Abstract
We evaluated the effects of a behavioral treatment on the safe passing of sharp instruments using the hands-free technique among hospital operating room personnel during surgical procedures. Treatment consisted of participative goal setting, task clarification, and feedback. The average percentage of sharp instruments passed safely increased from 32% to 64% and 31% to 70% between baseline and treatment phases in the inpatient and outpatient surgery units, respectively. Five-month follow-up data suggested maintenance of treatment effects. These findings suggest the utility of organizational behavior management strategies in reducing risky behavior in hospital settings.
Keywords: injury reduction, organizational behavior management, goal setting, feedback, task clarification, surgical procedures
Health-care and manufacturing industries have the most serious nonfatal injuries, with health care accounting for 16% of all U.S. nonfatal injuries annually. In 2005, a total of 281,500 recordable injuries to health-care workers were reported, resulting in an injury rate of 8.1 per 100 full-time workers (U.S. Department of Labor Statistics, 2006).
The substantial costs associated with work-related injuries have prompted administrators to seek ways to reduce the occurrence of injuries among their employees. Logically speaking, reducing exposures to hazards is the only way to reduce injuries at work. Safety professionals use five levels of risk-exposure reduction practices: elimination of the hazard; substitution of the hazardous procedure with a less hazardous one; implementing engineering solutions to remove employee exposure; administration of policies and procedures to reduce employee exposure; and personal control of employees when interacting with the hazard (Plog, Niland, Quinlan, & Plogg, 2002). Behavioral approaches cover the latter two categories, and risk reduction is typically accomplished through coordination of efforts from all categories.
Behavioral approaches to risk reduction typically involve identifying behaviors associated with injury, clearly defining the behaviors, measuring the behaviors repeatedly and frequently through observation, and then applying behavior-change strategies such as training, reinforcement, feedback, and goal setting to change the critical behaviors. For example, DeVries, Burnette, and Redmon (1991) used a behavioral feedback system to increase nurses' compliance with glove wearing to reduce exposure to bloodborne pathogens.
Sharps injuries (e.g., being stuck with a needle) are of such prevalence in the health-care industry that states have passed laws (i.e., policy controls) requiring that health-care providers use devices (i.e., engineering controls) to reduce exposure to sharps (Eck, 2000). Laws such as these are helpful, but without a plan to change behaviors, change may be difficult. One way to reduce sharps exposures in the operating room is to ensure that the surgeon and scrub nurse do not touch the same instrument at the same time. This is known as the hands-free technique (Stringer, Infante-Rivard, & Hanley, 2002). The technique requires that a neutral zone be established between the surgeon and the scrub nurse where instruments are placed in the process of exchange, thereby reducing the exposure of both parties to exchange-related risks associated with sharps.
The present study was designed to increase the use of the hands-free technique during surgical procedures by using well-established techniques from the field of organizational behavior management.
Method
Participants and Settings
The participants were hospital operating room (OR) employees ranging in age from 20 to 63 years. Observed teams ranged from 2 to 5 people and included at least 1 surgeon and registered nurse (RN) and occasionally scrub technicians and other nurses and surgeons. The settings were ORs in the inpatient and outpatient surgery units of a 348-bed hospital that served a nine-county region in the midwestern U.S. Hospital injury data showed the inpatient and outpatient surgery units had the highest injury frequencies, particularly sharps injuries to RNs, which were apparently linked to sharps exposure.
Data Collection
The first author collected data in 78 30-min sessions during surgical procedures, beginning at the time of opening incision or at any point estimated by the circulating nurse to be at least 30 min prior to final closure. On three occasions the nurse's estimate was inaccurate (yielding a session shorter than 30 min), so these data were discarded, but the data were not sufficiently different to threaten internal validity.
Observers stood in the operating room, beyond the sterile surgical field, in view of the area where instruments were being exchanged. Although participants may have been aware of the presence of data collectors, it was common for observers to be present during surgical procedures. Nonetheless, to minimize reactivity, observers stood behind participants, remained silent during data collection (unless spoken to by a surgical team member), and responded to questions regarding their presence with nonspecific answers such as “I am here to conduct safety observations for a school project.” Observations occurred between 11:30 a.m. and 3:00 p.m., and varied between the inpatient and outpatient units based on scheduling of surgical procedures and random selection by unit coordinators.
Dependent Variable and Interobserver Agreement
In the hands-free technique, sharps are passed by one person placing the instrument in a preestablished neutral zone and another person picking up that same instrument. Neutral zones included a magnetic pad, towel, or basin on the sterile field located between the scrub person and the surgeon. Instruments identified as sharps in the hospital OR online manual were the targeted objects and included anything sharp enough to puncture a glove, including scalpels, loaded needle holders, sharp rake retractors, gelpi retractors, skin hooks, and sharp-pointed electrocautery tips.
