Abstract
Spondylolysis is a common entity, a minority of people affected by this disease need medical care, and only a few require surgery. Reconstruction of the pars interarticularis is an interesting alternative to segmental fusion; this technique has the advantage of preserving segmental motion. Most authors report good results for young patients without intervertebral disk or facet degenerative changes. Moreover Louis also showed good to excellent results with his technique carried out among people who presented a satisfactory disk height (equal to two thirds of normal height). This could extend the number of patients for whom pars interarticularis repair could be proposed. In this study, the limit of reconstruction was set at grade 3of the Pfirrmann’s classification. The fixation of the isthmus was done with a new kind of pedicle screw hook system. This stable and strong device is easy to use, allows an anatomic pars interarticularis reconstruction of spondylolysis and avoids a postoperative bracing. Twenty-three patients were assessed in this study, the mean age at operation was 34 (range 16–52 years) and the average follow-up was for 59 months (range 6–113 months). Eight patients showed moderate degenerative disk disease before the surgery and 12 patients had a grade 1 spondylolisthesis. The visual analogical scale, the Oswestry disability index (ODI) and the modified Prolo score were used for assessment of pain and clinical outcome before and after surgery. The results were from “excellent” to “good” for twenty patients (87%) and “fair” for three of them (13%). The consolidation of the isthmus was assessed at the end of the study (CT-scan); the fusion rate was observed in 91%. Among patients aged less than 30 years results are from “good”, to “excellent” in all cases and consolidation was always observed. All of them showed normal disc signal before the surgery. In the group aged more than 30 years, the results varied from “good” to “excellent’ in 73% and fusion of the defect was discovered in 82% of cases. Eight of them (73%) had moderate disk signal modification before the surgery. All people with fair results displayed moderate disk degeneration signs at MRI before surgery; but two of those three patients had a failure of defect consolidation too and it is also associated with poor results by several authors. No complication was found in this series. According to the good results reported by Louis and upto the current finding, the authors believe that pars interarticularis repair can be carried out on patients with moderate degenerative disk disease; the stage 3 of Pfirrmann’s classification seems a good limit. The Bone and joint research (B.J.R. system) is readily usable by any surgeon using pedicle screw systems and having a short learning curve. No device failure has been observed in this series.
Keywords: Pars interarticularis repair, Lumbar spondylolysis, Functional outcome, Surgery, Pedicular screw hook fixation
Introduction
Spondylolysis is a common finding on adult spine radiographies; frequently this fracture occurs during childhood and its discovery is often fortuitous. A minority of these patients experience chronic disabling low back pain, sometimes radiating to the thighs without true sciatica. These people need medical care; conservative measures are often successful but those who remain symptomatic may benefit of surgery [13, 27].
In situ spinal fusion of the involved level is widely accepted as the treatment of symptomatic spondylolysis; good and excellent results are found in 75–100% [13, 27]. Nevertheless, some investigators believe that this fusion has a biomechanical effect on the adjacent unfused spinal segments and can lead to a significant acceleration of pathologic lesions [20, 25]. Reconstruction of the pars interarticularis seems a logical and less aggressive approach than lumbosacral fusion for symptomatic patients mainly when they display no associated slip or degenerative disc disease.
The first to develop this concept as an alternative to segmental fusion was Kimura in 1968 [17]. Since then, different osteosynthesis techniques such as translaminar screw fixation, cerclage wiring loop, tempory fixation (butterfly plate), pedicle screw hook system, rod–screw construct… were developed.
Deguchi compared the biomechanics performance of these various fixation techniques and found that the pedicle screw hook system brings a biomechanical advantage for pseudarthrosis fusion (great stability to the defect during motion) [7].
The goal of the pars defect reconstruction is to obtain the consolidation of the isthmus, to restore the anatomy and the stability of the spine, and to preserve the mobility of the stage concerned. Several authors reported good results with these techniques for young people without spondylolisthesis, evidence of advanced facet arthritis or degenerative disk disease [1, 6, 29, 39]. Moreover, in 1988 Louis [22] reported good results in people who displayed a “satisfactory” disk space (discal height is at least two thirds of its normal height) and a slip inferior to 10 mm. This could extend the number of patients in whom pars interarticularis repair could be contemplated in comparison with the stricter criteria used in other studies.
The objective of this study is to report the results of the treatment for symptomatic spondylolysis in 23 patients by a new pedicle screw hook system (B.J.R. system), to describe the surgical technique, to determine the rate of fusion and to analyze the outcome of patients with an average follow-up of 5 years. According to Louis’ criteria, the surgery was carried out among patients with moderate disk signal modification (T2-weighted MRI). The classification of Pfirrmann was used to assess the vertebral disc signal and the limit of reconstruction was set at the grade 3 [33].
