Abstract
Retrospective radiographic review of surgically treated double major curves (Lenke type 3C) in adolescent idiopathic scoliosis. To evaluate the role of selective posterior thoracic correction and fusion in double major curves with third generation instrumentation and to identify preoperative radiographic parameters that predict postoperative coronal spinal decompensation. Traditionally the surgical treatment of double major curves consists of fusion of both the thoracic and the lumbar curve. Few attempt to perform selective thoracic fusion in this curve pattern because of the potential to create spinal imbalance. Thirty-six patients with Lenke type 3C curves underwent a selective posterior thoracic correction and fusion with either Cotrel–Dubousset instrumentation or the Universal Spine System. Radiographs were evaluated to assess coronal and sagittal balance, curve flexibility, and curve correction at a minimum follow up of 2 years. Postoperative coronal spinal decompensation was investigated with respect to preoperative radiographic parameters on standing anteroposterior (AP), standing lateral radiographs, thoracic and lumbar supine side-bending radiographs. Coronal spinal decompensation was defined as plumbline deviation of C7 of more than 2 cm with respect to the centre sacral vertical line (CSVL) within 2 years of surgery. Twenty-six patients (72%) showed satisfactory frontal plane alignment patients (28%) showed coronal spinal decompensation. Significant group differences, however, were identified for lumbar apical vertebral rotation, measured according to Perdriolle (La scoliose. Son êtude tridimensionnelle. Maloine, Paris, pp 179, 1979) (A 16°, B 22°, P = 0.02), percentage correction (derotation) of lumbar apical vertebrae in lumbar supine side-bending films in comparison to standing AP radiographs (A 49%, B 27%, P = 0.002) and thoracic curve flexibility (A 43%, B 25%, P = 0.03). High correlation was noted between postoperative decompensation and derotation of lumbar apical vertebrae in pre-operative lumbar supine side-bending films with a critical value of 40% (Pearson correlation coefficient; P = 0.62, P < 0.001). Ten of 36 patients (28%) with Lenke type 3C adolescent idiopathic scoliosis showed coronal spinal decompensation of more than 2 cm after selective posterior thoracic correction and fusion. Lumbar apical vertebral derotation of less than 40% provided the radiographic prediction of postoperative coronal spinal imbalance. We advise close scrutiny of the transverse plane in the lumbar supine bending film when planning surgical strategy.
Keywords: Adolescent idiopathic scoliosis, Double major curve, Scoliosis correction, Spinal decompensation, Lenke classification
Introduction
The purpose of our study was to evaluate the role of selective posterior thoracic correction and fusion in double major curves with third generation instrumentation and to identify preoperative radiographic parameters that predict postoperative coronal spinal decompensation.
The intention of scoliosis surgery is to achieve a solid fusion and prevent curve progression by fusing the minimum number of segments. Both coronal and sagittal spinal balance should be achieved. According to Bridwell [3] the cranial and caudal extent of the fusion should be within the stable zone to obtain satisfactory spinal balance. Ideally the cranial and caudal segments included in the fusion should have neutral rotation. For curves fused into the lumbar spine, the last fused vertebra should be neutral, stable and should have minimum tilt postoperatively. In obtaining these goals, one should fuse the smallest number of spinal segments to preserve motion. This theory has been borne out, especially when fusing into the lumbar spine. The incidence of low back pain increases with the number of lumbar segments fused [7, 10, 15].
One of the basic principles in scoliosis surgery is to include structural curves within the fusion. The importance of defining structural curves becomes evident when one looks at classifications in everyday use. One of the most commonly used classifications in adolescent idiopathic scoliosis is that described by King et al. [12]. The authors describe five specific thoracic curve patterns in 405 patients and recommend different fusion levels for different curve patterns using Harrington rod instrumentation [11]. This classification worked well with Harrington rod instrumentation. However, when segmental instrumentation capable of three-dimensional correction was used the results became less reliable, particularly with King type II curves (false double major curve). These curves continue to generate controversy regarding the optimal surgical management with postoperative decompensation not infrequently occurring in selective fusions. Numerous studies into the cause and prevention of postoperative spinal imbalance are available. Authors cite different causative factors responsible for decompensation including the choice of fusion levels [5, 14, 25, 28], incorrect identification of curve patterns [13, 16], progression of the lumbar curve after surgery [16, 22], type of instrumentation used [5, 29, 33] and overcorrection of the thoracic curve [16, 33]. Some authors have suggested that King’s criteria for choosing fusing levels maybe invalid when using third generation instrumentation [5, 14, 29]. The reliability of the King classification has also been questioned [2, 9, 17]. It could be shown that one reason for poor reliability is disagreement on structural characteristics of lumbar curves among observers [2].
