Abstract
In this investigation, 3 adults who met criteria for marijuana dependence were treated using an abbreviated version of acceptance and commitment therapy (ACT). The treatment was delivered in eight weekly 90-min individual sessions. The effects of the intervention were assessed using a nonconcurrent multiple baseline across participants design. Self-reported marijuana use, confirmed through oral swabs, reached zero levels for all participants at posttreatment. At a 3-month follow-up, 1 participant was still abstinent and the other 2 were using but at a lower average level of consumption compared to baseline. Depression, anxiety, withdrawal symptoms, and general levels of experiential avoidance generally improved. This preliminary test suggests that additional development and testing of ACT for marijuana use are warranted.
Keywords: acceptance and commitment therapy, treatment, marijuana, dependence
Regular marijuana use has a significant negative impact physically (e.g., Tapert, Aaron, Sedlar, & Brown, 2001; Tashkin et al., 1990), psychologically (e.g., Pope & Yurgelun-Todd, 2004; Solowij, Michie, & Foxe, 1995), and socially (e.g., Haas & Hendin, 1987; Lynskey, Coffey, Degenhardt, Carlin, & Patton, 2003; Rainone, Deren, Kleinman, & Wish, 1987). Despite this, marijuana continues to be the most commonly used illicit drug in the United States, with 16% of 18- to 25-year-olds reporting marijuana use in 2004 (Substance Abuse and Mental Health Services Administration, 2005). Rates are even higher among young adults, with 34% of high school seniors reporting use of marijuana at some time in 2004 and 4% reporting daily use (Johnston, O'Malley, Bachman, & Schulenberg, 2005).
Treatment seems to be necessary for many to quit using marijuana (McRae, Budney, & Brady, 2003), and the percentage of patients who seek treatment for marijuana dependence has increased from 9% in 1994 to 16% in 2004 (Substance Abuse and Mental Health Services Administration, 2006). Unfortunately, empirical support for treatment is limited, in that there were no published controlled studies prior to 1994 (Stephens, Babor, Kadden, Miller, & The Marijuana Treatment Project Research Group, 2002), and only a handful of controlled studies are available today (see McRae et al., 2003, for a review).
In controlled trials, a variety of interventions have been examined, drawing particularly from treatments that have been successfully used with other substances including alcohol (Chaney, O'Leary, & Marlatt, 1978; N. S. Miller, Gold, Pottash, & Carter, 1989) and cigarette smoking (Goldstein, Niaura, Follick, & Abrams, 1989). These include relapse prevention (Stephens, Roffman, & Curtin, 2000; Stephens, Roffman, & Simpson, 1994); W. R. Miller and Rollnick's (1991) motivational enhancement approach (Budney, Higgins, Radonovich, & Novy, 2000; Stephens et al., 2002); cognitive behavior therapy and coping skills training (Budney et al., 2000; Copeland, Swift, Roffman, & Stephens, 2001; Stephens et al., 2002); and voucher-based motivational incentives (Budney et al., 2000).
Abstinence rates immediately following treatment have generally been in the 50% to 70% range for treatments that last for 9 to 14 sessions (e.g., Stephens et al., 1994, 2000, 2002). Some studies have failed to report follow-up data (Stephens et al., 2002), but those that have report abstinence rates between 0% and 30% at 3-month follow-up (e.g., Budney et al., 2000; Stephens et al., 2000) and about half that or less at 9- to 12-month follow-up (e.g., Budney et al., 2000; Copeland et al., 2001; Stephens et al., 1994, 2000).
One possible area for potential development in the treatment of marijuana dependence deals with the manner in which cognitions regarding using (e.g., “I will not fit in socially unless I also use”) and urges to use marijuana are addressed. It is known that a number of private events, including negative thoughts, emotions, cravings, and bodily states, play an important role in substance use and relapse (Beck, Wright, Newman, & Liese, 1993; Childress, McClellan, Natale, & O'Brien 1986; Meyer, 1986; N. S. Miller & Gold, 1991; Newcomb, Chou, Bentler, & Huba, 1988; Sher & Trull, 1994). A number of methods used in substance abuse treatment approaches focus on attempts to reduce or eliminate these private events, because they are hypothesized to exert control over the actual behavior of engaging in substance use. For instance, avoidance of triggering situations and cognitive restructuring techniques are often employed in substance abuse treatment protocols in an attempt to reduce cravings and alter substance-related cognitions. Many relapse prevention treatments encourage avoidance of “triggering” or “slippery” situations to reduce or avoid the experience of craving (Stephens et al., 2000).
With respect to substance-related cognitions, typical strategies used by cognitive-behavioral therapists involve detecting, testing, and then challenging the factual basis of the cognitions so as to reduce erroneous thinking (Beck et al., 1993). Clients are encouraged to reduce “irrational thoughts” and “unmanageable feelings” through the use of cognitive restructuring techniques, which are designed to alter interpretations of substance-related cognitions and urges or cravings and to replace uncomfortable thoughts and feelings with positive alternatives (e.g., Stephens et al., 2002).
Other, more behavioral approaches have used the introduction of external rewards such as financial incentives or vouchers for desired items to enhance motivation and reinforce the desired outcome of reduction in substance use (e.g., Budney et al., 2000). Although such strategies can be highly effective in modifying behavior for short periods of time, many of these approaches do not address the role of private events directly. Other examples of strategies that are widely used to control substance use include postponing or altering legal sanctions or imprisonment contingent on sobriety and social pressure exerted by a peer group or counselor.