Materials and methods
Patients
Twenty three patients were treated surgically for symptomatic spondylolysis between 1996 and 2005. Each one showed the following criteria: symptomatic bilateral spondylolysis, L4 or L5 localization, disabling pain located in the low back and possibly radiating to the thighs, lack of response to conservative treatment for at least 6 months, no signs of severe degenerative disc disease and no high grade of spondylolisthesis.
The state of the adjacent disk was assessed by magnetic resonance imaging (T2-weighted MRI) and was classified according to the Pfirrmann’s criteria (Table 1). This grading system seems to be a standardized and reliable assessment of MRI disc morphology for research and clinical purposes [33].
Table 1.
Classification of Pfirrmann [33]
| Signal characteristics of the disc in T2-weighted MRI. | |
|---|---|
| Grade 1 | The structure of the disc is homogeneous with a bright hyperintense white signal intensity and normal disc height. |
| Grade 2 | The structure of the disc is inhomogeneous with a hyperintense white signal, the distinction between nucleus and annulus stay clear but a loss of signal intensity in the nucleus is present (correlate with the alteration of the proteoglycans), the disc height is normal with or without horizontal grey bands. |
| Grade 3 | The structure of the disc is inhomogeneous with an intermediate grey signal intensity and an unclear distinction between nucleus and annulus. The disk height is normal or slightly decreased. |
| Grade 4 | The structure of the disc is inhomogeneous, with a hypointense dark grey signal intensity. The distinction between the nucleus and annulus is lost, the disc height is decreased. |
| Grade 5 | The structure of the disc is inhomogeneous, with a hypointense black signal intensity. The distinction between nucleus and annulus is lost, total collapse of the disc space with the presence of intradiscal gas or calcifications. |
The limit for a pars defect reconstruction was set at the grade 3 of this classification (a logical threshold of disease for this technique for us). The vertebral slip was recorded from an upright lateral radiography of the lumbar spine. Before the reconstruction, an infiltration of a long-acting local anaesthetic in the defect was carried out (Marcaine); if pain did not decrease significantly, the surgery was not contemplated.
Litigation, compensation cases, psychological and personality disorders, high grade of spondylolisthesis (>Meyerding grade 1) and severe modification of disk signal (>grade 3 of Pfirrmann) were considered as a procedure contraindication. Each patient was studied according to the age, sex, personal and familial histories, jobs, initial symptoms (type, length, intensity,...), earlier treatments, clinical examination and assessment of imagery (radiography, CT scan and magnetic resonance imaging).
Methods
All patients were followed closely; clinical examination and radiographies were performed 2, 6 and 12 months after the surgery as well as at the end of the study. Moreover, a computed tomography (reverse gantry angle and thin section) was done at the last visit to check the fusion of the pars interarticularis. It was considered to be present when trabeculae across the lytic and the bone-grafted area were observed in at least three consecutive CT scan cuts.
Pain, subjective disability of the disease, quality of the patient’s life as well as functional and economic status were analyzed before the surgery and at the end of this study. The intensity of pain was recorded using the visual analogical scale described by Huskisson in 1974 [15]; the subjective disability was assessed by the Oswestry index (ODI) [10].
The Prolo score modified by Dreysin and Esses was used for the functional and economic statutes [8] as well as to compare our results with those reported in other previous studies. All of these tools are scientifically validated for assessment of low back pain and questionnaires were filled during consultations. According to the age, results were separated in two groups: below and above 30 years.
Surgical technique
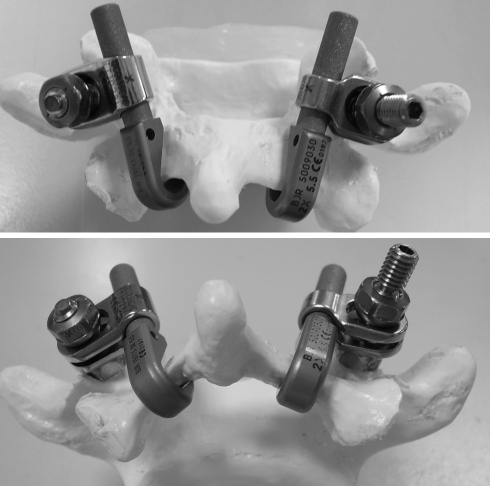
The implant type used in this series was a titanium pedicle screw hook system, which is made up of a standard or polyaxial pedicle screw (5.5 or 6.2 mm) and a rod–laminar hook complex (30° angle inclination for a more anatomic reconstruction and an easy introduction). This complex is connected to the screw through a hemispherical clamp, which allows self-positioning, thus avoiding complicated bending and positioning of the rod. The clamps move laterally on the spherical part of the screw and the hook and the screw are positioned according to the anatomy of the graft defect and the pedicle, respectively. This hook is available in two sizes; small and larger sizes, for an adequate fit (Fig. 1).
Fig. 1.
