Abstract
Although osteogenesis imperfecta is a well-known skeletal disorder, reports of spondylolisthesis in osteogenesis imperfecta are rare. Only very few cases of spondylolisthesis caused by elongation of lumbar pedicles have been described in the literature. Here we report three patients suffering from osteogenesis imperfecta showing a severe form of hyperlordosis caused by lumbar pedicle elongation and consecutive spondylolisthesis. Radiographs in the course of childhood and adolescence show a rapid progression of pedicle elongation and hyperlordosis with increased mechanical loads. The treatment strategy consists of physiotherapy, medical treatment with bisphosphonates, and orthopedic surgery and is preferably conservative. In the three patients reported here, one patient was treated with laminectomy and postero-lateral fusion, whereas in the other two patients surgery is currently not considered as necessary.
Keywords: Osteogenesis imperfecta, Spondylolisthesis, Pedicle elongation, Hyperlordosis
Introduction
Osteogenesis imperfecta is a hereditary skeletal disorder affecting approximately 1 in 20,000 births [10]. Mean characteristics of the disease are low bone mass, increased bone fragility and progressive skeletal deformities. The majority of osteogenesis imperfecta cases result from mutations of the COL1A1 and COL1A2 genes encoding the α1 and α2 chains of type I collagen, the major structural protein of the bone. As type I collagen is also an integral component of several extraskeletal tissues there are some extraskeletal manifestations such as dentinogenesis imperfecta, blue sclerae, hearing impairment and hyperlaxity of the skin and ligaments which are associated variably with osteogenesis imperfecta.
According to genetic and clinical heterogeneity several classification systems were introduced. The most widely used is the Sillence classification [9] distinguishing four clinical types (type I–IV) of osteogenesis imperfecta typically associated with COL1A1 or COL1A2 mutations. Recently, three additional types (type V–VII) displaying distinct features of the disease and caused by yet unknown mutations were introduced [2, 3, 11]. For these osteogenesis imperfecta types there is no evidence for collagen type I abnormality.
Characteristic spinal manifestations of the disorder are vertebral body deformities, scoliosis, pathological kyphosis, and basilar impression. So far only few cases of spondylolisthesis in patients suffering from osteogenesis imperfecta have been described in the literature.
Rask et al. [7] described a 40-year-old patient suffering from osteogenesis imperfecta with grade II spondylolisthesis of the lumbosacral joint due to a defect of the pars interarticularis of L5. Hanscom et al. [4] reported two patients with grade I and grade III spondylolisthesis, respectively, and one patient with elongation of the pars interarticularis. All individuals were classified as type A of the disease according to the classification system proposed by Hanscom. Newman and Stone [6] showed radiographs of a 6-year-old girl suffering from osteogenesis imperfecta with spondylolisthesis due to elongation of the lumbar pedicles, markedly of L4 and L5. Review of 60 individuals with osteogenesis imperfecta by King and Bobechko [5] revealed four patients with spondylolisthesis due to elongated pedicles without any break of the pars interarticularis. Recently, Basu et al. [1] reported two adolescent girls suffering from osteogenesis imperfecta type III and IV showing spondylolisthesis due to severe pedicle elongation of the lumbar vertebrae. One of them was treated with anterior interbody fusion.
Here we report three patients suffering from osteogenesis imperfecta showing a severe form of hyperlordosis caused by lumbar pedicle elongation and consecutive spondylolisthesis without spondylolysis.