These kinds of approaches are common in many areas of clinical psychology, but there are a variety of newer behavior therapies that also focus on the role of private events in disordered behavior but do so in a different way (Hayes, 2004). Instead of trying to change the content of substance-use-related cognitions or focusing on altering substance-use-related internal states (i.e., urges, cravings, images), acceptance and commitment therapy (ACT; Hayes, Strosahl, & Wilson, 1999) establishes acceptance behavior, implements cognitive defusion, and then explicitly links behavior to individually determined client values. Acceptance procedures are designed to alter the avoidance functions of negative private events by teaching clients how to more fully experience emotions in the moment. For example, if not using marijuana is associated with a feeling of agitation, ACT would encourage the client to accept those feelings and notice more what they are like (where do they occur; do they come and go; what do they feel like) all while continuing not to use. The empirically demonstrated benefit of acceptance is that it decreases the aversive properties of negative private events and increases the client's willingness and ability to engage in difficult activities while experiencing them (Eifert & Heffner, 2003; Levitt, Brown, Orsillo, & Barlow, 2004). Thus, acceptance procedures involve exposure to aversive events and creation of a social context in which approaching previously difficult activities is reinforced by the therapist.
When the client can discriminate and experience thoughts (e.g., “I need a hit”) as merely verbal behavior and not a literal truth, the evocative effects of such thoughts should decrease and the functional relation between the thought and corresponding actions (e.g., preparing to or engaging in substance use) can be weakened. This process has been labeled cognitive defusion and involves systematically extinguishing (a) the behavioral excesses categorized as cognitive fusion and (b) the emotional reason giving that characterizes letting behavior be guided by private stimuli. In accord with ACT theory, cognitive defusion has been found to decrease the believability of one's thoughts (e.g., Masuda, Hayes, Sackett, & Twohig, 2004) and reduce the need to react to them while persisting with an aversive task (e.g., Gutiérrez, Luciano, Rodríguez, & Fink, 2004).
Finally, ACT links behavior change to values (i.e., self-identified reinforcing events). The use of values in ACT is intended to shift behavior from the repertoire-narrowing effects of controlling private events and cognitive fusion to the repertoire-expanding and constructional approach traditionally emphasized within behavior analysis (Goldiamond, 1974/2002). Said in another way, ACT is designed to shift behavior from aversive control (e.g., avoidance of negatively valenced emotions and thoughts) to appetitive control by focusing the client on overt behavior linked to personally identified reinforcers. Empirically, linking action to personal values has been shown to produce greater goal-directed effort and goal attainment (Sheldon & Elliot, 1999).
There is a growing body of research illustrating the benefits of ACT for other substance abuse disorders including polysubstance-abusing opiate addicts (Hayes, Wilson, et al., 2004) and nicotine-dependent smokers (Gifford et al., 2004). The present study was designed to obtain preliminary data on the effectiveness of a brief ACT intervention for adults with marijuana dependence using a nonconcurrent multiple baseline across participants design.
Method
Participants
Participants were recruited through postings on the local university campus and announcements in undergraduate psychology classes. Five individuals responded and scheduled pretreatment sessions. One individual was seen for three sessions by the second author and dropped out due to time constraints imposed by volunteer commitments. Another individual was seen for one session by the first author and dropped out because of a job promotion. Results are reported for the 3 individuals with substantial data.
The first and second authors conducted all clinical interviews. Both investigators had received their master's degrees in psychology and had completed a minimum of 3 years of training in an APA-accredited clinical psychology program. In addition, the second author is a licensed drug and alcohol counselor. Both researchers were under the supervision of the third author, a professor of clinical psychology and licensed psychologist. Based on an unstructured clinical interview, all individuals met criteria for marijuana dependence (as defined in the Diagnostic and Statistical Manual of Mental Disorders, 2000) and reported that they were not receiving any psychiatric medications or psychological services elsewhere. All participants reported that they had never received formal treatment for marijuana use. Participant 1 reported that she had attempted to stop using on her own but was never successful. The other participants had not attempted to quit on their own. They also reported that they were not using other illicit drugs at the present time, although all reported having used them previously. No formal assessment of co-occurring psychological conditions was conducted, but participants reported having received other diagnoses (see Table 1).
Table 1.
Participant Characteristics
| P1 | P2 | P3 | |
| Gender | F | M | M |
| Marital status | M | S | S |
| Age | 43 | 19 | 20 |
| Years of education | 15 | 13 | 15 |
| Ethnicity | C | H | C |
| Years using marijuana | 26 | 5 | 3 |
| Years marijuana has been a problem | 6 | 2 | 1.5 |
| Previous diagnoses | MDD | none | none |
| Panic disorder |
Note. Years of education begin with first grade (e.g., 12 = high school education, 16 = 4 years of college); C = Caucasian, H = Hispanic; MDD = major depressive disorder.
Measures
A variety of measures were used in this investigation. The main dependent variable was self-monitoring of marijuana intake. Results from this measure were confirmed through objective oral swab tests. In addition, a variety of commonly used psychological measures were used to further explore the effects of treatment.
Intake Self-monitoring
Based on the procedures of Twohig, Hayes, and Masuda (2006), participants were given index cards and asked to place a mark on the card each time they used marijuana. Because the participants used varying amounts of marijuana, they were instructed to use the metric that most closely fit with the amount they used: either bowls smoked per day (Participant 1) or inhalations per day (Participants 2 and 3). This metric, although not exact, was applied consistently across time so as to allow the detection of changes in the most applicable measurement unit for each participant as a function of the introduction of the independent variable (ACT). At the end of each day, the participants reported the intake amounts to the experimenter either via a telephone message machine or electronic mail, ensuring roughly contemporaneous self-monitoring. These data served as the primary dependent variable, and treatment decisions were based on these data.
Oral Swab Test
Marijuana use was monitored periodically using the Intercept Oral Fluid Drug Test. The oral swab test is a noninvasive procedure that involves having the participant place a salted collection pad between the lower cheek and gum for 2 to 5 min. Samples were sent via overnight mail to Bendinger and Schlesinger Laboratories, and results were received via electronic mail within 24 hr. This test can detect marijuana use up to 3 days prior to testing, and only the presence or absence of marijuana metabolites (a dichotomous rather than a continuous measure) was reported by the laboratory. This test was performed at three points in the study: pretreatment, posttreatment, and at 3-month follow-up.
