Abstract
Objective
Effort‐reward imbalance at work is an established psychosocial risk factor but there are also newer conceptualisations, such as procedural injustice (decisions at work lack consistency, openness and input from all affected parties) and relational injustice (problems in considerate and fair treatment of employees by supervisors). The authors examined whether procedural injustice and relational injustice are associated with employee health in addition to, and in combination with, effort‐reward imbalance.
Methods
Prospective survey data from two cohorts related to public‐sector employees: the 10‐Town study (n = 18 066 (78% women, age range 19–62) and the Finnish Hospital Personnel study (n = 4833, 89% women, age range 20–60). Self‐rated poor health, minor psychiatric morbidity and doctor‐diagnosed depression were assessed at baseline (2000–2) and at follow‐up (2004). To determine incident morbidity, baseline cases were excluded.
Results
In multivariate models including age, sex, occupational status and all three psychosocial factors as predictors, high effort‐reward imbalance and either high procedural injustice or high relational injustice were associated with increased morbidity at follow‐up in both cohorts. After combining procedural and relational injustice into a single measure of organisational injustice, high effort‐reward imbalance and high injustice were both independently associated with health. For all outcome measures, a combination of high effort‐reward imbalance and high organisational injustice was related to a greater health risk than high effort‐reward imbalance or injustice alone.
Conclusion
Evidence from two independent occupational cohorts suggests that procedural and relational components of injustice, as a combined index, and effort‐reward imbalance are complementary risk factors.
A number of theoretical conceptualisations of stressful experience at work have been described, but only a few have proven their ability to predict the incidence of disease in prospective epidemiological studies.1 The effort‐reward imbalance model is one such concept that was repeatedly found to be associated with significantly increased risks of physical and mental disorders, such as cardiovascular disease, depression, alcohol dependence or type 2 diabetes.2,3 This model is based on the fundamental sociological notion of contractual reciprocity where any normative action provided by person A to person B that has some utility to B is expected to elicit an equivalent return from person B to A.4 As is the case with other types of relevant social exchange, this notion lies at the core of the employment contract which defines distinct obligations or tasks to be performed in exchange with equitable rewards.
The model of effort‐reward imbalance at work claims that lack of reciprocity between costs and gains (that is, high‐cost low‐gain conditions) occurs frequently under specific circumstances and elicits strong negative emotions, with particular propensity to sustained autonomic and neuroendocrine activation and their adverse long‐term consequences for health. In this model, three types of reward are distinguished: money, esteem and promotion prospects including job security. The specific circumstances in which effort‐reward imbalance is frequent are when employees have no alternative choice in the labour market, when they strive for highly competitive jobs, or when they exhibit a motivational pattern of excessive work‐related “overcommitment”.
In the framework of justice theory, effort‐reward imbalance concerns injustice of exchange or, if scarce rewards are to be assigned to several people, distributive injustice.5 It is of interest to learn how this type of injustice relates to other types of injustice at work, such as procedural and relational injustice.6,7,8 Moreover, it is unknown whether each type of injustice elicits similar experiences of psychosocial stress at work and, thus, may be associated with comparable health outcomes. Procedural justice concerns the conformity to agreed‐upon formal procedures within an organisation that guarantee fair and consistent decision‐making, whereas relational justice describes the extent to which employees are treated with respect and fairness by their supervisors. In several recent epidemiological investigations, procedural and/or relational injustice were related to adverse health.9,10,11,12,13 However, these reports raised some critical comments as the conceptual and operational similarities with and differences from earlier established concepts of psychosocial stress at work remain unclear.14 To our knowledge, no previous study has examined whether procedural injustice and relational injustice are complementary or redundant to effort‐reward imbalance as health risk factors.
In this paper, we compare the notions of injustice of exchange (effort‐reward imbalance), procedural and relational injustice at the operational level, and we examine their independent contribution to employee health in two prospective epidemiological investigations. Moreover, in the Discussion section, conceptual similarities and differences between the three notions of injustice are elaborated.
Methods
Study population and design
We used data from the 10‐Town study15 and the Finnish Hospital Personnel study16 in Finland. The former is focused on all 47 351 local government employees (72% women, mean age 44.5 years) in 10 Finnish towns at baseline in 2000 and 2001, and the latter investigation is focused on all 21 938 employees (84% women, mean age 43.1 years) in the service of 21 public hospitals in Finland in 2000–2. At baseline, a standardised questionnaire on psychosocial stress at work and on health was sent to all these employees. In both studies, a follow‐up survey was sent for those remaining in the service of the target organisations in 2004.
Respondents at baseline were 31 749 employees (response rate 67%; 77% women, mean age 44.9 years) in the 10‐Town study and 15 338 employees (response rate 70%) in the Hospital Personnel study. In the latter study the survey instrument for seven hospitals did not include the measure of effort‐reward imbalance, thus reducing the number of participants at baseline to 8001 (88% women, mean age 44.3 years) in that cohort.