Case reports
Case 1
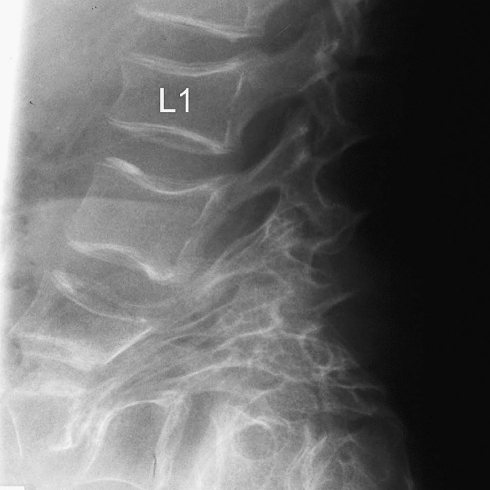
Case 1 is a 29-year-old girl of Turkish origin suffering from osteogenesis imperfecta of a not clinically to be specified type, as the results of a biochemical analysis of α1 and α2 chains of type I collagen were regular. She was born by normal vaginal delivery. At the age of 3 years, lumbar hyperlordosis (92° from L3 to S1) and spondylolisthesis due to initial elongation of the lumbar pedicles particularly of L3, L4, and L5 was detected for the first time (Fig. 1a). During childhood with increased mechanical loads elongation of lumbar pedicles and consecutive spondylolisthesis showed a rapid progression (Fig. 1b). In addition, in early adolescence the girl developed a moderate thoraco-lumbal scoliosis. At 17 years of age, the patient complained about considerable low back pain with a limited walking distance of some hundred meters. Radiographs show a progression of lumbar hyperlordosis to an angular deformation of the lumbar spine (126° from L3 to S1) and extreme elongation of the lumbar pedicles, markedly of L2–L5, with consecutive spondylolisthesis (Fig. 1c). Therefore, a lumbar laminectomy and postero-lateral fusion with Cotrel–Dubousset instrumentation were performed (Fig. 1d, e). Due to lank, elongated pedicles, placement of screws is partially extrapedicular. After surgery, lumbar pain was slightly improved. As subsequent radiographs confirmed fusion and the patient complained about local pressure sores, instrumentation was gradually removed until 23 years of age. A recent MRI scan of the lumbar spine at the age of 28 years (Fig. 1f) demonstrates that the lumbar deformation shows no significant progress since the postero-lateral fusion. Temporarily ambulation (with a cane) for substantial distances (more than 1,000 m) and riding a bicycle for up to 40 km was possible. However, as the patient also suffers from pelvic deformation with acetabular protrusion and several pelvic fractures (Fig. 1g), ambulation is currently restricted.
Fig. 1.
a Radiograph of the lumbar spine of patient 1 at the age of 3 years and 5 month shows a lumbar hyperlordosis of 92° (from L3 to S1) and spondylolisthesis due to elongation of lumbar pedicles, markedly of L3, L4, and L5. b At 7 years and 11 month of age, lumbar pedicle elongation and consecutive spondylolisthesis show a rapid progression. c Radiograph of patient 1 at 17 years of age shows angular hyperlordosis of 126° (from L3 to S1) and spondylolisthesis as a result of extreme elongation of lumbar pedicles. d, e Radiographs of patient 1 after laminectomy and postero-lateral fusion using Cotrel–Dubousset instrumentation. f A recent MRI scan of the lumbar spine of patient 1 at the age of 28 years shows no significant progression of the lumbar deformation. g A current antero-posterior radiograph of the pelvis of patient 1 shows the pelvic deformity with acetabular protrusion and fracture of the right acetabulum
Case 2
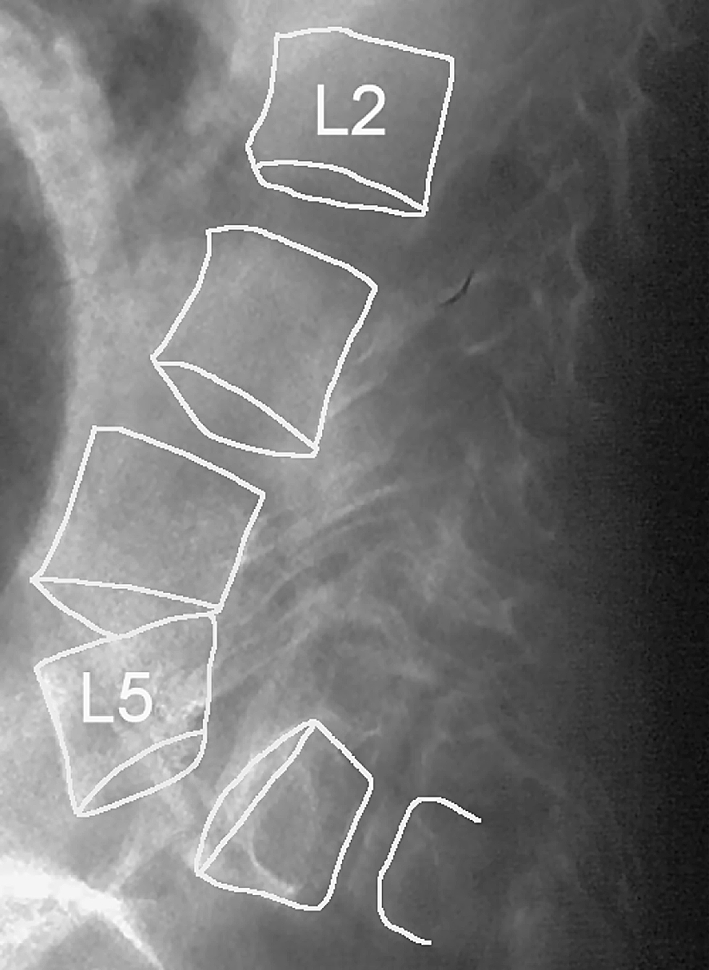
