Abstract
Recent studies suggested a predominant role of spinopelvic parameters to explain lumbosacral spondylolisthesis pathogeny. We compare the pelvic incidence and other parameters of sagittal spinopelvic balance in adolescents and young adults with developmental spondylolisthesis to those parameters in a control group of healthy volunteers. We compared the angular parameters of the sagittal balance of the spine in a cohort of 244 patients with a developmental L5–S1 spondylolisthesis with those of a control cohort of 300 healthy volunteers. A descriptive and correlation study was performed. The L5 anterior slipping and lumbosacral kyphosis in spondylolisthesis patients was described using multiple regression analysis study. Our study demonstrates that the related measures of sagittal spinopelvic alignment are disturbed in adolescents and young adults with developmental spondylolisthesis. These subjects stand with an increased sacral slope, pelvic tilt and lumbar lordosis but with a decreased thoracic kyphosis. Pelvic incidence was significantly higher in spondylolisthesis patients as compared with controls but was not clearly correlated with the grade of slipping. We showed the same “sagittal balance strategy” in spondylolisthesis patients as in the control group regarding correlations between pelvic incidence, sacral slope, pelvic tilt and lumbar lordosis. We believe that the lumbosacral kyphosis is a stronger factor than pelvic incidence which need to be taken into account as a predominant factor in theories of pathogenesis of lumbosacral spondylolithesis. We thus believe that increased lumbar lordosis associated with L5–S1 spondylolisthesis is secondary to the high pelvic incidence and is an important factor causing high shear stresses at the L5–S1 pars interarticularis. However, the “local” sagittal imbalance of the lumbosacral junction is compensated by adjacent mobile segments in the upper lumbar spine, the pelvis orientation and the thoracic spine. The result is not optimal but a satisfactory global sagittal balance of the trunk, even in the most severe grade of slipping.
Keywords: High-grade spondylolisthesis, Sagittal balance of the trunk, Pelvic incidence, Lumbosacral kyphosis
Introduction
Differences in the anatomic development of the spine and the pelvis may cause individual variation in vertebropelvic alignment. Studies have confirmed that some structural features of the pelvis modulate and largely determine the amount of standing lumbar lordosis, as well as the sagittal pelvic alignment and spinopelvic balance [3, 5, 13, 22]. These relationships have been documented in adult volunteers [3–8, 22] and in patients with spinal disorders. The most important roentgenographic parameters of the sagittal balance of the spine in upright posture are well defined, and their normal physiological values have been reported [13, 22]. These stable relationships are disturbed in pathological conditions such as spondylolisthesis but few studies have addressed sagittal balance of the spine in spondylolisthesis patients [2, 11, 12, 17]. Numerous radiographic measurements have been proposed to quantify this abnormal anatomic relationship between L5 and S1, such as percentage of listhesis, slip angle, and lumbosacral kyphosis. Unfortunately, none of these measurements reliably predict the outcome of spondylolisthesis. Legaye et al. [13] have described pelvic incidence (PI) as a fundamental pelvic anatomic parameter that is specific and constant for each individual and determines pelvic orientation as well as the size of lumbar lordosis (LL). Recent studies [10–12, 17] have suggested an association between an increased PI and the presence of L5–S1 isthmic spondylolisthesis in adults and adolescents, but this relationship has not been fully explored.
The purpose of this work was to compare the PI and other parameters of sagittal spinopelvic balance in adolescents and young adults with developmental spondylolisthesis to those parameters in a control group of healthy volunteers.
Material and methods
Spondylolisthesis patients
Patients with a developmental L5–S1 spondylolisthesis according to the classification of Marchetti and Bartholozzi [16], were recruited into the study. These patients came from five paediatric orthopaedics centers. The same radiographic protocol was used at all participating institutions. All patients gave informed consent. Ethics commission approval was granted before commencement of this project
Control group
Healthy volunteers were enrolled in a previously published study [22] on sagittal balance of the spine. Three hundred subjects volunteered and were accepted into the study. Inclusion criteria included: age between 20 and 70 years, no previous history of spinal disorders or spinal surgery, no radiographic abnormality detected prior or during the study (i.e. isthmic lysis, spondylolisthesis or spinal abnormality), no significant lower extremity joint pathology (i.e. hip, knee, ankle). Volunteers were informed of the risks and benefits of participating in the study and gave informed consent.
Radiographic protocol
For each patient, one standing lateral radiograph of the spine was obtained in a standardized fashion. The same protocol was used for radiographs of the control group subjects. A vertical 30 × 90-cm film was used with a constant distance between the subject and the X-ray source, The subject assumed a comfortable standing position with the knees fully extended and upper limbs raised horizontally forward at 45° of flexion at the shoulder resting on two arm supports). The central ray was centred on the 12th thoracic vertebra and the film was exposed during inspiration. The complete axial skeleton between the external auditory ducts and superior third of the femurs was visualized in these films.