In 2001 a new classification was published by Lenke et al. [20]. This classification consists of three components: curve type (1 through 6), lumbar spine modifier (A, B, C) and a sagittal thoracic modifier (−, N, +) with 42 possibilities of curve type. The curve types have specific characteristics on coronal and sagittal radiographs that differentiate structural and non-structural curves. Based on these specific structural characteristics the authors make recommendations on the extent of the fusion. In many cases when a curve is assigned the lumbar modifier C, the lumbar spine should be included in the arthrodesis. However, the authors state that patients with type 1C and 2C curves may have selective thoracic fusion as long as an acceptable balance over the lumbar curve can be maintained. In the double major curves (type 3), especially with lumbar modifier C, where the lumbar curve is structural and deviates completely from the midline, the authors recommend fusion of both the thoracic and the thoracolumbar/lumbar components [20]. In contrast to King’s classification, the Lenke classification is a wholly radiographic classification and should display better reproducibility. Though the interobserver reproducibility seems to be better for Lenke’s classification [26], this does not necessarily mean the classification helps when choosing fusion levels [19].
The aim of our study were to evaluate the role for selective posterior thoracic correction and fusion in double major curves (Lenke type 3C) with third generation instrumentation and to identify preoperative radiographic parameters to predict postoperative coronal spinal decompensation in such cases.
Materials and methods
Thirty-six patients undergoing selective posterior thoracic correction and fusion for double major adolescent idiopathic scoliosis were included in the study. These patients were treated in two major spine centers in Europe between 1995 and 2000. In 21 patients Cotrel–Dubousset instrumentation [8] was used and in 15 patients the Universal Spine System was used. All patients were followed for a minimum of 2 years (mean 38 months, range 25–82). The average age at operation was 14 years + 2 months (range 12 + 1 to 17 + 4). All 36 cases were treated with a single posterior approach to the thoracic curve with the distal fusion levels ending at T11 (n = 1), T12 (n = 32) or L1 (n = 3). In all cases the lowest level of instrumentation was the stable vertebra. These patients had a retrospective clinical chart and radiographic review of preoperative, immediate postoperative and ultimate postoperative radiographs by two of us (HB, AAC).
Double major curves where both thoracic and lumbar curves were structural were identified on preoperative antero-posterior (AP) standing, supine side-bending and lateral standing radiographs as follows. According to Lenke et al. [20] a structural thoracic curve has a Cobb angle of ≥25° on supine side-bending radiographs and/or kyphosis between the tenth thoracic and the second lumbar level of at least +20°. A structural lumbar curve has a Cobb angle of ≥25° on supine side-bending radiographs and/or kyphosis between the tenth thoracic and the second lumbar level of at least +20°. Only curves with a lumbar modifier C, where the centre sacral vertical line (CSVL) does not touch the apical vertebral body or bodies immediately above and below the apical disc (if the apex is a disc) were included. The CSVL was drawn as a line that bisected the proximal sacrum, vertically to parallel the lateral edge of the upright radiograph.
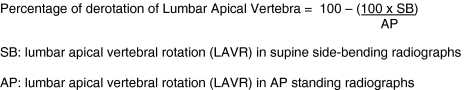
The thoracic and lumbar curves were measured according to Cobb on the pre-operative AP standing radiographs [6]. Additional measurements made included the thoracic apical vertebral translation (TAVT: defined as the distance in centimeters of the midpoint of the thoracic apical vertebra from the CSVL), the lumbar apical vertebral translation (LAVT: defined as the distance in centimeters of the midpoint of the lumbar apical vertebra from the CSVL), the lumbar apical vertebral rotation (LAVR) according to Perdriolle [27]. Coronal spinal balance was defined as the distance in centimeters of the midpoint of C7 from the CSVL on the AP standing lateral radiographs. From the supine side-bending radiographs the thoracic and lumbar curve magnitude, the flexibility index [12, 16], and the LAVR were assessed. From the LAVR obtained from AP standing and the LAVR obtained from the supine side-bending radiographs the percentage of correction (derotation) of lumbar apical vertebrae (LAV) was calculated (Fig. 1).
Fig. 1.
Percentage of derotation of
 . SB lumbar apical vertebral rotation (LAVR) in supine side-bending radiographs. AP lumbar apical vertebral rotation (LAVR) in AP standing radiographs
. SB lumbar apical vertebral rotation (LAVR) in supine side-bending radiographs. AP lumbar apical vertebral rotation (LAVR) in AP standing radiographs
Preoperative and postoperative sagittal radiographs were measured according to Cobb to determine thoracic kyphosis (T5–T12), thoracolumbar kyphosis (T10–L2) and lumbar lordosis (L1–L5). Sagittal balance was assessed by drawing a vertical line downward from the centre of the body of C7 to the area of the sacrum, measuring anterior or posterior displacement in centimeters from the midpoint of the sacrum as described by McCance et al. [21].