Marijuana Withdrawal Checklist (mwc)
The MWC (Budney, Novey, & Hughes, 1999) is a 31-item questionnaire that assesses reported cannabis-withdrawal symptoms such as decreased appetite, stuffy nose, or depressed mood. Participants rate each item on a scale on which 0 = none, 1 = mild, 2 = moderate, and 3 = severe, based on their experiences over the last 24 hr. Higher scores on this measure reflect greater withdrawal experiences. No clinical norms are available for this measure.
Beck Anxiety Inventory (bai)
The BAI (Beck, Epstein, Brown, & Steer, 1988) is a 21-question self-report measure that assesses anxiety. Each question is rated on a scale from 0 to 3. Scores in the 0 to 7 range are considered minimal, 8 to 15 are considered mild, 16 to 25 are considered moderate, and 26 to 63 are considered severe. The BAI has high internal consistency (Cronbach's alpha < .90), adequate test-retest reliability (rs > .60), and moderate to high convergent and discriminant validity.
Beck Depression Inventory-ii (bdi-ii)
The BDI-II (Beck, 1996) is a 21-item self-report measure that assesses the severity of depression. Each question is rated on a scale from 0 to 3. Scores in the 0 to13 range are considered minimal, 14 to 19 are considered mild, 20 to 28 are considered moderate, and 29 to 63 are considered severe. The BDI-II has shown good test-retest reliability (r = .93), and has demonstrated a high correlation with the original BDI (r = .93; Beck, 1996).
Acceptance and Action Questionnaire (aaq)
The AAQ (Hayes, Strosahl, et al., 2004) is a nine-item questionnaire; the questions are rated on a seven-point Likert-type scale. Lower scores reflect greater experiential willingness and ability to act in the presence of difficult thoughts and feelings. The means for the AAQ are 36.4 for clinical samples and 33.3 for nonclinical samples. The AAQ has been found to be internally consistent and has good convergent and discriminant validity (Hayes, Strosahl, et al., 2004).
Procedure
Interested participants contacted one of the investigators and were scheduled for an intake session. During this session the participant completed a university-approved consent form and the assessment materials listed above, and was shown how to self-monitor his or her marijuana intake. He or she also completed an oral swab test. The consent form indicated that the participant would receive up to five random oral swab tests throughout the study. He or she was not specifically informed that the tests would occur at pre-, post-, and follow-up assessments. Treatment consisted of eight weekly 90-min sessions of ACT (Hayes et al., 1999). The specific protocol was tailored for marijuana use and abbreviated for use in this study. The first author served as the therapist for all 3 participants. All sessions were videotaped, and 25% (one randomly selected tape of each session) were scored for treatment integrity by the second author. The third author, a developer of the treatment, trained the first and second authors.
The intervention was evaluated using a nonconcurrent multiple baseline across participants design. All participants were told that they would need to monitor their usage patterns during baseline for an unspecified amount of time. Participant 1 started treatment after 1 week of monitoring. The other participants began treatment after the previous participant showed decreases in reported marijuana use during the treatment phase. This resulted in lengthy baseline phases for Participants 2 and 3.
Acceptance and Commitment Therapy for Marijuana Dependence
Space limitations do not allow description of the treatment in sufficient detail for replication. Therefore, a brief description of what occurred in the treatment will be provided and the entire manual will be available from the authors or at contextualpsychology.org. The treatment will be described under labels that correspond with the treatment integrity rating system used in this investigation.
All sessions followed the same pattern: Events since the last session and homework were reviewed, the material from the previous session was reviewed, new material was presented, new homework was assigned, and behavioral exercises were agreed on.
General Assessment of Participant Functioning
The first session began with collection of pertinent information about the participant's pattern of substance use. Information on the participant's weekly substance use was also collected at the beginning of each therapy session thereafter.
Values
ACT formally began by identifying personally relevant appetitive and aversive events that were relevant to particular behaviors and were likely to affect the occurrence of target behaviors. This usually occurred through discussion of areas of life that were important and how using marijuana has been interfering with the pursuit of activities relevant to those areas.
Values assessment was accomplished through completion of the Valued Living Questionnaire (Hayes et al., 1999, p. 224). The questionnaire assessed a variety of areas that could potentially be important, including family, occupation, and recreation. After the participant was able to state what was important to him or her in these different domains, he or she was asked to rate how important each domain was and then how much he or she was working toward each of these areas. Next, the participant was asked to indicate the degree to which marijuana use interfered with these areas. For example, Participant 1 stated that smoking was inconsistent with her wanting to be a good mother because it was a bad example for her son. Participant 2's major concern was that smoking was severely getting in the way of his ability to do well in college as a first generation college student. Participant 3 stated that using marijuana was interfering with school and was inconsistent with his goal of being a useful member of society. Discussion of topics such as these also helped to motivate the participants to participate in treatment, an area that is notably difficult in the treatment of marijuana abuse. Although only the first two sessions were dedicated to this topic, discussions on how using marijuana interfered in many ways and how not using has positive outcomes were integrated into the following six sessions as necessary.
