Abstract
Aim
To investigate the relationships between body mass index (BMI), dietary habits, and cardiovascular risk factors in isolated Adriatic island populations of Croatia.
Methods
Random sample of subjects (n = 1001) was interviewed, using a validated questionnaire developed for this research program. Dietary habits were assessed on the basis of applied Food Frequency Questionnaire (FFQ). Biochemical analyses of total cholesterol, high density lipoprotein (HDL), low density lipoprotein (LDL), triglycerides, and blood glucose were performed. Blood pressure (mm Hg), height (m), and weight (kg) were measured following standard procedures.
Results
Out of 1001 study participants, 507 (50.7%) were overweight (247 [48.7%] men and 260 [51.3%] women), whereas 268 (26.8%) were obese (122 [45.5%] men and 146 [54.5%] women). In both genders, there was a positive correlation between body mass index (BMI) and levels of triglycerides (P<0.001), glucose (P<0.001), diastolic blood pressure (P<0.001), and systolic blood pressure (male: P = 0.002, female: P<0.001). Logistic regression showed that female gender (OR, 2.31; 95% CI, 1.61-3.31), overweight (OR, 1.97; 95% CI, 1.34-2.88), obesity (OR, 1.90; 95% CI, 1.22-2.96), more frequent consumption of meat (OR 1.17; 95% CI, 1.06-1.30) and beer (OR 1.14; 95% CI, 1.03-1.27), and less frequent consumption of potatoes (OR 0.91; 95% CI, 0.83-0.99) were predictive for the presence of cardiovascular risk factors.
Conclusion
Prevalence of obesity and related health outcomes was surprisingly high for the studied population. We found a correlation between BMI, dietary habits, and cardiovascular risk factors.
The health of an individual and the population in general is the result of interactions between genetics and a number of environmental factors. An environmental factor of major importance is nutrition (1), which is also one of the key determinants of health care expenditures (2).
Excessive body weight is a major problem in industrialized and developed countries where it has reached the proportions of an epidemic (3). Overweight and obesity have been related to increased morbidity and mortality rates due to diabetes mellitus, several forms of cancer, digestive disease, and coronary heart diseases (4,5).
Furthermore, overweight and obesity are believed to represent an independent risk for cardiovascular diseases. A part of the increased risk of cardiovascular diseases conferred by increased body weight is explained by the effects on blood pressure, glucose tolerance, and plasma lipid metabolism (6,7). Because of the strong relationship between excessive body weight and these diseases, it is important to provide information on the determinants of overweight and obesity from population-based surveys (6,7).
Body mass index (BMI) is an easily and reliably obtained measure of relative body size. It is often used as an indirect index of adiposity and has been strongly associated with cardiovascular disease risk (8).
During the few last years, cardiovascular diseases have caused approximately 4.3 million deaths in Europe and 1.9 million deaths in the European Union (EU) per year, representing 49% of all deaths in Europe and 42% in the EU (9). In Croatia, these diseases also represent a leading cause of mortality and morbidity: the standardized death rate has been increasing for the last three decades, and reached 91.7 per 100 000 population in 2001 (10).
At the same time, in Finland, Sweden, Norway, and Denmark, the mortality rates of standardized deaths rates from coronary heart disease have been declining at all ages over the past decades (11,12). The reasons for the decline are probably healthier lifestyle, reduction of risk factors, and better treatment of diseases. Populations in South European countries, such as France, Spain, and Portugal, have relatively low death rates due to the Mediterranean diet (13).
Studies have suggested that health-conferring benefits of the Mediterranean diet are mainly due to high consumption of fish, fruit, and vegetables. More recent research has focused on other important factors, such as olives and olive oil. Fiber, especially from wholegrain-derived products, fruit, and vegetables, is an important source of dietary antioxidants (14). Furthermore, data suggest that the traditional Mediterranean dietary pattern is inversely associated with body mass index (BMI) and obesity (15).
The aim of the study was to investigate the relationship between BMI and dietary habits and cardiovascular risk factors in isolated Adriatic island populations of Croatia.