Consistent with other authors [21], coronal spinal decompensation was defined as deviation of C7 of greater than 2 cm from the CSVL. Patients were divided into two groups: Group A (compensated, satisfactory coronal balance) and Group B (decompensated). Statistical analysis was performed to determine whether significant differences existed between the compensated and decompensated group with respect to preoperative radiographic parameters on standing AP, standing lateral, thoracic and lumbar supine side-bending radiographs. Where data conformed to a normal distribution, parametric statistical analysis was applied, otherwise non-parametric tests were applied. For correlation analysis Pearson’s correlation coefficient was calculated. High correlation was noted between postoperative decompensation and a specific variable. A 2 × 2 contingency table was used to consider the probability of this specific variable to predict postoperative spinal decompensation. All test results where P < 0.05 were considered statistically significant.
Results
Twenty-six patients (72%) showed satisfactory frontal plane alignment by means of C7 plumb line deviation (group A, mean = 1.2 cm to the left), whereas 10 patients (28%) showed coronal spinal decompensation (group B, mean = 2.7 cm to the left).
The two groups were statistically equivalent in terms of preoperative C7 plumb line deviation (A 0.8 cm, B 0.7 cm to the left, P = 0.112), thoracic Cobb angles (A 56°, B 62° P = 0.093), lumbar Cobb angles (A 42°, B 47° P = 0.115), lumbar curve flexibility (A 78%, B 67%, P = 0.153), lumbar apical vertebral translation (A 2.5 cm to the left, B 2.8 cm to the left, P = 0.124), thoracic kyphosis from T5–T12 (P = 0.153), thoraco lumbar kyphosis from T10–L2 (P = 0.454), lumbar lordosis from L1–L5 (p = 0.534), sagittal C7 alignment (A 0.5 cm posterior, B 0.7 cm posterior, P = 0.165) and age at operation (A 14 + 4, B 15 + 1, P = 0.195).
Significant group differences were identified for lumbar apical vertebral rotation measured according to Perdriolle [27]. (A 16°, B 22°, P = 0.02) and the percentage correction (derotation) of lumbar apical vertebrae in lumbar supine side-bending films when compared to AP standing radiographs (A 49%, B 27%, P = 0.002) and for thoracic curve flexibility (A 43%, B 25%, P = 0.03).
Average thoracic curve correction was 51% in group A and 41% in group B (P = 0.05). Average lumbar curve correction was 34% in group A and 23% in group B (P = 0.09). No group differences were identified for postoperative thoracic kyphosis, lumbar lordosis or sagittal C7 alignment (A 1.2 cm post, B 1.6 cm post P = 0.092). Mean values and standard deviation for these parameters in both the compensated and decompensated curves are summarized in Table 1.
Table 1.
Radiographic measurements
| Group A compensated (n = 26) | Group B decompensated (n = 10) | P | |||
|---|---|---|---|---|---|
| M | SD | M | SD | ||
| Preop thoracic | 56 | 7 | 62° | 13 | NS |
| Impost thoracic | 24 | 9 | 32 | 10 | 0.05 |
| Two year post thoracic | 27 | 7 | 37 | 8 | 0.04 |
| Thoracic curve correction (%) | 51 | 12 | 41 | 12 | 0.05 |
| Thoracic SB | 31 | 12 | 47 | 16 | 0.02 |
| Thoracic curve flexibility (%) | 43 | 16 | 25 | 12 | 0.03 |
| Preop lumbar | 42 | 10 | 47 | 5 | NS |
| Impost lumbar | 31 | 12 | 35 | 9 | NS |
| Two years post lumbar | 28 | 11 | 36 | 9 | NS |
| Lumbar correction (%) | 34 | 21 | 23 | 20 | NS |
| Lumbar SB | 33 | 13 | 32 | 18 | NS |
| Lumbar curve flexibility (%) | 78 | 28 | 67 | 23 | NS |
| Lumbar AVR AP | 16 | 7 | 22 | 5 | 0.03 |
| Lumbar AVR SB | 10 | 8 | 17 | 7 | 0.02 |
| Percent derotation LAV (%) | 49 | 25 | 27 | 21 | 0.002 |
| Preop lumbar AVT | 2.5 | 0.8 | 2.9 | 1.1 | NS |
| Postop lumbar AVT | 1.4 | 0.6 | 1.8 | 1 | NS |
| Preop C7 PL deviation | −0.8 | 0.9 | −0.7 | 0.6 | NS |
