Abstract
Aim
To determine the relationship between the intensity of combat-related posttraumatic stress disorder (PTSD) and the intensity of predominating symptoms.
Method
The study included 151 veterans from 1992-1995 war in Croatia with PTSD, aged 38.3 ± 7.3 years (mean ± standard deviation). The veterans were psychologically tested with the Mississippi Scale for Combat-related PTSD (M-PTSD), Questionnaire on Traumatic Combat and War Experiences (USTBI-M), and Minnesota Multiphasic Personality Inventory-version 201 (MMPI-201).
Results
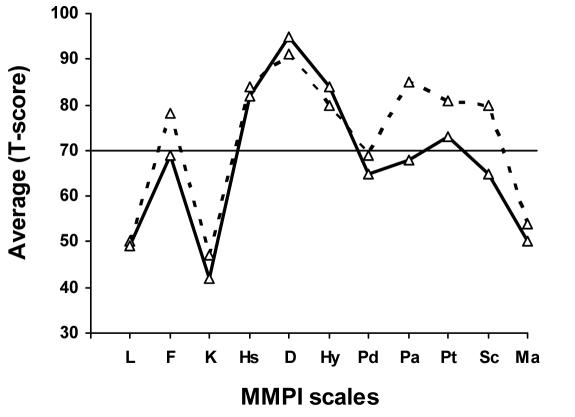
The discriminative analysis of the data revealed that the group with lower PTSD intensity had the highest scores on MMPI scales D (depression, T-score 95.7 ± 5.6), Hs (hypochondriasis, 87.6 ± 5.1), and Hy (hysteria, 85.6 ± 4.9), whereas the group with higher PTSD intensity, besides these three scales (D = 98.3 ± 5.3; Hs = 90.1 ± 4.3; Hy = 89.5 ± 4.7), also had clinically significantly elevated Pt (psychastenia, 80.6 ± 5.6), Sc (schizophrenia, 79.6 ± 4.8), and Pa (paranoia, 85.6 ± 5.4) scales, with the highest Pa scale.
Conclusion
It was possible to differentiate study participants with different PTSD intensity on the basis of their MMPI profile. More intense PTSD was associated with externalized symptoms, such as aggression, acting-out, hostility, and mistrust, whereas less intensive PTSD was associated with mostly depressive symptoms. Our study showed that different intensity of PTSD has different symptom patterns.
A person’s reaction to trauma depends on the traumatic situation itself, personality characteristics of the person exposed to trauma, and posttraumatic social environment. Most people develop some form of acute stress reaction to traumatic event, but in the majority of cases the stress-related difficulties spontaneously withdraw once the person is removed from the situation (1). Fewer people will develop chronic disorders which may evolve into a clinical picture of posttraumatic stress disorder (PTSD) (2). Symptoms that characterize PTSD include repeated re-experiencing of the trauma, emotional numbing, detachment, lack of affect, anhedonia, and avoidance of activities and situations reminiscent of the traumatic event (3).
PTSD is often comorbid with other psychiatric disorders (4-7). Patients with PTSD often complain of psychosomatic disturbances, ranging from anxiety accompanied with tremor and restlessness to depressive problems with predominant cognitive aspects of depression (dark thoughts, shame, guilt, and suicidal thoughts and intentions) and to vegetative symptoms (insomnia and loss of appetite) (8). Comorbidity of PTSD with anxiety or depressive disorders is diagnosed in cases where anxiety or depressive symptoms are prevalent. Due to these psychiatric problems, patients with PTSD often resort to alcohol or drug abuse (4). Memory and concentration impairment, often present in PTSD, may seriously interfere with everyday functioning of these patients (9).
Because PTSD symptoms are so heterogeneous, many researchers presume that there are different subtypes of the disorder. Previous attempts to determine different types of PTSD used different methodologic approaches (10-12). Some studies analyzed characteristics of PTSD with respect to predominant symptomatology (6,8), whereas others tried to associate PTSD symptoms with different types of stressors (12,13). Electrophysiological indicators of PTSD as well as the possibility to determine different types of PTSD on the basis of specific electrophysiological indicators were investigated (14,15).
