase at 380 and 412 nm, decrease at 456 nm). After 2 h at 20°C, the spectrum indicated almost complete conversion of MAO A to the semiquinone form. No further change was observed even 24 h later.
Discussion
MB has been in medical use for many years with few reports of toxic effects. In early experiments, oral MB was found to be innocuous in 15 kg dogs at 2 g per day, but an intravenous dose of 0.5 g was lethal (Agell and Agell, 1929). The recent case reports of neurological sequelae following MB infusions summarised by Gillman (2006c) confirm that MB is not an innocuous substance. Indeed, MB is cytotoxic to bacteria and has been reported to increase oxidative stress (May et al., 2003). Furthermore, its reactive redox chemistry led to its use as a photosensitiser. However, the particular clinical observations in ST and their occurrence only in patients on SSRIs indicated that MB must also influence the 5-hydroxytryptamine system.
The high Ki value for MAO B of 5.6 μM (Bachurin et al., 2001), confirmed by the IC50 reported here, was not consistent with MAO B as a target for the action of MB. Despite this, in rats, where the brain concentration of MB was estimated to be about 0.5 μM (Callaway et al., 2004), both MAO inhibition and increase of 5-hydroxytryptamine as a result of MB treatment have been reported (Lerch et al., 2006). If MAO B is not inhibited, then MAO A could be the target. At the molecular level, both the crystal structure (Binda et al., 2002) and the inhibitor profile for MAO B (Efange et al., 1993) indicate that the active site is relatively narrow. In contrast, MAO A accommodates (De Colibus et al., 2005) and is strongly inhibited by larger molecules such as β-carbolines (Kim et al., 1997) and oxazolidinones such as linezolid (Jones et al., 2005). The data presented here establish that MB is a very potent inhibitor of MAO A with a Ki of 27 nM and that it binds in the active site of MAO A.
The prediction based on the clinical observations, that MAO A would be inhibited by MB, has been proven. It is consistent with structural information about the two MAO isoforms and is supported by information from studies on rat brain. MB is an effective MAO A inhibitor and thus will influence 5-hydroxytryptamine levels at doses expected during MB infusion. For comparison, linezolid, for which the risk of ST in patients receiving SSRIs is established (Morales-Molina et al., 2005), has a Ki for MAO A of 20 μM (Jones et al., 2005). We conclude that the use of MB by infusion in combination with other 5-hydroxytryptaminergic agents could lead to the ST syndrome as a result of MAO A inhibition.
Acknowledgments
Some of the experiments formed part of CD's undergraduate thesis (University of St Andrews). Some initial experiments were performed by Mr Aleksey Zholobenko, University of St Andrews, during summer work experience and were reported in a poster presented at the 12th Amine Oxidase Workshop, August 2006 and at the Biochemical Society focus meeting on Health Implications of Dietary Amines, October 2006 (http://www.biochemistry.org/meetings/postertoc/SA062/default.htm).
Abbreviations
- MAO
monoamine oxidase
- MAOI
monoamine oxidase inhibitor
- MB
methylene blue (methylthionium chloride)
- SSRI
selective serotonin reuptake inhibitor
- ST
serotonin toxicity
Conflict of interest
The authors state no conflict of interest.