All measurements were performed by means of the Spineview® software package (Surgiview, 64, rue Tiquetonne, 75002 Paris, France) which was validated in a previous study [20].
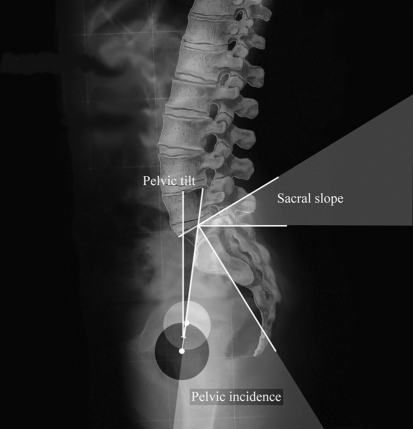
On each lateral radiograph, three pelvic parameters were measured (Fig. 1). The sacral slope (SS) is the angle between the horizontal line and the cranial sacral endplate tangent. The pelvic tilt (PT) is the angle between the vertical line and the line joining the middle of the sacral plate to the center of the bicoxo-femoral axis. The pelvic incidence (PI) is the angle between the line perpendicular to the middle of the cranial sacral endplate and the line joining the middle of the cranial sacral endplate to the center of the bicoxo-femoral axis.
Fig. 1.
Three spinopelvic paramters were measured: The Pelvic incidence (PI), the Sacral slope (SS) and the Pelvic tilt (PT)
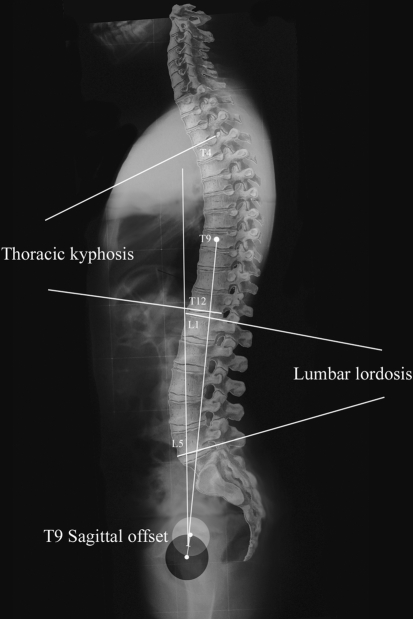
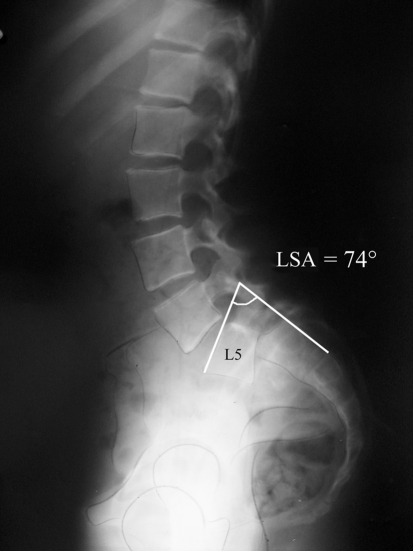
On each lateral radiograph, four spinal parameters were also measured (Fig. 2). The lumbar lordosis (LL) is the angle between the cranial endplate of L1 and the caudal endplate of L5. The thoracic kyphosis (TK) is the angle between the cranial endplate of T4 and the caudal endplate of T12. The T9 sagittal offset (T9SO) is the angle between the vertical plumb line and the line between the center of the vertebral body of T9 and the center of the bicoxo-femoral axis. The degree of L5 anterior slip (L5S) was measured and grades were defined according to Meyerdings’ classification [18]. We considered “grade 5” complete spondyloptosis of L5. The lumbosacral kyphosis was evaluated by the “lumbosacral” angle (LSA) which is the reciprocal of the slip angle described by Boxall [1] (Fig. 3).
Fig. 2.
The Lumbar lordosis (LL) between L1 and L5, the Thoracic kyphosis (TK) between T4 and T12 and the T9 sagittal offset (T9SO) were measured
Fig. 3.
The Lumbosacral angle (LSA) was used to evaluate the lumbosacral kyphosis
Statistical analysis
The data was analyzed by the use of the SPSS® software (SPSS Inc. Chicago, Illinois, USA).
Our analysis was conducted in four steps. We first performed a descriptive analysis of the demographic and morphological parameters of the cohort. Second we calculated the mean value, standard deviation, standard error and range of the angular parameters previously defined, Third, we studied variations of all parameters according to each other using ANOVA study and reciprocal correlations using unpaired t test using correction to account for multiple testing. Finally, we explored the relationships between the two main descriptive parameters of lumbosacral spondylolisthesis (L5S and LSA) and other parameters using multivariate linear regression and principal components analysis.