Further attempts to discern among different types of PTSD were based on personality tests, primarily Minnesota Multiphasic Personality Inventory (MMPI) (16), response to specific pharmacotherapy (17), and existing aggressive behavior (18-20). Recently, intensity of PTSD has been investigated as a factor that determines the type of the disorder (21-23).
The aim of the present study was to determine the relationship between the intensity of PTSD and predominating symptoms in a sample of Croatian 1991-1995 war veterans.
Participants and methods
The study was conducted at the Department of Psychiatry and Department of Psychological Medicine, Zagreb University Hospital Center, from January 2003 to May 2005.
Participants
The study included a convenient sample of patients hospitalized for diagnostic workup and/or therapy either at the Department of Psychiatry or Department of Psychological Medicine, Zagreb University Hospital Center, between January 2003 and May 2005. As a rule, all patients hospitalized at these departments are referred for psychological evaluation, and the present study included only those who met the following inclusion criteria: male sex, combat experience, and diagnosis of PTSD according to the 10th revision of the International Classification of Diseases (ICD-10) (24). The patients who had PTSD comorbid with other psychiatric conditions, neurological disorders, and alcohol or drug abuse were excluded from the study. Thus, out of 217 of eligible patients 151 men were included in the final sample. They all had direct combat experience as members of the Croatian Army during the 1991-1995 war in Croatia. The mean (± standard deviation, SD) age of participants was 38.3 ± 7.3 years. All participants had a status of war veterans and were repeatedly exposed to high intensity stress, which accumulated over the years.
Each participant was psychologically tested and psychiatrically examined by two independent psychiatrists. After the diagnostic workup, the study participants were referred for psychological evaluation consisting of clinical interview followed by psychological testing. The tests were administered in the following order: MMPI-201, M-PTSD, and USTBI-M.
Psychological examination included testing with Mississippi Scale for Combat-related PTSD (M-PTSD) (25) to determine the severity of PTSD symptoms; Questionnaire on Traumatic Combat and War Experiences (USTBI-M) (26) to measure the exposure to stressful events; and Minnesota Multiphasic Personality Inventory-version 201 (MMPI-201) (27) to measure general symptoms.
Study participants were informed on the purpose of the study and all provided their informed consent. The study was approved by the Ethical Committee of the Zagreb University Hospital Center.
Instruments
Mississippi Scale for Combat-related PTSD (M-PTSD) (25) was developed in 1984 and specially designed according to Diagnostic and Statistical Manual (DSM)-III criteria for PTSD. Since then, the instrument has been revised according to the changes in DSM criteria. It consists of 35 statements that are rated on a 5-point Likert scale, ranging from 1 – “absolutely incorrect” to 5 – “absolutely correct”. The result is calculated by adding up the scores for each statement. Thus, a continuous measure of expression of PTSD symptoms is obtained, as opposed to the usual dichotomous results (disorder present or absent) produced by other instruments. The total score may range from 35 to 175 points. The author of the scale recommended ≥107 as the cut-off value for the diagnosis of PTSD (25).
The questionnaire on Traumatic Combat and War Experiences (USTBI-M) was used for the assessment of stressful events and was designed specifically for the war stressors in Croatia (26). It consists of 40 items rated on a 3-point scale (1 – never, 2 – once, 3 – more than once). The result is calculated by adding up the scores for each item, ranging from 40 to 120. This instrument measures combat and traumatic experiences specific for the war in Croatia, such as refuge experience or witnessing destruction of buildings.
Minnesota Multiphasic Personality Inventory (MMPI)-201 is a variant of MMPI standardized to the population of former Yugoslavia (27). It consists of 201 statements, which could be rated as “correct” or “incorrect.” Statements are grouped into 11 scales, and answers may be indicative of one or more of them. Three scales – L, F, and K – are the validity scales that measure the appropriateness and readiness of respondents for this type of testing (response bias): the L scale reflects the rigidity or naiveté in respondents’ approach to the test material; the F scale shows confused thinking, lack of understanding of the material, or malingering; and the K scale reveals a lack of readiness to express one’s own characteristics and a tendency to provide socially acceptable answers. The remaining scales are the clinical scales: Hs (hypochondriasis) scale – narcissism of the body and hypochondriasis; D (depression) scale – depressive symptoms; Hy (hysteria) scale – conversive symptoms; Pd (psychopathic deviation) scale – immaturity, impulsiveness, and asocial behavior; Pa (paranoia) scale – sensitivity, hostility; Pt (psychasthenia) scale – anxiety and obsessive thinking; Sc (schizophrenia) scale – confused and bizarre thinking; and Ma (hypomania) scale – euphoria and hyperactivity.