Subjects and Methods
Subjects
This study is the part of the “1001 Dalmatians” research program, which was launched with an aim to study isolated populations of Croatian islands (Rab, Vis, Lastovo, and Mljet) that share similar environment and lifestyle (16). A random sample of 1001 adult inhabitants was selected from the total number of inhabitants of these 4 islands. Sampling was based on computerized randomization of the most complete and accessible population registries in each village, which included medical records (Mljet and Lastovo islands), voting lists (Vis island), and household numbers (Rab island). The field work of data gathering was performed during 2002 and 2003 by the team of researchers from the Andrija Štampar School of Public Health, Zagreb University School of Medicine, and the Institute for Anthropological Research in Zagreb, Croatia.
The ethical approval for this research was obtained from the Research Ethics Committee of the Zagreb University School of Medicine, Zagreb, Croatia. Informed written consent was obtained from all participants in the study.
Measures of health-related variables
All of the examinees were first interviewed by one of the trained surveyors, using a validated questionnaire developed specifically for this research program. The details of this program are described elsewhere (17). The questionnaire was designed for collecting extensive information on personal data (name, date and place of birth, gender, marital status, occupation, and various lifestyle variables), health complaints, drug intake, and hospitalization records. It also included Food Frequency Questionnaire (18). The consumption frequency of the selected foodstuffs (dietary habits) was determined on the basis of the reported weekly frequency of intake: 5-7 times a week, 3-4 times a week, 1-2 times a week, or never.
Height and body mass were measured using a single anthropometer (Hospitalija, Zagreb, Croatia). Body mass index was determined as weight divided by height squared (kg/m2). Subjects were classified into three groups, as follows: normal (acceptable) weight, BMI<25; overweight, BMI 25-29.9; obesity, BMI≥30 (3). Since no underweighted persons were identified, there was no need to form this group.
Blood pressure (mm Hg), height (m), and weight (kg) were each measured by a single observer in local health centers and dispensaries between 8 and 11 am, following the standard procedure (19). Blood pressure was measured on the right forearm in sitting position. Two measurements of both systolic and diastolic blood pressure in each individual were taken two times in a 5-minute interval. The mean value obtained from two readings was used in the analysis. Hypertension was defined according to World Health Organization (WHO) criteria as systolic blood pressure ≥140 mm Hg or diastolic blood pressure ≥90 mm Hg (20).
Biochemical analyses of high and low density lipoproteins (HDL and LDL) and total cholesterol, triglycerides, and blood glucose were performed from fasting blood samples taken from the examinees between 7 and 9 am. Plasma and serum were rapidly frozen and stored at -20°C in 200 ml aliquots using standardized sample handling procedures. They were then transported frozen within a maximum of 3 days to the single biochemical laboratory, based in Zagreb. The laboratory was chosen as it has been internationally accredited for performing this type of analysis and included in the internal quality assessment by Roche and Olympus, and in external monitoring programs by Croatian reference center for biochemical measurements and RIQAS international agency for quality control (21).
Statistical analysis
Descriptive statistics were given as median with range, and with absolute and relative frequencies. Kruskal-Wallis test was used for multiple group comparisons (lipids, glucose, and blood pressure values according to BMI groups), with post hoc Mann-Whitney test for significant differences. Correlations of BMI, laboratory findings, and blood pressures were evaluated using Spearman rank correlation coefficients due to non-normal distributions of most values. Differences between qualitatively expressed originally quantitative variables regarding BMI groups were tested with χ2 test. Logistic regression was used to estimate prediction (power) of dietary habits, age, BMI, and gender for presence of cardiovascular risk factors (defined as presence of high cholesterol, and/or high LDL, and/or low HDL levels). Statistical significance of Spearman rank correlation coefficients of biochemical variables, blood pressure, and BMI was used as a criterion for defining the presence of cardiovascular risk. The maximal acceptable significant level was α = 0.05. All statistical procedures were performed using STATISTICA, version 7.1 (StatSoft, Inc., Tulsa, OK, USA).