Creative Hopelessness/workability
The third and fourth sessions focused on what the participant has done to control thoughts and feelings that are evaluated as negative (e.g., urges to smoke and worries about not fitting in). Smoking marijuana seemed to decrease certain private events that the participant reported as being establishing operations for using. These particular targets were partially determined by asking “What does smoking do for you?” or “What comes up in the area of thoughts and feelings when you try and not smoke?” Answers included “I have great feelings of discomfort and tension,” or “I feel out of place with my friends.” To help the participant to evaluate the effectiveness of his or her attempts to control these thoughts and feelings, he or she was asked what had been tried in the past to decrease these feelings and how effective these strategies were. Many examples were given in addition to using marijuana to control these thoughts and feelings. In general, all of these procedures were either ineffective or effective only in the short term for decreasing these particular thoughts and feelings. For example, when asked how well smoking worked to decrease the urge to use, the participant reported that it immediately decreased the urge but that the urge returned either that same day or the next day. The “person in the hole” metaphor (Hayes et al., 1999, p. 101) was used to demonstrate the ultimate ineffectiveness of attempts to control these types of thoughts and feelings. The metaphor described the participant falling in a hole (representing the urge to smoke) with only a shovel to get out (tool for decreasing this feeling). The metaphor went on to describe how the participant's attempts to dig out of the hole (representing attempts to reduce or control the urge to smoke) never got him or her out of the hole and actually made the hole larger (the paradox of how struggling with thoughts and feelings can make them larger and more difficult to handle).
Additional work was done to help the participant realize that it was a common occurrence that certain thoughts and feelings are very difficult to control. For example, the participant was asked not to think of something such as “chocolate cake” (Hayes et al., 1999, p. 124) or not to get nervous when hooked to a “polygraph” (Hayes et al., p. 123). These exercises showed the paradoxical effects of direct control attempts on private events. Each participant was asked if he or she felt that the struggle with these thoughts and feelings was easier or harder over time. Unanimously they agreed that their struggles with these thoughts and feelings were becoming harder with time.
Acceptance
Acceptance in ACT means not engaging in behaviors (public or private) to decrease unwanted private events. In the case of marijuana abusers, participants were taught how to “accept” their urges to use marijuana. Participants were also taught to “accept” other private events that lead to using such as “feeling out of place” when not using. Acceptance was often presented as a behavioral choice that clients could make when experiencing particular private events that were associated with marijuana use. Examples of overt behaviors that were consistent with acting in an accepting way included not using marijuana, not avoiding situations or people that make them want to use marijuana, and continuing to engage in activities that that are meaningful even if they create urges to use marijuana. For example, 1 participant commonly smoked marijuana while snowboarding and suggested that he avoid snowboarding because it would make him want to use. He was instructed to continue to engage in the activity because he enjoyed it, but to do so while not using and practicing accepting the urges to use when they showed. One can also behave in an “accepting” way covertly. This involves not distracting oneself or doing any private actions to decrease a feeling.
Defusion
Defusion is the process of undermining the behavioral impact of verbal events, particularly private ones such as thoughts about the need to use marijuana. Examples of defusion exercises involve rapidly repeating a thought such as “can't stand it” until it no longer sounds like the thought but rather a funny string of sounds (Masuda et al., 2004). Another example involves treating the thoughts or urges as passengers on a bus on which the participant is the bus driver. This metaphor illustrates that the passengers rather than the driver have had control of the bus (the participant responding to his or her thoughts and urges), and offers a choice to shift control of the bus back to the driver by not acknowledging the “demands” of the passengers. The participant is told that the passengers will probably get upset (these feelings might become more intense), but that the driver (participant) will eventually gain control of the bus by staying on course (following one's values; Hayes et al., 1999, p. 157).
Committed Action
There were two types of behavioral commitment exercises used in this study: commitments to engage in meaningful activities and commitments not to use marijuana for specified periods of time. Although these exercises were topographically different for each participant, their function was the same: to help the participants engage in meaningful activities while practicing the material from sessions (e.g., defusion and acceptance). Examples of commitments to increase pleasurable activities included walking her dog every day and joining and attending a weekly yoga class for Participant 1, doing specified amounts of homework and calling his parents on the telephone for Participant 2, and setting up a basketball game with his friends and joining certain campus groups for Participant 3. All behavioral commitments not to use marijuana were for specified periods of time without regard to urges to use or other events not under the participant's control. No comments or suggestions were made that following these commitments would result in decreases in the urge to use or ease in stopping using; instead they were presented as opportunities to practice other ACT techniques (e.g., acceptance, defusion, values) while engaging in meaningful activities.
The final two sessions, Sessions 7 and 8, involved reviewing the material from the previous sessions, creating bolder and broader commitments, and troubleshooting possible problems that the participant might encounter after leaving therapy. Each therapy session was tailored to fit the individual participant.
Finally, each participant was asked to discuss any concerns regarding termination. The participants expressed concerns regarding relapsing or difficult situations that they might encounter in the future such as events where peers will be using marijuana. These problems were addressed in a manner that is consistent with ACT.
One week after treatment was completed, the participants were asked to discontinue self-monitoring and return to the clinic for the posttreatment assessment, which involved completing the same measures as the pretreatment assessment. At 3 months posttreatment, participants were asked to self-monitor for 3 additional concurrent days and to complete the same assessments completed at the posttreatment assessment. Participant 3 was asked to monitor for a week at the 3-month posttreatment assessment because he reported that he was not using during the work week but had used on the weekends.
Treatment Integrity
All therapy sessions were videotaped, and three sessions were scored for each participant. Random selection led the rater to watch Sessions 1 through 3 for Participant 2, Sessions 4 through 6 for Participant 3, and Sessions 6 through 8 for Participant 1. Thus, at least one of each session (Sessions 1 through 8) were scored. The second author conducted the scoring. Session tapes were scored for the quantity and quality of the coverage of each component of ACT using a validated and reliable scoring system (Pierson, Bunting, Smith, Gifford, & Hayes, 2004) that has been previously used in ACT research (Twohig et al., 2006): 1 = the variable was never explicitly covered, 2 = the variable occurred at least once and not in an in-depth manner, 3 = the variable occurred several times and was covered at least once in a moderately in-depth manner, 4 = the variable occurred with relatively high frequency and was addressed in moderate depth, 5 = the variable occurred with high frequency and was covered in a very in-depth manner. ACT is a type of psychotherapy, and the therapist must be flexible about what is targeted during a therapy session. Therefore, many of the processes were targeted in each session although the major focus changed according to the protocol.