The dependent variable measured during the project was the percentage of sharps exchanges using the neutral zone, derived by dividing the total number of sharps exchanges using the hands-free technique by the total number of sharps exchanges observed and multiplying by 100%.
Interobserver agreement was assessed during approximately 25% of sessions using the point-by-point formula (the number of agreements divided by the number of agreements and disagreements and multiplied by 100%). The judgment unit used was the passing of a sharp (neutral zone vs. hand to hand). Overall agreement for neutral zone use averaged 90% (range, 69% to 100%; SD = 9.5%).
Experimental Design and Procedure
A multiple baseline design across participants and settings was used to evaluate the effects of our treatment package.
Baseline. Behavioral observations were conducted on the inpatient unit for 15 sessions over 4 weeks and on the outpatient unit for 24 sessions over 5.5 weeks.
Treatment Package
A combination of goal setting, task clarification, and feedback was used to increase use of the hands-free technique. In a meeting at the start of the treatment phase, the unit coordinator reminded staff of the extant hospital policy regarding the hands-free technique during surgery, explained the importance of the neutral zone when passing sharps (i.e., infection, contamination, costs of injuries, physical pain), and informed them that although neutral zones were being established at a rate of 75%, the use of the neutral zone was occurring at a rate of only 32%. The coordinator then asked the staff to set a goal percentage of neutral zone use that was “challenging yet attainable,” and recorded the goal. The inpatient OR staff goal was 45%, and the outpatient OR staff goal was 75%.
Task clarification was accomplished during an initial meeting by having staff members model safe (use of a neutral zone) and unsafe (hand-to-hand) methods of exchanging a sharp instrument as the unit coordinator pointed out the safe and risky aspects of the tasks.
Based on reports sent by the first author, the coordinator verbally related feedback about whether staff met their goal percentage of neutral zone use, reported the average percentage of sharps passed safely using the neutral zone for the past week, and praised improvements at the weekly unit staff meeting.
Maintenance
A maintenance check of five observations during 1 week in both units was conducted approximately 5 months following the end of the treatment phase.
Results and Discussion
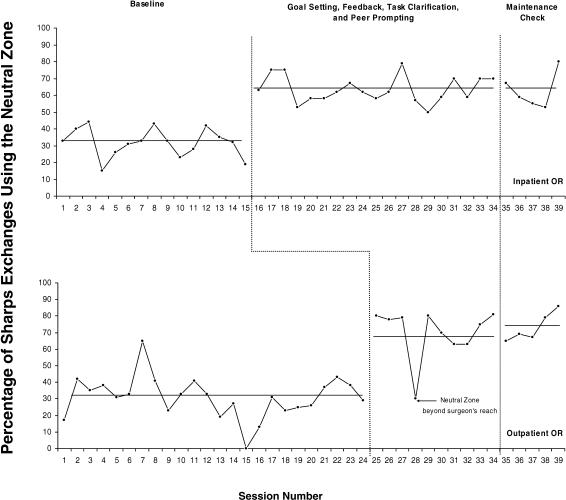
During baseline, the average percentage of sharps exchanged using the neutral zone was 32% (range, 15% to 44%; SD = 8.6%) for the inpatient OR and 31% (range, 0% to 65%; SD = 12.5%) for the outpatient unit (see Figure 1). During treatment, the average percentage of sharps exchanged using the neutral zone increased to 64% (range, 57% to 79%; SD = 7.9%) in the inpatient OR and to 70% (range, 30% to 81%; SD = 15.6%) in the outpatient OR. During the maintenance phase the average percentage of sharps exchanged using the neutral zone decreased slightly to 63% (range, 55% to 80%; SD = 11.0%) in the inpatient OR and increased to 73% (range, 65% to 86%; SD = 8.9%) in the outpatient OR.
Figure 1.
Percentage of sharp instruments exchanged using the neutral zone across the inpatient and outpatient OR units. Solid horizontal lines represent phase averages.
The treatment package resulted in immediate and sizable improvements in the use of the hands-free technique among OR staff. Before this study, the efforts in the OR department to monitor compliance with the policy regarding use of the hands-free technique amounted to measuring neutral zone establishment at the start of a procedure. We found that establishing the neutral zone before surgery was not resulting in an acceptable rate of using the neutral zone. Interestingly, we also observed that surgical teams that established a neutral zone at the onset of a procedure did not use the neutral zone more often than teams that failed to do so. This suggests that governmental and organizational policies must focus not only on establishing neutral zones but also on the sharps handling behavior of surgery teams during procedures.