Results
We examined 454 men (45.4%), with the mean age of 55.0 ± 15.4 years (range 18-87) and 547 women (54.6%), with the mean age of 55.0 ± 14.0 (range 19-88) years. Among them, 247 (54.4%) men and 260 (47.5%) women were overweight and 122 (26.9%) men and 146 (26.7%) women were obese.
In both genders, significant differences were found among normal, overweight, and obese examinees in the levels of triglycerides, glucose, diastolic blood pressure (for both genders P<0.001), total serum cholesterol (men: P = 0.002; women: P = 0.013), and systolic blood pressure (men: P = 0.030; women: P<0.001; Table 1). For LDL levels, the difference between BMI groups was significant in men only (P<0.001).
Table 1.
Cardiovascular risk factors (median, range) by gender and body mass index (BMI) in the population of Croatian Adriatic islands
| BMI groups* |
||||||||
|---|---|---|---|---|---|---|---|---|
| men (n = 454) |
women (n = 547) |
|||||||
| Parameters | normal weight (n = 85) | overweight (n = 247) | obesity (n = 122) | P† | normal weight (n = 141) | overweight (n = 260) | obesity (n = 146) | P† |
| Total cholesterol (<5.2 mmol/L)‡ | 5.2 (3.12–9.78) | 5.9 (3.30–11.41) | 5.4 (3.18–9.99) | 0.002 | 5.7 (2.92–11.72) | 6.2 (3.71–11.75) | 6.2 (3.52–10.44) | 0.013 |
| LDL cholesterol (2.0-3.9 mmol/L)‡ | 3.6 (1.42–8.38) | 4.1 (1.45–8.51) | 3.5 (1.58–7.34) | <0.001 | 4.1 (1.42–9.87) | 4.4 (1.89–9.72) | 4.4 (1.34–7.62) | 0.273 |
| HDL cholesterol (0.9-1.4 mmol/L)‡ | 1.1 (0.59–1.31) | 1.0 (0.50–1.31) | 1.1 (0.55–1.41) | 0.224 | 1.1 (0.77–1.45) | 1.0 (0.62–1.92) | 1.1 (0.51–1.34) | 0.095 |
| Triglycerides (0-1.5 mmol/L)‡ | 1.1 (0.46–7.07) | 1.2 (0.46–10.61) | 1.4 (0.61–11.79) | <0.001 | 1.1 (0.44–3.15) | 1.2 (0.49–4.25) | 1.3 (0.58–5.17) | <0.001 |
| Glucose (4.2-6.4 mmol/L)‡ | 5.3 (3.73–8.58) | 5.4 (3.78–18.15) | 5.8 (4.02–16.24) | <0.001 | 5.2 (3.54–13.58) | 5.4 (3.53–18.68) | 5.6 (3.73–20.86) | <0.001 |
| Systolic pressure (<140mm Hg)‡ | 141.2 (94–200) | 145.6 (100–198) | 147.2 (106–233) | 0.030 | 135.5 (99–218) | 138.6 (97–207) | 149.3 (95–227) | <0.001 |
| Diastolic pressure (<90 mm Hg)‡ | 86.48 (63–123) | 89.7 (55–120) | 92.8 (61–124) | <0.001 | 83.9 (50–121) | 87.3 (55–125) | 91.08 (68–126) | <0.001 |
*Normal weight – BMI<25; over-weight – BMI = 25-29.99; obesity – BMI≥30. There were no underweight persons.
†Kruskal-Wallis test.
‡Laboratory referent values.
Overweight men had significantly higher levels of cholesterol, LDL, triglycerides, glucose, and diastolic pressure than men of normal weight. Obese men had significantly higher levels of cholesterol, triglycerides, glucose, systolic and diastolic pressure than men of normal weight. Obese men had significantly higher levels of triglycerides, glucose, systolic and diastolic pressure, when compared with overweight men.
