Abstract
Aim
To evaluate the possible prognostic role of the expression of MAGE-A4 and NY-ESO-1 cancer/testis antigens in women diagnosed with invasive ductal breast cancer and determine the expression of HER-2 antigen.
Methods
The expression of MAGE-A4, NY-ESO-1, and HER-2 antigens was evaluated immunohistochemically on archival paraffin-embedded samples of breast cancer tissue from 81 patients. All patients had T1 to T3, N0 to N1, M0 tumors and underwent postoperative radiotherapy and, if indicated, systemic therapy (chemotherapy and hormonal therapy). The antigen expression in women who were disease-free for 5 years of follow up (n = 23) was compared with that in women with either locoregional relapse (n = 30) or bone metastases (n = 28). Patient survival after 10 years of follow up was assessed.
Results
The three groups of women were comparable in terms of age, type of operation, tumor size, tumor grade, number of metastatically involved axillary lymph nodes, Nottingham prognostic index (NPI), progesterone receptor (PR) status, and adjuvant hormonal therapy. Estrogen receptors (ER) were positive in 13 women in the 5-year relapse-free group vs 8 in locoregional relapse and 7 in bone metastases group (P = 0.032). There were significantly fewer women who received adjuvant chemotherapy in the 5-year relapse-free group than in other two groups (7 vs 23 with locoregional relapse and 25 with bone metastases; P<0.001). This group also had a significantly better 10-year survival (14 women vs 1 with locoregional relapse and 1 with bone metastases; P<0.001). The three groups did not differ in the NY-ESO-1 or HER-2 expression, but the number of patients expressing MAGE-A4 antigen was significantly lower in the group with locoregional relapse (P = 0.014). In all groups, MAGE-A4 antigen expression was associated with the NY-ESO-1 antigen expression (P = 0.006), but not with tumor size and grade, number of metastatically involved axillary lymph nodes, or the ER and PR status. MAGE-A4-positive patients had a significantly longer survival than the MAGE-A4-negative patients (P = 0.046). This was not observed with NY-ESO-1 and HER-2 antigens.
Conclusion
Our results suggest that the MAGE-A4 antigen may be used as a tumor marker of potential prognostic relevance.
Breast cancer is the most common malignancy in women (1). Its clinical course may vary from indolent and slowly progressive to rapidly metastatic disease. Identification of prognostic and predictive factors that reflect the biology of breast cancer is important for the assessment of prognosis and selection of patients who may benefit from adjuvant and/or systemic therapy. The important aspects of prognostic factors suitable for clinical use are their availability, reproducibility, and cost. In routine clinical practice, treatment decisions and selection of treatment modalities for each individual patient are based on the standard prognostic factors, such as age (1,2), menopausal status (3), tumor size (1-4), tumor grade (3-5), steroid-hormone receptor status (1-5), and nodal metastases (1-5).
Variability in clinical course of breast cancer is partly related to tumor cell growth rate and other features, such as invasiveness or metastatic potential. Research in molecular biology has identified genes and their products involved in or associated with the malignant cell transformation and behavior. Moreover, expression of some of these molecules, such as p53 (1,6,7), Ki-67 (7,8), nm23 (1,7), catepsin D (1,7), Ep-CAM (9,10), HER-2 (1,2,6), and urokinase-type plasminogen activator and its inhibitor (1,11), is associated with the patient’s prognosis. As it seems that many genes and molecules might be involved in malignant transformation and cell behavior, other additional molecules may also be tested as potential prognostic factors.
The cancer/testis (C/T) genes encode tumor-associated antigens (TAA) found in various tumors of different histological origin, but not in normal tissues other than testis (12,13). Their physiological function is unknown. Peptides derived from these antigens could be used as targets in active immunotherapy. Analysis of the expression of these genes or their products in malignancies could also be of potential diagnostic and/or prognostic relevance (14,15). Therefore, we performed a retrospective analysis of immunohistochemical expression of C/T antigens MAGE-A4 and NY-ESO 1 in women with invasive breast cancer. We also analyzed the expression of HER-2 antigen, because it has a prognostic and predictive role (1,16).
Patients and methods
Patients
Women who had invasive breast cancer in 1995 and underwent postoperative adjuvant radiotherapy were identified from medical documentation available at the Department of Radiotherapy, University Hospital for Tumors, Zagreb, in 2000. Only women with complete medical data and adequate tumor-tissue samples available from archival paraffin-embedded blocks were eligible. Women were included in the study if, at the moment of initial diagnosis, they had breast cancer without distant metastases (pT1-3pN0-1M0) for which they received surgical and adjuvant treatment of radiotherapy and, if indicated, systemic treatment (chemotherapy and hormonal therapy) in our Hospital. Women who received neoadjuvant therapy, had another primary cancer, or received treatment at an institution other than ours were excluded from the study. The final number of women included in the analysis was 81. According to the disease status, there were three groups, as follows: women who had been relapse-free for five years, ie, from 1995 to 2000, those with locoregional relapse, and those with bone metastases. Almost all women with locoregional relapse had undergone repeated surgical and irradiation treatment. Locoregional relapse was defined as the first recognized recurrence of the disease in the chest wall, breast, axilla, or supraclavicular region. Women with bone metastases had all undergone irradiation treatment. Those who were diagnosed with invasive breast cancer in years other than 1995 were included in groups with locoregional and metastatic disease, so that each group consisted of a similar number of patients.
