Abstract
The study design was a retrospective study in adolescent scar contracture scoliosis caused by back scalding during the infantile period. The objective of the study was to investigate the pathogenesis, clinical manifestation and treatment of adolescent scar contracture scoliosis caused by back scalding during the infantile period. This condition seldom occurs and is not reported in current English literature. One patient was first treated with skin expansion, back scar excision and skin flap transfer, followed by anterior correction with TSRH instrumentation. Two patients were first treated with back scar excision and anterior spinal release. One patient was treated with posterior correction with TSRH instrumentation, and thoracoplasty was performed after 50 days in halo-wheelchair traction. The other patient was treated with posterior correction with TSRH instrumentation. No management of scalding was performed on the fourth patient. Anterior release and posterior correction were performed at an interval of 3 weeks. The deformities of four patients were well corrected. Trunk balance was restored and the pelvis leveled. The skin incision wounds healed well. Minor loss of correction was recorded during the last follow-up. Severe scar contracture caused by back scalding during the infantile period could lead to adolescent scoliosis. Its pathogenesis and clinical manifestation are different from the typical adolescent idiopathic scoliosis. The treatment of this kind of scoliosis should be individualized.
Keywords: Scoliosis, Scar contracture, Scalding, Treatment
Adolescent idiopathic scoliosis (AIS) is the most common type of spinal deformity arising during pubertal growth. The etiology and pathogenesis of AIS are still largely unknown [6]. However, there are many types of scoliosis caused by known etiological factors. Duchenne muscular dystrophy, thoracotomy, multicore myopathy with paraspinal contractures, contractures and growth disturbances in the hip and pelvis, radiation to the juxtaspinal and fractures to the bony spinal column along with continued exposure to physiological stresses were reported to be the causes of scoliosis [1, 4, 7–10]. The prevalence of these types of scoliosis is much lower than that of AIS, and their physiological characters and treatment principles are different from that of AIS.
Adolescent scar contracture scoliosis caused by scalding during the infantile period seldom occurs. We carried out a wide search for literature on this kind of scoliosis, but none was found. From August 1997 to May 2005, about 1,300 patients were operated on by the authors, which include 756 cases of adolescent idiopathic scoliosis, 381 cases of congenital scoliosis, 131 cases of neuromuscular scoliosis, 47 cases of type 1 neurofibromatosis with scoliosis and 58 cases of the other kind of scoliosis. Only four of them were diagnosed with adolescent scar contracture scoliosis. The aim of this study was to investigate its pathogenesis, clinical manifestation and surgical management.
Cases
Case 1
A 15-year-old boy suffered from 25% full thickness scalding by hot water at the age of 1 month. The scalding was treated at that time. Scoliosis was found when he was 5 years old and developed rapidly after the age of 12; but no management was proposed before his consultation at our center. On examination, a contractured scar was present on the left side of the back. There was little muscle tissue felt under the contractured scar. The trunk deviated to the right on standing view. Curvature of the thoracolumbar spine was right-sided (convex to the side without the contractured scar). The pelvis was oblique with the left side higher than the right side. The length of his legs was equal. Flexibility on right-sided bending was very limited. The curve ranged from T10 to L3 with a Cobb angle of 54°. The side-bending films showed a flexibility of 30%. The apex vertebra rotation was ++ (Nash-Moe method) and the Risser sign was ++++. The left iliac crest was 3 cm higher than the right (Fig. 1b).
Fig. 1.
A 15-year-old boy with scar contracture thoracolumbar scoliosis with a Cobb angle of 54° (a, b, c). Skin expansion, back scar excision and flap transfer were performed before spine surgery (d, e, f). Four months later, he had anterior TSRH instrumentation for his thoracolumbar scoliosis with a correction rate of 72% (g)
Skin expansion (Fig. 1d–f), back scar excision and flap transfer were performed. Anterior correction of his thoracolumbar scoliosis with TSRH (Medtronic, USA) instrumentation was performed 4 months after his back plastic surgery, followed by a 3-month post-operative cast immobilization. The curvature was corrected to 15° immediately after operation with a correction rate of 72% (Fig. 1g).
Case 2
The patient was a 15-year-old girl who suffered from 35% full thickness scalding by hot water when she was 4 years old. The contractured scar was on the left side of the back, abdomen, hip and two thighs. Scoliosis appeared at the age of 7 years and became severe in the last 3 years; she never received any bracing or casting to treat her scoliosis. The trunk deviated to the left as the patient stood; the curvature of the thoracic spine was convex on the left side. The length of her legs was equal and the pelvis was oblique, with the right side higher than the other side in a standing position. The correction of the curve on the left side bending was limited (Fig. 2a). The curve started from T6 to L1 with a Cobb angle of 103°. The right iliac crest was 3 cm higher than the left. The Risser sign was ++++ (Fig. 2b).