Given that the scales are psychometrically and phenomenologically interconnected, the interpretation of results is based on a profile configuration rather than on an individual scale result. A general rule is that only the scales with T score ≥70 are interpreted.
Biro and Berger (27) reported that the MMPI-201 had good metric characteristics. Discriminative and predictive power of the items was increased in comparison with the original scale, while the validity of both the bimodal code, when the final result is based on two most prominent scales, and the entire profile is excellent (27).
The results on MMPI-201 were used to determine the predominant symptomatology of PTSD in war veterans.
Statistical analysis
Results are presented as mean ± standard deviation (SD) or median with range. Study participants were divided into two groups according to the PTSD intensity, with the median M-PTSD score as the cut-off value. The MMPI-201 scores in the two groups were compared using the discriminant analysis to determine the differences in the symptom structure. Discriminative analysis reveals the nature and size of the difference between the groups while taking into account the relationship between the investigated variables. Statistical analysis was performed with the Statistical Package for the Social Sciences, version 11.0 (SPSS Inc., Chicago, IL, USA). The level of statistical difference was set at P<.01.
Results
The study participants were exposed to multiple traumatic events and had pronounced symptoms of PTSD. The average MMPI-201 profile of the sample matched most closely the D-Pa (Depression – Paranoia) profile (Table 1).
Table 1.
Scores achieved by 151 Croatian war veterans diagnosed with posttraumatic stress disorder on the Questionnaire on Traumatic Combat and War Experiences (USTBI-M), Mississippi Scale for Combat-Related Post-Traumatic Stress Disorder (M-PTSD), and Minnesota Multiphasic Personality Inventory (MMPI)-201 (presented as T values)
| Questionnaire | Score (mean ± standard deviation) | Cut-off score |
|---|---|---|
| USTBI-M | 77.8 ± 14.3 | Maximum: 120 |
| M-PTSD | 122.1 ± 22.9 | 107 |
| MMPI-201 scales* | ||
| L | 51.1 ± 2.0 | 70 |
| F | 73.2 ± 6.3 | 70 |
| K | 42.4 ± 3.2 | 70 |
| Hs | 87.6 ± 5.1 | 70 |
| D | 96.7 ± 6.6 | 70 |
| Hy | 88.2 ± 4.7 | 70 |
| Pd | 67.3 ± 4.8 | 70 |
| Pa | 79.3 ± 5.8 | 70 |
| Pt | 75.4 ± 5.7 | 70 |
| Sc | 72.1 ± 7.4 | 70 |
| Ma | 52.3 ± 2.6 | 70 |
*Abbreviations: L – rigidity in respondents’ approach to the test material; F – lack of understanding of the material; K – tendency to provide socially acceptable answers; Hs – hypochondriasis; D – depression; Hy – hysteria; Pd – psychopathologic deviation; Pa – paranoia; Pt – psychastenia; Sc – schizophrenia; Ma – hypomania.
We assessed the relationship between PTSD intensity and the predominating symptomatology, which was defined according to the MMPI-201 results. For this purpose, we performed discriminant analysis after dividing the participants into two groups. One group, with less intense PTSD, consisted of veterans who scored below the median M-PTSD score (n = 75) and the other, with more intense PTSD, consisted of those who scored above the median M-PTSD score (n = 76). The median M-PTSD score was 118 (range, 95-170). The groups did not differ in the educational level (χ2 = 0.34; P = 0.234), age (t = 0.47; P = 0.523), or marital status (χ2 = 0.23; P = 0.476). The group with more intense PTSD had significantly higher USTBI-M score than the group with less intense PTSD (80.2 ± 14.1 vs 74.8 ± 12.0, respectively; t = 4.32; P = 0.002).