Data collection
Medical files at the Department of Radiotherapy contained the data on the patients' clinicopathological findings, radiotherapy decisions, and/or treatments. Other data, such as those on the existence and sites of visceral organ metastatic disease or previous or planned systemic treatments of metastatic disease, were often not recorded or available for patients who were referred to the Department for radiotherapy and otherwise followed-up by other oncologists, surgeons, or general practitioners. Often, the day of disease relapse (locoregional or metastatic) could not be precisely determined. The complete data were collected on the date of breast cancer operation, pathological findings, and the type of adjuvant systemic therapy.
Patient survival analysis was performed in 2005. The survival data were also checked against the Croatian National Cancer Registry and rechecked whenever possible by telephone calls to patients presumed to be alive. The study protocol was approved by the Ethics Committee of the Hospital and informed consent was obtained from all patients included in the study.
Clinicopathological features
Clinicopathological and laboratory data included age, year of diagnosis, type of surgery, median time to disease relapse, tumor size, histological grade, axillary node status, Nottingham Prognostic Index (NPI) (17), estrogen and progesterone receptor positivity, administration of adjuvant chemotherapy or of adjuvant tamoxifen, and patient survival (Table 1).
Table 1.
Characteristics of 81 women diagnosed with invasive ductal breast cancer in 1995 after 5 years of follow-up
| No. of women with breast cancer |
|||||
|---|---|---|---|---|---|
| Characteristics* | relapse-free (n = 23) | locoregional relapse (n = 30) | bone metastases (n = 28) | total | P† |
| Age at diagnosis (y): | |||||
| 30-39 | 0 | 3 | 0 | 3 | 0.720‡ |
| 40-49 | 6 | 7 | 7 | 20 | |
| 50-59 | 7 | 7 | 7 | 21 | |
| 60-69 | 6 | 10 | 12 | 28 | |
| 70-79 | 3 | 2 | 1 | 6 | |
| 80-89 | 1 | 1 | 1 | 3 | |
| Year of initial diagnosis (No. of patients) | 1995 (23) | 1992 (1), 1993 (2), 1994 (8), 1995 (15), 1996 (2), 1997 (2) | 1995 (9), 1997 (10), 1998 (7), 1999 (2) | ||
| Type of operation: | |||||
| mastectomy with axillary dissection | 20 | 30 | 26 | 76 | 0.143 |
| segmentectomy with axillary dissection | 3 | 0 | 2 | 5 | |
| Disease relapse in 2000 (median; mo) | / | 18 | 13 | <0.001 | |
| range (mo) | / | (3-49) | (2-44) | ||
| Tumor size (cm): | |||||
| <2 | 7 | 7 | 13 | 27 | 0.200 |
| 2-5 | 16 | 20 | 13 | 49 | |
| >5 | 0 | 3 | 2 | 5 | |
| Histological grade:§ | |||||
| I | 4 | 3 | 1 | 8 | 0.521 |
| II | 13 | 18 | 16 | 47 | |
| III | 6 | 9 | 11 | 26 | |
| Axillary lymph node status: | |||||
| 0 | 0 | 4 | 2 | 6 | 0.203 |
| 1-3 | 14 | 10 | 12 | 36 | |
| ≥4 | 9 | 16 | 14 | 39 | |
| Nottingham prognostic index: | |||||
| ≤3.4 | 1 | 3 | 1 | 5 | 0.383 |
| 3.41-5.4 | 14 | 11 | 16 | 41 | |
| >5.4 | 8 | 16 | 11 | 35 | |
| Estrogen receptor (fmol/mg): | |||||
| <5 | 10 | 22 | 21 | 53 | 0.032 |
| ≥5 | 13 | 8 | 7 | 28 | |
| Progesterone receptor (fmol/mg): | |||||
| <10 | 8 | 15 | 8 | 31 | 0.225 |
| ≥10 | 15 | 15 | 20 | 50 | |
| Adjuvant chemotherapy CMF/FAC | 6/1 | 20/3 | 16/9 | 42/13 | <0.001 |
| Adjuvant tamoxifen | 12 | 10 | 12 | 34 | 0.385 |
| 5-y survival: | |||||
| alive | 23 | 7 | 2 | 32 | <0.001 |
| dead | - | 18 | 22 | 40 | |
| unknown | - | 5 | 4 | 9 | |
| 10-y survival: | |||||
| alive | 14 | 1 | 1 | 16 | <0.001 |
| dead | 7 | 24 | 23 | 54 | |
| unknown | 2 | 5 | 4 | 11 | |
*Abbreviations: CMF – cyclophosphamide, methotrexate, 5-fluorouracil; FAC – 5-fluorouracil, doxorubicine, cyclophosphamide.
†Pearson χ2 test for all values except time to disease relapse and 5-year survival (F test within analysis of variance test).
‡P value refers only to 40-69-year age groups, because other age groups had cell frequencies <5.
§Histological grading according to the method by Elston (18).
