Abstract
Background
Growth of the foreign-born population in the U.S. has led to increasing numbers of limited-English-proficient (LEP) patients. Innovative medical interpreting strategies, including remote simultaneous medical interpreting (RSMI), have arisen to address the language barrier. This study evaluates the impact of interpreting method on patient satisfaction.
Methods
1,276 English-, Spanish-, Mandarin-, and Cantonese-speaking patients attending the primary care clinic and emergency department of a large New York City municipal hospital were screened for enrollment in a randomized controlled trial. Language-discordant patients were randomized to RSMI or usual and customary (U&C) interpreting. Patients with language-concordant providers received usual care. Demographic and patient satisfaction questionnaires were administered to all participants.
Results
541 patients were language-concordant with their providers and not randomized; 371 were randomized to RSMI, 167 of whom were exposed to RSMI; and 364 were randomized to U&C, 198 of whom were exposed to U&C. Patients randomized to RSMI were more likely than those with U&C to think doctors treated them with respect (RSMI 71%, U&C 64%, p < 0.05), but they did not differ in other measures of physician communication/care. In a linear regression analysis, exposure to RSMI was significantly associated with an increase in overall satisfaction with physician communication/care (β 0.10, 95% CI 0.02–0.18, scale 0–1.0). Patients randomized to RSMI were more likely to think the interpreting method protected their privacy (RSMI 51%, U&C 38%, p < 0.05). Patients randomized to either arm of interpretation reported less comprehension and satisfaction than patients in language-concordant encounters.
Conclusions
While not a substitute for language-concordant providers, RSMI can improve patient satisfaction and privacy among LEP patients. Implementing RSMI should be considered an important component of a multipronged approach to addressing language barriers in health care.
KEY WORDS: immigrant health, satisfaction, language
BACKGROUND
Growth of the foreign-born population in the United States has led to increasing numbers of limited-English-proficient (LEP) patients. The LEP population (defined as speaking English less than very well) increased from 14 million in 1990 to 21.4 million in 2000.1 Language discordance between patients and their medical providers is a major factor impeding effective provision of health care.2–10
Communication barriers can adversely affect health services access, health outcomes, and patient satisfaction.2,3,11,12 LEP patients are less likely to have a usual source of medical care4 and have lower utilization of preventive services,5,6 higher usage of unnecessary diagnostic testing,7 and worse adherence with medical advice9 and follow-up care.8 Baker et al. showed that Latino patients in emergency care who were unable to get an interpreter were less satisfied with their providers.13 Dissatisfied patients are less likely to follow their medical regimens,11,14–16 whereas satisfaction appears to have a positive impact on clinical outcomes17–20 and continuity of care.21–24
No studies have sufficiently examined how patient satisfaction varies by interpreting method. Medical interpreting can be either consecutive or simultaneous. In consecutive interpreting, the interpreting occurs after the speaker has completed speaking,25 necessitating that the speakers pause for the interpreter. In simultaneous interpreting, the interpreter interprets at the same time as s/he is hearing the original speech.25 Interpreting can also be proximate or remote. Proximate interpreting involves an interpreter who is physically present at the encounter. In remote interpreting, the interpreter is outside the room of the encounter. Medical interpreting is usually proximate consecutive (PCMI) or over-the-telephone consecutive [remote consecutive medical interpreting (RCMI)]; less commonly utilized is the newer method of remote simultaneous (so-called United Nations-style) medical interpreting (RSMI).
RSMI has not yet been widely utilized, as it has only recently been made commercially available. Currently, the service is being provided to three hospitals and their satellite facilities in New York City. RSMI is similar to a voice-over; the interpretation is provided within milliseconds of the original speech. The trained medical interpreters are located remotely and communicate via wireless headsets with microphones worn by the provider and the patient. The wireless headsets and microphones offer mobility to the patient and provider but are not necessary. The same interpreting method can be accomplished using two regular phone lines. The current wait time to be connected is comparable to any commercially available telephone service (RCMI), as are the per-minute rates. Privacy is potentially increased because of the remote, audio-only, nature of the interpreting method.
Regardless of the interpreting method, use of professionally trained interpreters yields higher patient satisfaction than use of nonprofessionals.26–28 An earlier randomized controlled study of RSMI, involving families during a well-baby visit, showed high levels of satisfaction with this interpreting method.25 Patients were randomized to either RSMI or PCMI for the initial visit and then alternated experimental and control methods in four follow-up visits. An exploratory study that compared patient satisfaction across professional interpreting services found that, generally, patients were most satisfied when the interpreting method was perceived to decrease waiting time and delay.29 Patients indicated higher satisfaction with the increased sense of privacy conveyed by RSMI but dissatisfaction when technical glitches occurred.