Fig. 2.
A 15-year-old girl with severe scar and scar contracture scoliosis (a). The pre-operative Cobb angle was 103° (b, c) and the spinal deformity was corrected dramatically, the trunk well balanced and the pelvis leveled. The post-operative X-ray films showed that the residual Cobb angle was 46° with a correction rate of 55% (d). The X-ray films at 3 months and 3 years follow-up showed no implant migration and no obvious loss of correction was found. (e, f)
Back scar excision with skin grafting (mainly on the concave side) was done and 2 months later, anterior release of the spine was performed. After 50 days in a halo-wheelchair traction, posterior instrumentation was done from T5 to L4 with TSRH system and thoracoplasty was performed simultaneously. Three-months’ cast immobilization was prescribed after the surgery. The Cobb angle reduced to 46° immediately after the surgery with a correction rate of 55%(Fig. 2d). At the 3-year-follow-up, the total loss of correction was 6% (Fig. 2e).
Case 3
The patient was a 23-year-old girl who had 35% full thickness scalding by hot water at the age of 3 years old; her scald was never treated. Scoliosis presented when she was 8 years old and progressed rapidly after the age of 13 years.
A contractured scar was present on the chest, the whole back, abdomen, two thighs, two gluteus and part of the upper extremities. There were little muscular tissues under the contractured scar of the back. The trunk deviated to the right side in the standing position. Curvature of the thoracic spine was on the right side (the convex side of the curve was the side with less scar tissues). The pelvis was oblique to the right side. There was no length discrepancy of her legs. Right-sided bending of the spine was severely limited (Fig. 3a). Scoliosis involved T6 to T12 with a Cobb angle of 85°. The side-bending films showed a flexibility of 18%. The apical vertebrae rotation was +++ (Nash–Moe method) and the Risser sign was ++++. The left iliac crest was 2 cm higher than the right (Fig. 3b).
Fig. 3.
A 23-year-old girl with scars located on the chest, the whole back, abdomen, two thighs, two gluteus and part of the upper extremities (a). The Cobb angle of curvature was 85° (b, c). The spinal deformity was corrected and the post-operative Cobb angle was 39° with a correction rate of 54% (d). The X-ray films at 1 year 9 months follow-up showed that the implant position was very good and no obvious loss of correction was seen (e)
There was no management of scalding before the correction of scoliosis. Thoracoscopic anterior release was performed. After 20 days in a halo-femoral traction, posterior correction with TSRH instrumentation was done. A 3-month cast immobilization was proposed after the surgery. After the correction of scoliosis, the Cobb angle was 39° with a correction rate of 54% (Fig. 3d). At the first 12 months follow-up, the loss of correction was 6%.
Case 4
The patient was an 11-year-old girl who suffered from 10% full thickness scalding because of hot water burning at the age of 5 years. There was no treatment for the scalding. Scoliosis presented at the age of 9 years and progressed rapidly after 10 years
About 10% contractured scars were found on the left armpit and left hypochondrium. The trunk deviated to the right side in the standing position. Curvature of the thoracic spine was on the right side (The convex side of the curve was the side with less scar tissues). The pelvis was oblique on the right side. There was no length discrepancy of her legs. Right-sided bending of the spine was severely limited (Fig. 4a). In the AP films, the curve was found to be convex to the right side involving the vertebrae from T7 to L5, with a Cobb angle of 80° (Fig. 4b). There was flexibility of 12.5% on the side-bending films. The apical vertebrae rotation was +++ (Nash–Moe method) and the Risser sign was 0. The left iliac crest was 3 cm higher than the right.
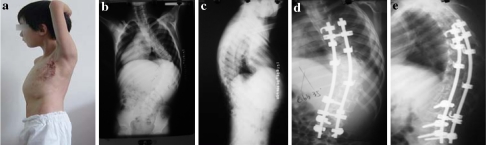
Fig. 4.
The clinical photo of an 11-year-old girl with scar located on the left armpit and left hypochondrium (a). The curve ranged from T5 to L5 with a Cobb angle of 80° (b, c). The spinal deformity was corrected after the operation. The trunk was balanced. The post-operative Cobb angle was 35° with a correction rate of 56% (d, e)
Scar excision, free skin grafting and anterior release were performed. Posterior correction with TSRH instrumentation was done 2 weeks later (Fig. 4d, e). With a post-operative Cobb angle of 35°, the correction rate was 56%. The details of all the four patients are summarized in Table 1 and Table 2.
Table 1.