Pathological examination of primary tumors and axillary lymph nodes was performed at the Department of Pathology. For routine histological analysis, the resected tissue was fixed in 10% buffered formalin, embedded in paraffin, and stained with hematoxylin and eosin. The histological grade of tumors was determined according to the method by Elston (18). Tumors were divided into three groups according to tumor size (0.1-2.0 cm as pT1, 2.1-5.0 cm as pT2, and >5.0 cm as pT3) and the ipsilateral axillary lymph node status (negative lymph node as N0, and positive lymph node as N1) (19). NPI scores were calculated according to Rampault et al (17), as follows: NPI = 0.2 × tumor size (cm) + lymph-node stage (1, 2, or 3) + histological grade (1, 2, or 3), where size was measured in centimeters; lymph node stage 1 was lymph node-negative, stage 2 was one to three positive lymph nodes, stage 3 was more than three positive lymph nodes; and the scoring of histological grade was 1 to 3 (see below). For prognostic considerations, NPI was categorized into three groups, as follows: low (good prognosis), NPI≤3.4; intermediate (moderate prognosis), 3.4<NPI≤5.4; and high (poor prognosis), NPI>5.4. Concentrations of estrogen and progesterone receptors in tumor cytosol were evaluated by the dextran-coated charcoal assay as described elsewhere (20). Concentration of estrogen receptors (ER) of ≥5 fmol/mg of protein and progesterone receptors (PR) of ≥10 fmol/mg of protein were considered to be positive (20).
Adjuvant therapies were based and prescribed according to the University Hospital Treatment Protocol for Breast Cancer (unpublished document for in-house use). Cut-off values for ER and PR at the University Hospital for Tumors (20) were less strict than usually recommended (10 fmol/mg of protein for ER and 20 fmol/mg of protein for PR) (21). Consequently, decisions about the adjuvant therapies were based on these lower cut-off values. Adjuvant radiotherapy consisted of external megavoltage irradiation delivered from the linear accelerator (22). Adjuvant chemotherapy included either the CMF protocol (cyclophosphamide, 600 mg/m2 IV on day 1; methotrexate, 40 mg/m2 IV on day 1; 5-fluorouracil, 600 mg/m2 IV on day 1) or the FAC protocol (5-fluorouracil, 500 mg/m2 IV on day 1; doxorubicine, 50 mg/m2 IV on day 1; cyclophosphamide, 500 mg/m2 IV on day 1). Cycles were repeated every 3 weeks, for a total of 6 cycles. Tamoxifen was administered as systemic hormonal therapy (2 × 10 mg over 5 years) (23).
Immunohistochemical analysis for MAGE-A4, NY-ESO-1, and HER-2
Immunohistochemical analysis of primary breast cancer tissue was performed in 2000. Expression of MAGE-A4 and NY-ESO-1 tumor-associated C/T antigens in primary breast cancer tissue was determined by monoclonal antibody (mAb) 57B (24) and mAb B9.8.1.1 (25), respectively. Within our panel of monoclonal antibodies, mAb 57B (23) recognized many MAGE-A-related gene products, including MAGE-A2, MAGE-A3, MAGE-A4, MAGE-A6, and MAGE-A12 (26). In paraffin-embedded specimens, however, it had been shown to predominantly recognize MAGE-A4 TAA (27). Monoclonal antibody B9.8.1.1 is specific to NY-ESO-1 TAA (25). Briefly, tissue sections from paraffin-embedded breast tumor samples (0.5 mm thick) were placed on Silane (3-aminopropyltriethoxysilane, A 3648, Sigma, St Louis, MO, USA)-treated microscope glass slides. After deparaffinization, the sections were heated in a 800W household microwave oven at a maximum power for 8.5 and 5 minutes in 10 mmol/L citric buffer (pH 6.0) and washed with phosphate buffered saline (PBS; pH 7.2). The sections were treated by H2O2 to suppress endogenous peroxidase activity. After an additional PBS wash, the sections were incubated for 20 minutes with 1:10 diluted normal rabbit sera (DAKO X0902, DAKO A/S, Copenhagen, Denmark) at room temperature in a humidified chamber to prevent nonspecific immunoglobulin binding. The sections were then treated with mAb 57B or mAb B9.8.1.1., in the form of undiluted hybridoma supernatant, for 90 minutes at room temperature. A streptoavidin-biotinylated horseradish peroxidase-based detection system (DAKO K 0355) was used to reveal specific binding (28,29).
Immunoreactivity for MAGE-A4 and NY-ESO-1 was scored in the following way: 0, no positive tumor cells (negative); 1+, <20% positive tumor cells (“mild reaction”); 2+, 21-50% positive tumor cells (“moderate reaction”); and 3+, >50% positive tumor cells (“strong reaction”). Non-neoplastic cells, such as normal ductal epithelial cells and fibroblasts, were indeed present in all specimens but were not stained, and thus served as internal negative controls (28,29). The immunoreactivity scores were presented as either “negative” or “positive,” with positive including mild, moderate, and strong reactions.
DAKO Hercep TestTM kit was used for HER-2 immunohistochemical staining in accordance with manufacturer’s instructions. The monoclonal antibody in the DAKO Hercep TestTM kit is approved by Food and Drug Administration as the specific reagent for the HER-2 detection. Samples with 3+ staining intensity score (standard control slides were included in the Hercep TestTM kit) were considered to be HER-2 positive. When Hercep test scoring system was used, a strong positive reaction implied a complete (diffuse) membrane staining in >10% of tumor cells (16).
Statistical analysis
STATISTICA 6.1 software package (StatSoft Inc., Tulsa, OK, USA) was used for all statistical analyses. Differences in time to disease relapse and 5-year survival were tested by one way analysis of variance (ANOVA). Pearson χ2 test was applied for other clinicopathologic and immunohistochemical parameters represented as qualitative values. Kaplan-Meier survival method was used for the construction of survival probability curves, and Gehan’s Wilcoxon test for their comparison. P value of <0.05 was considered statistically significant.