As the health care system decides how to best spend its limited medical interpreting dollars, studies evaluating patient satisfaction, effectiveness, and costs of the various methods are needed. RSMI, by virtue of its simultaneous nature, has the promise to provide a more efficient form of interpreting, but there is a lack of adequate data with regard to patient satisfaction. This study, to our knowledge the first randomized controlled trial of RSMI in adult care, addresses this knowledge gap.
METHODS
This trial was conducted at the primary care clinic and the urgent care center of the emergency department (ED) at a large New York City municipal hospital. More than half of the hospital’s patients prefer to communicate in languages other than English. Spanish, Mandarin, and Cantonese are the most widely spoken languages. Approval for this study was obtained from both the New York University School of Medicine Institutional Review Board and the Hospital Center Research Protocol Group.
Participants
Primary care clinic patients were recruited between November 2003 and June 2005. Eligible patients were all English-, Spanish-, Mandarin-, and Cantonese-speaking adults (over 18 years old) who presented between the hours of 9 a.m. and 5 p.m. Patients were only eligible to enroll in the study if they were new patients being seen for the first time at the clinic. ED patients were recruited between October 2003 and December 2004. Eligible ED patients were all English and Spanish speaking adults who presented between 9 a.m. and 5 p.m. with symptoms of lower back pain, urinary-tract infection, sore throat, ear pain, or musculoskeletal pain. Patients with these conditions were more likely to be treated in urgent care (rather than critical care) and therefore more likely to be able to fully participate.
Eligible patients were identified by trained bilingual research assistants prior to their encounters with the provider. Bilingual research assistants determined Spanish or Chinese concordance by asking patients if they preferred an interpreter for their medical visit that day. This question was first asked in English, then in Mandarin, Cantonese, or Spanish, to ensure the patient understood the question. If a patient stated that he/she was comfortable speaking English, the patient encounter was categorized as language-concordant, and the patient was not randomized to an interpreting method. Non-English-speaking patients who were scheduled to see providers fluent in their primary language, determined by provider self-assessment, were also deemed language-concordant and not randomized. All study participants consented to voluntary, uncompensated participation.
Study Procedure and Measures
This study investigated patient satisfaction with RSMI, the experimental method, compared with usual and customary (U&C) interpreting methods. RSMI interpreters participate in a 60 hour simultaneous medical interpreting training conducted by the Center for Immigrant Health at New York University School of Medicine. U&C methods included PCMI and RCMI. PCMI methods included both trained interpreters (e.g., hospital interpreter services) and ad hoc interpreters (i.e., family, friends, untrained hospital staff, and volunteers). The RCMI method used by study participants was a commercial language line accessed via a landline telephone.
Language-discordant encounters were randomized to RSMI or U&C interpreting, using SPSS v.12 for Windows. We selected several variables to stratify the randomization according to expected variability and strong association with our outcomes of interest. Primary Care Clinic patients were stratified by primary language (Spanish, Mandarin, or Cantonese), health insurance coverage (yes or no), and English fluency. ED patients were stratified by English fluency and insurance coverage. English fluency was determined using the question “How well do you speak English?”,30 and responses were grouped into two categories “very well”/“well” and “not well”/“not at all”. Patients and providers were not aware of allocation, and research assistants were required to call the central study office to determine allocation each time a new patient was enrolled. Providers were informed of patient participation, and their consent was obtained. Research assistants gave the physician a set of RSMI headsets if the patient was randomized to RSMI. If a patient was randomized to U&C, the physician selected an interpreter, or decided not to use one, as he/she usually would. He/she called the hospital interpreter service, called the commercial over-the-telephone interpreting service, found an ad hoc interpreter, or proceeded with the encounter without an interpreter.
An 80-item demographic questionnaire was administered to all study patients prior to their encounters with the provider. After their medical encounters, participants were surveyed by a bilingual research assistant on their satisfaction with their provider, medical care, and interpreter and interpreting method (if used). Data were also collected on the actual method of interpretation received, and, if the interpreting method allocated by randomization was not used, the reasons why. All patient study interviews were conducted in the patients’ primary language by bilingual interviewers using study instruments in that language.