Every ACT component was covered to the highest extent during at least one session, indicating that at least one session targeted each of these processes. Means are provided for each of the psychological processes because all sessions covered more than one process, even though each session had a particular focus. Means for each component over the eight sessions are as follows: creative hopelessness/workability = 2.6 (SD = 1.3), willingness/acceptance = 2.6 (SD = 1.4), defusion = 3.3 (SD = 1.8), values = 4.1 (SD = 1.0), committed action = 3.8 (SD = 1.1), and general assessment of participant's functioning = 3.4 (SD = 0.7). The therapist's overall adherence to the manual and overall competence were rated very highly, Ms = 4.6 (SD = 0.5) and 4.8 (SD = 0.4), respectively. In addition, the sessions were scored for therapeutic practices that were inconsistent with ACT, including challenging cognitive content, promoting change strategies that involved avoidance of experience, indicating that thoughts or feelings cause overt behavior, and use of cognitive therapy rationales. All measures inconsistent with ACT received scores of 1, indicating that they were not observed.
Results
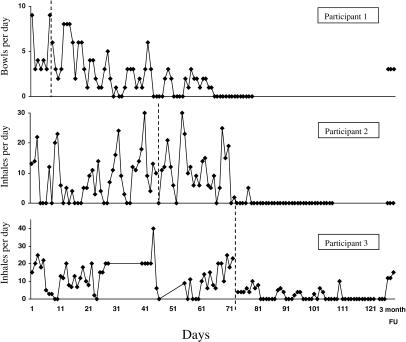
Self-monitoring data on the primary measure are presented in Figure 1, and self-report data for all measures are presented in Table 2 for all participants.
Figure 1.
Daily frequency of self-reported marijuana use for the 3 participants at baseline, treatment, and follow-up phases.
Table 2.
Month Follow-Up
| P1 |
P2 |
P3 |
M |
|||||||||
| Pre | Post | FU | Pre | Post | FU | Pre | Post | FU | Pre | Post | FU | |
| Oral swab | pos | neg | pos | pos | neg | neg | pos | neg | pos | |||
| Mean intake | 5 | 0 | 3 | 6.7 | 0 | 0 | 12.3 | 0 | 6.5 | 8.5 | 0 | 3.2 |
| BAI | 12 | 3 | 1 | 3 | 1 | 1 | 8 | 11 | 9 | 7.7 | 5 | 3.7 |
| BDI-II | 13 | 3 | 0 | 4 | 6 | 1 | 16 | 6 | 15 | 11 | 5 | 5.3 |
| MWC | 20 | 9 | 2 | 15 | 7 | 1 | 16 | 20 | 23 | 17 | 12 | 8.7 |
| AAQ | 15 | 19 | 17 | 29 | 15 | 14 | 40 | 34 | 31 | 28 | 22.7 | 20.7 |
Note. AAQ = Acceptance and Action Questionnaire, BAI = Beck Anxiety Inventory, BDI-II = Beck Depression Inventory-II, MWC = Marijuana Withdrawal Checklist, Mean intake = bowls per day for P1 and inhalations per day for P2 and P3, calculated on all of baseline and follow-up and the last week of treatment.
Because the participants used varying amounts of marijuana, two different metrics were used. Participant 1 recorded bowls smoked per day, and Participants 2 and 3 reported inhalations of marijuana per day. None of the participants showed decreases in self-reported marijuana use during a 1- to 10-week baseline, but all participants showed objectively confirmed large reductions in marijuana intake during treatment. This pattern of results provides controlled evidence that treatment reduced intake of marijuana. Data were collected throughout treatment, but in Table 2, posttreatment is considered data collected the week following the eighth and final treatment session. All participants reported (and oral swabs confirmed) abstinence at posttreatment. One was still abstinent at a 3-month follow-up, and the other 2 were still using, although at lower self-reported levels.
Participant 1
At baseline, Participant 1 reported smoking a mean of five (SD = 2.77) bowls of marijuana per day. Her oral swab test confirmed her usage. Her decrease throughout treatment was gradual. The participant and therapist gradually increased her commitments to engage in valued behaviors and to decrease her marijuana intake, and she was able to comply with her commitments not to use for the final 2 weeks of treatment. She reported using no marijuana at posttreatment, and her oral swab test confirmed this. According to her report, she ceased her use for the 2 months following posttreatment and then began using again at a social event (follow-up M = 3, SD = 0). Her follow-up oral swab test was positive for the presence of marijuana. The participant showed a decrease in her anxiety, depression, and withdrawal symptoms following treatment. The participant began with low scores on the AAQ at pretreatment that did not change throughout the study.
Participant 2
At baseline, Participant 2 reported a mean of eight inhalations per day (SD = 7.9), and his oral swab test confirmed his usage. He reported no longer using marijuana at posttreatment and 3-month follow-up, and these reports were confirmed with oral swab tests. Participant 2 had near floor-level scores on the BAI and BDI throughout the study. He had a moderate score on the AAQ at pretreatment and showed large reductions at posttreatment and follow-up. He also showed decreases in withdrawal symptoms following treatment.
Participant 3
Participant 3 reported a mean of 12 (SD = 8.6) inhalations per day during baseline. In addition to his marijuana usage, during Week 5 he reported using cocaine on one occasion and inhaling the prescription medication Adderall on two occasions. He stopped using on most weekdays but used more often on weekends. According to his report he was no longer using at posttreatment, which was confirmed by his oral swab test. At 3-month follow-up he reported that he was not using during the week but continued to use on the weekends. He reported that this amount of use was not hindering his ability to do well in school and at work and indicated that it was an active choice to use only on the weekends. His self-monitoring (follow-up M = 6.5, SD = 7.2) and his positive oral swab test supported this report. His scores on the BAI were within the mild anxiety range throughout the study. Participant 3's score on the BDI-II was in the mild range of depressive symptoms at pretreatment, in the minimal range at posttreatment, and back in the mild range at 3-month follow-up. He showed small increases in withdrawal symptoms from pre- to posttreatment and again at follow-up. He began with a high score on the AAQ and showed moderate decreases throughout assessments.