Results
Most women were diagnosed with breast cancer in 1995 and most underwent modified radical mastectomy (Table 1). In the group of women with locoregional disease relapse, the median time to disease relapse was 18 months (range, 3-49), which was significantly longer than 13 months (range, 2-44) in the group with bone metastases (P<0.001). The three groups of patients did not differ in the standard clinical parameters except for ER status (P = 0.032) and adjuvant chemotherapy (P<0.001). In the 5-year relapse-free group, significantly more women had positive ER and significantly fewer received adjuvant chemotherapy; this group had a significantly better survival outcome (P<0.001). In 2005, 14 out of 23 women in this group were alive (with 2 women of unknown survival status), whereas in other two groups, only one women from each group was alive.
Immunohistochemical results
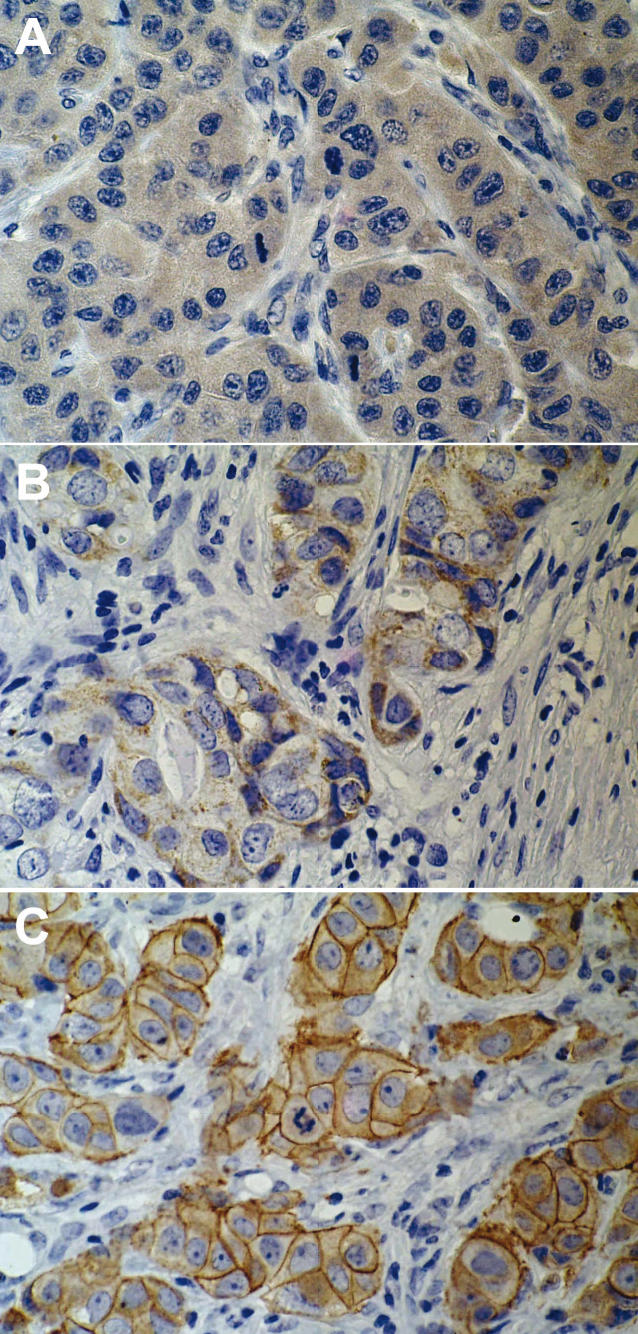
Immunohistochemical staining of C/T proteins, MAGE-A4 and NY-ESO-1, was predominantly visible as cytoplasmic staining limited to tumor cells (Figure 1A and 1B). HER-2 staining was visible as membrane staining (Figure 1C). Overall, positivity of mAb 57B and mAb B9.8.1.1 was found in 60 (74%) and 32 (40%) out of 81 women included in the study, respectively. The expression of MAGE-A4 antigen was detected in a significantly fewer women with locoregional relapse (P = 0.014; Table 2). Further analysis showed significant difference only in MAGE-A4 expression between the women with locoregional relapse and 5-year relapse-free group (P = 0.005). The expression of MAGE-A4 did not significantly differ between patients with locoregional relapse and those with bone metastases (P = 0.076). No significant difference was found in NY-ESO-1 antigen expression between the three groups of women. Positive HER-2 reaction was found in 18 out of 81 patients (22%), with equal distribution in all three groups.
Figure 1.
Immunohistochemical staining in invasive ductal breast cancer tissue. A. Intense cytoplasmic MAGE-A4 staining with monoclonal antibody (mAb) 57B observed in the absence of staining of normal ducts (peroxidase anti-peroxidase [PAP], ×400). B. NY-ESO-1 positivity with specific cytoplasmic tumor distribution detected by mAb B9.8.1.1 (PAP, ×400). C. Overexpression of HER-2 detected by Hercep test, with strong complete membrane staining in >10% of tumor cells, noticed as a strong immunohistochemical reaction (PAP, ×400).
Table 2.