To assess satisfaction with physician communication/care, patients were asked (yes/no) if physicians listened to them carefully, if time spent with physicians was adequate, and if they would recommend their physician to a friend. They rated on a four-point scale how well they thought their physicians understood them, understanding of physician instructions and explanations, and overall quality of medical care. They rated on a five-point scale the level of respect from the physician and overall physician care. For satisfaction with interpretation, patients were queried on a four-point scale about how well the interpreter understood them, how well the interpreter interpreted, and how well patient privacy was protected by the interpreting method. They were asked via a five-point scale about the level of respect from the interpreter. Patients were also queried (yes/no) about whether the interpreter listened to them carefully, whether they would recommend the interpreter used during the visit to a friend, and if they would recommend the method of interpretation to a friend. Where questions involved responses along a scale, a four- or five-bar graph was presented to patients with bars of different heights for each response. This enabled patients to visualize the interval between response choices.
Statistical Analysis
Analyses were performed according to the interpreting method to which the patient was randomized (intent-to-treat analysis) and according to the interpreting method the patient actually received (analysis of actual interpreting method received). The Chi-square test was used to test for sociodemographic differences between (a) the randomized groups (RSMI and U&C) to establish the validity of the randomization process, (b) the two randomized arms and the language concordant group to determine whether there were other factors that differed across groups, and (c) the five groups in the analysis of actual interpreting method received (RSMI, U&C trained interpreters only, U&C untrained interpreters, English concordant, and non-English concordant).
As in other patient satisfaction studies,31 our results were generally skewed towards the higher end of a scale. We therefore grouped all responses other than the highest level together. The Chi-square test was used to test for statistical significance; the Fisher’s exact test was used when cell sizes were less than 5.
To create multi-item satisfaction scales to efficiently test the impact of interpreting method, a factor analysis was conducted using the 16 satisfaction items. The factor analyses were run on all 16 items together and separately on those items specific to physicians (nine items) and interpreters (seven items). Two prominent factors were identified, one specific to interaction with the physician and one to interpreter interactions. The composite score for satisfaction with physician communication/care combined five items (How well did you understand your doctor’s explanation of medical procedures and test results? How well did you understand your doctor’s instructions about follow-up care? How would you rate your doctor in treating you with respect? How would you rate your doctor overall? Overall how satisfied are you with the quality of your medical care today?), which had a Cronbach’s alpha coefficient of 0.7692.
Similarly, the composite interpreter score combined four items (How well do you think your interpreter understood you? How would you rate your interpreter in treating you with respect? How well did the interpreter interpret your visit with the doctor? How well do you think this method of interpretation protected your privacy during this visit?), which had a Cronbach’s alpha coefficient of 0.7394. Physician or interpreter composite scores were considered missing if two or more questions in the four- or five-item scale were missing. Composite scores were created as sums of individual item scores divided by the highest possible sum (range 0–1). A maximum of one item was permitted to be missing; score denominators were the sum of highest possible scores for all nonmissing items.
In the intent-to-treat analysis of satisfaction measures, RSMI was compared with U&C. In the analysis of actual interpreting method received, the three groups that were compared were RSMI, U&C (trained interpreters only), and language concordant. The U&C untrained group was excluded to avoid biasing the results towards RSMI, which was administered by trained interpreters only.
Linear regression analyses were performed on both composite satisfaction scores. If a given case was missing data for one of the covariates in the regression, it was dropped from the analysis. Regression analyses were performed using both the category of interpreting method to which the patient was randomized (intent-to-treat analysis) and as the category the patient actually received during the encounter (analysis of actual interpreting method received). The conventional p < 0.05 significance level was used.
RESULTS
Among 1,276 patients screened for enrollment in the randomized controlled trial, 541 were deemed by our protocol to be language-concordant with their provider and, hence, were not randomized to either interpreting method (Fig. 1). Among the 371 who were randomized to RSMI, 167 (45%) actually received RSMI; among the 364 patients randomized to U&C, 198 (54%) actually received U&C. Most of those who did not receive their randomized interpreting method were deemed language-concordant by the treating physician (either the patient spoke English or the physician spoke Spanish, Mandarin, or Cantonese), and consequently proceeded without an interpreter. Interpreter satisfaction data for these patients were not collected.
Figure 1.
