Abstract
Anterior cervical plate fixation is an approved surgical technique for cervical spine stabilization in the presence of anterior cervical instability. Rigid plate design with screws rigidly locked to the plate is widely used and is thought to provide a better fixation for the treated spinal segment than a dynamic design in which the screws may slide when the graft is settling. Recent biomechanical studies showed that dynamic anterior plates provide a better graft loading possibly leading to accelerated spinal fusion with a lower incidence of implant complications. This, however, was investigated in vitro and does not necessarily mean to be the case in vivo, as well. Thus, the two major aspects of this study were to compare the speed of bone fusion and the rate of implant complications using either rigid- or dynamic plates. The study design is prospective, randomized, controlled, and multi-centric, having been approved by respective ethic committees of all participating sites. One hundred and thirty-two patients were included in this study and randomly assigned to one of the two groups, both undergoing routine level-1- or level-2 anterior cervical discectomy with autograft fusion receiving either a dynamic plate with screws being locked in ap - position (ABC, Aesculap, Germany), or a rigid plate (CSLP, Synthes, Switzerland). Segmental mobility and implant complications were compared after 3- and 6 months, respectively. All measurements were performed by an independent radiologist. Mobility results after 6 months were available for 77 patients (43 ABC/34 CSLP). Mean segmental mobility for the ABC group was 1.7 mm at the time of discharge, 1.4 mm after 3 months, and 0.8 mm after 6 months. For the CSLP- group the measurements were 1.0, 1.8, and 1.7 mm, respectively. The differences of mean segmental mobility were statistically significant between both groups after 6 months (P = 0.02). Four patients of the CSLP-group demonstrated surgical hardware complications, whereas no implant complications were observed within the ABC-group (P = 0.0375). Dynamic plate designs provided a faster fusion of the cervical spine compared with rigid plate designs after prior spinal surgery. Moreover, the rate of implant complications was lower within the group of patients receiving a dynamic plate. These interim results refer to a follow-up period of 6 months after prior spinal surgery. Further investigations will be performed 2 years postoperatively.
Keywords: Cervical Spine, Anterior plates, Implant, Randomized controlled study
Introduction
Anterior cervical discectomy and fusion (ACDF) has first been introduced by Bailey and Badgley [1], Smith and Robinson [20], and Cloward [8] in the 1950s and the early 1960s. Despite minor technical differences, major problems of these surgical techniques have been graft complications (i. e., graft settling, graft compression fractures, graft dislocations, pseudarthrotic segmental healings, and kyphotic segmental deformations) [4–6, 10, 19, 22, 23]. To overcome these graft-related complications, adding an anterior plate to the treated segment was highly recommended [2, 5, 16]. In fact, adding an anterior plate to a cervical spine segment treated with ACDF helped much to markedly reduce subsequent graft-related surgical complications [6, 10]. However, further implant-related complications, such as screw loosening, screw breakage, and plate breakage, did occur by using this particular surgical technique [13, 17]: The incidence of implant-related complications was found to be as high as 22% [17], or even 44% [13]. This however, was mainly related to the fact that screws were not firmly attached to the plate. As a consequence, a rigid plate design, with screws firmly attached to the plate, was developed [14]. This rigid plate design was commonly used and thought to provide sufficient mechanical fixation to the injured segment, and rapid bone healing. However, further investigations showed that rigid plates demonstrated a bothersome tendency to simply detach from the bone [11, 21]. Thus, developing anterior cervical plates in which the screws are not tightly attached to the plate but properly secured against breaking loose seemed to be the next logical step in the development of cervical spine plate designs. This design should allow the screws to glide towards each other in the setting of graft settling. Moreover, the screws are also prevented from loosening by their design [15]. These plates are commonly known as dynamic plates.
Recently, a mechanical study gave evidence that dynamic anterior plates provide better graft loading [3]. This might result in faster fusion and, as a possible consequence, in a lower rate of implant complications. This, however, might not be necessarily the case under “in vivo” conditions.
Thus, the aim of this study was to analyze the speed of fusion and overall implant complications in both dynamic- and rigid plates.