Pedicle screw hook system A and B (B.J.R.—Orhtogese Belgium)
The operative technique was the usual placement of pedicle screws in each pedicle of the spondylolytic vertebra by a midline incision. All pseudarthrosis tissue was removed and the defect was filled with cancellous allograft. The hook–rod complex was inserted and impacted, the clamp was positioned on the rod and it was introduced into the screw head. The construct was then loaded with by means of a secured hook compressor (to avoid subluxation of the posterior facet joint). The good positioning of the implants was checked by intraoperative radiography. Closure of the wound was performed as routine, and an aspirative drainage was left.
Two days after surgery, patients were allowed to stand up, no brace was worn after this procedure because the construct was enough resistant to keep the graft and the lamina in compression until the fusion was acquired.
Patients stayed for 4–5 days in the hospital, they were encouraged to walk; daily activities were authorized with caution and without excessive load. Physiotherapy, exercise, sport and the most of professional activities could be restarted 3 months later. Heavy activities (with heavy loads) were to be totally avoided during 6 months post-operatively (Fig. 2).
Fig. 2.
Postoperative anteroposterior and lateral radiographs
Ethical consideration
The informed consent of all participants was obtained and the permission to perform this study was obtained from the Ethics committee of the hospital.
Statistics
Statistical comparisons of preoperative and postoperative results were performed using paired Student’s t test. The chosen level of significance was 0.05.
Results
Between 1996 and 2005, 23 patients were operated for a symptomatic spondylolysis in our hospital (with the B.J.R. pedicle screw hook system). This group was made of 15 males (65%) and 8 females (35%), the average age was 34 years (range 16–52). At surgical time twelve patients were 30 years old or below, whereas the other 11 patients were older.
The pars defect was bilateral in all patients; the level was L4 in 3 cases (13%) and L5 in 20 cases (87%). The postoperative follow-up period was ranged from 6 to 113 months (mean 59 months). All patients displayed a low back pain resistant to conservative treatment (100%), the pain was localized only to the back in nine cases (39%) and was accompanied by radicular leg pain in others (61%). Nobody exhibited motor or sensitivity defect.
The mean period from the onset of symptoms was ranged from 6 months to 20 years (mean 57 months). A familial history of spondylolysis was found in four cases (18%). In this population 5 patients did not have a job at time of surgery (21.5%), 7 were office workers (30.5%) and 11 were manual laborers (48%).
Radiographic findings showed that 12 patients had a grade 1 spondylolisthesis (Meyerding’s classification) and 8 had disk signal dehydration at MRI (grade 2 or 3 of the Pfirrmann’s classification). In the latter group, all patients were older than 30.
Before the surgery, 21 patients (91.3%) presented severe pain (V.A.S. > 6), the mean score was 7.8/10 (SD 0.9). At the end of the study, 20 patients (87%) had no or minimal pain without disability in daily activities (V.A.S. < 3); the three other (13%) kept a moderate pain (V.A.S. between three and five). The mean postoperative V.A.S. score became 2/10 with a standard deviation of 1. These results were considered significant with a P value < 0.05 (Table 2).
Table 2.
Patients’ results
| Patients | V.A.S. preop | V.A.S. postop | Prolo postop | Work resumption | Type of work | Leisure activities |
|---|---|---|---|---|---|---|
| 1 | 8 | 1 | 10 | 5 months | Same | Yes |
| 2 | 7 | 2 | 7 | Jobless | – | – |
| 3 | 9 | 2 | 8 | 12 months | Same | No |
| 4 | 8 | 2 | 8 | Jobless | – | No |
| 5 | 7 | 1 | 9 | 6 months | Same | Yes |
| 6 | 8 | 1 | 8 | 5 months | Same | Yes |
| 7 | 8 | 2 | 9 | 6 months | Same | Yes |
| 8 | 7 | 4 | 6 | 12 months | Adapted | No |
| 9 | 8 | 1 | 10 | 9 months | Same | Yes |
| 10 | 7 | 4 | 6 | 12 months | Adapted | No |
| 11 | 9 | 2 | 8 | 12 months | Same | – |
| 12 | 7 | 2 | 8 | Jobless | – | Yes |
| 13 | 9 | 2 | 7 | 5 months | Adapted | – |
| 14 | 7 | 1 | 9 | 5 months | Same | Yes |
| 15 | 9 | 2 | 8 | 3 months | Same | Yes |
| 16 | 8 | 5 | 6 | Jobless | – | – |
| 17 | 8 | 1 | 10 | 3 months | Same | No |
| 18 | 6 | 2 | 9 | 6 months | Same | Yes |
| 19 | 8 | 1 | 9 | 12 months | Same | Yes |
| 20 | 9 | 2 | 9 | 12 months | Same | – |
| 21 | 8 | 2 | 8 | 9 months | Same | Yes |
| 22 | 8 | 2 | 8 | Jobless | – | – |
| 23 | 6 | 2 | 8 | 6 months | Same | Yes |
The postoperative functional and economic status (modified Prolo score), ability to resume work and leisure activities are also resumed in Table 2. Modified Prolo scores were excellent (9–10) for 9 patients (39%), good (7–8) for 11 patients (47.8%) and fair (5 or 6) for 3 patients (13%). Good and excellent results were then found in 87% of cases (20 patients) and the mean Prolo score was 8.2/10 (SD 1.2). Nobody showed poor outcome (Prolo score less than 5).