Immunohistochemically detected expression of HER-2, MAGE-A-4, and NY-ESO-1 antigens in 81 women with invasive ductal breast cancer
| No. (%) of women with breast cancer |
|||||
|---|---|---|---|---|---|
| Antigen | relapse-free for 5 y (n = 23) | locoregional relapse (n = 30) | bone metastases (n = 28) | total | P* |
| HER-2: | |||||
| negative (0, 1+, 2+) | 19 (83.0) | 23 (77.0) | 22 (79.0) | 64 (79.0) | 0.868 |
| positive (3+) | 4 (17.0) | 7 (23.0) | 6 (21.0) | 17 (21.0) | |
| MAGE-A4:† | |||||
| negative (0) | 2 (9.0) | 13 (43.0) | 6 (21.0) | 21 (26.0) | 0.014‡ |
| positive (1+, 2+, 3+) | 21 (93.0) | 17 (57.0) | 22 (79.0) | 60 (74.0) | |
| NY-ESO-1:† | |||||
| negative (0) | 13 (57.0) | 22 (73.0) | 14 (50.0) | 49 (60.0) | 0.173 |
| positive (1+, 2+, 3+) | 10 (43.0) | 8 (27.0) | 14 (50.0) | 32 (40.0) | |
*Pearson χ2 test.
†Immunoreactivity was scored in the following way: 0, no positive tumor cells (negative); 1+, ≤20% positive tumor cells (“mild reaction”); 2+, 21-50% positive tumor cells (“moderate reaction”); and 3+, >50% positive tumor cells (“strong reaction”).
‡Comparison of data between locoregional group and 5-year relapse-free group (P = 0.005) and between locoregional group and group of patients with bone metastases (P = 0.076).
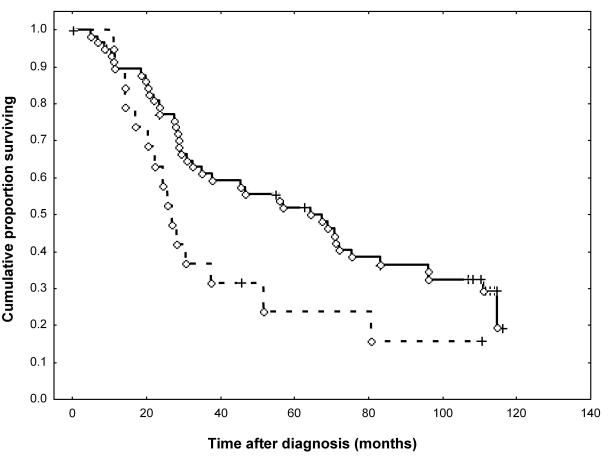
Survival of patients was also analyzed with respect to the expression of MAGE-A4, NY-ESO-1, and HER-2 antigen. It was found that MAGE-A4-positive patients had a significantly better survival than MAGE-A4-negative patients (P = 0.046; Figure 2). In contrast, NY-ESO-1 and HER-2 antigen expression did not correlate with survival (data not shown).
Figure 2.
Overall survival of 81 women with invasive ductal breast cancer according to the MAGE-A4 expression. Full line – MAGE-A4 positive (1+, 2+, 3+) (n = 60); dotted line – MAGE-A4 negative (0) (n = 21); plus sign – censored data; circle – complete data. Gehan’s Wilcoxon test, P = 0.046.
Relation of MAGE-A4 antigen to the standard prognostic and predictive factors
Since the three groups of women with breast cancer significantly differed in MAGE-A4 antigen expression, we analyzed the relationship between MAGE-A4 antigen and standard prognostic and predictive factors (Table 3). MAGE-A4 antigen expression was found to be associated to a significant degree only with the NY-ESO-1 antigen expression (P = 0.006), but not with tumor size and grade, number of metastatically involved axillary lymph nodes, or ER and PR status. Such results suggest that in our patients, MAGE-A4 antigen might have behaved as a prognostic factor unrelated to the above standard prognostic and predictive factors.
Table 3.
Relation of MAGE-A4 expression detected by immunohistochemistry with tumor size, histological grade, axillary lymph node status, estrogen and progesteron receptor positivity, and HER-2 and NY-ESO-1 expression*
| No. of women with breast cancer |
||||
|---|---|---|---|---|
| Characteristics | MAGE-A4 negative (0) | MAGE-A4 positive (1+, 2+, 3+) | total | P† |
| Tumor size (cm): | ||||
| <2 | 8 | 19 | 27 | 0.601 |
| 2-5 | 11 | 38 | 49 | |
| >5 | 2 | 3 | 5 | |
| Histological grade:‡ | ||||
| I | 2 | 6 | 8 | 0.911 |
| II | 13 | 34 | 47 | |
| III | 6 | 20 | 26 | |
| Axillary lymph nodes: | ||||
| negative | 3 | 3 | 6 | 0.369 |
| positive | 18 | 57 | 75 | |
| Estrogen receptors (fmol/mg): | ||||
| <5 | 17 | 36 | 53 | 0.082 |
| ≥5 | 4 | 24 | 28 | |
| Progesterone receptors (fmol/mg): | ||||
| <10 | 10 | 21 | 31 | 0.306 |
| ≥10 | 11 | 39 | 50 | |
| HER-2: | ||||
| negative (0, 1+, 2+) | 19 | 44 | 63 | 0.134 |
| positive (3+) | 2 | 16 | 18 | |
| NY-ESO-1: | ||||
| negative (0) | 18 | 31 | 49 | 0.006 |
| positive (1+, 2+, 3+) | 3 | 29 | 32 | |
*Immunoreactivity for MAGE-A4 and NY.ESO-1 was scored in the following way: 0, no positive tumor cells (negative); 1+, ≤20% positive tumor cells (“mild reaction”); 2+, 21-50% positive tumor cells (“moderate reaction”); and 3+, >50% positive tumor cells (“strong reaction”).