Discussion
The present study provides limited and preliminary but controlled evidence that an ACT approach may be at least somewhat helpful in the treatment of marijuana dependence. Objectively confirmed self-reports of marijuana use showed that all participants were no longer using marijuana at posttreatment. At 3-month follow-up, 1 participant was still at posttreatment levels and the other 2 were using at somewhat reduced levels compared to baseline. Two other participants dropped out of treatment in the early stages. However, high attrition is a common problem in marijuana abuse treatment research (e.g., Budney et al., 2000).
Marijuana dependence is an enormous problem, and effective treatment procedures are needed (McRae et al., 2003). Treatment options include relapse prevention (Stephens et al., 1994, 2000), motivational enhancement procedures (Budney et al., 2000; Stephens et al., 2002), cognitive behavior therapy and coping skills training (Budney et al.; Copeland et al., 2001; Stephens et al., 2002), and voucher-based motivational incentives (Budney et al.). Unfortunately, all these approaches suffer from limited effectiveness in both the short and long term as well as other limitations including high attrition (McRae et al.). Even though the findings from this study were no more notable than previous attempts at treating marijuana use, they are important because the treatment takes a theoretically and procedurally different approach. Specifically, ACT does not attempt to reduce or control private events that are associated with substance use, but rather helps to create a verbal context in which urges to use and thoughts about using can be experienced and not acted on. The ultimate effectiveness of approaches such as ACT is still unclear, but it provides preliminary evidence suggesting the need for additional research. Nonetheless, the application of this approach to marijuana dependence presented methodological complications.
First, the use of a multiple baseline design with a clinical intervention presents some unique challenges. In most behavioral interventions the independent variable can be administered in one session, and results are apparent relatively rapidly. In a clinical intervention the independent variable is gradually administered over a longer period of time, which resulted in lengthy baselines for the 2nd and 3rd participants in this study. This creates an ethical dilemma that must be balanced with the need for good experimental control, namely how much of a change must be seen in the previous participant before the independent variable can begin to be presented to the following participant? In this investigation, the treatment was initiated for Participants 2 and 3 as soon as a clinically significant change was seen for the preceding participant. This resulted in initiating treatment for Participants 2 and 3 prior to the preceding participant's marijuana use reaching near zero, but after significant changes determined by slope and means occurred. This resulted in a different, but experimentally sound, multiple baseline than is usually seen in single-subject research.
Second, it is unclear what is the best dependent variable for self-monitoring of marijuana use. In this investigation, 2 of the participants who smoked less and shared with peers reported inhalations per day, whereas the other participant reported bowls of marijuana smoked per day. This metric possesses limitations because each inhalation and bowl will possess slightly varying amounts of the substance, and participants may have reduced the number of inhalations or bowls but may have increased the depth of inhalation. This can affect what can be said about overall reduction. Nevertheless, this metric was applied consistently across time to allow the detection of changes for each participant. Thus, it is safe to say that the intervention was useful but the exact amount of reduction remains questionable.
A third limitation is that 2 of the 3 participants began using again at follow-up, although at lower rates. Even though it is not reasonable to compare studies, maintenance of treatment gains has been an issue in all other marijuana abuse treatment studies. This is certainly an issue that warrants further attention. One possibility is that moderation rather than abstinence could be a treatment goal for some. This might have been the goal for the 2 participants who were using at follow-up because they chose to start using; 1 of the participants used only on the weekends, which according to his reports, did not interfere with other areas of functioning. Nevertheless, it is unclear why 1 participant was no longer using at follow-up and why the other 2 were using at varying levels. Future research should determine what variables account for long-term improvements in ACT for marijuana dependence.
A fourth limitation is that the data are not totally consistent with regards to assessments of the AAQ, depression, anxiety, and withdrawal symptoms. The means for all participants decreased from pre- to posttreatment with stable or continued decreases at follow-up, but individual patterns are not all consistent with this finding. In addition, the findings on these secondary measures do not closely match the main dependent variable. These issues will likely be clarified through larger and more systematic research and through measure development. For example, across the ACT literature, problem-specific measures of acceptance, defusion, and values correlate better with outcome than general measures such as the AAQ (Hayes, Luoma, Bond, Masuda, & Lillis, 2006).
A final limitation is that formal assessment methods were not used for diagnoses of marijuana dependence because of the preliminary nature of the study and its focus on reduction of use over changes in diagnostic criteria. Nevertheless, formal diagnoses allow greater comparison across investigations because they clarify the participants' similarities. Thus, formal diagnostic devices should be used in future studies. In addition, standardized procedures should also be used to assess co-occurring conditions, because they provide insight into who might benefit from treatment.
Even though this study possesses many limitations, it is important to open up new alternatives to be explored. Previous studies on ACT for substance abuse (e.g., Gifford et al., 2004; Hayes, Wilson, et al., 2004) suggest that issues that have been championed by clinical behavior analysts for many years (Friman, Hayes, & Wilson, 1998; Hayes, Jacobson, Follette, & Dougher, 1994) can be helpful to substance users and can provide an alternative approach to the cravings and urges to use that are seen in substance abuse problems. The present study suggests that well-controlled group-comparison studies of ACT are a logical next step.