Methods
The study design is prospective, randomized, controlled, and multi-centric having been approved by respective ethic committees of all participating countries. Inclusion- as well as exclusion criteria are summarized in Table 1. Between January 1, 2003 and December 31, 2004, 132 patients were recruited, and randomly assigned to receive either a dynamic plate [15] (study group, n = 69), or a constrained, rigid plate [14] (control group, n = 63) in the setting of anterior cervical plating. All patients gave their written informed consent prior to enrolment into the study at least 24 h before surgery. Patients assigned to the study group underwent a routine anterior cervical discectomy with autograft fusion including a dynamic plate with screws locked in ap - position (ABC plate and screws, Aesculap AG + CoKG, Tuttlingen, Germany). Patients, assigned to the control group, received a rigid plate (CSLP, Synthes, SWitzerland).
Table 1.
Inclusion and exclusion study criteria
| Inclusion criteria | Exclusion criteria |
|---|---|
| Symptomatic degenerative disc disease in level-1 or 2 | Previous c-spine surgery |
| Traumatic discoligamentous injuries | Additional c-spine surgery (i.e. Posterior approach) |
| No previous c-spine surgery | Active or suspected infection |
| Male and non pregnant females | Aids, hepatitis type c |
| Age between 21 and 80 years | Severe osteoporosis |
| Signed informed consent | Known malignancy |
| Mental disease | |
| Sensitivity to one of the device materials | |
| Continuous use of steroids | |
| Pregnant females or females who plan to be pregnant during study |
The CSLP plate is a device for anterior cervical spine fixation in which the screws are tightly locked on to the plate. The ABC plate is a plate with screws locked only in ap direction. However, the screws may glide towards each other. Thus, such a device allows axial settling in response to graft resorption, maintains the graft under load, which is claimed to result in earlier fusions and thus, less hardware complications. Nevertheless, the plate provides segmental stability [3].
Surgery was performed by experienced spine surgeons only. No collars or other external ortheses were given to the patients after the surgery was over. All patients were mobilized directly after surgery.
Radiographic outcome was measured by an independent radiologist identifying segmental mobility and implant complications. Segmental mobility was measured as tip-to-tip distance of the outermost aspects of the spinous processes of the treated vertebrae in full flexion and full extension on standard lateral X-ray films. The difference between both distances in terms of millimeters was used for subsequent statistical analysis. Correction of magnification effects was performed. Implant complications were defined as screw loosening of more than two threads, screw fracture, plate loosening, plate dislocation, and/or plate fracture. These analyses were done at the time of clinical discharge, after 3 and 6 months, respectively. Statistical analysis was performed to detect statistically significant differences between patients of the study and the control group with respect to the outcome defined above. Statistical significance was assumed at P < 0.05.
Results
Patients’ data are summarized in Table 2. Please note, that no statistically significant differences were observed for sex, mean age, incidence of one-level/ two-level disease, level distribution, or indication (trauma, degenerative disc disease) between patients of both groups.
Table 2.
Patients’ data. No statistically significant differences were observed for sex, mean age, 1- or 2-level disease, level distribution, or indication between study- and control group
| Study group | Control group | P value | |
|---|---|---|---|
| Male | 33 | 27 | 0.60 |
| Female | 36 | 36 | |
| Mean Age | 50.1 | 49.5 | 0.76 |
| 1-level | 45 | 46 | 0.35 |
| 2-level | 24 | 17 | |
| C3/4 | 5 | 2 | 0.77 |
| C4/5 | 13 | 11 | |
| C5/6 | 41 | 36 | |
| C6/7 | 27 | 27 | |
| DDD | 62 | 61 | 0.28 |
| Trauma | 7 | 2 |
Segmental mobility results after 6 months were available for 77 patients, 43 of them having received a dynamic plate, 34 of them having received a constrained, rigid plate.
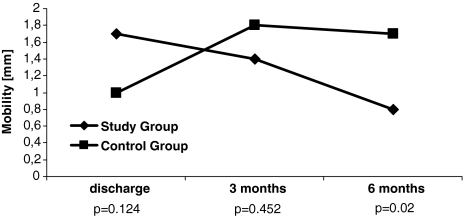
Mean segmental mobility in the study group was 1.7 mm at the time of discharge from the hospital, 1.4 mm after 3 months, and 0.8 mm after 6 months follow-up. As for the control group, the measurements were 1.0, 1.8, and 1.7 mm, respectively. The differences between both groups were statistically significant after 6 months (P = 0.02), but not at the time of discharge from the hospital (P = 0.124), and 3 months after surgery (P = 0.452) (Fig. 1).