Among the 18 working people before the surgery, 15 were able to go back to the same work without restraint (83%), the three others (all manual laborers) started less physical strenuous activities (17%); nobody stopped working. The labor was resumed after 3–12 months. Before the surgery, 18 patients had leisure activities; 12 of them were able to restart without disability and discomfort.
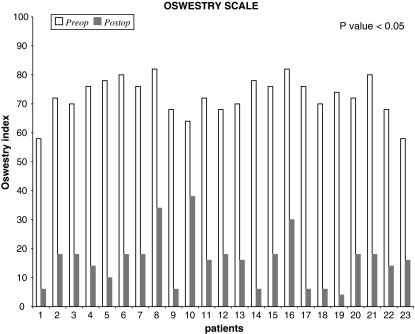
The scores of Oswestry disability index (ODI) are displayed in Fig. 3. They were studied and separated using a percentage of disability introduced by Fairbank et al. [10]. Before surgery 91% of patients were left in the severe disability group (percentage of disability > 60%), the mean index was 72.5 (SD 6.7).
Fig. 3.
Oswestry index (functional statute)
At the end of this study, the ODI scores were ranged between 4 and 38 with an average of 15.9 (SD 8.8); 87% of the patients were found in minimal disability group (ODI < 20%). These results are regarded as good to excellent by us. Others people (3 cases—13%) were placed in the moderate disability group, corresponding to fair results. These results were also considered significant with a P value < 0.05.
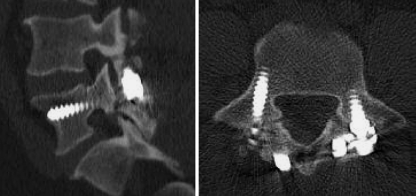
Bilateral consolidation of the defect was found among 21 patients (91%) with a follow-up of at least 6 months. No fusion was observed in the two others cases (9%), they were viewed as a failure of pseudarthrosis treatment (the consolidation was not acquired, respectively, at 12 and 91 months). Both were older than thirty and presented disc signal modification before surgery. In these patients, CT scan did not show evidence of healing, pars defect was broad and the bone graft did not fill it (avascular or atrophic pseudarthrosis) (Fig. 4).
Fig. 4.
Failure of consolidation postoperative sagittal (a) and axial (b) CT images
Patients were separated into groups: 30 years old or below and above 30 years (Table 3). Eighty-seven percent of the patients were very satisfied with our choice and would return to surgery if they had the same problem again.
Table 3.
Patients’ results according to the age
| 30 years old or below | Above 30 years | |
|---|---|---|
| V.A.S. preop. | 7.75 (SD 1) | 7.8 (SD 0.75) |
| V.A.S. postop. | 1.7 (SD 0.9) | 2.7 (SD 1.2) |
| Prolo score | 8.5 (SD 1) | 7.3 (SD 1.3) |
| ODI preop. | 71% (SD 7) | 74.2% (SD 6.2) |
| ODI postop. | 11.3% (SD 5.5) | 19.8% (SD 10.3) |
| Consolidation | 100% | 82% |
Discussion
Spondylolysis refers to a defect of the pars interarticularis of the vertebrae, it can be found at any level of the spine but the most common vertebrae involved are L4 and L5 [14].
The prevalence of 6% has been documented in radiographic screening of large numbers of adult spine in our population. More than 4% were identified before 7 years of age and few additional cases were found after 18 years [14].
Wiltse was the first to postulate that the lesion is a stress fracture mainly occurring after repeated minor trauma or occasionally after a single traumatic incident. A high prevalence in some populations (more than 50% in Inuit population) and a high familial predisposition (27–69%) probably imply genetic predisposition [44, 45].
This lesion is frequently asymptomatic and heals without treatment (spontaneous healing of the defect). Hypermobility of the loose posterior arch with stimulation of the defective tissue and relative instability of the vertebral body that induces excessive stress in the underlying disk can account for the symptoms. Likewise, fusion failure of this fracture (pseudarthrosis) can also cause complaints; neural elements (nociceptive nerve endings) are found in the pars defect tissue [37].
Conservative measures are successful in most patients (rest, bracing, physical therapy, temporary restriction of activity, analgesia, infiltration); the surgery must only be considered when these treatments fail (attempt of at least 6 months).
Fusion of the involved level has been widely accepted as the treatment of symptomatic spondylolysis with or without degenerative disc signals and spondylolisthesis [13, 27]. But, some investigators believe that lumbar fusion may lead to a significant acceleration of degenerative lesions at adjacent levels [3, 19, 20, 25, 43, 46].