Overweight women had significantly higher levels of cholesterol, triglycerides, systolic and diastolic pressure than women of normal weight. Obese women had significantly higher levels of cholesterol, triglycerides, glucose, systolic and diastolic pressure compared with women of normal weight. When overweight and obese women were compared, obese women had significantly higher levels of glucose, systolic and diastolic pressure. All other relevant variables showed no significant differences between groups (Table 1).
The differences between BMI groups were also found when values of cardiovascular risk factors were dichotomized according to referent values (Table 2). Abnormal values of all observed risk factors predominated in the overweight group. For all risk factors, the distribution of BMI groups was significant on at least 5% level.
Table 2.
Blood pressure and concentration of lipids and glucose, according to referent values by body mass index (BMI)
| BMI groups* |
|||||
|---|---|---|---|---|---|
| Parameters | normal weight (n = 226) | overweight (n = 507) | obesity (n = 268) | total n = 1001 | P† |
| Total cholesterol (mmol/L): | |||||
| <5.2 | 79 (28.1) | 125 (44.5) | 77 (27.4) | 281 (100.0) | 0.016 |
| ≥5.2 | 147 (20.4) | 382 (53.0) | 191 (26.6) | 720 (100.0) | |
| LDL cholesterol (mmol/L): | |||||
| ≤3.9 | 109 (25.3) | 194 (45.1) | 127 (29.5) | 430 (100.0) | 0.010 |
| >3.9 | 117 (20.5) | 313 (54.8) | 141 (24.7) | 571 (100.0) | |
| HDL cholesterol (mmol/L): | |||||
| ≥0.9 | 203 (24.5) | 410 (49.4) | 217 (26.1) | 830 (100.0) | 0.007 |
| <0.9 | 23 (13.5) | 97 (56.7) | 51 (29.8) | 171 (100.0) | |
| Triglycerides (mmol/L): | |||||
| ≤1.5 | 184 (26.7) | 349 (50.7) | 156 (22.6) | 689 (100.0) | <0.001 |
| >1.5 | 42 (13.5) | 158 (50.6) | 112 (35.9) | 312 (100.0) | |
| Glucose (mmol/L): | |||||
| 4.2-6.4 | 209 (24.3) | 443 (51.5) | 209 (24.3) | 861 (100.0) | <0.001 |
| >6.4 | 17 (12.1) | 64 (45.7) | 59 (42.1) | 140 (100.0) | |
| Systolic pressure (mm Hg): | |||||
| <140 | 122 (27.1) | 234 (52.0) | 94 (20.9) | 450 (100.0) | <0.001 |
| ≥140 | 104 (18.9) | 273 (49.5) | 174 (31.7) | 551 (100.0) | |
| Diastolic pressure (mm Hg): | |||||
| <90 | 157 (28.1) | 283 (50.7) | 118 (21.1) | 558 (100.0) | <0.001 |
| ≥90 | 69 (15.6) | 224 (50.6) | 150 (33.9) | 443 (100.0) | |
*Normal weight – BMI<25; overweight – BMI = 25-29.99; obesity – BMI≥30. There were no underweight persons.
†χ2 test.
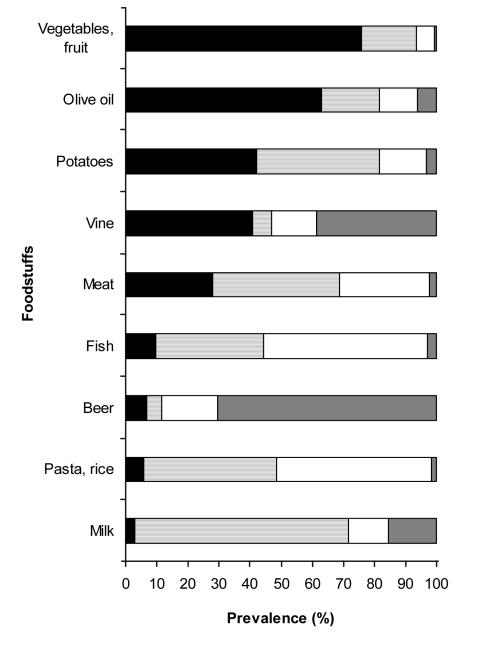
As far as dietary habits are concerned, the majority of participants consumed vegetables and fruit (n = 758; 75.8%), olive oil (n = 638; 63.8%), potatoes (n = 422; 42.2%), and vine (n = 409; 40.9%) frequently, ie, 5 to 7 times a week. Fish was consumed 5 to 7 times a week by 98 (9.8%) subjects and 3 to 4 times a week by 345 (34.5%) subjects. Meat and milk was mostly consumed 3 to 4 times a week. Rice and pasta was mostly consumed 1 to 2 times a week. Beer was consumed 5-7 times a week by 6.9% (n = 69) participants, whereas 70.3% (n = 704) of subjects never drank beer (Figure 1).