†Pearson χ2 test.
‡Histological grading according to the method by Elston (18).
Discussion
This retrospective study showed that the women with breast cancer who were disease-free for 5 years, those with locoregional relapse of the disease, and those with bone metastases differed in MAGE-A4 expression, but not in NY-ESO-1 and HER-2 expression. The three groups of women were comparable in clinicopathologic parameters, except for ER status and adjuvant systemic cytotoxic therapy. A significantly higher number of women with positive ER in the group of disease-free patients confirmed the positive prognostic and predictive role of ER. On the one hand, a significantly smaller number of women in this group received adjuvant chemotherapy, which was probably caused by higher proportion of ER positive cases, but on the other, there was no difference in adjuvant tamoxifen therapy between the three groups.
The biological course of the disease was probably not much influenced by the adjuvant chemotherapy and hormonal therapy in the women with locoregional relapse and those with bone metastatic disease. There were fewer women with positive MAGE-A4 antigen staining in the group with locoregional relapse than in the 5-year relapse-free group. No association was found between the MAGE-A4 immunohistochemical expression and standard prognostic and predictive markers. However, a link with the NY-ESO-1 immunohistochemical expression was found, which corresponds with previous findings of usually frequent concomitant expression of these two C/T antigens (13,30). Patients with positive and those with negative MAGE-A4 expression significantly differed in survival. Given the prognostic and predictive role of the HER-2 antigen, we would expect a similar difference in survival with respect to its expression (7,8,14), but it was not detected. These results suggest that MAGE-A4, along with traditional prognostic factors, could have a prognostically independent relevance in patients with breast cancer.
Breast cancer biology is complex, with multiple factors contributing to the development and growth of cancer and its metastatic progression. Clinical data from follow-up studies and studies of the biology of breast cancer could be used to identify parameters that could serve as prognostic or predictive factors. Treatment decision making is usually based on a combination of clinical features and tumor characteristics, such as age, tumor size, histological type and grade, lymph node status, and ER and PR status (1-5). However, since the prognostic value of these criteria is variable, it is obvious that additional and still unidentified molecular factors influence and determine the clinical course of breast cancer. By identifying these additional factors, therapeutic approaches to patients with breast cancer could be further individualized, thus increasing both the survival rate and quality of life of the patients. Novel high-performance screening methods, such as the DNA microarray, which can analyze simultaneously the expressions of thousands of genes in a tissue in a single experiment, may allow the identification of disease subsets that correlate with clinical outcomes. Clearly, such gene-expression profiling (holistic approach), although not yet routinely used in clinical practice, would provide highly useful prognostic information (6-11).
Immunohistochemical detection of HER-2 antigen expression was used as the control for detection of MAGE-A4 and NY-ESO-1 expression. HER-2 molecule belongs to a family of four homologous receptors involved in the tyrosine kinase-mediated regulation of normal breast tissue growth and development. Overexpression of HER-2 molecule in breast cancer cells is associated with poor prognosis (7,8,16).
C/T TAA antigens were discovered in the 1990s, initially as targets in CD8 T-cell recognition of autologous human melanoma cells (31). To date, 44 C/T genes have been identified and their expression in numerous cancer types has been studied. The antigen is expressed in normal tissues, but seems to be restricted to testis, fetal ovary, and placenta, and in cancers of diverse origin. Up to 30-40% of many different cancer types, eg, melanoma, bladder cancer, and sarcoma, express one or more C/T antigens. X chromosome codes for the majority of C/T antigens; however, many recently defined C/T coding genes have non-X chromosomal loci. The function of most C/T antigens is unknown, although they seem likely to have some role in regulating gene expression. The global demethylation associated with certain cancers might account for the aberrant C/T expression in cancer. Another important issue is whether the expression of these genes in the cancer cell contributes to its malignant behavior. There is increasing evidence that C/T expression is correlated with tumor progression and takes place in tumors of higher malignant potential (12,13,30).
The expression of C/T genes has mostly been studied on clinical material by use of polymerase chain reaction (PCR). However, PCR cannot show if the analyzed genes are expressed only in low percentage of tumor cells or in most of them. Therefore, clinical immunotherapy studies and trials should be aimed at antigens expressed in most – preferably all – tumor cells. Studies of therapeutic relevance are those where it is possible to quantify tumor cells expressing tumor antigens, such as immunohistochemical studies, which can be performed today because of the development of serological reagents (mAbs) against C/T TAA (13,30).
Expression of MAGE genes in breast cancers was reported by several groups (32-34), as well as particular MAGE-A1, -A2, -A3, -A4, -A6, and -A12 specific transcripts (35), whereas much less has been published on their immunodetection (30). Kavalar et al (28) reported a correlation between mAb 57B staining and the tumor grade, lymphatic vessel invasion, and intratumoral necrosis and an inverse correlation with ER staining.