The managers of each unit delivered the treatment package in reasonably similar ways. Feedback and praise were delivered weekly (as scheduled) in both units during the treatment package, three times in the inpatient unit and twice in the outpatient unit. The only significant treatment difference between the two units was the participative goals that were set (45% for the inpatient unit and 75% for the outpatient unit). Each of the treatment components has been used widely in organizational behavior management and for safety in particular, including feedback (Alavosius & Sulzer-Azaroff, 1990), goal setting (Ludwig & Geller, 1997), and task clarification (Komaki, Barwick, & Scott, 1978).
Participative goal setting (as opposed to assigned goals) was used in this study because participation was typical of this particular work environment and it gave employees an opportunity to exert control on the decision making of the organization. Task clarification assured that staff were aware of the hospital policy and how to properly comply with the policy on using the neutral zone in exchanging sharps, and managers in both units reported that staff did not initially identify the proper technique of passing sharps when asked to do so. Feedback was included to address the lack of knowledge among the staff regarding their rate of neutral zone use and to provide a consequence for performance of the desired behavior.
Although the treatment package substantially increased the use of the hands-free technique, the results of this study should be interpreted with caution. The duration of the study was relatively short, lasting only 3 months, with the maintenance check lasting for 1 week (5 months later). Although sharps-related injuries declined during the treatment period (from a frequency of 10.3 per quarter to 6 for the first full quarter of treatment implementation), the relatively brief length of the study prohibits a more complete analysis of the effects of neutral zone use on injury rates. Such analyses, although clearly preferable in a safety improvement study, require extended periods of data collection (i.e., more than 1 year).
The findings of this study are also limited by the use of a package intervention, which prevents the evaluation of the effects of individual treatment components. It could be valuable to know which component is most effective. In addition, it is somewhat surprising to find that similar levels of performance were achieved between the inpatient and outpatient units were achieved with such drastically different goals selected by the participants in each unit (45% inpatient goal vs. 75% outpatient goal). Although one might expect differences in performance based on differences in target performance goals, this could not be tested given the package treatment approach we used. It is possible that the feedback component was the most powerful component, and thus overwhelmed any differences in the effects of selected goals on performance.
For the site to continue using the procedures after the study was completed, modifications were made so that nurses, patient-care assistants, or coordinators could collect data quickly and easily. Therefore, the plan that was developed was an add-on to an extant audit procedure in which the rate of neutral zone establishment and a subjective rating of hands-free technique use (i.e., always, sometimes, or never) were recorded by the circulating nurse. This did not provide detailed percentages of neutral zone use, but it did provide staff with a result that could be used to provide feedback. The goal-setting component of the treatment was also integrated into an existing gainsharing pay system, wherein the staff selected a yearly target performance that could result in a year-end monetary bonus.
Footnotes
Correspondence concerning this article should be addressed to Thomas R. Cunningham, Department of Psychology, Virginia Polytechnic Institute and State University, Blacksburg, Virginia 24061 (e-mail: tcunning@vt.edu) or John Austin, Department of Psychology, Western Michigan University, Kalamazoo, Michigan 49008 (e-mail: john.austin@wmich.edu).
References
- Alavosius M.P, Sulzer-Azaroff B. Acquisition and maintenance of health-care routines as a function of feedback delivery. Journal of Applied Behavior Analysis. 1990;23:151–162. doi: 10.1901/jaba.1990.23-151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeVries J.M, Burnette M.M, Redmon W.K. AIDS prevention: Improving nurses' compliance with glove wearing through performance feedback. Journal of Applied Behavior Analysis. 1991;24:705–711. doi: 10.1901/jaba.1991.24-705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eck E.K. Infection Control Today. 2000. Sep, Achieving sharps injury reduction: Moving from theory to implementation. [Google Scholar]
- Komaki J, Barwick K.D, Scott L.W. A behavioral approach to occupational safety: Pinpointing and reinforcing safe performance in a food manufacturing plant. Journal of Applied Psychology. 1978;63:434–445. [PubMed] [Google Scholar]
- Ludwig T.D, Geller S.E. Assigned versus participative goal setting and response generalization: Managing injury control among professional pizza deliverers. Journal of Applied Psychology, 92. 1997;2:253–261. doi: 10.1037/0021-9010.82.2.253. [DOI] [PubMed] [Google Scholar]
- Plog B.A, Niland J, Quinlan P.J, Plogg H, editors. Fundamentals of industrial hygiene (5th ed.) Itasca, IL: National Safety Council; 2002. [Google Scholar]
- Stringer B, Infante-Rivard C, Hanley J.A. Effectiveness of the hands-freetechnique in reducing operating theatre injuries. Occupational and Environmental Medicine. 2002;59:703–707. doi: 10.1136/oem.59.10.703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Labor Statistics U.S. Workplace injuries and illnesses in 2005. 2006. [Google Scholar]