Discriminant analysis produced a single significant discriminant function, meaning that the two groups of veterans with different PTSD intensity also differed in their MMPI-201 results. The obtained Wilks Λ coefficient, which represents the ratio between the intragroup and total variability of results, was 0.58 (χ2 = 68.25, P<0.001). This indicates that there was a significant difference between the two groups with different PTSD intensity, as determined by MMPI-201. The analysis of the structure of discriminant functions (Table 2) was performed to determine the scales that best differentiated between the two groups.
Table 2.
Structure of discriminant function for Minnesota Multiphasic Personality Inventory (MMPI)-201 scales for Croatian war veterans with less and more intense posttraumatic stress disorder (PTSD) symptoms
| Coefficients |
||
|---|---|---|
| MMPI-201 scales* | standardized discriminant | structure |
| L | 0.12 | -0.13 |
| F | -0.67 | 0.57 |
| K | -0.34 | -0.44 |
| Hs | 0.17 | 0.52 |
| D | 0.16 | 0.85 |
| Hy | 0.30 | 0.53 |
| Pd | 0.23 | 0.40 |
| Pa | 0.34 | 0.73 |
| Pt | 0.35 | 0.78 |
| Sc | 0.51 | 0.71 |
| Ma | -0.24 | -0.21 |
*Abbreviations: L – rigidity in respondents’ approach to the test material; F – lack of understanding of the material; K – tendency to provide socially acceptable answers; Hs – hypochondriasis; D – depression; Hy – hysteria; Pd – psychopathologic deviation; Pa – paranoia; Pt – psychastenia; Sc – schizophrenia; Ma – hypomania.
The position of each group with respect to the obtained function was expressed as a group centroid, which was -0.82 for the group with less intense PTSD and 0.86 for the group with more intense PTSD.
All MMPI scales contributed to the differences between the groups, except the Ma (hypomania) and L (lie) scales. The scales that showed the best correlation with the function were for D (depression, 0.85), Pt (psychasthenia, 0.78), Pa (paranoia, 0.73), and Sc (schizophrenia, 0.71). Comparison of MMPI profiles of the two groups showed that the group with less intense PTSD had a clinically significant “elevation” in D (depression), Hs (hypochondriasis), and Hy (hysteria) scales – the so-called neurotic triad, whereas the group with more intense PTSD, in addition to the elevation in the neurotic triad, also had an “elevation“ in Pt (psychasthenia), Sc (schizophrenia), and Pa (paranoia) scales – the so-called psychotic triad, with Pa scale being the most prominent (Figure 1).
Figure 1.
Average (T-score) Minnesota Multiphasic Personality Inventory (MMPI) profiles of two groups of Croatian war veterans, with less (full line, n = 75) or more (dashed line, n = 76) intense posttraumatic stress disorder (PTSD) symptoms.
A posteriori classification performed on the basis of the discriminant function correctly classified 79.7% of the study participants.
Discussion
Our results showed that different PTSD intensity had different symptom structure. It was possible to differentiate study participants with different PTSD intensity on the basis of their MMPI profile. If only the neurotic triad (elevated D (depression), Hs (hypochondriasis), and Hy (hysteria) scales) was present in the MMPI profile, the participant could be classified into the group with less intense PTSD with 80% probability, assuming that conditions for diagnosis of PTSD were met. On the other hand, if Pa (paranoia), Sc (schizophrenia), Pt (psychasthenia), and F scales were elevated, the participant most probably had a more severe form of PTSD.
According to the MMPI-201 manual (27), the profile of the group with high-intensity disorder points to hypersensitive personalities with frequent interpersonal problems and a tendency to exclude people close to them. They are full of latent aggression, which erupts every once in a while and interferes with social activities and relationships. They are easily offended, prone to paranoid interpretations, and react with depression in stressful situations. Predominant defense mechanism is projection, which they use to overcome the strong feeling of inferiority. To re-establish self-respect, they transfer the blame to others. Psychosomatic reactions are often present, such as diabetes mellitus, allergies, or body weight disorders (27). In contrast, the MMPI profile of the group with less intense PTSD was characterized with elevated D (depression), Hs (hypochondriasis), and Hy (hysteria) scales. Psychosomatic reactions are quite frequent in persons with this profile (27). Their symptoms result from prolonged physiologic reactions that naturally accompany negative emotions, but due to suppression or delayed reaction lead to pathological somatic changes. The organs that are most frequently affected are those controlled by the autonomous nervous system (27).