Figure 1.
Dietary habits of the population of Croatian Adriatic islands (n=1001), expressed as the frequency of consumption of select foodstuffs, were determined on the basis of reporting the weekly frequency of intake. Closed bar, 5-7 times a week; dark horizontal bar, 3-4 times a week; open bar, 1-2 times a week; gray bar, never.
Due to the fact that triglycerides, glucose, and blood pressure showed highly significant correlation with BMI, they were not included in the definition of “being ill” (presence of cardiovascular risk factors), which was the criterion variable in the logistic regression analysis.
Logistic regression showed that female gender (OR, 2.31; 95% CI, 1.61-3.31), overweight (OR, 1.97; 95% CI, 1.34-2.88), obesity (OR, 1.90; 95% CI, 1.22-2.96), more frequent consumption of meat (OR, 1.17; 95% CI, 1.06-1.30) or beer (OR, 1.14; 95% CI, 1.03-1.27), and less frequent consumption of potatoes (OR = 0.91; 95% CI 0.83-0.99) were predictive for presence of cardiovascular risk factors, defined as high cholesterol, and/or high LDL, and/or low HDL levels (Table 3).
Table 3.
Effects of dietary habits, gender, age, and body mass index (BMI) on presence of risk factors*
| Variable | OR (95% CI) |
|---|---|
| Female gender | 2.31 (1.61-3.31) |
| Overweight | 1.97 (1.34-2.88) |
| Obesity | 1.90 (1.22-2.96) |
| Age | 1.01 (0.99-1.02) |
| Fish | 0.99 (0.88-1.11) |
| Meat | 1.17 (1.06-1.30) |
| Vegetables and fruits | 1.04 (0.99-1.09) |
| Milk | 0.97 (0.92-1.02) |
| Pasta and rice | 0.94 (0.88-1.01) |
| Potatoes | 0.91 (0.83-0.99) |
| Olive oil | 1.06 (0.99-1.14) |
| Vine | 1.02 (0.97-1.08) |
| Beer | 1.14 (1.03-1.27) |
*Logistic regression. Dependent variable included presence of high cholesterol and/or high LDL and/or low HDL levels.
Discussion
Our study demonstrated the correlation between BMI and dietary habits in relation to cardiovascular risk factors. Differences between BMI groups (normal, overweight, and obese) were found for all parameters tested, except HDL values in both genders and LDL values in women. Also, statistically significant differences in the distribution of qualitatively transformed cardiovascular risk factors, regarding referent values between BMI groups were found. Logistic regression showed that female gender, overweight, obesity, and frequent consumption of meat or beer had statistically significant positive predictive value for the classification of “being ill.” On the other hand, frequent consumption of potatoes showed statistically significant protective value for “being ill.”
Female gender, overweight, and obesity had OR between 2.31 to 1.90. There was 17% higher probability to be classified as “ill” for those who frequently consumed meat, whereas there was only 9% smaller probability for “being ill” for frequent potato eaters. Overweight subjects showed pathological values of total cholesterol, LDL, and HDL (53.0%, 54.8%, and 56.7% respectively).
These results are in accordance with the results of other studies, which showed that overweight and obesity are consistent parameters associated with cardiovascular risk in most populations (6,22-25).