The follow‐up survey was sent for those remaining in the service of the target organisations (n = 24 196 in the 10‐Town study; n = 6021 in the Hospital Personnel study). Of these, 19 077 employees from the 10‐Town study (response rate 79%) and 4974 employees from the Hospital Personnel study (response rate 83%) responded to the follow‐up survey.
After exclusion of those with missing data on exposure or outcomes, the final cohorts included 18 066 employees (78% women, mean age 44.9 years) in the 10‐Town study and 4833 (89% women, mean age 44.3) in the Hospital Personnel study. The proportions of women and, in the 10‐Town study, also older employees were slightly higher among participants than in the baseline respondents.
Assessment of effort‐reward imbalance
In these two studies, only proxy measures of the two components “effort” and “reward” of this model were available.17 “Effort” was measured with one question (“How much do you feel you invest in your job in terms of skill and energy?”) and “reward” was assessed with a scale containing three questions about feelings of getting a return from work in terms of (1) income and job benefits, (2) recognition and prestige, and (3) personal satisfaction (α = 0.64 in the 10‐Town study and 0.62 in the Hospital personnel study). The response format for all the questions was a Likert scale (1 = “very little” to 5 = “very much”). For each participant, we averaged the scores of the three items. Following an established procedure,18 a ratio was constructed with the “effort” score in the numerator and the “reward” score in the denominator, adjusting for unequal number of items where higher values indicate imbalance between high costs and low rewards.
Assessment of procedural and relational justice
Standard questionnaires of procedural justice (seven items, α = 0.92 in the 10‐Town study and 0.89 in the Hospital personnel study) and relational justice (six items, α = 0.92 in the 10‐Town study and 0.92 in the Hospital personnel study) were used.7 Response format for all the questions was a five‐point Likert scale (1 = “very little” to 5 = “very much”). For each participant, we averaged the scores of the items from both scales. To simplify comparisons between effort‐reward imbalance and organisational justice, scores of the scales assessing level of procedural and relational justice were reversed such that higher values indicate greater injustice.
Assessment of health
We assessed incident poor self‐rated health status, minor psychiatric disorders and doctor‐diagnosed depression with standard self‐assessment instruments in both studies.
Incident poor self‐rated health
The respondents made an assessment of their health using a five‐point scale (1 = very good, 2 = good, 3 = average, 4 = poor, 5 = very poor). This measure was dichotomised and used as an indicator of poor self‐rated health (average or worse vs good or very good). This is one of the most widely used measures of health status,19 shown to be related to a number of important medical endpoints,20,21,22 and sensitive to changes in health status.20,23 Participants with poor self‐rated health at baseline were excluded from the analysis and incident poor self‐rated health was determined based on follow‐up values.
Incident minor psychiatric disorder
Minor psychiatric morbidity was assessed using the 12‐item version of the General Health Questionnaire (GHQ)24 (α = 0.89 in both cohorts). Individuals scoring ⩾4 are estimated to have mental distress according to studies validating GHQ‐12 against standardised psychiatric interviews,24 and this threshold was applied in the present study to identify people with minor psychiatric morbidity at baseline and follow‐up. GHQ cases at baseline were excluded from the analysis and incident cases were determined based on follow‐up GHQ‐caseness.
Incident doctor‐diagnosed depression
The participants were asked the following question: “Do you have or have you had any of the following diseases diagnosed by a physician?”25 A list of common conditions with response options “yes” or “no” after each condition followed this question. Incident doctor‐diagnosed depression was determined by affirmative responses on “depression” at follow‐up among employees who reported not having depression at baseline (cases of depression at baseline were excluded from the analysis).
Assessment of covariates
We included data on gender, age and occupational status (higher grade non‐manual, lower grade non‐manual, manual according to the Statistics Finland classification)26 as covariates. These data were obtained from employers' records.
Data analysis
Effort‐reward imbalance, procedural injustice and relational injustice were divided into quartiles and treated as categorical variables. The associations between these exposure variables were tested with χ2 test. We used logistic regression analysis to examine the associations of effort‐reward imbalance and the two components of injustice with incident poor self‐rated health, GHQ‐caseness, and doctor‐diagnosed depression, adjusting for age, gender and occupational status. Fully adjusted models additionally included effort‐reward imbalance, procedural and relational injustice as independent variables.