It was determined that fusion altered the kinematics of the adjacent segments, redistributing the mobility toward relative hypermobility in the adjacent levels [2, 21]. These changes are certainly an important factor for persistent symptoms or new symptoms arising after a successful fusion [24]. For all these reasons pars repair deserves consideration.
The oldest technique was described by Kimura in 1968; no instrumentation was used during the procedure. Patients remained supine for at least 2 months followed by external immobilization by a cast for up to 6 months [17]. No subsequent reports of this method are available.
Two years later, Buck was the first to describe internal fixation with screws penetrating directly through the pars interarticularis [6]; all authors still agree that it is a demanding procedure due to the lamina narrowness, the proper placement of the screws is reported as difficult [9, 23]. This technique also decreases the available area for bone grafting which remains an essential part of the operation.
A complication rate from 5.6 to 40% related to the surgical technique or hardware failure has been reported [7]. Several surgeons still meet satisfactory results with the Buck’s technique (defect-healing rate obtained range from 82 to 100%) [5, 8, 18, 29, 31, 35, 42, 45] but it has a lengthy learning curve [4, 38].
In the seventies, Scott [28] described a wiring technique to stabilize the posterior arch. Placement of the wires under the transverse processes may be difficult and lead to significant bleeding or nerve root injury. The wires are not strong enough and thus patients are obliged to wear a postoperative brace for 3 months. Still several cases of wire breakage have been reported.
Different modifications of this technique were described to improve the biomechanical behavior of the system, to make easier the surgery and to reduce the level of complications. The consolidation rates observed with these wiring technique is ranged from 86 to 100% and a complication rate of 14% is reported in literature [8].
At the same time, an original technique of the lumbosacral junction temporary fixation was developed by Louis [22] (butterfly plate). The advantages are a large area available for the bone graft and the avoidance of possible shortening of the pars interarticularis, as could happen with techniques that apply compression over this area. Excellent results have been reported in a large series. However, implant removal as a secondary procedure is mandatory, and postoperative bracing is advised for 3 months. The author showed 86% of good results with this plate and a rate of fusion of 95% [22].
In 1984, Morscher was the first to introduce a special device to repair the par defect (laminar hook); this system allows fixation of the posterior arch and the bone graft under compression. Different authors showed that defect-healing rates ranged from 56 to 82% [1, 12, 28, 30, 36, 44] although complication rates up to 44% have been reported in the literature [8].
This technique is also demanding and the placement of the screws is difficult (technical mistake has been found in 15% of cases with the screw penetration into the inferior articular process of the above vertebra) [12].
Moreover a high device failure rate has been observed, implant loosening or screw breakage was frequently reported and a relative weakness of the instrumentation was described (resulting in a lack of defect consolidation) [36].
Segmental pedicle screw hook fixation (evolution of the Morscher’s concept) is nowadays performed to overcome drawbacks. This new device seems to offer several advantages; strength of the hardware (rod and screws) avoids the need for postoperative immobilization and decreases the probability of device failure; pedicle screws are placed in a classic manner and any surgeon experienced with pedicle screw systems should be able to learn the technique rapidly.
The first who introduced segmental pedicle screw hook fixation was Taddonio [40] using the CD system (Cotrel–Debousset). Later, different authors presented their own device variant, as Tokuhashi and Matsuzaki (Isola pediculolaminar implants) [41], Kakiuchi [16] (Texas Scottish Rite Hospital (TSRH) system,) and Roca [34] (Diapason system). Good and excellent result in 79–100% of cases has been reported by these authors. Since 1998 Gillet works with a rod screw construct to repair the spondylolysis (the rod was fixed again the spinous process), reporting 70% of good and excellent results [11].
The spondylolysis is pseudarthrosis of the isthmus with a failure of the fracture consolidation. So it requires rigid osteosynthesis with compression device and cancellous bone graft. The biomechanical comparison of fixation techniques carried out by Deguchi demonstrates that pedicle screw hook device is one of the most rigid systems, mainly regarding micromotion across the defect [7]. It brings a biomechanical advantage for the surgical treatment of pseudarthrosis.
The B.J.R system is very easy to use and allows anatomic pars interarticularis reconstruction of spondylolysis. The blade of the hook can grasp the lamina in a very close-fitting way and put the graft in compression. Using a hemispherical clamp for binding the rood hook and the screw allows an easy connection regardless of position of the hook.
A review of the literature reveals that the results of surgery in spondylolysis series seem to depend on the degree of disk degeneration, the existence of a previous slip, and the patient’s age. Almost all authors agree that no intervertebral disk or facet degenerative changes should be present [1, 6, 29]. Magnetic resonance imaging must show normal disk hydration; if not fusion must be performed. However, in 1988 Louis [22] expanded the indications and proposed this surgery for people if the discal height was at least two thirds its normal height and if there was no slip of more than 10 mm. Patient’s age was between 12 and 47.