Results
A total of 244 patients with a developmental lumbosacral spondylolisthesis were enrolled in the study. There were 86 males and 158 females aged from 6 to 25 years (mean 13.9 years). Data from these patients was compared to the control group which was composed of 300 volunteers (110 women and 190 men) with a mean age of 35 years (range 20–70 years). The values of angular parameters in both groups are reported in Table 1. The distribution of each angular parameter was normal (gaussian). Statistical comparison between the groups using unpaired t tests for equality of means showed that pelvic incidence, sacral slope, pelvic tilt, lumbar lordosis and T1 sagittal offset were significantly higher in patients with spondylolisthesis. The angular values of lumbosacral angle, thoracic kyphosis and T9 sagittal offset were significantly lower in patients with spondylolisthesis.
Table 1.
Details of the unpaired t test study for angular variables between spondylolisthesis and control patients
| Variable | Group | N | Mean (°) | SD | SEM | t value | P |
|---|---|---|---|---|---|---|---|
| AGE | Control | 300 | 35.37 | 12.13 | 0.70 | 50.498 | <0.0001 |
| Spondylolisthesis | 244 | 13.86 | 2.83 | 0.21 | |||
| LSA | Control | 300 | 109.94 | 7.18 | 0.41 | 21.146 | <0.0001 |
| Spondylolisthesis | 244 | 82.32 | 21.17 | 1.35 | |||
| SS | Control | 300 | 41.86 | 8.38 | 0.48 | −5.229 | <0.0001 |
| Spondylolisthesis | 244 | 46.57 | 12.55 | 0.80 | |||
| PT | Control | 300 | 13.21 | 6.09 | 0.35 | −18.007 | <0.0001 |
| Spondylolisthesis | 244 | 26.53 | 10.88 | 0.69 | |||
| PI | Control | 300 | 54.67 | 10.65 | 0.61 | −19.466 | <0.0001 |
| Spondylolisthesis | 244 | 73.05 | 11.30 | 0.72 | |||
| T9SO | Control | 300 | −10.35 | 3.05 | 0.17 | −10.580 | <0.0001 |
| Spondylolisthesis | 244 | −6.38 | 5.16 | 0.38 | |||
| T1SO | Control | 300 | −1.34 | 2.64 | 0.15 | 4.357 | <0.0001 |
| Spondylolisthesis | 244 | −3.49 | 4.92 | 0.75 | |||
| LL | Control | 300 | −43.13 | 11.20 | 0.64 | 21.624 | <0.0001 |
| Spondylolisthesis | 244 | −70.22 | 17.30 | 1.16 | |||
| TK | Control | 300 | 40.66 | 10.27 | 0.59 | 11.996 | <0.0001 |
| Spondylolisthesis | 244 | 23.09 | 20.81 | 1.69 |
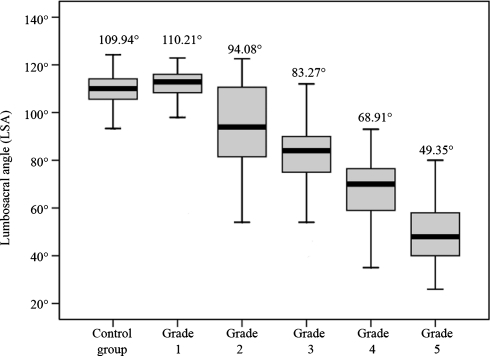
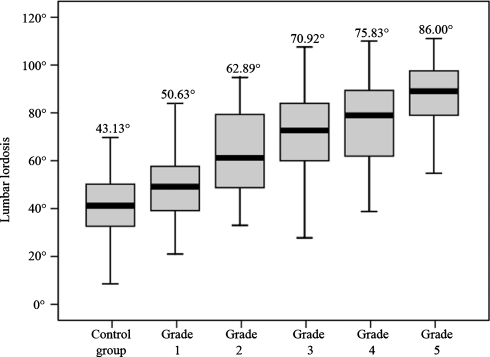
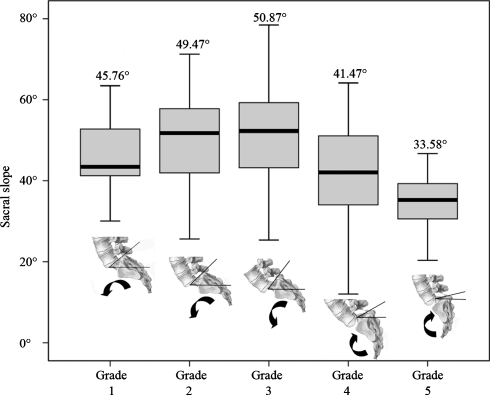
Regarding the severity of spondylolisthesis, 27 patients were classified as Meyerding’s grade 1, 43 patients as grade 2, 98 patients as grade 3, 59 patients as grade 4 and 17 patients as grade 5. There was a significant correlation between lumbosacral angle and the severity of L5 anterior slipping (Fig. 4). We also found a significant correlation between lumbar lordosis (Fig. 5), pelvic tilt, and the severity of L5 anterior slipping. For other variables, the correlation with the grade of slip was not the same for the five grades of slipping. The details of the ANOVA study of these correlations are reported in Table 2.