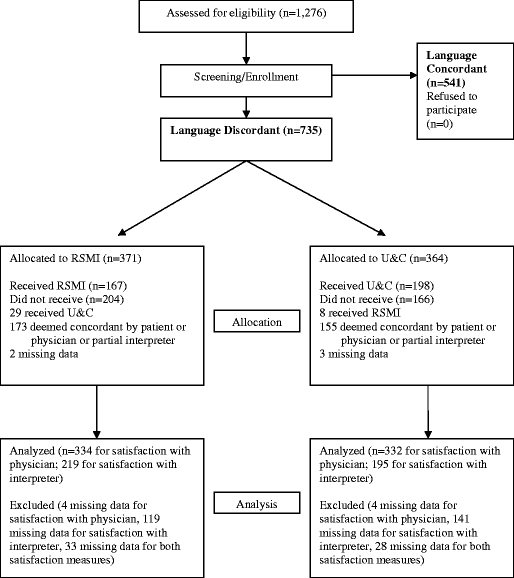
Flowchart: patient enrollment, randomization, and analysis
Randomized patients were mostly younger than age 65, had not completed high school, had resided in the U.S. for 10 years or less, spoke primarily Spanish or English, and had “good” to “fair” self-reported health status. There were no significant differences in sociodemographic characteristics between the randomized groups (Table 1). Sociodemographic characteristics of patients by actual interpreting method received [RSMI (n = 175), U&C trained interpreters (n = 165), U&C untrained (n = 185), English-concordant (n = 460), non-English-concordant (n = 291)] differed in that English-concordant patients were more highly educated (54% were college-educated vs. 26–39% in the other groups, p < 0.05) and more likely to report “excellent” or “good” health status (57% vs. 29–34% in the other groups, p < 0.05).
Table 1.
Sociodemographic Characteristics of Enrolled Patients—ED and Primary Care Clinic, Randomized and Language Concordant, n (%)
| Randomized Patients (n = 735) | Language-Concordant Patients (n = 541) | ||
|---|---|---|---|
| RSMI (n = 371) | U&C (n = 364) | ||
| Gender | |||
| Female | 208 (56) | 197 (54) | 244 (45)* |
| Male | 155 (42) | 162 (45) | 280 (52) |
| Age | |||
| 17–34 | 138 (37) | 124 (34) | 216 (40) |
| 35–64 | 198 (53) | 204 (56) | 287 (53) |
| 65+ | 16 (4) | 18 (5) | 15 (3) |
| Education | |||
| <8th | 73 (20) | 65 (18) | 45 (8)* |
| <HS | 110 (30) | 111 (30) | 73 (13) |
| HS Grad | 52 (14) | 55 (15) | 112 (21) |
| College | 113 (30) | 114 (31) | 271 (50) |
| Years in U.S. | |||
| <1 | 9 (2) | 13 (4) | 8 (1)* |
| 1–5 | 144 (39) | 113 (31) | 65 (12) |
| 6–10 | 68 (18) | 73 (20) | 69 (13) |
| 11+ | 128 (35) | 140 (38) | 143 (26) |
| U.S.-born | 4 (1) | 4 (1) | 125 (23) |
| Primary language | |||
| Spanish | 278 (75) | 260 (71) | 162 (30)* |
| Chinese | 70 (19) | 86 (24) | 41 (8) |
| English | 3 (1) | 2 (1) | 289 (53) |
| Fluency (speaks English...) | |||
| Very well | 0 (0) | 1 (0) | 139 (26)* |
| Well | 10 (3) | 16 (4) | 120 (22) |
| Not well | 176 (47) | 180 (49) | 75 (14) |
| Not at all | 155 (42) | 150 (41) | 26 (5) |
| Enrollment site | |||
| Clinic | 271 (73) | 279 (77) | 255 (47)* |
| ER | 100 (27) | 85 (23) | 286 (53) |
| Self-reported health status | |||
| Excellent | 16 (4) | 23 (6) | 77 (14)* |
| Good | 104 (28) | 100 (27) | 209 (39) |
| Fair | 156 (42) | 156 (43) | 150 (28) |
| Bad | 51 (14) | 36 (10) | 50 (9) |
| Very bad | 8 (2) | 17 (5) | 13 (2) |
Percentages may not add up to 100% because of missing values. No significant differences found between RSMI and U&C, at a level of p < 0.05.
*Significant differences at a level of p < 0.05 across all three categories.
Results by Intention to Treat
For satisfaction with physician communication/care, patients randomized to receive RSMI were more likely than those receiving U&C to rate their physicians “very well” in treating them with respect (71% RSMI vs. 64% U&C, p < 0.05) (Table 2). Patients also rated RSMI as better than U&C at protecting their privacy (RSMI 51% vs. U&C 38%, p < 0.05) (Table 3). The mean satisfaction with interpreter score was higher for patients in the RSMI group (RSMI 0.528 vs. U&C 0.462, p < 0.05) as well. There were no other significant differences between the groups.
Table 2.