Since this study was a preliminary investigation, the number of patients was relatively small, which may represent a limitation. Also, a small sample might be a possible reason why we did not observe the influence of HER-2 expression on patients’ survival. Therefore, potential differences in unknown factors in our, relatively small, patient groups may have lead to biased results or conclusions. Accordingly, the observation that the MAGE-A4 antigen has a prognostic role is only an initial hypothesis that should be tested on a much greater number of patients with breast cancer.
Acknowledgment
This work was partially supported by the Ministry of Science and Technology of the Republic of Croatia (grants No. 074001 and 074004 to AJ) and the Swiss National Fund for Scientific Research (grant No. 31-57473.99 to GCS).
References
- 1.Chang JC, Hilsenbeck SG. Prognostic and predictive markers. In: Harris JR, Lippman ME, Morrow M, Osborne CK, editors. Diseases of the breast. 3rd ed. Philadelphia (PA): Lippincott, Williams and Wilkins; 2004. p. 675-96. [Google Scholar]
- 2.Goldhirsch A, Glick JH, Gelber RD, Coates AS, Thurlimann B, Senn HJ. Meeting highlights: international expert consensus on the primary therapy of early breast cancer. Ann Oncol. 2005;16:1569–83. doi: 10.1093/annonc/mdi326. [DOI] [PubMed] [Google Scholar]
- 3.Colozza M, Cardoso F, Sotiriou C, Larsimont D, Piccart MJ. Bringing molecular prognosis and prediction to the clinic. Clin Breast Cancer. 2005;6:61–76. doi: 10.3816/CBC.2005.n.010. [DOI] [PubMed] [Google Scholar]
- 4.Keen JC, Davidson NE. The biology of breast carcinoma. Cancer. 2003;97(suppl 3):825–33. doi: 10.1002/cncr.11126. [DOI] [PubMed] [Google Scholar]
- 5.Cianfrocca M, Goldstein LJ. Prognostic and predictive factors in early-stage breast cancer. Oncologist. 2004;9:606–16. doi: 10.1634/theoncologist.9-6-606. [DOI] [PubMed] [Google Scholar]
- 6.Roukos DH, Pavlidis N, Agnantis NJ. Gene-expression profile: the future in the outcome prediction and treatment of breast cancer. Gastric Breast Cancer. 2003;2:5–8. [Google Scholar]
- 7.Ross JS, Linette GP, Stec J, Clark E, Ayers M, Leschly N, et al. Breast cancer biomarkers and molecular medicine. Expert Rev Mol Diagn. 2003;3:573–85. doi: 10.1586/14737159.3.5.573. [DOI] [PubMed] [Google Scholar]
- 8.Esteva FJ, Hortobagyi GN. Prognostic molecular markers in early breast cancer. Breast Cancer Res. 2004;6:109–18. doi: 10.1186/bcr777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Van de Vijver MJ. Microarray analysis of human breast cancer. In: Harris JR, Lippman ME, Morrow M, Osborne CK, editors. Diseases of the breast. 3rd ed. Philadelphia (PA): Lipponcott Williams and Wilkins; 2004. p. 433-9. [Google Scholar]
- 10.van’t Veer LJ, Paik S, Hayes DF. Gene expression profiling of breast cancer: a new tumor marker. J Clin Oncol. 2005;23:1631–5. doi: 10.1200/JCO.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 11.Sorlie T. Molecular portraits of breast cancer: tumour subtypes as distinct disease entities. Eur J Cancer. 2004;40:2667–75. doi: 10.1016/j.ejca.2004.08.021. [DOI] [PubMed] [Google Scholar]
- 12.Scanlan MJ, Simpson AJ, Old LJ. The cancer/testis genes: review, standardization, and commentary. Cancer Immun. 2004;4:1–15. [PubMed] [Google Scholar]
- 13.Simpson AJ, Caballero OL, Jungbluth A, Chen YT, Old LJ. Cancer/testis antigens, gametogenesis and cancer. Nat Rev Cancer. 2005;5:615–25. doi: 10.1038/nrc1669. [DOI] [PubMed] [Google Scholar]
- 14.Bolli M, Kocher T, Adamina M, Guller U, Dalquen P, Haas P, et al. Tissue microarray evaluation of melanoma antigen E (MAGE) tumor-associated antigen expression: potential indications for specific immunotherapy and prognostic relevance in squamous cell lung carcinoma. Ann Surg. 2002;236:785–93. doi: 10.1097/01.SLA.0000036266.09823.6C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kocher T, Zheng M, Bolli M, Simon R, Forster T, Schultz-Thater E, et al. Prognostic relevance of Mage-A4 tumor antigen expression in transitional cell carcinoma of the urinary bladder: a tissue microarray study. Int J Cancer. 2002;100:702–5. doi: 10.1002/ijc.10540. [DOI] [PubMed] [Google Scholar]
- 16.Ross JS, Fletcher JA, Bloom KJ, Linette GP, Stec J, Symmans WF, et al. Targeted therapy in breast cancer: the HER-2/neu gene and protein. Mol Cell Proteomics. 2004;3:379–98. doi: 10.1074/mcp.R400001-MCP200. [DOI] [PubMed] [Google Scholar]
- 17.Rampaul RS, Pinder SE, Elston CW, Ellis IO. Prognostic and predictive factors in primary breast cancer and their role in patient management: The Nottingham Breast Team. Eur J Surg Oncol. 2001;27:229–38. doi: 10.1053/ejso.2001.1114. [DOI] [PubMed] [Google Scholar]
- 18.Elston CW. Grading of invasive carcinoma of the breast. In: Page DL, Anderson TJ, editors. Diagnostic hystopathology of the breast. Edinburgh: Churchill Livingston; 1987. p. 300-11. [Google Scholar]
- 19 National Cancer Institute. Breast cancer. CancerNet, PDQ - Treatment -Health Professionals, date last modified 18/08/2005. Available at: http://www.nci.nih.gov/ cancer_info/pdq/treatment/breast/health_professional/ Accessed: August 9, 2005.