| Two years post C7 PL deviation | −1.2 | 0.9 | −2.7 | 0.8 | 0.003 |
| Preop sagittal T5–12 | 27 | 11 | 36 | 16 | NS |
| Postop sagittal T5–12 | 25 | 6 | 31 | 8 | NS |
| Preop sagittal L1–5 | 40 | 10 | 44 | 17 | NS |
| Postop sagittal L1–5 | 41 | 8 | 45 | 8 | NS |
Preop thoracic preoperative thoracic Cobb measurement (°), impost thoracic immediate postoperative thoracic Cobb measurement (°), Two years post thoracic Two years postoperative thoracic Cobb measurement (°), SB Cobb measurement on side-bending radiograph (°), AVR AP apical vertebral rotation on AP standing radiographs acc. to Perdriolle (°), AVR SB apical vertebral rotation on supine side-bending radiographs acc. to Perdriolle (°), LAV lumbar apical vertebrae, AVT apical vertebral translation measured in cm from the CSVL, PL plumbline deviation measured in cm from the CSVL (− indicates left from CSVL), sagittal Cobb measurement on lateral radiographs (°)
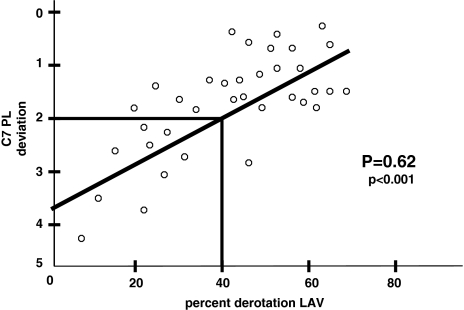
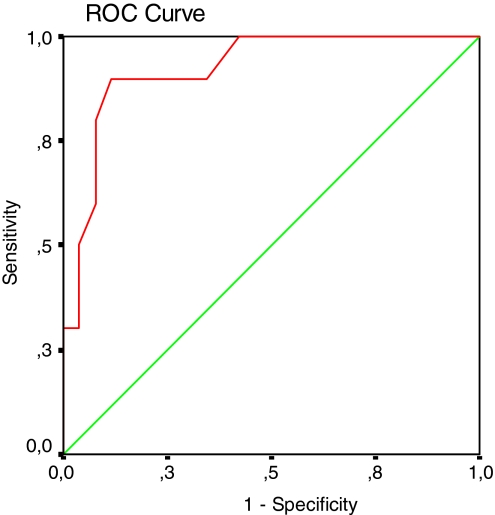
High correlation was identified between C7 plumb line coronal deviation postoperatively and derotation of lumbar apical vertebrae in lumbar supine side-bending films (Pearson correlation coefficient P = 0.62, P < 0.001; Table 2). Data are shown as scatter plot in Fig. 2. A 2 × 2 contingency table was used to consider the probabilities that the test-variable (derotation of lumbar apical vertebrae >40%/<40%) predicts postoperative spinal balance or decompensation. The positive predictive value was 0.95 (95% CI 0.86–0.99), the negative predictive value 0.64 (95% CI 0.39–0.89) respectively. Sensitivity was 0.81 (95% CI 0.65–0.96) and specificity 0.90 (95% CI 0.71–1.0). The positive Likelihood-ratio was 8.1 (Table 3). The cut point for decompensation was determined by means of a ROC curve and was calculated (multiple regression analysis) between 39 and 40% derotation of lumbar apical vertebrae (Fig. 3).
Table 2.
Correlation of various radiographic measurements with postoperative coronal decompensation
| A compensated | B decompensated | |
|---|---|---|
| Preop C7 PL deviation | NS | NS |
| Preop thoracic | NS | NS |
| Thoracic SB | NS | NS |
| Thoracic curve flexibility (%) | NS | 0.061 |
| Two years post thoracic | NS | NS |
| Preop thoracic AVT | NS | 0.058 |
| Postop thoracic AVT | NS | NS |
| Preop lumbar | NS | NS |
| Lumbar SB | NS | NS |
| Lumbar curve flexibility (%) | NS | NS |
| Two years post lumbar | NS | NS |
| Preop lumbar AVT | NS | NS |
| Postop lumbar AVT | NS | NS |
| Preop lumbar AVR AP | 0.048 | 0.037 |
| Preop lumbar AVR SB | 0.063 | 0.042 |
| Percent derotation LAV | 0.005 | <0.001 |
| Preop sagittal T5–12 | NS | NS |
| Postop sagittal T5–12 | NS | NS |
| Preop sagittal T10–L2 | NS | NS |
| Postop sagittal T10–L2 | NS | NS |
| Preop sagittal L1–5 | NS | NS |
| Postop sagittal L1–5 | NS | NS |
Correlation of various radiographic measurements with postoperative coronal decompensation expressed as Pearson correlation coefficients, significance set at P < 0.05
PL Plumbline deviation measured in cm from the CSVL, preop thoracic preoperative thoracic Cobb measurement (°), SB Cobb measurement on side-bending radiographs (°), Two years post thoracic 2 years postoperative Cobb measurement (°), AVT apical vertebral translation measured in cm from the CSVL, AVR AP apical vertebral rotation on AP standing radiographs acc. to Perdriolle (°), AVR SB apical vertebral rotation on supine side-bending radiographs acc. to Perdriolle (°), LAV lumbar apical vertebrae, AVT apical vertebral translation measured in cm from the CSVL, sagittal Cobb measurement on lateral radiographs (°)
Fig. 2.
Scatter plot Correlation of parameters expressed as Pearson correlation coefficient, significance set at P < 0.05. C7 PL deviation C7 plumbline deviation measured in centimeter from the CSVL. LAV lumbar apical vertebrae
Table 3.