References
- Aeschlimann C, Cerny T, Kupfer A. Inhibition of (mono)amine oxidase activity and prevention of ifosfamide encephalopathy by methylene blue. Drug Metab Dispos. 1996;24:1336–1339. [PubMed] [Google Scholar]
- Agell J, Agell Y. La coloracion atrificial de los alimentos y bebidas en su aspeto toxicologico y medico-legal. Quim Ind. 1929;6:137–149. [Google Scholar]
- Bachurin SO, Byzova NA, Dubova LG, Yaropolov AI. Monooxidase catalysis of amine oxidation by organic electron acceptors. Dokl Chem. 2001;376:1–4. [Google Scholar]
- Bergmann K, O'Konski C. A spectroscopic study of methylene blue monomer, dimer, and complexes with montmorillonite. J Phys Chem. 1963;67:2169–2177. [Google Scholar]
- Binda C, Newton-Vinson P, Hubalek F, Edmondson DE, Mattevi A. Structure of human monoamine oxidase B, a drug target for the treatment of neurological disorders. Nat Struct Biol. 2002;9:22–26. doi: 10.1038/nsb732. [DOI] [PubMed] [Google Scholar]
- Callaway NL, Riha PD, Bruchey AK, Munshi Z, Gonzalez-Lima F. Methylene blue improves brain oxidative metabolism and memory retention in rats. Pharmacol Biochem Behav. 2004;77:175–181. doi: 10.1016/j.pbb.2003.10.007. [DOI] [PubMed] [Google Scholar]
- Cassens S, Nickel EA, Quintel M, Neumann P. The serotonin syndrome. Fatal course of intoxication with citalopram and moclobemide. Anaesthesist. 2006;55:1189. doi: 10.1007/s00101-006-1089-1. [DOI] [PubMed] [Google Scholar]
- De Colibus L, Li M, Binda C, Lustig A, Edmondson DE, Mattevi A. Three-dimensional structure of human monoamine oxidase A (MAO A): relation to the structures of rat MAO A and human MAO B. Proc Natl Acad Sci USA. 2005;102:12684–12689. doi: 10.1073/pnas.0505975102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunkley EJC, Isbister GK, Sibbritt D, Dawson AH, Whyte IM. The Hunter serotonin toxicity criteria: simple and accurate diagnostic decision rules for serotonin toxicity. QJM—An Int J Med. 2003;96:635–642. doi: 10.1093/qjmed/hcg109. [DOI] [PubMed] [Google Scholar]
- Efange SMN, Michelson RH, Tan AK, Krueger MJ, Singer TP. Molecular-size and flexibility as determinants of selectivity in the oxidation of N-methyl-4-phenyl-1,2,3,6-tetrahydropyridine analogs of Monoamine Oxidase-A and Oxidase-B. J Med Chem. 1993;36:1278–1283. doi: 10.1021/jm00061a020. [DOI] [PubMed] [Google Scholar]
- Fujimoto BS, Clendenning JB, Delrow JJ, Heath PJ, Schurr M. Fluorescence and photobleaching studies of Methylene-Blue binding to DNA. J Phys Chem. 1994;98:6633–6643. [Google Scholar]
- Gillman K. Drug interactions and fluoxetine: a commentary from a clinician's perspective. Exp Opin Drug Safety. 2005;4:965–968. doi: 10.1517/14740338.4.6.965. [DOI] [PubMed] [Google Scholar]
- Gillman PK. Serotonin syndrome: history and risk. Fundam Clin Pharmacol. 1998;12:482–491. doi: 10.1111/j.1472-8206.1998.tb00976.x. [DOI] [PubMed] [Google Scholar]
- Gillman PK. A review of serotonin toxicity data: implications for the mechanisms of antidepressant drug action. Biol Psychiatry. 2006a;59:1046–1051. doi: 10.1016/j.biopsych.2005.11.016. [DOI] [PubMed] [Google Scholar]
- Gillman PK. Extracting value from case reports: lessons from serotonin toxicity. Anaesthesia. 2006b;61:419–422. doi: 10.1111/j.1365-2044.2006.04588.x. [DOI] [PubMed] [Google Scholar]
- Gillman PK. Methylene blue implicated in potentially fatal serotonin toxicity. Anaesthesia. 2006c;61:1013–1014. doi: 10.1111/j.1365-2044.2006.04808.x. [DOI] [PubMed] [Google Scholar]