Satisfaction with Physician Communication/Care, by Interpreting Method
| Intent-to-treat Analysis (by randomization mode) | Actual Interpreting Method Received | ||||
|---|---|---|---|---|---|
| U&C | RSMI | U&C Trained | RSMI | Language Concordant | |
| n | 364 | 371 | 165 | 175 | 751 |
| Did your doctor listen carefully? | |||||
| Yes | 324 (96) | 336 (98) | 145 (95) | 165 (99) | 697 (99)* |
| Did your doctor spend enough time with you? | |||||
| Yes | 316 (94) | 325 (96) | 145 (95) | 161 (98) | 656 (96) |
| How would you rate your doctor in treating you with respect? | |||||
| Very well | 213 (64) | 242 (71)† | 85 (57) | 115 (70)‡ | 527 (75)* |
| How well do you think your doctor understood you? | |||||
| Very well | 132 (39) | 150 (45) | 57 (37) | 79 (49)‡ | 454 (64)* |
| How well did you understand your doctor’s explanation of medical procedures and test results? | |||||
| Very well | 125 (38) | 128 (39) | 52 (35) | 62 (39) | 404 (59)* |
| How well did you understand your doctor’s instructions about follow-up care? | |||||
| Very well | 125 (38) | 134 (41) | 48 (33) | 60 (38) | 436 (63 )* |
| How would you rate your doctor overall? | |||||
| Very well | 178 (54) | 195 (59) | 72 (48) | 91 (56) | 436 (63)* |
| Would your recommend your doctor to a friend? | |||||
| Yes | 287 (95) | 287 (95) | 125 (94) | 140 (97) | 615 (96) |
| Overall, how satisfied were you with the quality of your medical care? | |||||
| Very well | 155 (47) | 169 (51) | 72 (48) | 93 (57) | 396 (57) |
| Composite satisfaction with physician communication/care score | |||||
| Mean(SD) | 0.478 (0.340) | 0.514 (0.355) | 0.436 (0.330) | 0.518 (0.351)‡ | 0.628 (0.350)* |
Denominators for percentages exclude missing values.
*Actual interpreting method received, significant differences between all three groups at a level of p < 0.05.
†Intent-to-treat analysis, significant difference between RSMI and U&C at a level of p < 0.05.
‡Actual interpreting method received, significant differences between RSMI and U&C trained.
Table 3.
Satisfaction with Interpretation, by Interpreting Method
| Intent-to-treat Analysis (by randomization mode) | Actual Interpreting Method Received | |||
|---|---|---|---|---|
| U&C | RSMI | U&C Trained | RSMI | |
| n | 364 | 371 | 165 | 175 |
| Did your interpreter listen to you carefully? | ||||
| Yes | 192 (99) | 214 (98) | 149 (99) | 158 (99) |
| How would you rate your interpreter in treating you with respect? | ||||
| Very well | 99 (51) | 129 (58) | 71 (48) | 88 (54) |
| How well do you think your interpreter understood you? | ||||
| Very well | 95 (48) | 111 (50) | 70 (45) | 73 (45) |
| How well do you think your interpreter interpreted your visit with the doctor? | ||||
| Very Well | 98 (50) | 124 (56) | 76 (50) | 90 (55) |
| How well do you think this method of interpretation protected your privacy? | ||||
| Very Well | 73 (38) | 104 (51)* | 52 (35) | 74 (49)† |
| Would you recommend the interpreter to a friend? | ||||
| Yes | 175 (97) | 200 (97) | 136 (96) | 147 (99) |
| Would you recommend this method of interpretation to a friend? | ||||
| Yes | 178 (93) | 204 (96) | 136 (94) | 151 (97) |
| Composite satisfaction with interpreter score | ||||
| Mean (SD) | 0.462 (0.368) | 0.528 (0.393)* | 0.449 (0.365) | 0.502 (0.395) |
Denominators for percentages exclude missing values and those for whom the response was not applicable (i.e., those who did not receive interpreter services).
*Intent-to-treat analysis, significant difference between RSMI and U&C at a level of p < 0.05.
†Actual interpreting method received, significant differences between RSMI and U&C trained at a level of p < 0.05.
Results by Actual Interpreting Method Received
In the analysis of satisfaction with physician communication/care by actual interpreting method received, patients in the RSMI group were more likely than those in the U&C trained interpreter group to rate their physicians “very well” in treating them with respect (70% RSMI vs. 57% U&C trained, p < 0.05) and to think their physicians understood them “very well” (45% RSMI vs. 35% U&C trained, p < 0.05) (Table 2). The mean composite satisfaction with physician communication/care score was also higher for patients in the RSMI group (RSMI 0.518 vs. U&C trained 0.436, p < 0.05). For most measures of satisfaction with physician communication/care, however, patients in the language-concordant group rated physicians more highly than patients in both the RSMI and U&C trained groups.