Our findings suggest that female gender, overweight, and obesity are predictors of cardiovascular risk, and are very consistent in their relationships. This could partly be related to the age of women. The average age of the surveyed population was 55.0 ± 14.8 (range: 18-88 years), with most of the women aged 50 years and older. This is menopausal age, which includes hormonal deficiency associated with higher level of biochemical parameters, and can contribute to higher cardiovascular risk (26). Also, CRO-CAN study conducted on Croatian population showed that the prevalence of cardiovascular risk factors was generally high, but the hierarchy varied between regions and between sexes (27).
We also wanted to find out whether there was a correlation between cardiovascular risk factors and dietary habits of an isolated island population. Most of the authors analyzed the influence of the Mediterranean diet on the decrease of BMI and thus, indirectly, on cardiovascular risk factors (15,28).
Although the islands and coast are home to more elderly population, the mortality from circulatory diseases is lower. This means that among other factors, the Mediterranean diet plays an important role in preventing atherosclerosis, and decreasing the morbidity and mortality from circulatory diseases in Croatia (29).
As proposed by other authors (15), we expected to confirm the beneficial impact of the Mediterranean diet on cardiovascular status of the surveyed island population. Although the investigated island population showed significant frequency of consuming foodstuffs characteristic for the Mediterranean diet (vegetables and fruit, olive oil, fish, and vine), none of these foodstuffs was found to be a negative predictor for cardiovascular risk. This could suggest that the intake of typical Mediterranean foodstuffs is decreasing, whereas the intake of meat is on the increase. The change in dietary pattern is partly related to the change in lifestyle which occurred due to socioeconomic factors, existing food markets, and the wide range of industrially prepared foodstuffs available. This change has been facilitated by tourism which has substituted agriculture as the main source of income, as well as by better connections with the mainland which enabled better supply with meat and industrially prepared food.
Similar changes were noticed by Ortega et al in the dietary pattern of a Spanish population (30). They reported that in the last few years, changes in lifestyle have triggered a move away from the recommended intakes of several nutrients. The intake of cereals and vegetables has decreased, whereas the intake of fats and animal products has increased.
Our findings are similar to the results of the First Croatian Health survey, conducted 1995-1997. The survey showed that olive oil consumption has decreased due to high market price and low local production, whereas the consumption of red meat has increased. Also, there were no regional differences between continental and coastal region in the consumption of meat and eggs. Obviously, some changes in the structure of diet and dietary habits have occurred over time, making the dietary habits on the islands more similar to the continental diet pattern. The change may have multi factorial etiology such as personal attitudes, change in tradition and economic factors, as well as availability of industrial food products, as opposed to private individual food production (31,32).
Our study showed high prevalence of obesity and cardiovascular risk factors in isolated island populations of the Mediterranean. According to some authors, substantial reassessment of the importance of obesity for cardiovascular disease in most regions of the world is needed (33). Also, in order to obtain better insight into the nutrition quality we recommend a 24-hour recall study in order to provide quantitative data and meal pattern.
Acknowledgments
The study was partially supported by the grants from the Ministry of Science, Education and Sports of the Republic of Croatia No.0108330 and 0108332.