In a further step of analysis we combined the two measures of injustice into one single variable (mean of procedural injustice score and relational injustice score). This decision was based on the high correlation between the two scales and the internal consistency of a scale combining the two subscales (see below). We repeated the logistic regression analyses with this combined measure. In addition, we tested the effect of an interaction between effort‐reward imbalance and injustice on each health outcome by including the corresponding interaction term in regression models that already included the main effects. Finally, the two indicators, effort‐reward imbalance and organisational injustice, were used to construct three independent categories, based on median split in both scales: (1) low effort‐reward imbalance‐low injustice, (2) high effort‐reward imbalance‐low injustice or low effort‐reward imbalance‐high injustice, (3) high effort‐reward imbalance‐high injustice. Corresponding age‐, gender‐, and occupational status‐adjusted odds ratios of incident poor self‐rated health, incident GHQ‐caseness, and incident doctor‐diagnosed depression were calculated. All analyses were done with the SAS 9.12 statistical software.
Results
Sample characteristics
Sample characteristics of the two cohorts are shown in table 1. Comparison of baseline health between participants and all baseline respondents suggests that health‐related selection during the follow‐up was small in both cohorts. Prevalence of poor self‐rated health at baseline was 27% among the participants and 29% among all of the baseline respondents in the 10‐Town study and 17% and 18% in the Hospital Personnel study. The prevalence estimates for GHQ‐caseness at baseline were 26% versus 27% in the 10‐Town study and 22% versus 22% in the Hospital Personnel study and the corresponding figures for diagnosed depression were 12% versus 13% in the 10‐Town study and 8% versus 10% in the Hospital Personnel study.
Table 1 Demographic characteristics at baseline in two epidemiological cohorts.
| Characteristic | 10‐Town study | Hospital Personnel study | ||
|---|---|---|---|---|
| n | %* | n | %* | |
| Baseline | ||||
| Mean age (range) | 18066 | 44.9 (19–62) | 4833 | 44.3 (20–60) |
| Sex | ||||
| Men | 3946 | 22 | 520 | 11 |
| Women | 14120 | 78 | 4313 | 89 |
| Occupational status | ||||
| Higher‐grade non‐manual | 6220 | 34 | 824 | 17 |
| Lower‐grade non‐manual | 8779 | 49 | 3419 | 71 |
| Manual | 3067 | 17 | 590 | 12 |
| Effort‐reward imbalance, mean (SD) | 18066 | 1.58 (0.54) | 4833 | 1.46 (0.46) |
| Procedural injustice, mean (SD) | 18066 | 3.65 (0.92) | 4833 | 3.61 (0.94) |
| Relational injustice, mean (SD) | 18066 | 3.16 (0.86) | 4833 | 2.75 (0.77) |
| Pre‐existing poor self‐rated health | ||||
| No | 13039 | 73 | 3981 | 83 |
| Yes | 4796 | 27 | 835 | 17 |
| Pre‐existing GHQ cases | ||||
| No | 13375 | 74 | 3781 | 78 |
| Yes | 4623 | 26 | 1040 | 22 |
| History of doctor‐diagnosed depression | ||||
| No | 14779 | 88 | 4232 | 92 |
| Yes | 2071 | 12 | 388 | 8 |
| Follow‐up† | ||||
| Incident poor self‐rated health | ||||
| No | 10552 | 82 | 3327 | 84 |
| Yes | 2342 | 18 | 625 | 16 |
| Incident GHQ caseness | ||||
| No | 10861 | 82 | 3127 | 83 |
| Yes | 2457 | 18 | 636 | 17 |
| Incident cases of doctor‐diagnosed depression | ||||
| No | 12929 | 94 | 3937 | 96 |
| Yes | 896 | 6 | 153 | 4 |
*Unless otherwise stated.
†In each indicator of morbidity, we excluded participants with morbidity at baseline.
Associations between effort‐reward imbalance and components of injustice
There was a moderate association of effort‐reward imbalance with procedural and relational injustice in both cohorts. In the 10‐Town study, 34% of employees in the top quartile of effort‐reward imbalance but only 14% of those in the bottom quartile of effort‐reward imbalance belonged to the bottom quartile in procedural injustice (χ2(9) = 1147.3, p<0.001). This association was almost identical in the Hospital Personnel study (χ2(9) = 299.5, p<0.001) and very similar associations were also seen for effort‐reward imbalance and relational injustice in both cohorts (χ2(9) = 1099, p<0.001 in the 10‐Town study; χ2(9) = 384.8, p<0.001 in the Hospital study).
There was a stronger association between procedural and relational injustice as 50% of those in the top quartile of procedural injustice also belonged to the top quartile of relational injustice (χ2(9) = 4277.8, p<0.001 in the 10‐Town study and χ2(9) = 537.6 in the Hospital study, p<0.001). Moreover, combining the two scales of injustice into one formed an internally consistent scale with equally high Cronbach alpha (α = 0.92 in the 10‐Town cohort, α = 0.90 in the Hospital Personnel cohort) as those for the original procedural and relational injustice scales (α between 0.89 and 0.92). For these reasons, the following results are shown for the separate and combined measures of the two scales of organisational justice.