For interpreter satisfaction, patients felt RSMI protected their privacy better than U&C trained interpreters (49% RSMI vs. 35% U&C trained, p < 0.05). There were no significant differences between the groups among the other measures. (Table 3)
Tables 4 and 5 show composite physician communication/care and interpreter satisfaction scores regressed on the randomized method of interpretation, and on actual interpreting method received. The intent-to-treat analysis, which included patients who did not work with any interpreter, did not illustrate a significant association between RSMI and the composite physician communication/care satisfaction score (Table 4). Actual receipt of RSMI, however, was significantly associated with increased satisfaction with physician communication/care compared to receipt of U&C trained interpretation (Table 5). Controlling for other potential explanatory factors (such as a patient’s gender, primary language, self-reported health status, or enrollment site) did not significantly reduce this association (coefficient = 0.100, p = 0.010). The coefficient in this context means that an encounter utilizing RSMI should lead to a satisfaction score that is 10 points higher out of 100 than the average encounter utilizing PCMI or RCMI with trained interpreters. There were no significant differences between groups in satisfaction with interpreter scores in either the intent-to-treat analysis (Table 4) or in the analysis of actual interpreting method received (Table 5).
Table 4.
Linear Regression Analysis of Satisfaction with Physician Communication/Care and Satisfaction with Interpretation Scores, Intent-to-treat Analysis
| Satisfaction with Physician Communication/Care | Satisfaction with Interpreter | |||
|---|---|---|---|---|
| Score (m, SD) | β (95% CI)* | Score (m, SD) | β (95% CI)* | |
| U&C | 0.478 (0.340) | Referent | 0.462 (0.368) | Referent |
| RSMI | 0.514 (0.355) | 0.041 (−0.013, 0.094) | 0.528 (0.393) | 0.071 (−0.004, 0.145) |
*Adjusted for gender, primary language, self-reported health status, enrollment site
Table 5.
Linear Regression Analysis of Satisfaction with Physician Communication/Care and Satisfaction with Interpretation Scores, by Actual Interpreting Method Received
| Satisfaction with Physician Communication/Care | Satisfaction with Interpreter | |||
|---|---|---|---|---|
| Score (m, SD) | β (95% CI)* | Score (m, SD) | β (95% CI)* | |
| U&C Trained | 0.436 (0.330) | Referent | 0.449 (0.365) | Referent |
| RSMI | 0.518 (0.351) | 0.100 (.024, 0.176) | 0.502 (0.395) | 0.070 (−0.015, 0.155) |
| Language concordant | 0.628 (0.350) | 0.142 (0.076, 0.208) | N/A | N/A |
*Adjusted for gender, primary language, self-reported health status, enrollment site
CONCLUSIONS
With the large growth of the foreign-born population in the United States, the study of interpreting strategies outcomes for language-discordant encounters is of great importance. The introduction of RSMI, with its potential for more efficient interpreting because of its simultaneity, compelled studying its impact in relation to U&C interpreting.
In this randomized controlled trial of RSMI vs. U&C interpreting, there were a few areas in which patients in the RSMI group were more satisfied than in the U&C group. Patients felt they were treated with more respect by their physicians and that their privacy was better protected. The exposure analysis revealed similar outcomes. Exposure analysis results are relevant, as patients usually did not receive the randomized method because of language concordance with their physicians, not because of interpreting method preference.
Alarmingly, all groups reported poor satisfaction with important aspects of doctor–patient communication, in particular, feeling understood by the physician, understanding physicians’ explanations of procedures and results, and understanding instructions for follow-up care. However, this was much worse for patients in the interpreted medical encounter, indicating that current interpreting strategies still do not approximate a language-concordant encounter. Among language-concordant patients, dissatisfaction may have been due in part to physician “false fluency”, with physicians overestimating their language abilities; to patients’ overestimating their English-speaking ability; or to other shortcomings in doctor–patient communication. In a separate study, we found a significantly lower error rate with RSMI compared with U&C interpreting in Spanish–English language-discordant encounters.32 However, comprehension was still perceived to be poor in our study, suggesting that technical accuracy alone is not sufficient. More studies are needed encompassing other languages and settings to further assess accuracy, efficiency, and patient satisfaction with the different methods of interpretation.