- Henderson PJ. Linear equation that describes steady-state kinetics of enzymes and subcellular particles interacting with tightly bound inhibitors. Biochem J. 1972;127:321–333. doi: 10.1042/bj1270321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu YJ, Li W, Liu Y, Dong JX, Qu SS. Fluorometric investigation of the interaction between methylene blue and human serum albumin. J Pharm Biomed Anal. 2005;39:740–745. doi: 10.1016/j.jpba.2005.04.009. [DOI] [PubMed] [Google Scholar]
- Husain M, Edmondson DE, Singer TP. Kinetic-studies on the catalytic mechanism of liver Monoamine-Oxidase. Biochemistry. 1982;21:595–600. doi: 10.1021/bi00532a028. [DOI] [PubMed] [Google Scholar]
- Hynson RMG, Wouters J, Ramsay RR. Monoamine oxidase A inhibitory potency and flavin perturbation are influenced by different aspects of pirlindole inhibitor structure. Biochem Pharmacol. 2003;65:1867–1874. doi: 10.1016/s0006-2952(03)00185-0. [DOI] [PubMed] [Google Scholar]
- Isbister GK, Buckley NA. The pathophysiology of serotonin toxicity in animals and humans—implications for diagnosis and treatment. Clin Neuropharmacol. 2005;28:205–214. doi: 10.1097/01.wnf.0000177642.89888.85. [DOI] [PubMed] [Google Scholar]
- Jones TZE, Fleming P, Eyermann CJ, Gravestock MB, Ramsay RR. Orientation of oxazolidinones in the active site of monoamine oxidase. Biochem Pharmacol. 2005;70:407–416. doi: 10.1016/j.bcp.2005.05.001. [DOI] [PubMed] [Google Scholar]
- Jonnalagadda SB, Tshabalala D. A kinetic-study of the reduction of toluidine blue with thiourea in acidic solution. Int J Chem Kinet. 1992;24:999–1007. [Google Scholar]
- Kalgutkar AS, Dalvie DK, Castagnoli N, Taylor TJ. Interactions of nitrogen-containing xenobiotics with monoamine oxidase (MAO) isozymes A and B: SAR studies on MAO substrates and inhibitors. Chem Res Toxicol. 2001;14:1139–1162. doi: 10.1021/tx010073b. [DOI] [PubMed] [Google Scholar]
- Kim D, Scranton A. The role of diphenyl iodonium salt (DPI) in three-component photoinitiator systems containing methylene blue (MB) and an electron donor. J Polymer Sci (Part A Polymer Chem) 2004;42:5863–5871. [Google Scholar]
- Kim H, Sablin SO, Ramsay RR. Inhibition of monoamine oxidase A by beta-carboline derivatives. Arch Biochem Biophys. 1997;337:137–142. doi: 10.1006/abbi.1996.9771. [DOI] [PubMed] [Google Scholar]
- Kupfer A, Aeschlimann C, Cerny T. Methylene blue and the neurotoxic mechanisms of ifosfamide encephalopathy. Eur J Clin Pharmacol. 1996;50:249–252. doi: 10.1007/s002280050102. [DOI] [PubMed] [Google Scholar]
- Lerch S, Kupfer A, Idle JR, Lauterburg BH. Cerebral formation in situ of S-carboxymethylcysteine after ifosfamide administration to mice: a further clue to the mechanism of ifosfamide encephalopathy. Toxicol Lett. 2006;161:188–194. doi: 10.1016/j.toxlet.2005.09.002. [DOI] [PubMed] [Google Scholar]
- Lewis GN, Goldschmid O, Magel T, Bigeleisen DJ. Dimeric and other forms of methylene blue: absorption and fluorescence of the pure monomer. J Am Chem Soc. 1943;65:1150–1154. [Google Scholar]
- May JM, Qu ZC, Whitesell RR. Generation of oxidant stress in cultured endothelial cells by methylene blue: protective effects of glucose and ascorbic acid. Biochem Pharmacol. 2003;66:777–784. doi: 10.1016/s0006-2952(03)00408-8. [DOI] [PubMed] [Google Scholar]
- Medvedev AE, Veselovsky AV, Shvedov VI, Tikhonova OV, Moskvitina TA, Fedotova OA, et al. Inhibition of monoamine oxidase by pirlindole analogues: 3D- QSAR and CoMFA analysis. J Chem Inf Comput Sci. 1998;38:1137–1144. doi: 10.1021/ci9802068. [DOI] [PubMed] [Google Scholar]
- Morales-Molina JA, Mateu-de Antonio J, Marin-Casino M, Grau S. Linezolid-associated serotonin syndrome: what we can learn from cases reported so far. J Antimicrob Chemother. 2005;56:1176–1178. doi: 10.1093/jac/dki368. [DOI] [PubMed] [Google Scholar]