The main difference between these two types of MMPI profile was in the way how they perceived and reacted to their social environment. Everyday functioning of a person with elevated Pa (paranoia), Sc (schizophrenia), and Pt (psychasthenia) scales is imbued with feelings of injustice, frustrating intolerance, occasional acting-out, and constant transfer of blame for his problems to others – the state, society, and family. In our sample, war veterans with this MMPI profile had more intense PTSD.
Elevation in only D (depression), Hs (hypochondriasis), and Hy (hysteria) scales was characteristic of personalities who did not perceive their environment as threatening but, on the contrary, were quite dependent on people around them. They are self-centered and focused on their feeling of helplessness, depressive mood, tiredness, and neurovegetative dystonia. Predominant mechanisms of defense in these persons are suppression and negation. Low-intensity PTSD is not marked by hostility and distrustfulness.
Our results corresponded with the classification of subtypes of psychopathology into externalizing and internalizing subtypes of combat-related PTSD (28-30). Externalizers often showed aggression and alienation, whereas internalizers more often suffered from depressive disorder (28). It is probably a question of the predisposition either toward externalizing or internalizing psychopathological posttraumatic response. Persons with externalized symptoms have a history of delinquency and substance-related disorders more often than those with internalized symptoms (30). Adolescent behavior disorders have been confirmed as risk factors for PTSD (31). The study conducted by Resnik et al (32) showed a significant association between the exposure to combat-related stress on the one hand and adolescent antisocial behavior on the other with aggressive and asocial behavior in the adult age. Both variables predict asocial behavior.
Part of the differences in the intensity and clinical picture of PTSD could be explained by differences in exposure to stressful events. Although both groups were exposed to traumatic events for a long time, the group with more intense PTSD scored significantly higher on USTBI-M questionnaire.
Our results should be interpreted with caution, because of the possibility that the respondents could have exaggerated their symptoms. The respondent who simulates the symptoms scores high on all questionnaires. In such a case, the result cannot be interpreted as a measure of the intensity of symptoms but only as a response style. However, this limitation is present in all studies which use questionnaires to measure the intensity of a disorder.
In conclusion, our study showed that different intensity of PTSD has different symptom patterns. The group with more intense PTSD symptoms differed in their MMPI-201 profile from the group with less intense PTSD. More intense PTSD was associated with externalized symptoms, such as aggression, acting-out, hostility, and mistrust, whereas less intensive PTSD was associated with mostly depressive symptoms. Future studies investigating the strength of association between the intensity of PTSD in Croatian war veterans on the one hand and early traumatization and adolescent behavior disorders on the other would further contribute to our understanding of heterogeneity of clinical picture of PTSD.