Patient satisfaction in cross-cultural patient–physician interactions is likely related to a constellation of factors, including socioeconomics, culture, race and ethnicity, time, and the logistics and quality of the interpreting method. In previous studies, satisfaction has been shown to have a positive impact on clinical outcomes.17–20 The results of this study, therefore, have important implications.
RSMI may be particularly useful in clinical situations where sensitive topics are discussed and patient privacy is paramount. The mental health encounter, the discussion of sexual behavior, and the evaluation of sexually transmitted diseases, for example, require a high level of patient comfort with their providers and assurance of privacy.33,34 The absence of a third party from the actual exam room during an RSMI (or RCMI) encounter may remove one potential barrier to patients’ willingness to disclose sensitive information.
Our findings suggest that RSMI could be an important component of a multipronged approach to improving patient satisfaction in the interpreted encounter, but also that much more work needs to be done. Professional interpreters, physicians, and patients need more training and education on how best to facilitate the interpreted medical encounter. Further studies need to be conducted on interpreting modalities, and should examine errors, medical outcomes, and costs. Physician-related factors should also be assessed, including physician satisfaction and barriers to utilization. We also need qualitative data to learn more about what specifically detracts from patient satisfaction with interpreting so that appropriate interventions can be developed to address the dissatisfaction documented in this study. Future studies should include additional technology-based interpreting delivery systems, including video and computer-assisted linguistic access.
Acknowledgements
The work described was supported by The California Endowment and The Commonwealth Fund. It is registered at clinicaltrials.gov, ID#NCT00522327. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the awarding agencies. The authors wish to thank the dedicated efforts of Abraham Aragones, M.D.; Alexis Rourk; Yu-hui Ferng, M.P.A.; and Nicole Hewitt, M.P.A, on this study.
Conflict of Interest Two of the authors (FG, JC) have ownership in a company that provides technology solutions for remote simultaneous medical interpreting.
References
- 1.U.S. Census Bureau. Language Use and English-speaking Ability: 2000. Washington, DC: U.S. Census Bureau; 2003.
- 2.Flores G. The impact of medical interpreter services on the quality of health care: a systematic review. Med Care Res Rev. 2005;62:255–99. [DOI] [PubMed]
- 3.Ku L, Flores G. Pay now or pay later: providing interpreter services in health care. Health Aff. 2005;24:435–44. [DOI] [PubMed]
- 4.Kirkman-Liff B, Mondragon D. Language of interview: relevance for research of southwest Hispanics. Am J Public Health. 1991;81:1399–404. [DOI] [PMC free article] [PubMed]
- 5.Marks G, Solis J, Richardson JL, Collins LM, Birba L, Hisserich JC. Health behavior of elderly Hispanic women: does cultural assimilation make a difference? Am J Public Health. 1987;77:1315–9. [DOI] [PMC free article] [PubMed]
- 6.Woloshin S, Schwartz LM, Katz SJ, Welch HG. Is language a barrier to the use of preventive services? J Gen Intern Med. 1997;12:472–7. [DOI] [PMC free article] [PubMed]
- 7.Hampers LC, Cha S, Gutglass DJ, Binns HJ, Krug SE. Language barriers and resource utilization in a pediatric emergency department. Pediatrics. 1999;103:1253–6. [DOI] [PubMed]
- 8.Kline F, Acosta FX, Austin W, Johnson RG Jr. The misunderstood Spanish-speaking patient. Am J Psychiatry. 1980;137:1530–3. [DOI] [PubMed]
- 9.Manson A. Language concordance as a determinant of patient compliance and emergency room use in patients with asthma. Med Care. 1988;26:1119–28. [DOI] [PubMed]
- 10.Yeo S. Language barriers and access to care. Annu Rev Nurs Res. 2004;22:59–73. [PubMed]
- 11.Andrulis D, Goodman N, Pryor C. What a difference an interpreter can make: health care experiences of underinsured with limited English proficiency. The Access Project. Boston, 2002. 1–14. Available at: http://www.accessproject.org/downloads/c_LEPreportENG.pdf.