Fig. 1.
Differences for mean segmental mobility between both study group (harboring dynamic plate) and control group (harboring a rigid plate). It is important to note that flexibility is increasing within the control group, while decreasing in the study group. This statistically significant difference refers to a 6 months’ time interval after prior spinal surgery
Four patients of the control group demonstrated surgical hardware complications. In one patient a surgical plate broke (Fig. 2), in two patients the lower screws dislocated through the vertebra towards the adjacent intervertebral disc (Fig. 3), and in one patient a lower surgical screw backed out. No implant complications were observed in the study group. Patients in the study group demonstrated less implant complications compared with the control group (P = 0.0375).
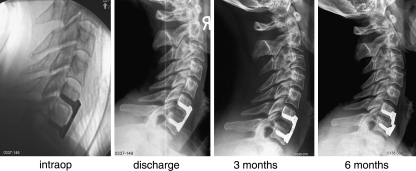
Fig. 2.
Serial radiographs of a patient harboring a rigid plate (CSLP). Both decalcification of the graft over time and plate fracture due to pseudarthrotic healing can be observed
Fig. 3.
Serial lateral radiographs of a patient harboring a rigid plate (CSLP). The lower surgical screws are increasingly cutting through the vertebral bone with time, finally ending up within the intervertebral disc space
Discussion
Aim and results of the study
In this study, we compared the surgical efficacy of an anterior dynamic plate with the effectiveness of an anterior rigid plate in terms of segmental mobility, and implant complications of cervical spine segments up to 6 months after cervical spine surgery. Segmental mobility is significantly lower with the use of anterior dynamic plates being associated with less implant complications, as well.
Biomechanical background
Whereas rigid surgical plates are commonly used, dynamic plates are less frequently used. This may be due to the fact that rigid plates are thought to provide a better fixation to the cervical spine segments. However, a recent in-vitro investigation [9] has shown that this does not necessarily be the case. By using human cervical spine segments, the authors reported dynamic plates to provide better stabilization in terms of spinal extension as compared to a segment having been treated with a rigid plate, especially in the case of an endplate removal during anterior cervical discectomy [9].
Also, graft loading is much more effective by using a dynamic plate compared with the use of rigid plate designs, as shown by Brodke et al. in the setting of a plastic bloc model [3]. As improved mechanical fixation and better loading conditions of the graft were observed with the use of a dynamic device, shorter fusion times and less implant complications could be expected, as well.
Comparison to the literature
The tendency of the CSLP plate after cervical spine surgery to cut through the lower vertebral body of a treated spinal segment is a well-known phenomenon. In 2001, Ulrich described “a tendency for the CSLP plate to break away from the bone” [21]. Half of all implant complications observed in our study were complications of such manner. Kim reported a hardware complication rate to be as low as 0% in case of a dynamic-, and 10% in case of rigid plate fixation, both observed one year after prior spinal surgery [12]. Moreover, in cervical spine surgery, not only rigid implants seem to display a higher rate of complications compared with their dynamic counterparts. A similar parallelism can be found in hip surgery. Chinoy and Parker [7] performed a meta-analysis including 2,855 patients treated with either rigid surgical nails, or dynamic hip screws. They reported that screw cutouts (13% vs. 4%), pseudarthroses (2% vs. 0.5%), screw fractures (14% vs. 0.7%), and the rate of re-operations (10% vs. 4%) were statistically significantly higher with the use of rigid surgical nails.
Limits of the study
For 6 months’ follow-up 41.6% of the data were lost (29 patients having received a rigid plate and 26 patients having received a dynamic plate). Some of these patients did not appear, others refused to receive another X-ray. The difference between the groups concerning missing data, however, is not significant (Fishers Exact test, P = 0,379). Thus, we consider the final conclusion of our study as not having been influenced.