References
- 1.McNally RJ, Bryant RA, Ehlers A. Does early psychological intervention promote recovery from posttraumatic stress? Psychological Science in the Public Interest. 2003;4:45–79. doi: 10.1111/1529-1006.01421. [DOI] [PubMed] [Google Scholar]
- 2.Yehuda R. Risk and resilience in posttraumatic stress disorder. J Clin Psychiatry. 2004;65(Suppl 1):29–36. [PubMed] [Google Scholar]
- 3.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington (DC): APA; 1994. [Google Scholar]
- 4.Kozaric-Kovacic D, Kocijan-Hercigonja D. Assessment of post-traumatic stress disorder and comorbidity. Mil Med. 2001;166:677–80. [PubMed] [Google Scholar]
- 5.Prorokovic A, Cavka M, Cubela Adoric V. Psychosomatic and depressive symptoms in civilians, refugees, and soldiers: 1993-2004 longitudinal study in Croatia. Croat Med J. 2005;46:275–81. [PubMed] [Google Scholar]
- 6.Kozaric-Kovacic D, Hercigonja DK, Grubisic-Ilic M. Posttraumatic stress disorder and depression in soldiers with combat experiences. Croat Med J. 2001;42:165–70. [PubMed] [Google Scholar]
- 7.Calhoun PS, Bosworth HB, Stechuchak KA, Strauss J, Butterfield MI. The impact of posttraumatic stress disorder on quality of life and health service utilization among veterans who have schizophrenia. J Trauma Stress. 2006;19:393–7. doi: 10.1002/jts.20114. [DOI] [PubMed] [Google Scholar]
- 8.Green BL, Krupnick JL, Chung J, Siddique J, Krause ED, Revicki D, et al. Impact of PTSD comorbidity on one-year outcomes in a depression trial. J Clin Psychol. 2006;62:815–35. doi: 10.1002/jclp.20279. [DOI] [PubMed] [Google Scholar]
- 9.Yehuda R, Keefe RS, Harvey PD, Levengood RA, Gerber DK, Geni J, et al. Learning and memory in combat veterans with post-traumatic stress disorder. Am J Psychiatry. 1995;152:137–9. doi: 10.1176/ajp.152.1.137. [DOI] [PubMed] [Google Scholar]
- 10.Breslau N, Reboussin BA, Anthony JC, Storr CL. The structure of posttraumatic stress disorder: latent class analysis in 2 community samples. Arch Gen Psychiatry. 2005;62:1343–51. doi: 10.1001/archpsyc.62.12.1343. [DOI] [PubMed] [Google Scholar]
- 11.Marshall RD, Turner JB, Lewis-Fernandez R, Koenan K, Neria Y, Dohrenwend BP. Symptom patterns associated with chronic PTSD in male veterans: new findings from the National Vietnam Veterans Readjustment Study. J Nerv Ment Dis. 2006;194:275–8. doi: 10.1097/01.nmd.0000207363.25750.56. [DOI] [PubMed] [Google Scholar]
- 12.Kaufman ML, Kimble MO, Kaloupek DG, McTeague LM, Bachrach P, Forti AM, et al. Peritraumatic dissociation and psychological response to trauma-relevant stimuli in Vietnam combat veterans with posttraumatic stress disorder. J Nerv Ment Dis. 2002;190:167–74. doi: 10.1097/00005053-200203000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Henigsberg N, Folnegovic-Smalc V, Moro L. Stressor characteristics and post-traumatic stress disorder symptom dimensions in war victims. Croat Med J. 2001;42:543–50. [PubMed] [Google Scholar]
- 14.Jokic-Begic N, Begic D. Quantitative electroencephalogram (qEEG) in combat veterans with post-traumatic stress disorder (PTSD). Nord J Psychiatry. 2003;57:351–5. doi: 10.1080/08039480310002688. [DOI] [PubMed] [Google Scholar]
- 15.Ehlers CL, Hurst S, Phillips E, Gilder DA, Dixon M, Gross A, et al. Electrophysiological responses to affective stimuli in American Indians experiencing trauma with and without PTSD. Ann N Y Acad Sci. 2006;1071:125–36. doi: 10.1196/annals.1364.011. [DOI] [PubMed] [Google Scholar]
- 16.Glenn DM, Beckham JC, Sampson WS, Feldman ME, Hertzberg MA, Moore SD. MMPI-2 profiles of Gulf and Vietnam combat veterans with chronic posttraumatic stress disorder. J Clin Psychol. 2002;58:371–81. doi: 10.1002/jclp.1149. [DOI] [PubMed] [Google Scholar]