Fig. 4.
Graphic representation of the Lumbosacral angle (LSA) mean values according to the grade of slipping (ANOVA study)
Fig. 5.
Graphic representation of the Lumbar lordosis (LL) mean values according to the grade of slipping (ANOVA study)
Table 2.
Details of the ANOVA study of angular parameters in both control group and spondylolisthesis patients according to the grade of slipping
| Variable | Group | N | Mean (°) | SD | SE | ANOVA study | |
|---|---|---|---|---|---|---|---|
| F | P | ||||||
| ALS | Control group | 300 | 109.94 | 7.18 | 0.41 | 250.256 | <0.0001 |
| Grade 1 | 27 | 110.21 | 12.66 | 2.44 | |||
| Grade 2 | 43 | 94.08 | 18.86 | 2.88 | |||
| Grade 3 | 98 | 83.28 | 14.13 | 1.43 | |||
| Grade 4 | 59 | 68.92 | 14.03 | 1.83 | |||
| Grade 5 | 17 | 49.35 | 13.56 | 3.29 | |||
| SS | Control group | 300 | 41.86 | 8.38 | 0.48 | 19.568 | <0.0001 |
| Grade 1 | 27 | 45.76 | 10.59 | 2.04 | |||
| Grade 2 | 43 | 49.47 | 11.06 | 1.69 | |||
| Grade 3 | 98 | 50.87 | 11.76 | 1.19 | |||
| Grade 4 | 59 | 41.47 | 12.14 | 1.58 | |||
| Grade 5 | 17 | 33.58 | 10.26 | 2.49 | |||
| PT | Control group | 300 | 13.21 | 6.10 | 0.35 | 112.443 | <0.0001 |
| Grade 1 | 27 | 16.22 | 5.58 | 1.07 | |||
| Grade 2 | 43 | 22.70 | 10.11 | 1.54 | |||
| Grade 3 | 98 | 24.94 | 9.62 | 0.97 | |||
| Grade 4 | 59 | 33.46 | 9.58 | 1.25 | |||
| Grade 5 | 17 | 37.75 | 6.40 | 1.55 | |||
| IP | Control group | 300 | 54.68 | 10.66 | 0.62 | 86.999 | <0.0001 |
| Grade 1 | 27 | 62.87 | 12.35 | 2.38 | |||
| Grade 2 | 43 | 71.29 | 11.66 | 1.78 | |||
| Grade 3 | 98 | 75.81 | 10.48 | 1.06 | |||
| Grade 4 | 59 | 74.92 | 9.17 | 1.19 | |||
| Grade 5 | 17 | 71.33 | 10.91 | 2.65 | |||
| T9SO | Control group | 300 | −10.35 | 3.06 | 0.18 | 30.052 | <0.0001 |
| Grade 1 | 27 | −10.06 | 2.38 | 0.46 | |||
| Grade 2 | 43 | −6.32 | 5.43 | 0.83 | |||
| Grade 3 | 98 | −5.88 | 5.88 | 0.77 | |||
| Grade 4 | 59 | −4.80 | 4.31 | 0.71 | |||
| Grade 5 | 17 | −5.89 | 4.35 | 1.12 | |||
| T1SO | Control group | 300 | −1.35 | 2.65 | 0.15 | 6.874 | <0.0001 |
| Grade 1 | 27 | −2.45. | 2.65 | 0.23 | |||
| Grade 2 | 43 | −3.56 | 3.32 | 0.56 | |||
| Grade 3 | 98 | -2.96 | 5.50 | 1.15 | |||
| Grade 4 | 59 | −4.29 | 4.16 | 1.20 | |||
| Grade 5 | 17 | −3.85 | 4.61 | 1.63 | |||
| LL | Control group | 300 | −43.14 | 11.21 | 0.65 | 132.813 | <0.0001 |
| Grade 1 | 27 | −50.64 | 14.47 | 2.79 | |||
| Grade 2 | 43 | −62.90 | 17.51 | 4.02 | |||
| Grade 3 | 98 | −70.93 | 14.82 | 1.50 | |||
| Grade 4 | 59 | −75.83 | 14.86 | 1.93 | |||
| Grade 5 | 17 | −86.01 | 13.67 | 3.32 | |||
| TK | Control group | 300 | 40.66 | 10.27 | 0.59 | 48.063 | <0.0001 |
| Grade 1 | 27 | 37.74 | 12.21 | 2.35 | |||
| Grade 2 | 43 | 36.20 | 9.01 | 2.07 | |||
| Grade 3 | 98 | 18.37 | 26.69 | 3.57 | |||
| Grade 4 | 59 | 13.21 | 10.67 | 1.86 | |||
| Grade 5 | 17 | 19.55 | 13.81 | 3.57 | |||
The matrix of correlations (Table 3) among the main spinal and pelvic parameters in spondylolisthesis patients (Pearson correlation coefficient) highlights statistically significant positive correlations between parameters including the degree of slip and the lumbosacral kyphosis (Lumbosacral angle), and the pelvic tilt and the Lumbar lordosis. Negative correlations were noted between L5 anterior slipping and several parameters including PI, Thoracic kyphosis (TK), Sacral slope (SS) and T9 sagital offset (T9SO).