Effects on health
Tables 2 and 3 report the associations of effort‐reward imbalance and components of injustice with three health outcomes. Among healthy participants at baseline, effort‐reward imbalance was associated with increased risk of poor self‐rated health, GHQ‐caseness and doctor‐diagnosed depression at follow‐up; fully adjusted odds ratios for high versus low effort‐reward imbalance varied between 1.29 and 2.04 depending on the cohort and outcome (four of six odds ratios were statistically significant). In each fully‐adjusted model, either high procedural injustice or relational injustice was associated with increased risk (odds ratios between 1.30 and 2.13 for the stronger component of injustice, and between 1.01 and 1.27 for the weaker component). As this suggests redundancy between the two components of organisational injustice, we combined them into one measure, as indicated.
Table 2 Adjusted odds ratios for health impairment, as indicated by poor self‐rated health, GHQ‐caseness and doctor‐diagnosed depression at follow‐up, by levels of effort‐reward imbalance and organisational injustice among healthy employees at baseline in the 10‐Town study.
| Psychosocial factor | Odds ratio (95% CI) for incident poor self‐rated health | Odds ratio (95% CI) for incident GHQ‐caseness | Odds ratio (95% CI) for incident doctor‐diagnosed depression | |||
|---|---|---|---|---|---|---|
| Model 1* | Model 2† | Model 1* | Model 2† | Model 1* | Model 2† | |
| Effort‐reward imbalance (quartiles) | ||||||
| 1 (lowest) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 2 | 1.01 (0.88 to 1.16) | 1.00 (0.87 to 1.14) | 1.26 (1.10 to 1.44) | 1.24 (1.09 to 1.42) | 1.02 (0.83 to 1.27) | 1.01 (0.81 to 1.25) |
| 3 | 1.16 (1.02 to 1.31) | 1.11 (0.98 to 1.25) | 1.47 (1.30 to 1.66) | 1.40 (1.24 to 1.58) | 1.12 (0.92 to 1.35) | 1.06 (0.87 to 1.29) |
| 4 (highest) | 1.57 (1.38 to 1.78) | 1.43 (1.25 to 1.63) | 2.04 (1.80 to 2.32) | 1.83 (1.60 to 2.08) | 1.66 (1.38 to 2.01) | 1.48 (1.21 to 1.80) |
| Test for trend | p<0.001 | p<0.001 | p<0.001 | p<0.001 | p<0.001 | p<0.001 |
| Procedural injustice (quartiles) | ||||||
| 1 (lowest) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 2 | 1.08 (0.96 to 1.23) | 1.04 (0.91 to 1.19) | 1.25 (1.11 to 1.42) | 1.17 (1.03 to 1.33) | 1.17 (0.96 to 1.42) | 1.07 (0.87 to 1.31) |
| 3 | 1.31 (1.15 to 1.49) | 1.21 (1.05 to 1.39) | 1.35 (1.19 to 1.53) | 1.20 (1.04 to 1.37) | 1.26 (1.03 to 1.54) | 1.08 (0.87 to 1.34) |
| 4 (highest) | 1.51 (1.32 to 1.72) | 1.30 (1.12 to 1.51) | 1.81 (1.60 to 2.06) | 1.51 (1.31 to 1.73) | 1.56 (1.28 to 1.90) | 1.22 (0.97 to 1.52) |
| Test for trend | p<0.001 | p<0.001 | p<0.001 | p<0.001 | p<0.001 | p<0.001 |
| Relational injustice (quartiles) | ||||||
| 1 (lowest) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 2 | 1.04 (0.91 to 1.18) | 1.00 (0.88 to 1.14) | 1.11 (0.98 to 1.25) | 1.04 (0.92 to 1.18) | 0.99 (0.81 to 1.21) | 0.96 (0.78 to 1.18) |
| 3 | 1.15 (1.01 to 1.31) | 1.06 (0.92 to 1.21) | 1.30 (1.14 to 1.47) | 1.14 (1.00 to 1.30) | 1.26 (1.03 to 1.53) | 1.17 (0.95 to 1.44) |
| 4 (highest) | 1.38 (1.21 to 1.57) | 1.13 (0.98 to 1.30) | 1.50 (1.32 to 1.70) | 1.14 (0.99 to 1.31) | 1.57 (1.29 to 1.89) | 1.32 (1.07 to 1.63) |
| Test for trend | p<0.001 | p = 0.07 | p<0.001 | p = 0.03 | p<0.001 | p = 0.002 |
*Model 1 is adjusted for age, sex and occupational status.
†Model 2 includes age, sex, occupational status, effort‐reward imbalance and both components of organisational injustice as predictors.