To detect differences going down to 0.1 mm—as it is the case within the control group at the 3 and 6 months’ follow up—one observer could not be sufficient. It would have been interesting if such small differences could have been approved by a second radiologist. However, it is probably more important to check trends within study and control group than to check the data for small changes within each group.
The use of anterior cervical spine plates—whether rigid or dynamic in character—for monosegmental degenerative disease is at least debatable. One may argue that using cervical spine plates in these conditions is an overtreatment including the risk of hardware failure. This gets even truer regarding possibilities available today for cervical spine fixation, including different types of cages especially in degenerative disc disease. However, it was not the aim of the study to highlight the use of plates in cervical spine surgery: the goal was to check the efficacy of the different types of plates, in which the human cervical spine serves as a model.
Clinical relevance
This study examines the use of different surgical plate designs in the clinical setting of cervical spine surgery with most patients having been treated in one spinal segment. The use of anterior plates in cervical spine surgery for degenerative disease is debatable and this is especially true for monosegmental degenerative disease. Although in vitro investigations demonstrated anterior plates to be able to significantly stabilize the spine after prior anterior discectomy and graft insertion [18], the risks of surgical over-treatment entailing additional costs and complications have to be taken into clinical consideration as well. Conversely, the use of anterior plates has been shown to significantly reduce surgical graft complications, such as graft compression fractures, graft resorptions, and/or -dislocations resulting in pathologic kyphotic angulation and/or pseudarthrotic healing [6, 10]. However, whether anterior plating is beneficial for monosegmental fixation of the degenerated cervical spine, was not an objective to be analyzed in this study. If anterior plating is planned to be performed in the setting of cervical spine surgery for a variety of reasons, the use of dynamic plates seems to be more beneficial when compared to plain rigid plate designs. Thus, dynamic plates should be considered to be the preferred treatment option.
Conclusion
Dynamic plate designs provided a faster fusion of the cervical spine compared with rigid plate designs after prior spinal surgery. Moreover, the rate of implant complications is lower within the group of patients receiving a dynamic plate. These interim results refer to a follow-up period of 6 months after prior spinal surgery with no statistically significant differences observed after shorter time intervals.
Financial and industrial disclosure
The study was monitored by N. Borm, Frictionless, Kiel, Germany (not listed among the authors), who was paid by Aesculap, Germany. None of the investigators has a financial interest in one of the implants used within the study. None of the authors was paid for his participation within this study. The hospitals involved here had to pay for the implants used within surgery. T. Pitzen is a Neurosurgeon working at the Department of Neurosurgery, Homburg, Germany. He is also a consultant to Aesculap, Germany.
References
- 1.Bailey RW, Badgley CE. Stabilization of the cervical spine by anterior fusion. Am J Orthop. 1960;42-A:565–594. [PubMed] [Google Scholar]
- 2.Böhler J, Gaudernak T. Anterior plate stabilization for fracture-dislocations of the lower cervical spine. J Trauma. 1980;20:203–205. doi: 10.1097/00005373-198003000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Brodke DS, Gollogly S, Alexander Mohr R, Nguyen BK, Dailey AT, Bachus AK. Dynamic cervical plates: biomechanical evaluation of load sharing and stiffness. Spine. 2001;26:1324–9. doi: 10.1097/00007632-200106150-00010. [DOI] [PubMed] [Google Scholar]