References
- 1.Simopoulos AP. The Mediterranean diets: What is so special about the diet of Greece? The scientific evidence. J Nutr. 2001;131(11 Suppl):3065S–73S. doi: 10.1093/jn/131.11.3065S. [DOI] [PubMed] [Google Scholar]
- 2.Arterburn DE, Maciejewski ML, Tsevat J. Impact of morbid obesity on medical expenditures in adults. Int J Obes (Lond) 2005;29:334–9. doi: 10.1038/sj.ijo.0802896. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Food and health in Europe: a new basis for action WHO. Regional Publications European Series, No 96. Copenhagen: WHO; 2004. [PubMed] [Google Scholar]
- 4.Bellanger TM, Bray GA.Obesity related morbidity and mortality. J La State Med Soc2005157Spec No 1S42–9. [PubMed] [Google Scholar]
- 5.Bener A, Zirie M, Al-Rikabi A. Genetics, obesity, and environmental risk factors associated with type 2 diabetes. Croat Med J. 2005;46:302–7. [PubMed] [Google Scholar]
- 6.Lamon-Fava S, Wilson PW, Schaefer EJ. Impact of body mass index on coronary heart disease risk factors in men and women. The Framingham Offspring Study. Arterioscler Thromb Vasc Biol. 1996;16:1509–15. doi: 10.1161/01.atv.16.12.1509. [DOI] [PubMed] [Google Scholar]
- 7.Schroder H, Marrugat J, Elosua R, Covas MI. Relationship between body mass index, serum cholesterol, leisure-time physical activity, and diet in a Mediterranean Southern-Europe population. Br J Nutr. 2003;90:431–9. doi: 10.1079/bjn2003899. [DOI] [PubMed] [Google Scholar]
- 8.Ferrannini E. Physiological and metabolic consequences of obesity. Metabolism. 1995;44(9) Suppl 3:15–7. doi: 10.1016/0026-0495(95)90313-5. [DOI] [PubMed] [Google Scholar]
- 9.Petersen S, Peto V, Rayner M, Leal J, Luengo Fernandez R, Gray A. European cardiovascular disease statistics 2005. London: British Heart Fundation; 2005. [Google Scholar]
- 10.Kralj V, Hrabak ZV, Erceg M, Tomic B. Cardiovascular diseases in Republic of Croatia [in Croatian]. Zagreb: Croatian National Institute of Public Health; 2004. [Google Scholar]
- 11.Shelley E, Conference Expert Committee. Promoting heart health – a European consensus. Background paper prepared by the Irish Presidency for a meeting in Cork, Ireland, February 2004. Eur J Cardiovasc Prev Rehabil. 2004;11:87–100. doi: 10.1097/01.hjr.0000125756.33795.5f. [DOI] [PubMed] [Google Scholar]
- 12.World Health Organization Regional Office for Europe. European health for all database. Available from: http://www.euro.who.int/hfadb Accessed: June 13, 2005.
- 13.Heim I, Jembrek-Gostovic M, Kern J, Jonke V, Svetina M. Trends in acute myocardial infarction mortality and morbidity from 1979 to 2001 in the City of Zagreb, Croatia. Croat Med J. 2005;46:970–6. [PubMed] [Google Scholar]
- 14.Owen RW, Haubner R, Wurtele G, Hull E, Spiegelhalder B, Bartsch H. Olives and olive oil in cancer prevention. Eur J Cancer Prev. 2004;13:319–26. doi: 10.1097/01.cej.0000130221.19480.7e. [DOI] [PubMed] [Google Scholar]
- 15.Schroder H, Marrugat J, Vila J, Covas IM, Elosua R. Adherence to the traditional Medterranean diet is inversely associated with body mass index and obesity in a Spanish population. J Nutr. 2004;134:3355–61. doi: 10.1093/jn/134.12.3355. [DOI] [PubMed] [Google Scholar]
- 16.Rudan I, Campbell H, Rudan P. Genetic epidemiological studies of eastern Adriatic Island isolates, Croatia: objective and strategies. Coll Antropol. 1999;23:531–46. [PubMed] [Google Scholar]
- 17.Rudan I, Biloglav Z, Vorko-Jovic A, Kujundzic-Tiljak M, Stevanovic R, Ropac D, et al. Effects of inbreeding, endogamy, genetic admixture and outbreeding on human health: “a 1001 Dalmatians” study. Croat Med J. 2006;47:601–10. [PMC free article] [PubMed] [Google Scholar]
- 18.Senta A, Pucarin-Cvetković J, Doko Jelinić J. Quantitative models of foodstuffs and meals [in Croatian]. Zagreb: Medicinska Naklada; 2004. [Google Scholar]
- 19.Weiner JS, Lourie JA, editors. Human biology: a guide to field methods. Oxford (UK): Blackwell Scientific Publications; 1969. [Google Scholar]
- 20.1999 World Health Organization-International Society of Hypertension Guidelines for the Management of Hypertension. Guidelines Subcommittee. J Hypertens. 1999;17:151–83. [PubMed] [Google Scholar]
- 21.Riqas-To-MultiQC. user manual. Available from: http://www.multiqc.com/Riqas2MultiQC.pdf Accessed June 13, 2005.