2 × 2 contingency table test
| Derotation of LAV > 40% | Derotation of LAV < 40% | Σ | |
|---|---|---|---|
| C7 plumbline deviation <2 cm | 21 | 5 | 26 |
| C7 plumbline deviation > 2cm | 1 | 9 | 10 |
| 22 | 14 | 36 |
Positive predictive value: 21/22 (0.95; 95% CI 0.86–0.99); Negative predictive value: 9/14 (0.64; 95% CI 0.39–0.89); Sensitivity: 21/26 (0.81; 95% CI 0.65–0.96); Specificity: 9/10 (0.90; 95% CI 0.71–1.0); Positive Likelihood-ratio 8.1
LAV lumbar apical vertebrae; CI confidence interval
Fig. 3.
ROC curve. The cut point for decompensation was determined by means of a multiple regression analysis and was calculated between 39° and 40° derotation of lumbar apical vertebrae
There was no association between postoperative coronal decompensation and the instrumentation system used, thoracic and lumbar curve flexibility, lumbar apical vertebral translation, pre- and post-operative sagittal C7 alignment or thoracic curve correction (Table 2).
Discussion
Central to the issue of postoperative decompensation in adolescent idiopathic scoliosis is the distinction between structural and compensatory curves and the appropriate selection of fusion levels. Controversy exists regarding the operative treatment of double major curves. Most authors however, would recommend fusion of both the thoracic and the lumbar curve [1, 16, 18, 20, 24]. In contrast, Large et al. [15] reported on 44 patients with double major curves treated with selective fusion of the thoracic curve using Harrington Rod instrumentation system or the Dwyer system with a minimum 10-year follow-up. The authors report satisfactory results with regard to spinal balance and overall clinical outcome. The greater the number of lumbar segments fused the higher the incidence of subsequent low back pain. However a limitation of this study was that in only 30 of 44 patients were lateral bending films of the lumbar spine available. It is not clear how the authors assessed whether the lumbar curves were structural or compensatory in the remaining 14 cases.
Salanova et al. [31] reported satisfactory coronal spinal balance with only 10% imbalanced curves when the lower extent of fusion was the elected vertebra (end vertebra). King et al. [12] used side-bending radiographs to differentiate between structural and compensatory curves. The authors defined five specific thoracic curve patterns and identified the stable vertebra as the caudal extent of instrumentation (Harrington rod system) to establish satisfactory postoperative spinal balance. Despite the advent of segmental instrumentation, this method has remained popular in the preoperative planning of fusion levels for those with thoracic adolescent idiopathic scoliosis [14, 30]. Various reports of postoperative coronal spinal decompensation have led some authors to question the value of King’s Classification in identifying appropriate fusion levels, particularly when applying segmental correction forces [5, 14, 28, 29]. Others have questioned the inter- and intra-observer reliability of the King Classification [2, 9, 17].
Lenke’s method involves an assessment of the curve in two planes, but does not include an assessment in the transverse plane. Different curve types have specific coronal and sagittal radiographic characteristics as mentioned previously. To differentiate between structural and compensatory curves in the coronal plane supine side-bending radiographs are used [20]. King’s method also uses side-bending radiographs to differentiate between structural and compensatory curves. However, there is disagreement on defining characteristics of structural curves [2]. It has been proven in various studies that spinal decompensation occurs when King’s criteria are applied to the selection of fusion levels prior to instrumentation with third generation systems [4, 13, 14, 16, 22, 23, 28, 29, 30, 32, 33]. Lenke et al. [16] has focused on the differentiation between double major and false double major (King type II) curves. The authors note early postoperative coronal decompensation in King type II curve patterns (thoracic > lumbar curve, positive flexibility index) which satisfied King’s criteria for selective thoracic fusion. These curves had a significant lumbar curve, lumbar apical vertebral rotation and lumbar apical vertebral translation. Based on their operative results the authors suggest calculation of the ratios of the thoracic and lumbar curve magnitude, the ratio of thoracic versus lumbar apical vertebral rotation (AVR) and apical vertebral translation (AVT) on preoperative AP standing radiographs. If these ratios are >1.2 (curve magnitude), >1.0 (AVR), >1.0 (AVT) then selective thoracic fusion could be performed successfully. Lumbar bending films were not helpful in this study to distinguish between double major and false double major curves [16]. Like King’s classification, the Lenke classification relies (not exclusively) on supine side-bending films to identify structural curves. The authors suggest that a curve with a Cobb angle of ≥25° on supine side-bending radiographs is structural.