Patients’ clinical data
| Patient | Age | Sex | Scalding | Age on development of scoliosis (years) | Age at plastic surgery (years) | Plastic surgery | Scoliosis surgery | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Age | Percentage (%) | Site | Degree | |||||||
| 1 | 15 | M | 1 m | 25 | Left back | III | 5 | 14 | Skin expansion, scar excision and flap transfer | Anterior TSRH correction |
| 2 | 15 | F | 4 y | 35 | Right back, abdomen, hip | III | 7 | 15 | Scar excision | Anterior release and posterior correction |
| 3 | 23 | F | 3 y | 35 | Abdomen, back, two thighs, two gluteus and part of two arms | III | 8 | 23 | None | Anterior release and posterior correction |
| 4 | 11 | F | 5 y | 10 | Left armpit and left hypochondrium | III | 9 | 11 | Removal of scar, free skin grafting | Anterior thoracoscopic release and posterior correction |
Table 2.
Clinical results
| Patient | Pre-operative Cobb angle (°) | Post-operative Cobb angle (°) | Correction rate (%) | Loss of correction at follow-up (%) | Complication | ||||
|---|---|---|---|---|---|---|---|---|---|
| 3M | 6M | 12M | 24M | 36M | |||||
| 1 | 54 | 15 | 72 | Lost for follow-up | None | ||||
| 2 | 103 | 46 | 55 | 5 | 5 | 5 | 6 | 6 | None |
| 3 | 85 | 39 | 54 | 6 | 6 | 6 | Stress gastric ulcer | ||
| 4 | 80 | 35 | 56 | Lost for follow-up | Back pain | ||||
Discussion
Many studies have confirmed that the mechanical imbalance of the spine could lead to scoliosis [2, 7–10]. Injury of the paraspinal soft tissue beside the spine could result in this mechanical imbalance. Scar contracture due to back scalding or burning can also destroy this mechanical balance and cause scoliosis during the adolescent growth period. To our knowledge, adolescent scar contracture scoliosis caused by back scalding during infantile period has not been reported in current English literature. This type of scoliosis is seldom occurs. The pathogenesis of scar contracture scoliosis correlates more closely with the so-called pleural scoliosis following extensive pleural scarring from chronic infection.
The symmetric growth and development of bilateral soft tissues is very important to the mechanical balance of the spine. The skin, thoracolumbar fascia, intertransverse process ligament and paraspinal muscles, such as the rhomboid muscle, latissimus dorsi muscle, sacrospinalis and lumbar quadrate muscle, are all involved in the control and balance of the spine. Scalding during the infantile period can lead to contracture of these soft tissues and leave a large area of scar tissue, which can compromise the balance of the spine and lead to scoliosis and lodorsis. Due to the traction of the contractured scar tissues, the spine is convex toward the side without the contractured scar or with less scar tissue. During the adolescent growth spurt, the “bowstring effect” [5] of the contractured tissues becomes more apparent, which leads to the rapid progression of scoliosis. With the progression of the scoliosis, pelvic obliquity develops.
The diagnosis of scar contracture scoliosis is relatively easy. First, the patient has the experience of scalding during the infantile period. Second, the patient has a rapid progression of scoliosis during the adolescent growth spurt. Physical examination would find that the curve is convex toward the side without the contractured scar or with less scar tissue, which is different from the right side preference of thoracic AIS. Pelvic obliquity caused by contracture of the soft tissues is another characteristic of scar contracture scoliosis. For the traction of the contractured scar tissues, the iliac crest on the concave side of the scoliosis is higher than that on the convex side, which is the same as scoliosis caused by leg-length discrepancy.
The treatment for adolescent scar contracture scoliosis should follow individual and specific principles. Early recognition is very important for these patients. If there is a scar contracture in the back or armpit with imbalance tendency of the back soft tissue, the spine of the patient should be radiologically followed up regularly. Early management of skin contracture and bracing for spinal deformity should be proposed in case of development or progression of scoliosis. The contractured scar tissues should be sufficiently released before the correction of the scoliosis. In the first patient, the back scar excision, skin expansion and flap transfer were performed first. In the second patient, the preparative release surgery of soft tissues included stripping of paravertebral muscles, interception of contractured thoracolumbar fascia, iliocostal muscle and longissimus at different levels, excision of capsules and ligaments around the costo-transverse joints, the inter-transverse and intercostal muscles and the posterior section of the corresponding ribs. For the third patient, there was no management of the scalding due to the small amount of contractured scar for the correction of scoliosis. But anterior release and halo-femoral traction was mandatory for this patient. As for the fourth patient, because of local limited scar, scar excision, free skin grafting and anterior release were performed at the same stage.
In these four patients, scoliosis presented in only a short period after scalding and developed rapidly during the adolescent growth spurt. The curve types were single thoracic or long thoracolumbar curve, which was convex to the side without the contractured scar or with less scar tissue. Pelvic obliquity was found in all patients. The trunks shifted toward the convex side of the curve.