Table 3 Adjusted odds ratios for health impairment, as indicated by poor self‐rated health, GHQ‐caseness and doctor diagnosed depression, by levels of effort‐reward imbalance and organisational injustice among healthy employees at baseline in the Hospital Personnel study.
| Psychosocial factor | Odds ratio (95% CI) for incident poor self‐rated health | Odds ratio (95% CI) for incident GHQ‐caseness | Odds ratio (95% CI) for incident doctor‐diagnosed depression | |||
|---|---|---|---|---|---|---|
| Model 1* | Model 2† | Model 1* | Model 2† | Model 1* | Model 2† | |
| Effort‐reward imbalance (quartiles) | ||||||
| 1 (lowest) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 2 | 1.23 (10.97 to 1.56) | 1.18 (0.93 to 1.50) | 1.30 (1.02 to 1.65) | 1.23 (0.97 to 1.56) | 1.65 (1.00 to 2.73) | 1.53 (0.93 to 2.54) |
| 3 | 0.92 (0.70 to 1.21) | 0.89 (0.67 to 1.18) | 1.36 (1.04 to 1.77) | 1.26 (0.96 to 1.64) | 1.58 (0.92 to 2.73) | 1.43 (0.82 to 2.47) |
| 4 (highest) | 1.38 (1.08 to 1.78) | 1.29 (0.99 to 1.68) | 1.59 (1.24 to 2.05) | 1.38 (1.06 to 1.80) | 1.93 (1.16 to 3.20) | 1.58 (0.93 to 2.68) |
| Test for trend | p = 0.07 | p = 0.28 | p<0.001 | p<0.001 | p = 0.02 | p = 0.17 |
| Procedural injustice (quartiles) | ||||||
| 1 (lowest) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 2 | 1.58 (1.24 to 2.01) | 1.51 (1.18 to 1.94) | 1.25 (0.97 to 1.61) | 1.17 (0.90 to 1.52) | 1.29 (0.78 to 2.12) | 1.08 (0.65 to 1.80) |
| 3 | 1.19 (0.93 to 1.54) | 1.13 (0.87 to 1.47) | 1.84 (1.44 to 2.34) | 1.67 (1.30 to 2.14) | 1.78 (1.12 to 1.54) | 1.38 (0.85 to 2.24) |
| 4 (highest) | 1.45 (1.13 to 1.87) | 1.31 (1.00 to 1.72) | 1.67 (1.29 to 2.15) | 1.48 (1.13 to 1.94) | 1.46 (0.98 to 2.40) | 1.06 (0.62 to 1.81) |
| Test for trend | p = 0.04 | p = 0.19 | p<0.001 | p<0.001 | p = 0.06 | p = 0.65 |
| Relational injustice (quartiles) | ||||||
| 1 (lowest) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 2 | 0.81 (0.63 to 1.05) | 0.78 (0.61 to 1.01) | 1.41 (1.10 to 1.80) | 1.32 (1.03 to 1.70) | 1.50 (0.87 to 2.59) | 1.40 (0.81 to 2.43) |
| 3 | 1.12 (0.87 to 1.44) | 1.03 (0.80 to 1.33) | 1.60 (1.24 to 2.07) | 1.42 (1.09 to 1.84) | 1.96 (1.14 to 3.36) | 1.77 (1.02 to 3.07) |
| 4 (highest) | 1.14 (0.90 to 1.45) | 1.01 (0.78 to 1.31) | 1.56 (1.21 to 2.02) | 1.27 (0.97 to 1.66) | 2.45 (1.47 to 4.09) | 2.13 (1.24 to 3.64) |
| Test for trend | p = 0.06 | p = 0.27 | p<0.001 | p<0.001 | p<0.001 | p = 0.002 |
*Model 1 is adjusted for age, sex and occupational status.
†Model 2 includes age, sex, occupational status, effort‐reward imbalance and both components of organisational injustice as predictors.
After adjustment for all baseline characteristics, high effort‐reward imbalance and high injustice were independently associated with an increased health risk for all three outcomes (fully‐adjusted odds ratios in the two cohorts ranged between 1.20 and 1.87) (table 4). However, with one exception (p = 0.049, incident GHQ‐caseness in the Hospital Personnel study), no evidence was found for multiplicative interactions between effort‐reward imbalance and injustice on health outcomes (range of p for interaction between 0.07 and 0.80).