Case 2 is the 26-year-old sister of patient 1 also suffering from typical osteogenesis imperfecta-symptoms. She was born by normal vaginal delivery. At the age of 9 months wormian bones on skull radiographs, multiple fractures of the ribs and a scoliotic spinal deformity were observed. During infancy she suffered several fractures of both thigh bones. At the age of 7 years a lumbar hyperlordosis due to pedicle elongation of lumbar vertebrae was detected. As thoracal scoliosis showed a rapid progression to a Cobb scoliosis angle of 80° at 11 years of age, the girl underwent a posterior spinal fusion using Cotrel–Dubousset instrumentation from C6 to Th12. Radiographs of the lumbar spine at this age show an angular hyperlordosis (106° from L3 to S1) caused by extreme elongation of the lumbar pedicles (markedly of L2–L5) and consecutive spondylolisthesis (Fig. 2). As the patient did not complain about considerable lumbar pain nor showed any neurological symptoms, no surgical treatment of the lumbar spine was necessary. The patient is restricted to a wheelchair and is mobile with a special adapted car. She is working as a leading administrator. Patient 1 and patient 2 have a 16-year-old sister also suffering from typical clinical manifestations of osteogenesis imperfecta like multiple fractures, scoliosis, and pelvic deformation; however, this patient does not suffer from considerable lumbar spondylolisthesis.
Fig. 2.
Radiograph of patient 2 at the age of 11 years shows an angular hyperlordosis of 106° (from L3 to S1) caused by extreme elongation of lumbar pedicles (particularly of L2–L5) and consecutive spondylolisthesis
Case 3
Case 3 is a 12-year-old boy from Libya diagnosed as osteogenesis imperfecta type IV according to Sillence et al. [9]. During childhood he suffered several fractures of the lower extremities leading to distinct deformities of both legs. Current radiographs of the lumbar spine show a hyperlordosis of 72° (from L3 to S1) caused by elongation of the lumbar pedicles (particularly of L3, L4, and L5) and consecutive spondylolisthesis (Fig. 3). As the young patient does not complain about lumbar pain nor shows any neurological symptoms, the current treatment strategy is conservative (medical treatment with bisphosphonates, physiotherapy).
Fig. 3.
Radiograph of patient 3 at 11 years of age shows lumbar hyperlordosis of 72° (from L3 to S1) and spondylolisthesis caused by elongation of lumbar pedicles, markedly of L3, L4, and L5
Discussion
Although osteogenesis imperfecta is a well-known skeletal disease, there have been only a few reports of spondylolisthesis in this disease. Rask [7] and Hanscom et al. [4] reported altogether three patients with spondylolisthesis due to a defect of the pars interarticularis, whereas Newman and Stone [6], King and Bobechko [5] and Basu et al. [1] reported a total of seven patients suffering from osteogenesis imperfecta with spondylolisthesis due to pedicle elongation of the lumbar vertebrae. We report three patients with osteogenesis imperfecta showing angular hyperlordosis caused by elongation of the lumbar pedicles and consecutive spondylolisthesis. According to the classification of spondylolysis and spondylolisthesis as proposed by Wiltse et al. [12], all patients reported here are suffering from type V spondylolisthesis (pathological spondylolisthesis due to general bone disease). During childhood with increased mechanical loads, pedicle elongation and hyperlordosis show a rapid progression (Fig. 1a–c). No pedicle fractures were observed. This fits the hypothesis that osteopenia causes increased microdamage in osteogenesis imperfecta bones, resulting in increased bone remodeling and, with raised mechanical strains, progressive deformations.