Lenke [20] recommends fusing both curves of a double major curve pattern, particularly for those with a lumbar modifier C, to achieve satisfactory postoperative spinal balance. In our study, we performed selective thoracic fusion. Most of our patients should have been decompensated, but 26 out of 36 patients (72%) showed satisfactory postoperative coronal spinal balance. Lenke [16] and the results obtained in our study suggest that neither the Cobb angle observed on the lumbar side-bending radiographs nor the lumbar curve flexibility correlates with post-operative decompensation (Table 2). We would suggest the importance of the Cobb angle (AP standing radiograph compared to the supine lumbar side-bending radiograph) is overestimated as a method of solely distinguishing between structural or compensatory curves. Other parameters need to be considered to explain postoperative coronal spinal decompensation. From all the pre- and post-operative radiographic parameters measured in our study the most significant for predicting decompensation was the percent derotation of lumbar apical vertebrae (LAV) observed when comparing the standing AP film with the lumbar supine side-bending films (Table 1). Derotation of LAV of 40% seems to be critical with respect to postoperative decompensation (Fig. 2). In our series, if the lumbar apical derotation observed on the supine side bending film was less than 40%, the specificity of predicting spinal decompensation was 90% (Figs. 4, 5).
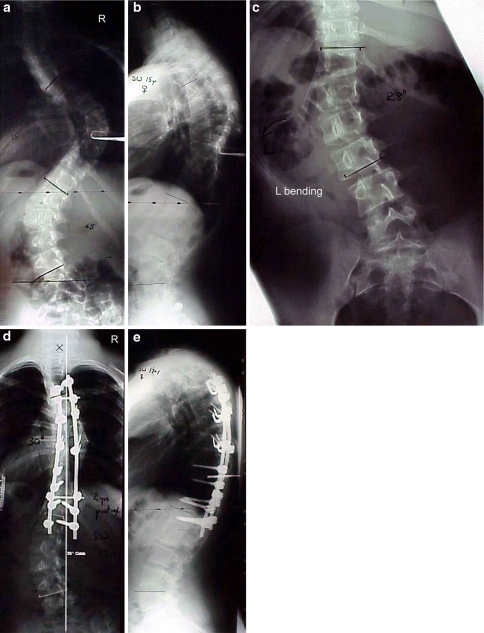
Fig. 4.
Case 1. a S.W. female, 15 years. Preoperative standing AP radiograph showed a right thoracic curve of 85° Cobb angle and a left lumbar curve of 65° Cobb angle. Lumbar apical vertebral rotation of L2 was 39° according to Perdriolle. b Preoperative standing lateral radiograph showed thoracic kyphosis T5–T12 of 48° and lumbar lordosis L1–L5 of 26°. cLeft side bending corrected the lumbar curve to 28° Cobb angle, and lumbar apical vertebral rotation to 23° for 41% correction. (Right side bending corrected the thoracic curve to 48° Cobb angle). d The patient underwent posterior correction and fusion with USS from T4 to L1 and was presented at 2 years follow up with satisfactory frontal and sagittal spinal alignment. Two years postoperative standing AP radiograph showed a thoracic Cobb angle of 30° and a lumbar Cobb angle of 23°. C7 plumb line deviation of C7 was 1.2 cm to the left. e Two years postoperative standing lateral radiograph: Thoracic kyphosis from T5–T12 of 46°, lumbar lordosis from L1–L5 of 28° Cobb angle
Fig. 5.
Case 1. a D.B. female, 14 years. Preoperative standing AP radiograph showed a right thoracic curve of 69° Cobb angle and a left lumbar curve of 52° Cobb angle. Lumbar apical vertebral rotation of L2 was 34° according to Perdriolle. b Preoperative standing lateral radiograph showed thoracic kyphosis T5–T12 of 34° and lumbar lordosis L1–L5 of 40°. cLeft side bending corrected the lumbar curve to 26° Cobb angle, and lumbar apical vertebral rotation to 30° for 12% correction. (Right side bending corrected the thoracic curve to 36°° Cobb angle). d The patient underwent posterior correction and fusion with USS from T3 to T11. At 2 years follow up the patient complained about coronal spinal imbalance to the left. Clinically plumb line deviation to the left of 3.5 cm was evident. Two years postoperative standing AP radiograph showed spinal decompensation to the left with respect to C7 of 3.6 cm. Thoracic Cobb angle was 25° and the lumbar Cobb angle was 34°, respectively. e Two years postoperative standing lateral radiograph: Thoracic kyphosis from T5–T12 of 15°, lumbar lordosis from L1–L5 of 55° Cobb angle
Traditionally radiographic features of a structural curve include a side bending Cobb angle of ≥25°, flexibility index and whether the curve crosses the CSVL. In our series, none of these features in lumbar curves correlated with, or where predictive for postoperative decompensation after selective fusion of the thoracic curve in the treatment of double major curves. Only the percent derotation of lumbar apical vertebrae determined on lumbar supine side-bending films provided the radiographic prediction of postoperative coronal spinal imbalance.
The results of our study were obtained by means of a post hoc analysis. Therefore a second study will be performed to prove our hypothesis.
Conclusion
Twenty-six of 36 patients (72%) with Lenke type 3C adolescent idiopathic scoliosis treated with selective thoracic correction and fusion showed satisfactory coronal plane alignment 2 years after surgery. Ten of 36 patients (28%) showed coronal spinal decompensation of more than 2 cm, 2 years after surgery. Lumbar apical vertebral derotation of less than 40% on lumbar supine side-bending films provided the radiographic prediction of postoperative coronal spinal imbalance. We advise close scrutiny of the transverse plane in the lumbar supine side-bending film when planning surgical strategy.