- 22.Panagiotakos DB, Pitsavos C, Chrysohoou C, Risvas G, Kontogianni MD, Zampelas A, et al. Epidemiology of overweight and obesity in a Greek adult population: the ATTICA Study. Obes Res. 2004;12:1914–20. doi: 10.1038/oby.2004.239. [DOI] [PubMed] [Google Scholar]
- 23.Brown CD, Higgins M, Donato KA, Rohde FC, Garrison R, Obarzanek E, et al. Body mass index and prevalence of hypertension and dyslipidemia. Obes Res. 2000;8:605–19. doi: 10.1038/oby.2000.79. [DOI] [PubMed] [Google Scholar]
- 24.McGee DL. Diverse Population Collaboration. Body mass index and mortality: a meta-analysis based on person-level data from twenty-six observational studies. Ann Epidemiol. 2005;15:87–97. doi: 10.1016/j.annepidem.2004.05.012. [DOI] [PubMed] [Google Scholar]
- 25.Kragelund C, Hassager C, Hildebrandt P, Torp-Pedersen C, Kober L. Impact of obesity on long-term prognosis following acute myocardial infarction. Int J Cardiol. 2005;98:123–31. doi: 10.1016/j.ijcard.2004.03.042. [DOI] [PubMed] [Google Scholar]
- 26.Bjorntorp P. The regulation of adipose tissue distribution in humans. Int J Obes Relat Metab Disord. 1996;20:291–302. [PubMed] [Google Scholar]
- 27.Kern J, Strnad M, Coric T, Vuletic S. Cardiovascular risk factor in Croatia: struggling to provide the evidence for developing policy recommendations. BMJ. 2005;331:208–10. doi: 10.1136/bmj.331.7510.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Garaulet M, Marin C, Perez-Llamas F, Canterasl M, Tebar FJ, Zamora S. Adiposity and dietary intake in cardiovascular risk in an obese population from a Mediterranean area. J Physiol Biochem. 2004;60:39–49. doi: 10.1007/BF03168219. [DOI] [PubMed] [Google Scholar]
- 29.Haim I. Mortality from circulatory diseases in Croatia by districts. In: International conference on Mediterranean diet and health, abstract book; 2002 Sept 12-15; Brijuni, Croatia. Zagreb: Croatian National Institute of Public Health; 2002. p. 18-9. [Google Scholar]
- 30.Ortega RM, Lopez Sobaler AM, Aranceta J, Serra Majem L. Are there any nutritional deficiencies in the Mediterranean diet? Arch Latinoam Nutr. 2004;54(2 Suppl 1):87–91. [in Spanish]. [PubMed] [Google Scholar]
- 31.Kaic-Rak A. Changes in dietary habits in Croatia. In: International conference on Mediterranean diet and health; September 12-15, 2002; Brijuni, Croatia. Zagreb: Hrvatski zavod za javno zdravstvo; 2002. p. 14-5. [Google Scholar]
- 32.Turek S, Rudan I, Smolej-Narancic N, Szirovicza L, Cubrilo-Turek M, Zerjavic-Hrabak V, et al. A large cross-sectional study of health attitudes, knowledge, behaviour and risks in the post-war Croatian population (the First Croatian Health Project). Coll Antropol. 2001;25:77–96. [PubMed] [Google Scholar]
- 33.Yusuf S, Hawken S, Ounpuu S, Bautista L, Franzosi MG, Commerford P, et al. Obesity and the risk of myocardial infarction in 27,000 participants from 52 countries: a case-control study. Lancet. 2005;366:1640–9. doi: 10.1016/S0140-6736(05)67663-5. [DOI] [PubMed] [Google Scholar]