Acknowledgments
We thank Tom Waltz, Doug Woods, and the anonymous reviewers for their many insightful comments on earlier versions of this manuscript.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (text rev.) Washington, DC: Author; 2000. [Google Scholar]
- Beck A.T. Beck depression inventory (2nd ed.) San Antonio, TX: The Psychological Corporation; 1996. [Google Scholar]
- Beck A.T, Epstein N, Brown G, Steer R.A. An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Beck A.T, Wright F.D, Newman C.F, Liese B.S. Cognitive therapy of substance abuse. New York: Guilford; 1993. [PubMed] [Google Scholar]
- Budney A.J, Higgins S.T, Radonovich K.J, Novy P.L. Adding voucher-based incentives to coping skills and motivational enhancement improves outcomes during treatment for marijuana dependence. Journal of Consulting and Clinical Psychology. 2000;68((6)):1051–1061. doi: 10.1037//0022-006x.68.6.1051. [DOI] [PubMed] [Google Scholar]
- Budney A.J, Novy P, Hughes J.R. Marijuana withdrawal among adults seeking treatment for marijuana dependence. Addiction. 1999;94:1311–1322. doi: 10.1046/j.1360-0443.1999.94913114.x. [DOI] [PubMed] [Google Scholar]
- Chaney E.F, O'Leary M.R, Marlatt G.A. Skill training with alcoholics. Journal of Consulting & Clinical Psychology. 1978;46((5)):1092–1104. doi: 10.1037//0022-006x.46.5.1092. [DOI] [PubMed] [Google Scholar]
- Childress A.R, McLellan A.T, Natale M, O'Brien P. Mood states can elicit conditioned withdrawal and craving in opiate abuse patients. Washington, DC: U.S. Department of Health & Human Services; 1986. pp. No. 76, 137–144. [PubMed] [Google Scholar]
- Copeland J, Swift W, Roffman R, Stephens R. A randomized controlled trial of brief cognitive behavioural interventions for cannabis use disorder. Journal of Substance Abuse Treatment. 2001;21:55–64. doi: 10.1016/s0740-5472(01)00179-9. [DOI] [PubMed] [Google Scholar]
- Eifert G.H, Heffner M. The effects of acceptance versus control contexts on avoidance of panic-related symptoms. Journal of Behavior Therapy and Experimental Psychiatry. 2003;34:293–312. doi: 10.1016/j.jbtep.2003.11.001. [DOI] [PubMed] [Google Scholar]
- Friman P.C, Hayes S.C, Wilson K.G. Why behavior analysts should study emotion: The example of anxiety. Journal of Applied Behavior Analysis. 1998;31:137–156. doi: 10.1901/jaba.1998.31-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gifford E.V, Kohlenberg B.S, Hayes S.C, Antonuccio D.O, Piasecki M.M, Rasmussen-Hall M.L, et al. Acceptance theory-based treatment for smoking cessation: An initial trial of acceptance and commitment therapy. Behavior Therapy. 2004;35:689–705. [Google Scholar]
- Goldiamond I. Toward a constructional approach to social problems: Ethical and constitutional issues raised by applied behavior analysis. Behavior and Social Issues. 2002;11:108–197. (Reprinted from Behaviorism, 2, 1-84, 1974) [PubMed] [Google Scholar]
- Goldstein M.G, Niaura R, Follick M.J, Abrams M.P. Effects of behavioral skills training and schedule of nicotine gum administration on smoking cessation. American Journal of Psychiatry. 1989;146:56–60. doi: 10.1176/ajp.146.1.56. [DOI] [PubMed] [Google Scholar]
- Gutiérrez O, Luciano C, Rodríguez M, Fink B.C. Comparison between an acceptance-based and a cognitive-control-based protocol for coping with pain. Behavior Therapy. 2004;35:767–784. [Google Scholar]
- Haas A.P, Hendin H. The meaning of chronic marijuana use among adults: A psychosocial perspective. Journal of Drug Issues. 1987;17:333–348. [Google Scholar]
- Hayes S.C. Acceptance and commitment therapy, relational frame theory, and the third wave of behavioral and cognitive therapies. Behavior Therapy. 2004;35:639–666. doi: 10.1016/j.beth.2016.11.006. [DOI] [PubMed] [Google Scholar]
- Hayes S.C, Jacobson N.S, Follette V.M, Dougher M.J, editors. Acceptance and change: Content and context in psychotherapy. Reno, NV: Context Press; 1994. [Google Scholar]
- Hayes S.C, Luoma J, Bond F, Masuda A, Lillis J. Acceptance and commitment therapy: Model, processes, and outcomes. Behaviour Research and Therapy. 2006;44:1–25. doi: 10.1016/j.brat.2005.06.006. [DOI] [PubMed] [Google Scholar]
- Hayes S.C, Strosahl K.D, Wilson K.G. Acceptance and commitment therapy: An experiential approach to behavior change. New York: Guilford; 1999. [Google Scholar]
- Hayes S.C, Strosahl K.D, Wilson K.G, Bissett R.T, Pistorello J, Toarmino D, et al. Measuring experiential avoidance: A preliminary test of a working model. The Psychological Record. 2004;54:553–578. [Google Scholar]
- Hayes S.C, Wilson K.G, Gifford E.V, Bissett R, Paisecki M, Batten S.V, et al. A preliminary trial of twelve-step facilitation and acceptance and commitment therapy with polysubstance-abusing methadone-maintained opiate addicts. Behavior Therapy. 2004;35:677–688. [Google Scholar]
- Johnston L.D, O'Malley P.M, Bachman J.G, Schulenberg J.E. Monitoring the future: National results on adolescent drug use: Overview of key findings 2004 (NIH Publication No. 05-5726) Bethesda, MD: National Institute on Drug Abuse; 2005. [Google Scholar]
- Levitt J.T, Brown T.A, Orsillo S.M, Barlow D.H. The effects of acceptance versus suppression of emotion on subjective and psychophysiological response to carbon dioxide challenge in patients with panic disorder. Behavior Therapy. 2004;35:747–766. [Google Scholar]