Table 3.
Correlation matrix of angular parameters in spondylolisthesis patients (italics) and in control patients (normal)
| LSA | SS | PT | PI | T9SO | T1SO | LL | TK | ||
|---|---|---|---|---|---|---|---|---|---|
| Slip | R/p spl |
−0.742 <0.0001 |
−0.235 <0.0001 |
0.530 <0.0001 |
0.247 <0.0001 |
0.250 0.001 |
−0.109 0.485 |
−0.534 <0.0001 |
−0.364 <0.0001 |
| LSA | R/p spl |
0.384 <0.0001 |
0.626 −<0.0001 |
−0.163 0.011 |
−0.274 <0.0001 |
−0.014 0.929 |
0.521 <0.0001 |
0.277 0.001 |
|
| R/p control | 0.818 <0.0001 |
0.083 0.151 |
0.665 <0.0001 |
0.312 <0.0001 |
0.151 0.009 |
−0.465 <0.0001 |
−0.043 0.456 |
||
| SS | R/p spl |
−0.508 <0.0001 |
0.606 <0.0001 |
0.176 0.018 |
0.307 0.046 |
0.214 −0.001 |
0.118 0.150 |
||
| R/p control | 0.104 0.072 |
0.805 <0.0001 |
0.214 <0.0001 |
0.098 0.089 |
−0.747 <0.0001 |
0.060 0.302 |
|||
| PT | R/p spl |
0.359 <0.0001 |
0.097 0.193 |
−0.082 0.601 |
−0.245 <0.0001 |
−0.266 0.001 |
|||
| R/p control | 0.650 <0.0001 |
−0.369 <0.0001 |
0.015 0.800 |
−0.219 <0.0001 |
−0.062 0.282 |
||||
| PI | R/p spl |
0.274 <0.0001 |
0.280 0.069 |
−0.454 <0.0001 |
−0.133 0.105 |
||||
| R/p control |
−0.45 0.441 |
0.100 0.084 |
−0.670 <0.0001 |
−0.005 0.928 |
|||||
| T9SO | R/p spl |
0.935 <0.0001 |
−0.108 0.179 |
−0.516 <0.0001 |
|||||
| R/p control | 0.654 <0.0001 |
0.021 0.720 |
−0.410 <0.0001 |
||||||
| T1SO | R/p spl |
0.125 0.425 |
−0.420 0.005 |
||||||
| R/p control | 0.063 0.280 |
−0.062 0.284 |
|||||||
| LL | R/p spl |
0.064 0.439 |
|||||||
| R/p control |
−0228 <0.0001 |
||||||||
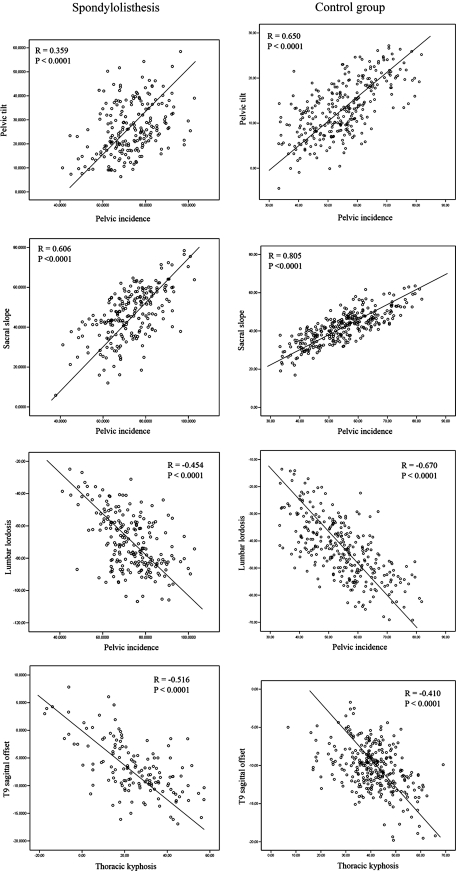
We noted the same pattern of negative correlation between spondylolisthesis patients and control group subjects regarding PI and SS, PT and PI, PI and LL, TK and T9SO (Fig. 6). However, the negative correlations were statistically less in spondylolisthesis patients than in control subjects regarding SS and LL (R = -0.214 vs. R = -0.747), PT and PI (R = 0.359 vs. R = 0.650) and PI and LL (R = -0.454 vs. R = -0.670).