- 17.Pivac N, Kozaric-Kovacic D. Pharmacotherapy of treatment-resistant combat-related posttraumatic stress disorder with psychotic features. Croat Med J. 2006;47:440–51. [PMC free article] [PubMed] [Google Scholar]
- 18.McFall M, Fontana A, Raskind M, Rosenheck R. Analysis of violent behavior in Vietnam combat veteran psychiatric inpatients with posttraumatic stress disorder. J Trauma Stress. 1999;12:501–17. doi: 10.1023/A:1024771121189. [DOI] [PubMed] [Google Scholar]
- 19.Yehuda R. Managing anger and aggression in patients with posttraumatic stress disorder. J Clin Psychiatry. 1999;60(Suppl 15):33–7. [PubMed] [Google Scholar]
- 20.Begic D, Jokic-Begic N. Aggressive behavior in combat veterans with post-traumatic stress disorder. Mil Med. 2001;166:671–6. [PubMed] [Google Scholar]
- 21.Clancy CP, Graybeal A, Tompson WP, Badgett KS, Feldman ME, Calhoun PS, et al. Lifetime trauma exposure in veterans with military-related posttraumatic stress disorder: association with current symptomatology. J Clin Psychiatry. 2006;67:1346–53. doi: 10.4088/jcp.v67n0904. [DOI] [PubMed] [Google Scholar]
- 22.Grieger TA, Cozza SJ, Ursano RJ, Hoge C, Martinez PE, Engel CC, et al. Posttraumatic stress disorder and depression in battle-injured soldiers. Am J Psychiatry. 2006;163:1777–83. doi: 10.1176/ajp.2006.163.10.1777. [DOI] [PubMed] [Google Scholar]
- 23.Elhai JD, Kashdan TB, Snyder JJ, North TC, Heaney CJ, Frueh BC. Symptom severity and lifetime and prospective health service use among military veterans evaluated for PTSD. Depress Anxiety. 2006;25:1–7. doi: 10.1002/da.20188. [DOI] [PubMed] [Google Scholar]
- 24.International statistical classification of diseases and related health problems. 10th revision. Geneva: World Health Organization; 2003. [Google Scholar]
- 25.Keane TM, Caddell JM, Taylor KL. Mississippi Scale for Combat-Related Posttraumatic Stress Disorder: three studies in reliability and validity. J Consult Clin Psychol. 1988;56:85–90. doi: 10.1037//0022-006x.56.1.85. [DOI] [PubMed] [Google Scholar]
- 26.Bunjevac T, Kuterovac-Jagodić G. The questionnaire on traumatic combat and war experiences: psychometric properties and its relationship to PTSD symptoms [in Croatian]. In: Proceedings of the 12th Days of Ramiro Bujas. Department of Psychology, Zagreb, Croatia, December 14-16, 1995. Jastrebarsko: Naklada Slap; 1995. p. 35. [Google Scholar]
- 27.Biro M, Berger J. Manual for modified and standardized MMPI-201 [in Serbian]. Belgrade: Association of Psychologists; 1986. [Google Scholar]
- 28.Miller MW, Greif JL, Smith AA. Multidimensional Personality Questionnaire profiles of veterans with traumatic combat exposure: externalizing and internalizing subtypes. Psychol Assess. 2003;15:205–15. doi: 10.1037/1040-3590.15.2.205. [DOI] [PubMed] [Google Scholar]
- 29.Forbes D, Creamer M, Allen N, Elliott P, McHugh T, Debenham P, et al. MMPI-2 based subgroups of veterans with combat-related PTSD: differential patterns of symptom change after treatment. J Nerv Ment Dis. 2003;191:531–7. doi: 10.1097/01.nmd.0000082181.79051.83. [DOI] [PubMed] [Google Scholar]
- 30.Miller MW, Kaloupek DG, Dillon AL, Keane TM. Externalizing and internalizing subtypes of combat-related PTSD: a replication and extension using PSY-5 scales. J Abnorm Psychol. 2004;113:636–45. doi: 10.1037/0021-843X.113.4.636. [DOI] [PubMed] [Google Scholar]
- 31.Green BL, Grace MC, Lindy JD, Gleser GC, Leonard A. Risk factors for PTSD and other diagnoses in a general sample of Vietnam veterans. Am J Psychiatry. 1990;147:729–33. doi: 10.1176/ajp.147.6.729. [DOI] [PubMed] [Google Scholar]
- 32.Resnick HS, Foy DW, Donahoe CP, Miller EN. Antisocial behavior and post-traumatic stress disorder in Vietnam veterans. J Clin Psychol. 1989;45:860–6. doi: 10.1002/1097-4679(198911)45:6<860::aid-jclp2270450605>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]