Table 4 Odds ratios for health impairment, as indicated by poor self‐rated health, GHQ‐caseness and doctor‐diagnosed depression, by levels of effort‐reward imbalance and combined organisational injustice among healthy employees at baseline*.
| Psychosocial factor | Incident poor self‐rated health | Incident GHQ‐caseness | Incident doctor‐diagnosed depression | |||
|---|---|---|---|---|---|---|
| 10‐Town study | Hospital Personnel study | 10‐Town study | Hospital Personnel study | 10‐Town study | Hospital Personnel study | |
| Effort‐reward imbalance (quartiles) | ||||||
| 1 (lowest) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 2 | 1.00 (0.87 to 1.14) | 1.20 (0.95 to 1.53) | 1.25 (1.09 to 1.42) | 1.23 (0.97 to 1.57) | 1.01 (0.81 to 1.25) | 1.54 (0.93 to 2.55) |
| 3 | 1.11 (0.98 to 1.26) | 0.89 (0.68 to 1.18) | 1.40 (1.4 to 1.59) | 1.26 (0.96 to 1.64) | 1.06 (0.87 to 1.28) | 1.43 (0.82 to 2.48) |
| 4 (highest) | 1.44 (1.27 to 1.65) | 1.30 (1.00 to 1.69) | 1.85 (1.63 to 2.11) | 1.38 (1.06 to 1.79) | 1.49 (1.22 to 1.81) | 1.52 (0.89 to 2.58) |
| Test for trend | p<0.001 | p = 0.25 | p<0.001 | p = 0.03 | p<0.001 | p = 0.24 |
| Organisational injustice (quartiles) | ||||||
| 1 (lowest) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 2 | 1.08 (0.95 to 1.23) | 1.03 (0.80 to 1.32) | 1.29 (1.13 to 1.46) | 1.30 (1.00 to 1.67) | 1.12 (0.92 to 1.38) | 0.96 (0.56 to 1.64) |
| 3 | 1.26 (1.10 to 1.43) | 1.14 (0.88 to 1.46) | 1.29 (1.14 to 1.47) | 1.62 (1.25 to 2.08) | 1.24 (1.01 to 1.52) | 1.46 (0.89 to 2.41) |
| 4 (highest) | 1.36 (1.18 to 1.55) | 1.20 (0.93 to 1.55) | 1.56 (1.37 to 1.79) | 1.64 (1.26 to 2.13) | 1.52 (1.24 to 1.86) | 1.87 (1.15 to 3.05) |
| Test for trend | p<0.001 | p = 0.08 | p<0.001 | p<0.001 | p<0.001 | p = 0.002 |
*Models include age, sex, occupational status, effort‐reward imbalance and organisational injustice as predictors.
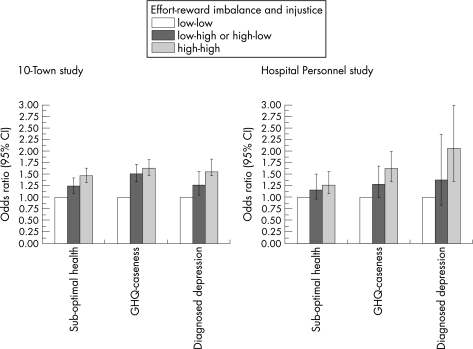
Results exploring the combined effect of the two measures (as defined by the three categorical variable described above) are illustrated in figure 1. As can be seen, the combination of high effort‐reward imbalance and high organisational injustice is associated with relatively higher risks of reduced health across all three health outcomes and in both cohorts.
Figure 1 Odds ratios for health impairment by combinations of effort‐reward imbalance and organisational injustice among healthy employees at baseline.
Discussion
The results of this report were based on data from two prospective epidemiological studies and indicate an independent association of effort‐reward imbalance and organisational injustice with three measures of incident impaired health. Moreover, combining these conditions resulted in a further increased risk of poor self‐rated health, GHQ‐caseness and diagnosed depression. Findings concerning the two subcomponents of organisational injustice—procedural and relational injustice—are somewhat less consistent, probably because of their high redundancy at the operational level.
To our knowledge, this is the first study to document independent risk prediction of three notions of work‐related injustice, exchange injustice (effort‐reward imbalance), procedural injustice and relational injustice (the latter two in combination). One recent study analysing associations of effort‐reward imbalance and relational (but not procedural) injustice with regard to sickness absence found evidence of their independent prediction (Head et al. Paper presented in the Conference of Work, Stress, and Health, Miami, Florida, USA, 2006) and in the same cohort relational justice also predicted incident coronary heart disease after adjusting for effort‐reward imbalance.11 In the current investigation, we included established measures of procedural and relational injustice and combined the findings from two large scale studies with regard to three different health measures, thus strengthening the robustness of results.
At the empirical level, it is of interest to note that odds ratios for effort‐reward imbalance and organisational justice were consistently attenuated after mutual adjustments in regression models. This observation points to some limited overlap between effort‐reward imbalance and organisational injustice. On the other hand, we found some indication that the combination of the two stressful conditions (effort‐reward imbalance and organisational injustice) results in the highest odd ratios for reduced health.