Pelvic obliquity is one key point of the treatment for scar contracture scoliosis, because a level pelvis is very important for a stable and balanced spine [11]. In the first patient, an anterior approach was used. An anterior approach could shorten the spine and reduce the bowstring effect of the contractured tissues, which would be beneficial for the correction of pelvic obliquity. In the other three patients, halo-femoral or wheelchair traction was performed before posterior correction. Huang et al. [3] suggested that halo-femoral traction before posterior spinal fusion could straighten the scoliotic spine, level the pelvis and thereby facilitate posterior instrumentation. The spine may be elongated during posterior surgery, but the contractured scar tissue was not elongated correspondingly. So theoretically, pelvis obliquity could become more progressive after posterior surgery. In this series, shortening the spine, multi-level “V” shape osteotomy, excision of joint capsule and yellow ligament were performed during posterior surgery.
Scar contracture in the back may biomechanically induce lordosis. The sagittal profile of the patients’ spine in this series does not present obvious lordosis or hyperkyphosis. This may be due to the locations of the scars. These four patients present scoliosis mainly because of the left–right imbalance produced by the scar contracture.
Compared with AIS, the wound of scar contracture scoliosis is more likely to get infected and its healing procedure is more difficult because of bad blood supply to the scar tissue. Two aspects should be noticed: (1) Manipulation during surgery should be gentle and repeated cutting with the electroscalpel should be avoided. (2) Keep the wound clean and dry and avoid compressing the wound.
Key points
The severe scar contracture caused by back scalding during the infantile period could lead to adolescent scoliosis.
Its pathogenesis and clinical manifestation are different from the typical adolescent idiopathic scoliosis.
The treatment of this kind of scoliosis should follow individual and specific principles.
Footnotes
The research was approved by the Ethics Committee of Nanjing University.
Contributor Information
Y. Qiu, Phone: +86-25-83105121, FAX: +86-25-83105121, Email: scoliosis2002@sina.com
S. F. Wang, Email: wangshoufeng@gmail.com
B. Wang, Email: scoliosis2002@sina.com
L. Wu, Email: Drwuliang@yahoo.com.cn
F. Zhu, Email: cnspine@hotmail.com
References
- 1.Chen SH, Chen PQ, Huang TJ, Ko JY, Wang CJ. Surgical correction of postradiation spinal deformity. Chang Gung Med J. 2003;26:160–169. [PubMed] [Google Scholar]
- 2.Durning RP, Scoles PV, Fox OD. Scoliosis after thoracotomy in tracheoesophageal fistula patients. A follow-up study. J Bone Joint Surg Am. 1980;62:1156–1159. [PubMed] [Google Scholar]
- 3.Huang MJ, Lenke LG. Scoliosis and severe pelvic obliquity in a patient with cerebral palsy: surgical treatment utilizing halo-femoral traction. Spine. 2001;26:2168–2170. doi: 10.1097/00007632-200110010-00026. [DOI] [PubMed] [Google Scholar]
- 4.Karski T. Hip abductor contracture as a biomechanical factor in the development of the so-called “idiopathic scoliosis”. Explanation of the etiology. Ann Univ Mariae Curie Sklodowska. 1997;52:87–94. [PubMed] [Google Scholar]
- 5.Liang D. An approach to correcting scoliosis. Mechanism and operative procedure. Zhonghua Wai Ke Za Zhi. 1991;29:228–230. [PubMed] [Google Scholar]
- 6.Machida M. Cause of idiopathic scoliosis. Spine. 1999;24:2576–2583. doi: 10.1097/00007632-199912150-00004. [DOI] [PubMed] [Google Scholar]
- 7.Rowe PW, Eagle M, Pollitt C, Bullock RE, Bushby KM. Multicore myopathy: respiratory failure and paraspinal muscle contractures are important complications. Dev Med Child Neurol. 2000;42:340–343. doi: 10.1017/S0012162200000591. [DOI] [PubMed] [Google Scholar]
- 8.Sengupta DK, Mehdian SH, McConnell JR, Eisenstein SM, Webb JK. Pelvic or lumbar fixation for the surgical management of scoliosis in Duchenne muscular dystrophy. Spine. 2002;27:2072–2079. doi: 10.1097/00007632-200209150-00020. [DOI] [PubMed] [Google Scholar]
- 9.Vaccaro AR, Silber JS. Post-traumatic spinal deformity. Spine. 2001;26:S111–S118. doi: 10.1097/00007632-200112151-00019. [DOI] [PubMed] [Google Scholar]
- 10.Biezen FC, Bakx PA, Villeneuve VH, Hop WC. Scoliosis in children after thoracotomy for aortic coarctation. J Bone Joint Surg Am. 1993;75:514–518. doi: 10.2106/00004623-199304000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Winter RB, Pinto WC. Pelvic obliquity. Its causes and its treatment. Spine. 1986;11:225–234. doi: 10.1097/00007632-198604000-00008. [DOI] [PubMed] [Google Scholar]