- Lynskey M.T, Coffey C, Degenhardt L, Carlin J.B, Patton G. A longitudinal study of the effects of adolescent cannabis abuse on high school completion. Addiction. 2003;98:685–692. doi: 10.1046/j.1360-0443.2003.00356.x. [DOI] [PubMed] [Google Scholar]
- Masuda A, Hayes S.C, Sackett C, Twohig M.P. Cognitive defusion and self- relevant negative thoughts: Examining the impact of a ninety year old technique. Behaviour Research and Therapy. 2004;42:477–485. doi: 10.1016/j.brat.2003.10.008. [DOI] [PubMed] [Google Scholar]
- McRae A.L, Budney A.J, Brady K.T. Treatment of marijuana dependence: A review of the literature. Journal of Substance Abuse Treatment. 2003;24:369–376. doi: 10.1016/s0740-5472(03)00041-2. [DOI] [PubMed] [Google Scholar]
- Meyer R.E. Old wine, new bottle: The alcohol dependence syndrome. Psychiatric Clinics of North America. 1986;9((3)):435–453. [PubMed] [Google Scholar]
- Miller N.S, Gold M.S. The disease and adaptive models of addiction: A re-evaluation. Journal of Drug Issues. 1991;20:29–35. [Google Scholar]
- Miller N.S, Gold M.S, Pottash A, Carter C. A 12-step approach for marijuana (Cannabis) dependence. Journal of Substance Abuse Treatment. 1989;6((4)):241–250. doi: 10.1016/0740-5472(89)90048-2. [DOI] [PubMed] [Google Scholar]
- Miller W.R, Rollnick S. Motivational interviewing: Preparing people to change addictive behavior. New York: Guilford; 1991. [Google Scholar]
- Newcomb M.D, Chou C, Bentler P.M, Huba G.J. Cognitive motivations for drug use among adolescents: Longitudinal tests of gender differences and predictors of change in drug use. Journal of Counseling Psychology. 1988;35((4)):426–438. [Google Scholar]
- Pierson H.M, Bunting K, Smith A.A, Gifford E.V, Hayes S.C. A functional approach to measuring therapists' adherence and competence in acceptance and commitment therapy (ACT) 2004. May, [Google Scholar]
- Pope H.G, Yurgelun-Todd D. Residual cognitive effects of long-term cannabis use. In: Castle, D, Murray R, editors. Marijuana and madness: Psychiatry and neurobiology. New York: Cambridge University Press; 2004. pp. 198–210. [Google Scholar]
- Rainone G.A, Deren S, Kleinman P.H, Wish E.D. Heavy marijuana users not in treatment. The continuing search for the “pure” marijuana user. Journal of Psychoactive Drugs. 1987;19:353–359. doi: 10.1080/02791072.1987.10472423. [DOI] [PubMed] [Google Scholar]
- Sheldon K.M, Elliot A.J. Goal striving, need satisfaction, and longitudinal well-being. Journal of Personality and Social Psychology. 1999;76:482–497. doi: 10.1037//0022-3514.76.3.482. [DOI] [PubMed] [Google Scholar]
- Sher K.J, Trull T.J. Personality and disinhibitory psychopathology: Alcoholism and antisocial personality disorder. Journal of Abnormal Psychology. 1994;103((1)):92–102. doi: 10.1037//0021-843x.103.1.92. [DOI] [PubMed] [Google Scholar]
- Solowij N, Michie P.T, Fox A.M. Differential impairments of selective attention due to frequency and duration of cannabis use. Biological Psychiatry. 1995;37((10)):731–739. doi: 10.1016/0006-3223(94)00178-6. [DOI] [PubMed] [Google Scholar]
- Stephens R.S, Babor T.F, Kadden R, Miller M The Marijuana Treatment Project Research Group. The marijuana treatment project: Rationale, design, and participant characteristics. Addiction. 2002;97((Suppl. 1)):109–124. doi: 10.1046/j.1360-0443.97.s01.6.x. [DOI] [PubMed] [Google Scholar]
- Stephens R.S, Roffman R.A, Curtin L. Comparison of extended versus brief treatments for marijuana use. Journal of Consulting and Clinical Psychology. 2000;68:898–908. [PubMed] [Google Scholar]
- Stephens R.S, Roffman R.A, Simpson E.E. Treating adult marijuana dependence: A test of the relapse prevention model. Journal of Consulting and Clinical Psychology. 1994;62:92–99. doi: 10.1037//0022-006x.62.1.92. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2004 national survey on drug use and health: National findings (Office of Applied Studies, NSDUH, Series H-28, DHHS Publication No. SMA 05-4062) 2005. Rockville, MD. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Treatment episode data set (TEDS)—Highlights 2004. Nation admissions to substance abuse treatment services (Office of Applied Studies, DASIS Series: S-31. DHHS Publication No. SMA 06-4140) 2006. Rockville, MD. [Google Scholar]
- Tapert S.F, Aaron G.A, Sedlar G.R, Brown S.A. Adolescent substance abuse and sexual risk-taking behavior. Journal of Adolescent Health. 2001;28:181–189. doi: 10.1016/s1054-139x(00)00169-5. [DOI] [PubMed] [Google Scholar]
- Tashkin D.P, Fligiel S, Wu T, Gong H, Barbers R.G, Coulson A.H, et al. Effects of habitual use of marijuana and/or cocaine on the lung. In: Chiang C.N, Hawks R.L, editors. Research findings on smoking of abused substances. National Institute on Drug Abuse Research Monograph No. 99, DHHS Publication No. 90-1690. Washington, DC: U.S. Government Printing Office; 1990. pp. 63–86. [Google Scholar]
- Twohig M.P, Hayes S.C, Masuda A. Increasing willingness to experience obsessions: Acceptance and commitment therapy as a treatment for obsessive compulsive disorder. Behavior Therapy. 2006;37:3–13. doi: 10.1016/j.beth.2005.02.001. [DOI] [PubMed] [Google Scholar]