References
- 1.Barr SJ, Schuette AM, Emans JB. Lumbar pedicle screws versus hooks. Results in double major curves in adolescent idiopathic scoliosis. Spine. 1997;22:1369–1379. doi: 10.1097/00007632-199706150-00016. [DOI] [PubMed] [Google Scholar]
- 2.Behensky H, Giesinger K, Ogon M, Krismer M. Multi surgeon assessment of coronal pattern classification systems of adolescent idiopathic scoliosis. Reliability and error analysis. Spine. 2002;16:769–777. doi: 10.1097/00007632-200204010-00015. [DOI] [PubMed] [Google Scholar]
- 3.Bridwell KH. Spine update. Surgical treatment of adolescent idiopathic scoliosis. The basics and the controversies. Spine. 1994;19:1095–1100. doi: 10.1097/00007632-199405000-00020. [DOI] [PubMed] [Google Scholar]
- 4.Bridwell KH, Betz RR, Capelli AM, Huss G, Harvey C. Sagittal plane analysis in idiopathic scoliosis patients treated with Cotrel–Dubousset instrumentation. Spine. 1990;15:921–926. doi: 10.1097/00007632-199009000-00016. [DOI] [PubMed] [Google Scholar]
- 5.Bridwell KH, Mc Allister JW, Betz RR, Huss G, Clancy M, Schoenecker PL. Coronal decompensation produced by Cotrel–Dubousset “derotation” maneuver for idiopathic right thoracic scoliosis. Spine. 1991;16:769–777. doi: 10.1097/00007632-199107000-00015. [DOI] [PubMed] [Google Scholar]
- 6.Cobb JR. Outline for the study of scoliosis. Am Acad Orthop Surg Lect. 1948;5:261–275. [Google Scholar]
- 7.Cochran T, Instram L, Nachemson A. Long term anatomic and functional changes in patients with adolescent idiopathic scoliosis treated by Harrington rod fusion. Spine. 1983;8:576–584. doi: 10.1097/00007632-198309000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Cotrel Y, Dubousset J, Guillaumat M. New universal instrumentation in spinal surgery. Clin Orthop. 1988;227:10–23. [PubMed] [Google Scholar]
- 9.Cummings RJ, Loveless EA, Campbell J, Samelson S, Mazur J. Interobserver reliability and intraobserver reproducibility of the system of King et al. for the classification of adolescent idiopathic scoliosis. J Bone Joint Surg. 1998;80A:1107–1111. doi: 10.2106/00004623-199808000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Edgar MA, Mehta MH. Long-term follow-up of fused and unfused idiopathic scoliosis. J Bone Joint Surg. 1998;70B:712–716. doi: 10.1302/0301-620X.70B5.3192566. [DOI] [PubMed] [Google Scholar]
- 11.Harrington PR. Treatment of scoliosis: correction and internal fixation by spine instrumentation. J Bone Joint Surg. 1962;44A:591–610. [PubMed] [Google Scholar]
- 12.King HA, Moe JH, Bradford DS, Winter RB. The selection of fusion levels in thoracic idiopathic scoliosis. J Bone Joint Surg. 1983;65A:1302–1313. [PubMed] [Google Scholar]
- 13.King HA. Analyses and treatment of type II idiopathic scoliosis. Orthop Clin North Am. 1994;25:225–237. [PubMed] [Google Scholar]
- 14.Knapp DR, Jr, Price CT, Jones ET, Coonrad RW, Flynn JC. Choosing fusion levels in progressive thoracic idiopathic scoliosis. Spine. 1992;17:1159–1165. doi: 10.1097/00007632-199210000-00006. [DOI] [PubMed] [Google Scholar]
- 15.Large DF, Doig WG, Dickens DRV, Torode IP, Cole WG. Surgical treatment of double major scoliosis. Improvement of the lumbar curve after fusion of the thoracic curve. J Bone Joint Surg. 1991;73B:121–124. doi: 10.1302/0301-620X.73B1.1991744. [DOI] [PubMed] [Google Scholar]
- 16.Lenke LG, Bridwell KH, Baldus CB, Blanke K. Preventing decompensation in King type II curves treated with Cotrel–Dubousset instrumentation. Strict guidelines for selective thoracic fusion. Spine. 1992;17(8 Suppl):274–281. doi: 10.1097/00007632-199208001-00011. [DOI] [PubMed] [Google Scholar]
- 17.Lenke LG, Betz RR, Bridwell KH, Clements DH, Harms J, Lowe TG, Shufflebarger HL. Intraobserver and interobserver reliability of the classification of thoracic adolescent idiopathic scoliosis. J Bone Joint Surg. 1998;80A:1097–1106. doi: 10.2106/00004623-199808000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Lenke LG, Betz RR, Haher T, Clements D, Merola AA, Haher T, Lowe T, Newton P, Bridwell KH, Blanke K. Curve prevalence of a new classification of operative adolescent idiopathic scoliosis. Spine. 2002;27:604–611. doi: 10.1097/00007632-200203150-00008. [DOI] [PubMed] [Google Scholar]