At the conceptual level, our findings lend support to the view that, in addition to the fundamental notion of contractual reciprocity (exchange justice) at work, procedural and/or relational justice within work organisations does matter for health and well‐being. Yet to what extent are these different facets of injustice independent of each other? It can be argued that the experience of esteem (one of the three components of reward) is closely linked to relational justice, both conceptually and operationally. However, in the effort‐reward imbalance model, esteem is weighted against efforts and does matter to the extent only that no equivalence of return is given, whereas relational injustice concerns non‐conditional ways of being treated without respect and with bias. A similar argument can be made with respect to low salary or poor promotion prospects as possible (yet unmeasured) experiences of procedural injustice. Similarities are more obvious between relational and procedural justice because violation of procedural rules is expected to result in relational unfairness. Conversely, recurrent relational injustice may indicate the supervisor's proneness towards violating procedural rules.
There are at least two conceptual differences between the effort‐reward imbalance and the organisational injustice models. First, the former is concerned with reciprocity of exchange within a formal contract—the employment contract. As such, it reflects the close links that exist between the constraints and opportunities of the work role and personal need satisfaction (for example, financial independence, self‐esteem, personal development, security). Organisational justice is more closely focused on managerial and interpersonal climate within formal organisations and the quality of interpersonal relationships in hierarchies. Second, the effort‐reward imbalance model distinguishes between three conditions of imbalance: dependency, strategic choice, and a specific motivational pattern (overcommitment). Thus, it considers additional social (for example, socioeconomic status of employees, employment conditions) and psychological (overcommitment) circumstances that are not directly addressed within the frame of organisational justice.
Future research
Future studies should take into account at least four limitations of this study. First, the original scales measuring the effort‐reward imbalance model were not available at the onset of the two investigations. Proxy measures of the scales “effort” and “reward” represent incomplete assessments of the construct. For example, our one‐item effort measure does not adequately tap both the intrinsic or extrinsic components of the effort concept. Moreover, the three questions measuring rewards (income and job benefits, recognition and prestige, and personal satisfaction) do not necessarily capture all the dimensions of the original scale which included 11 items measuring esteem, respect, job status, income and career opportunities. These scale modifications, together with the relatively low internal consistency of the effort measure (α<0.7) could lead to an underestimation of the associations.
Second, only one baseline measurement of the models was available. This may contribute to possible underestimation of the strength of effects as several recent reports documented stronger associations for consecutive than single‐time measures of work stress.27,28,29,30
Third, this study was based on prospective self‐reported data. It is well known that common‐method variance may artificially inflate associations in cross‐sectional data, for example through negative and positive response sets. Because we measured incidence (that is, change in health between the two surveys), an artificial inflation of associations would have occurred only if common‐method variance had affected the second survey but not the first survey. Although we believe that this is an unlikely alternative, future studies would benefit from inclusion of biomedical markers of disease susceptibility and objective indicators of morbidity to confirm the reported statistical associations.
Finally, the response rate was satisfactory (67%–83%) in all surveys, but dropouts were slightly more often men and, in the 10‐Town study, younger employees. We believe that a major selection bias is unlikely, as all odds ratios were adjusted for sex and age. Further analyses with substantially greater samples and more balanced composition of blue‐collar and male employees should address interaction terms between socioeconomic status and the types of injustice experienced at work in order to obtain information for occupational‐group‐specific intervention measures.
Main messages
Procedural injustice and relational injustice are closely related to each other, but less so to effort‐reward imbalance.
After combining procedural and relational injustice into a combined measure of organisational injustice, high effort‐reward imbalance and high injustice are both independently associated with health problems.
A combination of high effort‐reward imbalance and high organisational injustice is related to a greater health risk than high effort‐reward imbalance or organisational injustice alone.
Policy implications
Effort‐reward imbalance and organisational justice are complementary rather than redundant risk factors.
Conclusions
Evidence from two contemporary employee cohorts suggests that a combined index of procedural and relational injustice, in addition to effort‐reward imbalance (exchange justice), is related to increased health risk.
Abbreviations
GHQ - General Health Questionnaire
Footnotes
This study was supported by grants from the Academy of Finland (projects 105195 and 117604) and the Finnish Work Environment Fund. Data collection was supported by the participating cities and hospitals.
Competing interests: None declared.
References
- 1.Antoniou A S, Cooper CL Research companion to organizational health psychology. Cheltenham: Edward Elgar, 2005
- 2.Siegrist J. Adverse health effects of high‐effort/low‐reward conditions. J Occup Health Psychol 1996127–41. [DOI] [PubMed] [Google Scholar]
- 3.Siegrist J. Social reciprocity and health: new scientific evidence and policy implications. Psychoneuroendocrinology 2005301033–1038. [DOI] [PubMed] [Google Scholar]
- 4.Gouldner A W. The norm of reciprocity: a preliminary statement. Am Sociol Rev 196025161–178. [Google Scholar]
- 5.Adams J S. Inequity in social exchange. In: Berkowitz L, ed. Advances in experimental social psychology. New York: Academic Press, 1965267–299.