Considering his good results, this could extend the number of patients in which pars interarticularis repair could be contemplated (especially when taking into account poor long-term satisfaction with fusions).
In this study, the surgery was proposed for patients with normal MRI disk signal and also for patients with moderate signs of degeneration. Twenty patients (87%) presented good results regarding the pain relief (V.A.S. score) and the clinical outcome (ODI and modified Prolo scores). These patients had no complaints at the end of the study. Others (13%—3 cases) kept a moderate low back pain or pain radiating to the thighs during daily activities, work or sport practice; they are considered as fair results for us.
No significant difference was found between patients with or without grade 1 spondylolisthesis. In the younger group (12 cases), no one showed disc signal modification; all results were good to excellent and the consolidation was observed in all cases.
However in the older eleven patients, eight patients (73%) had moderate disk signal modification before the surgery; good to excellent results were found in eight people (73%) and fusion of the defect was present in 82% of cases (nine people).
All of these results were statistically significant with a P value < 0.05. These values are close to the results of Louis study [22] (86% of good and excellent results) and to the majority of studies proposing this surgery for patients without degenerative disk disease [1, 4–6, 11, 12, 26, 28–32, 34–36, 38, 40, 41, 45].
For most authors, the presence of hydration disk signal modification is associated with poor results and implies fusion. In this study, all patients with fair results showed MRI signal modification before surgery. But, in these patients with disc signal modification before surgery (eight cases), five presented good results; they were satisfied with the surgical treatment and they recovered a good quality of life.
Moreover, the failure of defect healing was observed among two of the three patients with fair results; literally this failure was also associated with disappointing results. Several authors believe that clinical outcome seem to be dependent on fusion rate; no consolidation of graft could be a cause of poor results [5, 34, 45]. Our data are in agreement with this hypothesis, all patients with no defect consolidation manifest fair outcome.
Viewing these results, the authors believe, as Louis, that isthmic repair can be proposed for patients with normal disk hydration but also to patients with moderate signs of disk degeneration. Grade 3 of the Pfirrmann’s classification, corresponding to a mild narrowing of the intervertebral space with a diffuse loss of signal (moderate sign of disk degeneration), seems to be a good limit for this surgical technique. Grade 4 of this classification is a too advanced lesion and will be associated with worse results.
In this study, a failure of pseudarthrosis consolidation was found in two cases. This is very likely in relation with a lack of mechanical stability of the procedure (although no technical modification was carried out compared to others). But in these two patients, the preoperative CT scan showed a very broad defect and hypotrophic bone edge (broad atrophic pseudarthrosis). This translates a severe lack of local vascularization, which must have a predictive value on consolidation.
No complications were found in this study. Hardware removal was not performed; donor site pain was not encountered, possibly because of the small amount of bone necessary for this procedure. No hardware breakage or loosening was also observed.
Conclusion
Defect repair using the pedicle screw hook system is a technically simple and safe procedure. It provides immediate fixation and minimizes the risk of neurologic injury.
The B.J.R. device is easy to use and allows an anatomic reconstruction of the isthmus. No material failure has been discovered with a mean follow-up of 5 years. Patients showed good clinical outcome and significant pain reduction in 87%. Return to a comfortable daily life was achieved early, in few weeks; work or demanding sports resumption was also obtained in most cases. Results are excellent for young people without disc degeneration and satisfactory in patients with moderate degenerative disc disease.
In agreement with good results found in this study, authors believe that this technique may be extended to patients showing moderate disc dehydration. It would be interesting to carry out such studies on a wider sample of this type of patients with a significant follow up.