- Morrison JF. Kinetics of reversible inhibition of enzyme-catalysed reactions by tight-binding inhibitors. Biochim Biophys Acta. 1968;185:269–286. doi: 10.1016/0005-2744(69)90420-3. [DOI] [PubMed] [Google Scholar]
- Naylor GJ, Smith AHW, Connelly P. A controlled trial of methylene blue in severe depressive-illness. Biol Psychiatry. 1987;22:657–659. doi: 10.1016/0006-3223(87)90194-6. [DOI] [PubMed] [Google Scholar]
- Otte W, Birkenhager TK, Van den Broek WW. Fatal interaction between tranylcypromine and imipramine. Eur Psychiatry. 2003;18:264–265. doi: 10.1016/s0924-9338(03)00090-7. [DOI] [PubMed] [Google Scholar]
- Peter C, Hongwan D, Kuepfer A, Lauterburg BH. Pharmacokinetics and organ distribution of intravenous and oral methylene blue. Eur J Clin Pharmacol. 2000;56:247–250. doi: 10.1007/s002280000124. [DOI] [PubMed] [Google Scholar]
- Ramsay RR. Kinetic mechanism of Monoamine Oxidase-A. Biochemistry. 1991;30:4624–4629. doi: 10.1021/bi00232a038. [DOI] [PubMed] [Google Scholar]
- Ramsay RR, Gravestock MB. Monoamine oxidases: to inhibit or not to inhibit. Mini-Rev Med Chem. 2003;3:129–136. doi: 10.2174/1389557033405287. [DOI] [PubMed] [Google Scholar]
- Ramsay RR, Hunter DJB. Inhibitors alter the spectrum and redox properties of monoamine oxidase A. BBA—Proteins Proteomics. 2002;1601:178–184. doi: 10.1016/s1570-9639(02)00466-1. [DOI] [PubMed] [Google Scholar]
- Ramsay RR, Koerber SC, Singer TP. Stopped-flow studies on the mechanism of oxidation of N-methyl-4-phenyltetrahydropyridine by bovine liver Monoamine Oxidase-B. Biochemistry. 1987;26:3045–3050. doi: 10.1021/bi00385a015. [DOI] [PubMed] [Google Scholar]
- Rosenbaum H. January 2006 Case of the Month. 2006.
- Shumakovich GP, Dubova LG, Byzova NA, Yaropolov AI, Bachurin SO. Efficient artificial electron acceptors for monoamino oxidase in bioelectrooxidation of monoamines: Phenothiazine dyes. Russ J Electrochem. 2004;40:963–968. [Google Scholar]
- Tan AK, Ramsay RR. Substrate-specific enhancement of the oxidative half-reaction of Monoamine-Oxidase. Biochemistry. 1993;32:2137–2143. doi: 10.1021/bi00060a003. [DOI] [PubMed] [Google Scholar]
- Whyte IM, Dawson AH, Buckley NA. Relative toxicity of venlafaxine and selective serotonin reuptake inhibitors in overdose compared to tricyclic antidepressants. QJM—An Int J Med. 2003;96:369–374. doi: 10.1093/qjmed/hcg062. [DOI] [PubMed] [Google Scholar]
- Whyte IM.Serotonin Toxicity (Syndrome) Medical Toxicology 2004Lippincott Williams & Wilkins: Baltimore, USA; 103–106.In: Dart RC (ed) [Google Scholar]
- Wouters J. Structural aspects of monoamine oxidase and its reversible inhibition. Curr Med Chem. 1998;5:137–162. [PubMed] [Google Scholar]
- Yamamoto S, Kobashi S, Tsutsui KI, Sueishi Y. Spectroscopic studies of the interaction between methylene blue-naphthol orange complex and anionic and cationic surfactants. Spectroc Acta Pt A—Molec Biomolec Spectr. 2007;66:302–306. doi: 10.1016/j.saa.2006.02.056. [DOI] [PubMed] [Google Scholar]
- Youdim MBH, Edmondson D, Tipton KF. The therapeutic potential of monoamine oxidase inhibitors. Nat Rev Neurosci. 2006;7:295–309. doi: 10.1038/nrn1883. [DOI] [PubMed] [Google Scholar]
- Zonneveld AM, Hagenaars M, Voermans NC, Gelissen HP, Claassen JA. Life-threatening serotonin syndrome following a single dose of a serotonin reuptake inhibitor during maintenance therapy with a monoamine oxidase inhibitor. Ned Tijdschr Geneeskd. 2006;150:1081–1084. [PubMed] [Google Scholar]