- 6.Leventhal G S. What should be done with equity theory? In: Gergen KJ, Greenberg MS, Willis RH, eds. Social exchanges: advances in theory and research New York: Plenum, 198027–55.
- 7.Moorman R H. Relationship between organizational justice and organizational citizenship behaviors: Do fairness perceptions influence employee citizenship? Journal of Applied Psychology 199176845–855. [Google Scholar]
- 8.Greenberg J, Cropanzano R. eds. Advances in organization justice: Stanford University Press 2001
- 9.Elovainio M, Kivimäki M, Vahtera J. Organizational justice: evidence of a new psychosocial predictor of health. Am J Public Health 200292105–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kivimäki M, Elovainio M, Vahtera J.et al Organisational justice and health of employees: prospective cohort study. Occup Environ Med 20036027–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kivimäki M, Ferrie J E, Brunner E.et al Justice at work and reduced risk of coronary heart disease among employees: the Whitehall II Study. Arch Intern Med 20051652245–2251. [DOI] [PubMed] [Google Scholar]
- 12.Elovainio M, Leino‐Arjas P, Vahtera J.et al Justice at work and cardiovascular mortality: a prospective cohort study. J Psychosom Res 200661271–274. [DOI] [PubMed] [Google Scholar]
- 13.Ferrie J E, Head J, Shipley M J.et al Injustice at work and incidence of psychiatric morbidity: the Whitehall II study. Occup Environ Med 200663443–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kawachi I. Injustice at work and health: causation or correlation? Occup Environ Med 200663578–579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vahtera J, Kivimäki M, Pentti J.et al Organisational downsizing, sickness absence, and mortality: 10‐town prospective cohort study. BMJ 2004328555–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kivimäki M, Virtanen M, Vartia M.et al Workplace bullying and the risk of cardiovascular disease and depression. Occup Environ Med 200360779–783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kouvonen A, Kivimäki M, Cox S J.et al Job strain, effort‐reward imbalance, and heavy drinking: a study in 40,851 employees. J Occup Environ Med 200547503–513. [DOI] [PubMed] [Google Scholar]
- 18.Siegrist J, Starke D, Chandola T.et al The measurement of effort‐reward imbalance at work: European comparisons. Soc Sci Med 2004581483–1499. [DOI] [PubMed] [Google Scholar]
- 19.Krause N M, Jay G M. What do global self‐rated health items measure? Med Care 199432930–942. [DOI] [PubMed] [Google Scholar]
- 20.Idler E L, Russell L B, Davis D. Survival, functional limitations, and self‐rated health in the NHANES I Epidemiologic Follow‐up Study, 1992. First National Health and Nutrition Examination Survey. Am J Epidemiol 2000152874–883. [DOI] [PubMed] [Google Scholar]
- 21.Kivimäki M, Head J, Ferrie J E.et al Sickness absence as a global measure of health: evidence from mortality in the Whitehall II prospective cohort study. BMJ 2003327364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Idler E L, Benyamini Y. Self‐rated health and mortality: a review of twenty‐seven community studies. J Health Soc Behav 19973821–37. [PubMed] [Google Scholar]
- 23.Bailis D S, Segall A, Chipperfield J G. Two views of self‐rated general health status. Soc Sci Med 200356203–217. [DOI] [PubMed] [Google Scholar]
- 24.Goldberg D, Williams P.A users guide to the general health questionnaire. Berkshire, UK: NFER‐Nelson Publishing Co, 1988
- 25.Haapanen N, Miilunpalo S, Pasanen M.et al Agreement between questionnaire data and medical records of chronic diseases in middle‐aged and elderly Finnish men and women. Am J Epidemiol 1997145762–769. [DOI] [PubMed] [Google Scholar]
- 26.Statistics Finland Classification of occupations. Helsinki: Statistics Finland, 1987
- 27.Kivimäki M, Ferrie J E, Head J.et al Organisational justice and change in justice as predictors of employee health: the Whitehall II study. J Epidemiol Community Health 200458931–937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chandola T, Siegrist J, Marmot M. Do changes in effort‐reward imbalance at work contribute to an explanation of the social gradient in angina? Occup Environ Med 200562223–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chandola T, Brunner E, Marmot M. Chronic stress at work and the metabolic syndrome: prospective study. BMJ 2006332521–525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kivimäki M, Head J, Ferrie J E.et al Why is evidence on job strain and coronary heart disease mixed? An illustration of measurement challenges in the Whitehall II study. Psychosom Med 200668398–401. [DOI] [PubMed] [Google Scholar]