- 19.Lenke LG, Betz RR, Haher T, Lapp MA, Merola AA, Harms J, Shufflebarger HL. Multisurgeon assessment of surgical decision-making in adolescent idiopathic scoliosis. Spine. 2001;26:2347–2353. doi: 10.1097/00007632-200111010-00011. [DOI] [PubMed] [Google Scholar]
- 20.Lenke LG, Betz RR, Harms J, Bridwell KH, Clements DH, Lowe TG, Blanke K. Adolescent idiopathic scoliosis. A new classification to determine extent of spinal arthrodesis. J Bone Joint Surg. 2001;83A:1169–1181. [PubMed] [Google Scholar]
- 21.McCance SE, Denis F, Lonstein JE, Winter RB. Coronal and sagittal balance in surgically treated adolescent idiopathic scoliosis with the King II curve pattern. A review of 67 consecutive cases having selective thoracic arthrodesis. Spine. 1998;23:2063–2073. doi: 10.1097/00007632-199810010-00005. [DOI] [PubMed] [Google Scholar]
- 22.McCall RE, Bronson W. Criteria for selective fusion in idiopathic scoliosis using Cotrel–Dubousset instrumentation. J Pediatr Orthop. 1992;12:475–479. doi: 10.1097/01241398-199207000-00011. [DOI] [PubMed] [Google Scholar]
- 23.Mielke CH, Lonstein JE, Denis F, Vandenbrink K, Winter RB. Surgical treatment of adolescent idiopathic scoliosis. J Bone Joint Surg. 1989;71A:1170–1177. [PubMed] [Google Scholar]
- 24.Moe JH, Byrd J, Abott III. Idiopathic scoliosis. In: Bradford DS, Lonstein JE, Moe JH, Ogilvie JW, Winter RB, editors. Moe’s textbook of scoliosis and other spinal deformities. Philadelphia: WB Saunders; 1987. pp. 191–232. [Google Scholar]
- 25.Moore MR, Baynham GC, Brown CW, Donaldson DH, Odom JA., Jr Analyses of factors related to truncal decompensation following Cotrel–Dubousset instrumentation. J Spinal Disord. 1991;4:188–192. doi: 10.1097/00002517-199106000-00009. [DOI] [PubMed] [Google Scholar]
- 26.Ogon M, Giesinger K, Behensky H, Wimmer C, Nogler M, Bach C, Krismer M. Interobserver and intraobserver reliability of Lenke’s new classification system. Spinal decompensation in Cotrel–Dubousset instrumentation. Spine. 2002;27:858–862. doi: 10.1097/00007632-200204150-00014. [DOI] [PubMed] [Google Scholar]
- 27.Perdriolle R. La scoliose. êtude tridimensionnelle. Paris: Maloine; 1979. p. 179. [Google Scholar]
- 28.Puno RM, Grossfeld SL, Johnson JR, Holt RT. Cotrel–Dubousset instrumentation in idiopathic scoliosis. Spine. 1992;17:258–262. doi: 10.1097/00007632-199208001-00008. [DOI] [PubMed] [Google Scholar]
- 29.Richards BS, Birch JG, Herring JA, Johnston CE, Roach JW. Frontal plane and sagittal plane balance following Cotrel–Dubousset instrumentation for idiopathic scoliosis. Spine. 1989;14:733–737. doi: 10.1097/00007632-198907000-00015. [DOI] [PubMed] [Google Scholar]
- 30.Roye DP, Jr, Farcy JP, Rickert JB, Godfried D. Results of spinal instrumentation of adolescent idiopathic scoliosis by King type. Spine. 1992;17:270–273. doi: 10.1097/00007632-199208001-00010. [DOI] [PubMed] [Google Scholar]
- 31.Salanova C, Dubousset J, Moreno P, Boulot J. Segmental instrumentation in idiopathic scoliosis. Role of the upright frontal plane for determination of the area of fusion. Rev Chir Orthop Reparatrice Appar Mot. 2000;86:441–451. [PubMed] [Google Scholar]
- 32.Shufflebarger HL, Clark CE. Fusion levels and hook patterns in thoracic scoliosis with Cotrel–Dubousset instrumentation (CDI) Spine. 1990;15:916–920. doi: 10.1097/00007632-199009000-00015. [DOI] [PubMed] [Google Scholar]
- 33.Thompson JP, Transfeldt EE, Bradford DS, Ogilvie JW, Boachie-Adjei O. Decompensation after Cotrel–Dubousset instrumentation of idiopathic scoliosis. Spine. 1990;15:927–931. doi: 10.1097/00007632-199009000-00017. [DOI] [PubMed] [Google Scholar]