- 4.Brodsky AE, Khalil MA, Sassard WR, Newmann BP. Repair of symptomatic pseudarthrosis of anterior cervical fusion. Posterior versus anterior repair. Spine. 1992;17:1137–1143. doi: 10.1097/00007632-199210000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Caspar W, Barbier D, Klara PM. Anterior cervical fusion and Caspar plate stabilization for cervical trauma. Neurosurgery. 1989;25:491–502. doi: 10.1097/00006123-198910000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Caspar W, Geisler FH, Pitzen T, Johnson TA. Anterior cervical plate stabilization in one- and two-level degenerative disease: overtreatment or benefit? J Spin Disord. 1989;11:1–11. [PubMed] [Google Scholar]
- 7.Chinoy MA, Parker MJ. Fixed nail plates versus sliding hip systems for the treatment of trochanteric femoral fractures: a meta analysis of 14 studies. Injury. 1999;30:157–163. doi: 10.1016/S0020-1383(99)00074-1. [DOI] [PubMed] [Google Scholar]
- 8.Cloward RB. The anterior approach for removal of ruptured discs. J Neurosurg. 1958;15:602–617. doi: 10.3171/jns.1958.15.6.0602. [DOI] [PubMed] [Google Scholar]
- 9.Dvorak MF, Pitzen T, Zhu Q, Gordon JD, Fisher CG, Oxland TR. Anterior cervical plate fixation: a biomechanical study to evaluate the effects of plate design, endplate preparation, and bone mineral density. Spine. 2005;30:294–301. doi: 10.1097/01.brs.0000152154.57171.92. [DOI] [PubMed] [Google Scholar]
- 10.Geisler FH, Caspar W, Pitzen T, Johnson TA. Reoperation in patients after anterior cervical plate stabilization in degenerative disease. Spine. 1998;23:911–920. doi: 10.1097/00007632-199804150-00013. [DOI] [PubMed] [Google Scholar]
- 11.Hofmeister M, Bühren V. Therapiekonzept für Verletzungen der unteren Halswirbelsäule. Orthopäde. 1999;5:401–413. [PubMed] [Google Scholar]
- 12.Kim S, Kim S, Moon S, Choi S. Outcome analysis of patients fusion with locking screw-plate and with dynamic abc screw-plate in degenerative disc disease. Eur Spine J. 2005;14(Suppl):S65. [Google Scholar]
- 13.Lowery GL, McDonough RF. The significance of hardware failure in anterior cervical plate fixation. Patients with 2- to 7-year follow-up. Spine. 1998;23:181–186. doi: 10.1097/00007632-199801150-00006. [DOI] [PubMed] [Google Scholar]
- 14.Morscher E, Sutter F, Jenny H, Olerud S. ) Anterior plating of the cervical spine with the hollow screw-plate system of titanium. Chirurg. 1986;11:702–707. [PubMed] [Google Scholar]
- 15.Omeis I, DeMatta JA, Hillard VH, Murali R, Kaushik D. History of instrumentation for stabilization of the subaxial cervical spine. Neurosurg Focus. 2004;16:1–6. doi: 10.3171/foc.2004.16.1.11. [DOI] [PubMed] [Google Scholar]
- 16.Orozco DR, Llovet TR. Osteosintesis en las lesiones traumaticas y degeneratives de la columna vertebral. Revista Traumatol Chirurg Rehabil. 1971;1:45–52. [Google Scholar]
- 17.Paramore CG, Dickmann CA, Sonntag VK. Radiographic and clinical follow-up review of Caspar plates in 49 patients. J Neurosurg. 1996;84:957–961. doi: 10.3171/jns.1996.84.6.0957. [DOI] [PubMed] [Google Scholar]
- 18.Pitzen T, Wilke HJ, Caspar W, Claes L, Steudel WI. Biomechanical evaluation of a new monocortical screw for anterior cervical fusion and plating by a combined biomechanical and clinical study. Eur Spine J. 1999;8:382–387. doi: 10.1007/s005860050191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Robinson RA, Walker AE, Ferlic DC, Wieking DK. The results of anterior interbody fusion of the cervical spine. J Bone Joint Surg [Am] 1962;44:1569–1587. [Google Scholar]
- 20.Smith GW, Robinson RA. The treatment of cervical spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg (Am) 1958;40:607–624. [PubMed] [Google Scholar]
- 21.Ulrich C, Arand Nothwang M; J. Internal fixation on the lower cervical spine—biomechanics and clinical practice of procedures and implants. Eur Spine J. 2001;10:88–100. doi: 10.1007/s005860000233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.White AA, Southwick WO, Deponte RJ, Gainor JW, Hardy R. Relief of pain by anterior cervical spine fusion for spondylosis: A report of sixty-five patients. J Bone Joint Surg [Am] 1973;55:525–534. [PubMed] [Google Scholar]
- 23.Zdeblick TA, Ducker TB. The use of freeze-dried allograft bone for anterior cervical fusions. Spine. 1991;16:726–729. doi: 10.1097/00007632-199107000-00006. [DOI] [PubMed] [Google Scholar]