Fig. 6.
Graphic representation of the relevant correlations between angular parameters in both (control and spondylolisthesis) groups
Multivariate regression analysis showed that variations in lumbosacral kyphosis (lumbosacral angle) could be explained by the associations of L5 anterior slipping, Sacral slope, Lumbar lordosis and T9 sagittal offset variations. The multivariate analysis of the L5 anterior slipping showed that its variations could be explained by the lumbosacral angle variations alone. Other angular parameters were excluded from the model. The details regarding the multivariate regression analysis are summarized in Table 4.
Table 4.
Simple and multivariate linear correlations between the main spinal and pelvic parameters, the degree of slip and the lumbosacral kyphosis (Lumbosacral angle)
| Linear regression models | r | R2 | β SE |
|---|---|---|---|
| LSA = 95.174 − 0.391L5S + 0.667 SS + 0.392 LL − 0.713 T9SO | 0.812 | 0.660 | Cst : 13.124 L5S : 0.114 SS : 0.172 LL : 0.123 T9SO : 0.288 |
| L5S = 121.351 − 0.713 LSA | 0.692 | 0.479 | Cst : 8.35 LSA : 0.116 |
These linear regression models describe the reciprocal relationship between these angular parameters through mathematical equations
β SE Beta coefficient standard error, Cst Constant, L5S L5 anterior slipping, SS Sacral slope, LL L1L5 lumbar lordosis, T9SO T9 sagittal offset, LSA Lumbosacral angle
Discussion
In a previous study, we proposed a physiological standard for several angular pelvic and spinal parameters that describe spinal balance base on measurements from a cohort of 300 volunteers [22]. Those measurements were facilitated by the use of a data processing software, the Spineview® software package, that enabled a rapid and precise measurement of all angular parameters on digitalized radiographs.
After studying sagital balance of the spine in asymptomatic subjects, we found it necessary to explore the sagittal balance of the spine in patients with pathological conditions. Because lumbosacral spondylolisthesis appeared as being an isolated sagittal imbalance of the lumbosacral junction, we designed the current study.
Some authors experienced technical difficulties when performing PI, SS and PT measurement on patients with high-grade spondylolisthesis because of sacral endplate dystrophic changes. In a recent study, we demonstrated the reliability and repeatability of the Spineview® software in patients with high-grade spondylolisthesis [21]. We believe it is necessary that standardized, precise and defined techniques of measurement be used.
Relatively little is known about the importance of spinopelvic parameters in human musculoskeletal disorders. An association between PI and spondylolisthesis has been reported in recent publications [10–12, 17]. Curylo et al. [2] noted an increased PI in 53 patients with spondyloptosis. In a cohort of 39 subjects with spondylolysis and low-grade (I or II) spondylolisthesis, Marty et al. [17] noted a greater PI and SS, and postulated (as have Labelle et al. [11, 12]) that this increased PI could predispose to spondylolisthesis, since PI is specific and remains constant for each individual after childhood. The same findings were reported by Rajnic et al. [19] in a cohort of 48 adults with low-grade isthmic. In addition, Hanson et al. [9] reported that PI was significantly higher in 40 patients with spondylolisthesis as compared with controls and PI was correlated with the grade of slipping. They were, however, unable to detect changes with LL or SS, probably because of their relatively small sample size. Two recent papers from Labelle et al. [11, 12] who studied a large cohort of spondylolisthesis patients confirm, as our results do, that PI is significantly increased in adolescents and young adults with L5–S1 developmental spondylolisthesis as compared to healthy volunteers.
It is interesting to note that the male/female ratio is different in both groups of our cohort with more female in the olisthetic group. A possible cause is higher PI in young female patients than in males, as we have reported in a previous study [22]. As Labelle et al. [11, 12], we fully recognize that there was a difference in age between our spondolisthesis cohort and our asymptomatic volunteers used for comparison. However, we believe our conclusion, little affected by this difference despite in normal individuals the PI gradually increasing with age from the onset of walking to late childhood [14, 15]. Other studies have suggested that this parameter increase with age but remain stable after the age of 10 [17].