- 12.Flores G, Laws MB, Mayo SJ, et al. Errors in medical interpretation and their potential clinical consequences in pediatric encounters. Pediatrics. 2003;11:6–14. [DOI] [PubMed]
- 13.Baker DW, Hayes R, Fortier JP. Interpreter use and satisfaction with interpersonal aspects of care for Spanish-speaking patients. Med Care. 1998;26:1461–70. [DOI] [PubMed]
- 14.Carrasquillo O, Orav EJ, Brennan TA, Burstin HR. Impact of language barriers on patient satisfaction in an emergency department. J Gen Intern Med. 1999;14:82–7. [DOI] [PubMed]
- 15.Lochman JE. Factors related to patients’ satisfaction with their medical care. J Community Health. 1983;9:91–109. [DOI] [PubMed]
- 16.Linn MW, Linn BS, Stein SR. Satisfaction with ambulatory care and compliance in older patients. Med Care. 1982;20:606–14. [DOI] [PubMed]
- 17.Feuerstein M, Huang GD, Ortiz JM, Shaw WS, Miller VI, Wood PM. Integrated case management for work-related upper-extremity disorders: impact of patient satisfaction on health and work status. J Occup Environ Med. 2003;45:803–12. [DOI] [PubMed]
- 18.Guldvog B. Can patient satisfaction improve health among patients with angina pectoris? Int J Qual Health Care. 1999;11:233–40. [DOI] [PubMed]
- 19.Hall JA, Dornan MC. Meta-analysis of satisfaction with medical care: description of research domain and analysis of overall satisfaction levels. Soc Sci Med. 1988;27:637–44. [DOI] [PubMed]
- 20.Kaplan SH, Greenfield S, Ware JE Jr. Assessing the effects of physician–patient interactions on the outcomes of chronic disease. Med Care. 1989;27:S110–27. [DOI] [PubMed]
- 21.Marquis MS, Davies AR, Ware JE Jr. Patient satisfaction and change in medical care provider: a longitudinal study. Med Care. 1983;21:821–9. [DOI] [PubMed]
- 22.Patrick DL, Marin DP, Madden CW, Diehr P, Cheadle A, Skillman SM. Dissatisfaction and disenrollment in a subsidized managed care program. Med Care Res Rev. 1997;54:61–79. [DOI] [PubMed]
- 23.Ware JE Jr, Davies AR. Behavioral consequences of consumer dissatisfaction with medical care. Eval Program Plann. 1983;6:291–7. [DOI] [PubMed]
- 24.Robbins JA, Bertakis KD, Helms LJ, Azari R, Callahan EJ, Creten DA. The influence of physician practice behaviors on patient satisfaction. Fam Med. 1993;25:17–20. [PubMed]
- 25.Hornberger JC, Gibson CD Jr, Wood W, et al. Eliminating language barriers for non-English-speaking patients. Med Care. 1996;34:845–56. [DOI] [PubMed]
- 26.Garcia EA, Roy LC, Okada PJ, Perkins SD, Wiebe RA. A comparison of the influence of hospital-trained, ad hoc, and telephone interpreters on perceived satisfaction of limited English-proficient parents presenting to a pediatric emergency department. Pediatr Emerg Care. 2004;20:373–8. [DOI] [PubMed]
- 27.Kuo D, Fagan MJ. Satisfaction with methods of Spanish interpretation in an ambulatory care clinic. J Gen Intern Med. 1999;14:547–50. [DOI] [PMC free article] [PubMed]
- 28.Lee LJ, Batal HA, Maselli JH, Kutner JS. Effect of Spanish interpretation method on patient satisfaction in an urban walk-in clinic. J Gen Intern Med. 2002;17:641–5. [DOI] [PMC free article] [PubMed]
- 29.Saint-Louis L, Friedman E, Chiasson E, Quessa A, Novaes F. Testing New Technologies in Medical Interpreting. Cambridge, MA: Cambridge Health Alliance Study; 2003.
- 30.U.S. Census Bureau. 2000 Census Long Form Questionnaire. Washington, DC: U.S. Census Bureau; 2000. Available at: http://www.census.gov/dmd/www/pdf/d02p.pdf.
- 31.Fox JG, Storms DM. A different approach to sociodemographic predictors of satisfaction with health care. Soc Sci Med [A]. 1981;15:557–64. [DOI] [PubMed]
- 32.Gany F, Kapelusznik L, Prakash K, Gonzalez J, Orta L, Changrani J. The impact of medical interpretation method on time and errors. J Gen Intern Med. In press. [DOI] [PMC free article] [PubMed]
- 33.Mimiaga M, Goldhammer H, Belanoff C, Tetu A, Mayer K. Men who have sex with men: perceptions about sexual risk, HIV and sexually transmitted disease testing, and provider communication. Sex Transm Dis. 2007;34(2):113–9. [DOI] [PubMed]
- 34.Mellor D, Davison T, McCabe M, Kuruvilla G, Moore K, Ski C. Satisfaction with general practitioner treatment of depression among residents of aged care facilities. J Aging Health. 2006;18(3):435–57. [DOI] [PubMed]