References
- 1.Albassir A, Samson I, Hendrickx L. Treatment of painful spondylolysis using Morscher’s hook. Acta Orthop Belg. 1990;56:489–495. [PubMed] [Google Scholar]
- 2.Aota Y, Kumano K, Hirabashi S. Postfusion instability at the adjacent segments alter rigid pedicle screw fixation for degenerative lumbar spinal disorders. J Spinal Disord. 1995;8:464–473. doi: 10.1097/00002517-199512000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Axelsson P, Johnson R, Ströngrist B. The spondylolytic vertebra and its adjacent segment. Mobility measured before and after posterolateral fusion. Spine. 1997;22:414–417. doi: 10.1097/00007632-199702150-00012. [DOI] [PubMed] [Google Scholar]
- 4.Beckers L. Buck’s operation for treatment of spondylolysis and spondylolisthesis. Acta Orthop Belg. 1986;52:819–823. [PubMed] [Google Scholar]
- 5.Bonnici AV, Koka SR, Richards DJ. Results of Buck screw fusion in grade I spondylolisthesis. J R Soc Med. 1991;84:270–273. doi: 10.1177/014107689108400509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Buck J. Direct repair of the defect in spondylolisthesis. Preliminary report. J Bone Joint Surg [Br] 1970;52:432–437. [PubMed] [Google Scholar]
- 7.Deguchi M, Rapoff AJ, et al. Biomechanical comparison of spondylolysis fixation techniques. Spine. 1998;24:328–333. doi: 10.1097/00007632-199902150-00004. [DOI] [PubMed] [Google Scholar]
- 8.Dreyzin V, Esses SI. A comparative analysis of spondylolysis repair. Spine. 1994;19:1909–1915. doi: 10.1097/00007632-199409000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Ebraheim NA, Lu J, Hao Y, et al. Anatomic considerations of the lumbar isthmus. Spine. 1997;22:941–945. doi: 10.1097/00007632-199705010-00002. [DOI] [PubMed] [Google Scholar]
- 10.Fairbank J, Davies J, Couper J, OBrien J. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66(8):271–273. [PubMed] [Google Scholar]
- 11.Gillet P, Petit M. Direct repair of spondylolysis without spondylolisthesis, using a rod-screw construct and bone grafting of the pars defect. Spine. 1999;24:1252–1256. doi: 10.1097/00007632-199906150-00014. [DOI] [PubMed] [Google Scholar]
- 12.Hefti F, Seeling W, Morscher E. Repair of lumbar spondylolysis with a hook-screw. Int Orthop. 1992;16:81–85. doi: 10.1007/BF00182992. [DOI] [PubMed] [Google Scholar]
- 13.Hensinger RN. Spondylolysis and spondylolisthesis in children and adolescents: current concepts review. J Bone Joint Surg. 1989;71:1084–1107. [PubMed] [Google Scholar]
- 14.Herkowitz HN, Dvorak J, Bell G, et al. The lumbar spine. Non degenerative spondylolisthesis. Philadelphia: Lippincott Williams and Wilkins; 2004. pp. 556–563. [Google Scholar]
- 15.Huskisson EC. Measurement of pain. Lancet. 1974;ii:884–886. doi: 10.1016/s0140-6736(74)90884-8. [DOI] [PubMed] [Google Scholar]
- 16.Kakiuchi M. Repair of the defect in spondylolysis. J Bone Joint Surg. 1997;79:818–825. doi: 10.2106/00004623-199706000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Kimura M. My method of filling the lesion with spongy bone in spondylolysis and spondylolisthesis. Orthop Surg (Jpn) 1968;19:285–295. [PubMed] [Google Scholar]
- 18.Kip PH, Esses SI, Doherty B, Alexander J, Crawford M. Biomechanical testing of pars defect repairs. Spine. 1994;23:2692–2697. [PubMed] [Google Scholar]
- 19.Lee CK. Accelerated degeneration of the segment adjacent to a lumbar fusion. Spine. 1988;13:375–377. doi: 10.1097/00007632-198803000-00029. [DOI] [PubMed] [Google Scholar]
- 20.Lehman Tr, Sprat KF, Tozzi JE, et al. Long-term follow-up of lumbar fusion patients. Spine. 1987;12:97–104. doi: 10.1097/00007632-198703000-00004. [DOI] [PubMed] [Google Scholar]
- 21.Leong JCY, Grange WJ, Fang D. Long term results of lumbar intervertebral disc prolapse. Spine. 1983;8:793–799. doi: 10.1097/00007632-198310000-00018. [DOI] [PubMed] [Google Scholar]
- 22.Louis R. Pars interarticularis reconstruction of spondylolysis using plates and screws with grafting without arthrodesis. Rev Chir Orthop Reparatrice Appar Mot. 1988;74(6):549–557. [PubMed] [Google Scholar]
- 23.Lu J, Ebraheim NA, Biyani A. Screw placement in the lumbar vertebral isthmus. Clin Orthop. 1997;338:227–230. doi: 10.1097/00003086-199705000-00030. [DOI] [PubMed] [Google Scholar]
- 24.Mihara H, Onari K, Cheng BC, et al. The biomechanical effects of spondylolysis and its treatment. Spine. 2003;28:235–238. doi: 10.1097/00007632-200302010-00006. [DOI] [PubMed] [Google Scholar]