Our study demonstrates that the related measures of sagittal spinopelvic alignment (SS, PT, LL, and TK) are disturbed in adolescents and young adults with developmental spondylolisthesis. These subjects stand with an increased SS, PT, and LL, but with decreased TK. Regarding SS variations, we found that SS gradually increase with Grade I, II and III slip and decrease in grade 4 and 5 (Fig. 7). We postulate that this phenomenon is secondary to forces on the cranial sacral endplate in grade 1, 2 and 3 patients. In Grade 4 and 5 patients, the loss of contact between the L5 vertebra and the sacral cranial endplate is responsible for a progressive sacral and pelvic retroversion. This phenomenon explains the vertical sacrum pattern in high-grade spondylolisthesis patients [23].
Fig. 7.
Graphic representation of the Sacral slope (SS) mean values according to the grade of slipping (ANOVA study). In Grade 4 and 5 patients, the loss of contact between the L5 vertebra and the sacral cranial endplate is responsible for a progressive sacral and pelvic retroversion. This phenomenon explains the vertical sacrum pattern in high-grade spondylolisthesis patients
Because PI could be considered as an anatomical parameter, we postulate that SS, PT and LL modifications are compensation phenomenon due to PI increase in spondylolisthesis patients. We showed the same “sagittal balance strategy” in spondylolisthesis patients as in the control group regarding negative correlations between PI and SS, and PT and LL. Contrary to Labelle [11, 12], we found the decrease of thoracic kyphosis in spondylolisthesis patients not being a logical compensation phenomenon due to LL increase. Our explanation of these TK values is that, because of trunk anterior displacement associated with L5 anterior slipping, TK is decreased to avoid the trunk line of gravity being displaced anteriorly to the femoral heads. As During [3], Legaye [13], and Duval-Beaupère [5], we postulate that the T9 sagittal offset is a good indicator of the position of the gravity center of the trunk above the femoral heads and therefore of the sagittal balance of the subject. We noted in this study a significant correlation between T9SO and TK in spondylolisthesis patients, higher than in control group (R = −0.516 vs. R = -0.410).
Multivariate linear correlations showed the twinning of both lumbosacral kyphosis (the lumbosacral angle) and L5 anterior slipping to describe the severity of lumbosacral spondylolisthesis. All the other angular parameters, even PI, were excluded from the model. Regarding the lumbosacral kyphosis severity, SS, LL and T9SO were influencing variables. We disagree with Labelle [11, 12] regarding the direct correlation of PI with the severity of L5–S1 developmental spondylolisthesis for several reasons. First, we experienced the same difficulties in proving this linear correlation between PI and the grade of slipping especially for high-grade patients. Second, the lumbosacral kyphosis is a stronger factor and we stress the importance of taking it into account as a predominant factor in theories of pathogenesis. However, we support the concept that a high PI is a predisposing factor of L5–S1 spondylolisthesis because high PI will necessarily predispose to a high SS and/or PT since PI is the arithmetic summation of SS and PT, and a high SS predisposes to a high LL in an attempt of the trunk to compensate and maintain the trunk centered over the femoral heads. We thus believe that this higher than normal LL associated with L5–S1 spondylolisthesis is secondary to the high PI and is an important factor causing high shear stresses at the L5–S1 pars interarticularis. However, the “local” sagittal imbalance of the lumbosacral junction is compensated by adjacent mobile segments in the upper lumbar spine, the pelvis orientation and the thoracic spine. The result is a not optimal but a satisfactory global sagittal balance of the trunk, even in the most severe grade of slipping.