- 20.Brdar B, Graf D, Padovan R, Nola P, Rudan N, Petrinec Z, et al. Estrogen and progesterone receptors as prognostic factors in breast cancer. Tumori. 1988;74:45–52. doi: 10.1177/030089168807400108. [DOI] [PubMed] [Google Scholar]
- 21.EORTC Breast Cancer Cooperative Group Revision of the standards for the assessment of hormone receptors in human breast cancer. Eur J Cancer. 1980;16:1513–5. doi: 10.1016/0014-2964(80)90064-x. [DOI] [PubMed] [Google Scholar]
- 22.Juretic A, Zivkovic M, Samija M, Bagovic D, Purisic A, Viculin T, et al. Radiotherapy of stage IEA primary breast lymphoma: case report. Croat Med J. 2002;43:569–72. [PubMed] [Google Scholar]
- 23.Jardines L, Haffy BG, Doroshow JH. Stage II breast cancer. In: Pazdur R, Coia L, Hoskins W, editors. Cancer management: a multidisciplinary approach. 8th ed. Melville (NY): PRR; 2004. p. 205-14. [Google Scholar]
- 24.Kocher T, Schultz-Thater E, Gudat F, Schaefer C, Casorati G, Juretic A, et al. Identification and intracellular location of MAGE-3 gene product. Cancer Res. 1995;55:2236–9. [PubMed] [Google Scholar]
- 25.Schultz-Thater E, Noppen C, Gudat F, Dürmüller U, Zajac P, Kocher T, et al. NY-ESO-1 tumour associated antigen is a cytoplasmic protein detectable by specific monoclonal antibodies in cell lines and clinical specimens. Br J Cancer. 2000;83:204–8. doi: 10.1054/bjoc.2000.1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Van Baren N, Brasseur F, Godelaine D, Hames G, Ferrant A, Lehmann F, et al. Genes encoding tumor-specific antigens are expressed in human myeloma cells. Blood. 1999;94:1156–64. [PubMed] [Google Scholar]
- 27.Landry C, Brasseur F, Spagnoli GC, Marbaix E, Boon T, Coulie P, et al. Monoclonal antibody 57B stains tumor tissues that express gene MAGE-A4. Int J Cancer. 2000;86:835–41. doi: 10.1002/(sici)1097-0215(20000615)86:6<835::aid-ijc12>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 28.Kavalar R, Sarcevic B, Spagnoli G, Separovic V, Samija M, Terraciano L, et al. Expression of MAGE tumor associated antigens is inversely correlated with tumor differentiation in invasive ductal breast cancers: an immunohistochemical study. Virchows Arch. 2001;439:127–31. doi: 10.1007/s004280100421. [DOI] [PubMed] [Google Scholar]
- 29.Sarcevic B, Spagnoli GC, Terraciano L, Schultz-Thater E, Heberer M, Gamulin M, et al. Expression of cancer/testis tumor associated antigens in invasive squamous cell cervical carcinoma. Oncology. 2003;64:443–9. doi: 10.1159/000070305. [DOI] [PubMed] [Google Scholar]
- 30.Juretic A, Spagnoli GC, Schultz-Thater E, Sarcevic B. Cancer/testis tumour-associated antigens: immunohistochemical detection with monoclonal antibodies. Lancet Oncol. 2003;4:104–9. doi: 10.1016/s1470-2045(03)00982-3. [DOI] [PubMed] [Google Scholar]
- 31.van der Bruggen P, Traversari C, Chomez P, Lurquin C, De Plaen E, Van den Eynde B, et al. A gene encoding an antigen recognized by cytolytic T lymphocytes on a human melanoma. Science. 1991;254:1643–7. doi: 10.1126/science.1840703. [DOI] [PubMed] [Google Scholar]
- 32.Brasseur F, Marchand M, Vanwijck R, Herin M, Lethe B, Chomez P, et al. Human gene MAGE-1, which codes for a tumor-rejection antigen, is expressed by some breast tumors. Int J Cancer. 1992;52:839–41. doi: 10.1002/ijc.2910520528. [DOI] [PubMed] [Google Scholar]
- 33.Wascher RA, Bostick PJ, Huynh KT, Turner R, Qi K, Giuliano AE, et al. Detection of MAGE-A3 in breast cancer patients’ sentinel lymph nodes. Br J Cancer. 2001;85:1340–6. doi: 10.1054/bjoc.2001.2079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mashino K, Sadanaga N, Tanaka F, Yamaguchi H, Nagashima H, Inoue H, et al. Expression of multiple cancer-testis antigen genes in gastrointestinal and breast carcinomas. Br J Cancer. 2001;85:713–20. doi: 10.1054/bjoc.2001.1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Otte M, Zafrakas M, Riethdorf L, Pichlmeier U, Loning T, Janicke F, et al. MAGE-A gene expression pattern in primary breast cancer. Cancer Res. 2001;61:6682–7. [PubMed] [Google Scholar]