Treatment strategies in osteogenesis imperfecta depend on clinical and radiological findings and consist of physiotherapy and rehabilitation, medical treatment with bisphosphonates (for dosage: see Rauch and Glorieux [8]), and orthopedic surgery. Treatment of patients suffering from spondylolisthesis caused by elongated lumbar pedicles in osteogenesis imperfecta is preferably conservative. Surgery may be necessary in case of rapid progression of spine deformations, considerable lumbar pain and neurological symptoms. The biomechanics in osteogenesis imperfecta is difficult to anticipate. Lumbar decompression without stabilization is prone to instability of the treated spinal segment, whereas posterior instrumentation is technically difficult to perform due to lank, elongated pedicles and holds the risk of instability of the adjacent spinal segments. Recently, Basu et al. [1] reported successful treatment of a patient suffering from spondylolisthesis in osteogenesis imperfecta due to lumbar pedicle elongation with anterior interbody fusion without instrumentation. In the three patients reported here, one patient was treated successfully with lumbar laminectomy and postero-lateral fusion, whereas in the two other patients surgery is currently not considered as necessary.
References
- 1.Basu PS, Noordeen MHH, Elsebaie H. Spondylolisthesis in osteogenesis imperfecta due to pedicle elongation. Spine. 2001;26(21):E506–E509. doi: 10.1097/00007632-200111010-00022. [DOI] [PubMed] [Google Scholar]
- 2.Glorieux FH, Rauch F, Plotkin H, Ward L, Travers R, Roughley P, Lalic L, Glorieux DF, Fassier F, Bishop NJ. Type V osteogenesis imperfecta: a new form of brittle bone disease. J Bone Miner Res. 2000;15:1650–1658. doi: 10.1359/jbmr.2000.15.9.1650. [DOI] [PubMed] [Google Scholar]
- 3.Glorieux FH, Ward LM, Rauch F, Lalic L, Roughley PJ, Travers R. Osteogenesis imperfecta type VI: a form of brittle boone disease with mineralization defect. J Bone Miner Res. 2002;17:30–38. doi: 10.1359/jbmr.2002.17.1.30. [DOI] [PubMed] [Google Scholar]
- 4.Hanscom DA, Winter RB, Lutter L, Lonstein JE, Bloom BA, Bradford DS. Osteogenesis imperfecta. Radiographic classification, natural history, and treatment of spinal deformities. J Bone Joint Surg. 1992;74A(4):598–616. [PubMed] [Google Scholar]
- 5.King JD, Bobechko WP. Osteogenesis imperfecta. An orthopaedic description and surgical review. J Bone Joint Surg. 1971;53B(1):72–89. [Google Scholar]
- 6.Newman PH, Stone KH. The etiology of spondylolisthesis. J Bone Joint Surg (Br) 1963;45:39–59. [Google Scholar]
- 7.Rask MR. Spondylolisthesis resulting from osteogenesis imperfecta. Report of a case. Clin Orthop. 1979;139:164–166. [PubMed] [Google Scholar]
- 8.Rauch F, Glorieux FH. Osteogenesis imperfecta. Lancet. 2004;363:1377–1385. doi: 10.1016/S0140-6736(04)16051-0. [DOI] [PubMed] [Google Scholar]
- 9.Sillence DO, Senn A, Danks DM. Genetic heterogeneity in osteogenesis imperfecta. J Med Genet. 1979;16:101–116. doi: 10.1136/jmg.16.2.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smith R. Osteogenesis imperfecta: the brittle bone syndrome. Curr Orthop. 1995;9:28–33. doi: 10.1016/0268-0890(95)90046-2. [DOI] [Google Scholar]
- 11.Ward LM, Rauch F, Travers R, Chabot G, Azouz EM, Lalic L, Roughley PJ, Glorieux FH. Osteogenesis imperfecta type VII: an autosomal recessive form of brittle bone disease. Bone. 2002;31:12–18. doi: 10.1016/S8756-3282(02)00790-1. [DOI] [PubMed] [Google Scholar]
- 12.Wiltse LL, Newman PH, Macnab I. Classification of spondylolisis and spondylolisthesis. Clin Orthop. 1976;117:23–29. [PubMed] [Google Scholar]