References
- 1.Boxall D, Bradford DS, Winter RB, Moe JH. Management of severe spondylolisthesis in children and adolescents. J Bone Joint Surg Am. 1979;61:479–495. [PubMed] [Google Scholar]
- 2.Curylo LJ, Edwards C, DeWald RW. Radiographic markers in spondyloptosis: implications for spondylolisthesis progression. Spine. 2002;27:2021–2025. doi: 10.1097/00007632-200209150-00010. [DOI] [PubMed] [Google Scholar]
- 3.During J, Goudfrooij H, Keessen W, Beeker TW, Crowe A. Toward standards for posture. Postural characteristics of the lower back system in normal and pathologic conditions. Spine. 1985;10:83–87. doi: 10.1097/00007632-198501000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Duval-Beaupere G, Robain G. Visualization on full spine radiographs of the anatomical connections of the centres of the segmental body mass supported by each vertebra and measured in vivo. Int Orthop. 1987;11:261–269. doi: 10.1007/BF00271459. [DOI] [PubMed] [Google Scholar]
- 5.Duval-Beaupere G, Schmidt C, Cosson P. A Barycentremetric study of the sagittal shape of spine and pelvis: the conditions required for an economic standing position. Ann Biomed Eng. 1992;20:451–462. doi: 10.1007/BF02368136. [DOI] [PubMed] [Google Scholar]
- 6.Gelb DE, Lenke LG, Bridwell KH, Blanke K, McEnery KW. An analysis of sagittal spinal alignment in 100 asymptomatic middle and older aged volunteers. Spine. 1995;20:1351–1358. doi: 10.1097/00007632-199506000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Guigui P, Levassor N, Rillardon L, Wodecki P, Cardinne L. [Physiological value of pelvic and spinal parameters of sagital balance: analysis of 250 healthy volunteers]. Rev Chir Orthop Reparatrice Appar Mot. 2003;89:496–506. [PubMed] [Google Scholar]
- 8.Hammerberg EM, Wood KB. Sagittal profile of the elderly. J Spinal Disord Tech. 2003;16:44–50. doi: 10.1097/00024720-200302000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Hanson DS, Bridwell KH, Rhee JM, Lenke LG. Correlation of pelvic incidence with low- and high-grade isthmic spondylolisthesis. Spine. 2002;27:2026–2029. doi: 10.1097/00007632-200209150-00011. [DOI] [PubMed] [Google Scholar]
- 10.Jackson RP, Phipps T, Hales C, Surber J. Pelvic lordosis and alignment in spondylolisthesis. Spine. 2003;28:151–160. doi: 10.1097/00007632-200301150-00011. [DOI] [PubMed] [Google Scholar]
- 11.Labelle H, Roussouly P, Berthonnaud E, Dimnet J, O’Brien M. The importance of spino-pelvic balance in L5-s1 developmental spondylolisthesis: a review of pertinent radiologic measurements. Spine. 2005;30:S27–S34. doi: 10.1097/01.brs.0000155560.92580.90. [DOI] [PubMed] [Google Scholar]
- 12.Labelle H, Roussouly P, Berthonnaud E, Transfeldt E, O’Brien M, Chopin D, et al. Spondylolisthesis, pelvic incidence, and spinopelvic balance: a correlation study. Spine. 2004;29:2049–2054. doi: 10.1097/01.brs.0000138279.53439.cc. [DOI] [PubMed] [Google Scholar]
- 13.Legaye J, Duval-Beaupere G, Hecquet J, Marty C. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998;7:99–103. doi: 10.1007/s005860050038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.MacThiong JM, Labelle H, Berthonnaud E, Betz RR, Roussouly P. Sagittal spinopelvic balance in normal children and adolescents. Eur Spine J. 2005;26:1–8. doi: 10.1007/s00586-005-0013-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mangione P, Gomez D, Senegas J. Study of the course of the incidence angle during growth. Eur Spine J. 1997;6:163–167. doi: 10.1007/BF01301430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marchetti P, Bartolozzi P. Le spondylolistesi: classificazione et etiopathogenesi. Prog Pat Vert. 1984;6:9. [Google Scholar]
- 17.Marty C, Boisaubert B, Descamps H, Montigny JP, Hecquet J, Legaye J, et al. The sagittal anatomy of the sacrum among young adults, infants, and spondylolisthesis patients. Eur Spine J. 2002;11:119–125. doi: 10.1007/s00586-001-0349-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Meyerding HW. Spondylolisthesis; surgical fusion of lumbosacral portion of spinal column and interarticular facets; use of autogenous bone grafts for relief of disabling backache. J Int Coll Surg. 1956;26:566–591. [PubMed] [Google Scholar]
- 19.Rajnics P, Templier A, Skalli W, Lavaste F, Illes T. The association of sagittal spinal and pelvic parameters in asymptomatic persons and patients with isthmic spondylolisthesis. J Spinal Disord Tech. 2002;15:24–30. doi: 10.1097/00024720-200202000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Rillardon L, Levassor N, Guigui P, Wodecki P, Cardinne L, Templier A, et al. [Validation of a tool to measure pelvic and spinal parameters of sagittal balance]. Rev Chir Orthop Reparatrice Appar Mot. 2003;89:218–227. [PubMed] [Google Scholar]
- 21.Vialle R, Ilharreborde B, Dauzac C, Guigui P (2006) Intra and inter-observer reliability of determining degree of pelvic incidence in high-grade spondylolisthesis using a computer assisted method. Eur Spine J [DOI] [PubMed]
- 22.Vialle R, Levassor N, Rillardon L, Templier A, Skalli W, Guigui P. Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J Bone Joint Surg Am. 2005;87:260–267. doi: 10.2106/JBJS.D.02043. [DOI] [PubMed] [Google Scholar]
- 23.Vialle R, Miladi L, Wicart P, Dubousset J. [Surgical treatment of lumbosacral spondylolisthesis with major displacement in children and adolescents: a continuous series of 20 patients with mean 5-year follow-up]. Rev Chir Orthop Reparatrice Appar Mot. 2005;91:5–14. doi: 10.1016/s0035-1040(05)84270-9. [DOI] [PubMed] [Google Scholar]