- 25.Miyakoshi N, Abe E, Shimada Y, et al. Outcome of one-level posterior lumbar interbody fusion for spondylolisthesis and postoperative intervertebral disc degeneration adjacent to the fusion. Spine. 2000;25:1837–1842. doi: 10.1097/00007632-200007150-00016. [DOI] [PubMed] [Google Scholar]
- 26.Morscher E, Gerber B, Fasel J. Surgical treatment of spondylolisthesis by bone grafting and direct stabilization of spondylolysis by means of a hook screw. Acta Orthop Trauma Surg. 1984;103:175–178. doi: 10.1007/BF00435550. [DOI] [PubMed] [Google Scholar]
- 27.Nachemson A. Repair of the spondylolisthesic defect and intertransverse fusion for young patients. Clin Orthop. 1976;117:101–105. [PubMed] [Google Scholar]
- 28.Nicol R, Scott J. Lytic spondylolysis, repair by wiring. Spine. 1986;11:1027–1030. doi: 10.1097/00007632-198612000-00011. [DOI] [PubMed] [Google Scholar]
- 29.Ohmori K, Suzuki K, Ishida Y. Translamino-pedicular screw fixation with bone grafting for symptomatic isthmic lumbar spondylolysis. Neurosurgery. 1992;30:379–384. doi: 10.1097/00006123-199203000-00011. [DOI] [PubMed] [Google Scholar]
- 30.Pavlovcic V. Surgical treatment of spondylolysis and spondylolisthesis with a hook screw. Int Orthop. 1994;18:6–9. doi: 10.1007/BF00180169. [DOI] [PubMed] [Google Scholar]
- 31.Pedersen A, Hagen R. Spondylolysis and spondylolisthesis: treatment by internal fixation and bone grafting of the defect. J Bone Joint Surg [Am] 1988;70:15–24. [PubMed] [Google Scholar]
- 32.Pellise F, Toribio J, Rivas A, et al. Clinical and CT scan evaluation after direct repair in spondylolysis using segmental pedicle screw hook fixation. J Spinal Disord. 1999;12:363–367. doi: 10.1097/00002517-199912050-00002. [DOI] [PubMed] [Google Scholar]
- 33.Pfirrmann CWA, Metzdorf A, Zanetti M, et al. Magnetic resonance classification of the lumbar intervertebral disc degeneration. Spine. 2001;26:1873–1878. doi: 10.1097/00007632-200109010-00011. [DOI] [PubMed] [Google Scholar]
- 34.Roca, Jaime MD, et al. Direct repair of spondylolysis using a new pedicle screw hook fixation: clinical and CT-assessed study: an analysis of 19 patients. J Spinal Disord Tech. 2005;18(suppl):S82–S89. doi: 10.1097/01.bsd.0000123425.12852.3c. [DOI] [PubMed] [Google Scholar]
- 35.Roca J, Moretta D, Fuster S, Roca A. Direct repair of spondylolysis. Clin Orthop. 1989;246:86–91. [PubMed] [Google Scholar]
- 36.Sales de Gauzi J, Vadier F, Cahuzac JP. Repair of lumbar spondylolysis using Morscher material. Acta Orthop Scand. 2000;71:292–296. doi: 10.1080/000164700317411906. [DOI] [PubMed] [Google Scholar]
- 37.Schneiderman G, Flannigan B, Kingston S, et al. Magnetic resonance imaging in the diagnosis of disc degeneration: correlation with discography. Spine. 1987;12(3):276–281. doi: 10.1097/00007632-198704000-00016. [DOI] [PubMed] [Google Scholar]
- 38.Scott JHS. The Edinburgh repair of isthmic (Group II) spondylolysis. J Bone Joint Surg. 1987;69:491. [Google Scholar]
- 39.Suh PB, Esses SI, Kostuik JP. Repair of pars interarticularis defect. The prognostic value of infiltration. Spine. 1991;16(suppl):445–448. doi: 10.1097/00007632-199108001-00027. [DOI] [PubMed] [Google Scholar]
- 40.Taddonio RF. Isthmic spondylolisthesis. In: Bridwell KH, DeWald RF, editors. The textbook of spinal surgery. Philadelphia: Lippincott; 1991. pp. 565–584. [Google Scholar]
- 41.Tokuhashi Y, Matsuzaki H. Repair of defects in spondylolysis by segmental pedicle screw hook fixation. Spine. 1996;21:2041–2045. doi: 10.1097/00007632-199609010-00023. [DOI] [PubMed] [Google Scholar]
- 42.Werf G, Tonino A, Zeegers W. Direct repair of lumbar spondylolysis. Acta Orthop Scand. 1985;56:378–379. doi: 10.3109/17453678508994351. [DOI] [PubMed] [Google Scholar]
- 43.Weinhoffer L, Guyer RD, Herbert M, et al. Intradiscal pressure measurements above an instrumented fusion. A cadaveric study. Spine. 1995;20:526–531. doi: 10.1097/00007632-199503010-00004. [DOI] [PubMed] [Google Scholar]
- 44.Wiltse LL, Widell EH, Jr, Jackson DW. Fatigue fracture the basic lesion is isthmic spondylolisthesis. J Bone Joint Surg Am. 1975;57(1):17–22. [PubMed] [Google Scholar]
- 45.Winter M, Jani L. Results of screw osteosynthesis in spondylolysis and low-grade spondylolisthesis. Arch Orthop Trauma Surg. 1989;108:96–99. doi: 10.1007/BF00932163. [DOI] [PubMed] [Google Scholar]
- 46.Yang SW, Langrana NA, Lee CK. Biomechanics of lombosacral spinal fusion in combined compression-torsion loads. Spine. 1980;11:937–941. doi: 10.1097/00007632-198611000-00014. [DOI] [PubMed] [Google Scholar]