Abstract
Study Objective:
Sleep related cognitions (e.g., faulty beliefs and appraisals, unrealistic expectations, perceptual and attention bias) play an important role in perpetuating insomnia. This paper presents new psychometric data on an abbreviated version of the Dysfunctional Beliefs and Attitudes about Sleep Scale (DBAS-16), a 16-item self-report measure designed to evaluate a subset of those sleep related cognitions.
Design:
Psychometric study of a patient-reported measure of sleep related beliefs based on existing clinical and research databases.
Participants:
A total of 283 individuals (60% women; mean age of 46.6 years old) with insomnia, including 124 clinical patients and 159 research participants.
Measurements and Results:
Participants completed the DBAS, Insomnia Severity Index, Beck Depression and Anxiety Inventories, daily sleep diaries for 2 weeks, and 3 nights of polysomnography (research sample only) as part of a baseline assessment. The DBAS-16 was found to be reliable, as evidenced by adequate internal consistency (Cronbach alpha = 0.77 for clinical and 0.79 for research samples) and temporal stability (r = 0.83). The factor structure was similar to the original 30-item version, with 4 factors emerging and reflecting: (a) perceived consequences of insomnia, (b) worry/helplessness about insomnia, (c) sleep expectations, and (d) medication. DBAS total scores were significantly correlated with other self-report measures of insomnia severity, anxiety, and depression, but not with specific sleep parameters.
Conclusion:
The psychometric qualities of this abbreviated DBAS-16 version seem adequate. This patient-reported measure should prove a useful instrument to evaluate the role of sleep related beliefs and attitudes in insomnia and to monitor change on this cognitive variable as a potential moderator of treatment outcome.
Citation:
Morin CM; Vallières A; Ivers H. Dysfunctional Beliefs and Attitudes about Sleep (DBAS): Validation of a Brief Version (DBAS-16). SLEEP 2007;30(11):1547-1554.
Keywords: Insomnia, assessment, beliefs, attitudes, sleep, measure, evaluation
INTRODUCTION
CLINICAL AND RESEARCH EVIDENCE SUGGEST THAT SLEEP RELATED COGNITIONS SUCH AS FAULTY BELIEFS, WORRY, AND ATTENTIONAL BIAS PLAY AN important mediating role in perpetuating or even exacerbating insomnia.1–4 For instance, some insomnia sufferers tend to hold unrealistic expectations about their sleep requirements and to worry excessively when such requirements are not met. Others fear the potential consequences of insomnia on their daytime functioning and tend to selectively channel their attention on any evidence of such consequences. In turn, such faulty expectations, perceptions, and excessive worry are instrumental in producing emotional distress, heightening arousal, and in feeding on the vicious cycle of insomnia.5
Recognizing the potential role of sleep-disruptive cognitions in insomnia, an increasing number of investigators and clinicians are incorporating cognitive therapy as a therapeutic component of psychological interventions for insomnia.6 Although the unique contribution of cognitive therapy to treatment outcome has not been assessed yet, recent clinical trials have shown that these therapeutic targets, including faulty beliefs and attitudes about sleep, are responsive to treatment and may actually play an important mediating role in reducing insomnia symptoms and in maintaining sleep improvements over time.7–9
Despite increasing recognition of the importance of cognitive factors in the etiology of insomnia, there are few instruments specifically designed to identify and evaluate patient-specific sleep related cognitions relevant for therapy. The development of reliable and valid measures is both timely and relevant given the increasing attention devoted to insomnia in general10,11 and, more specifically to sleep cognitions as a mediating factor and a treatment target. The Dysfunctional Beliefs and Attitudes about Sleep Scale4,12 was developed to evaluate such sleep-disruptive cognitions. The original DBAS version included 30 items that were rated on 100-mm visual analog scales. This instrument has been translated into several languages (e.g., French, Italian, German, Japanese, Swedish) and is increasingly used by clinicians and researchers throughout the world.13–20 The DBAS has been found reliable for discriminating between self-defined good and poor sleepers in both younger and older adults.2,21,22 It has also been shown sensitive to several indices of changes with insomnia treatment.7–9,21 To encourage a more widespread use of the DBAS among the sleep community, we examined the psychometric properties of an abbreviated version (16 items) using a more user-friendly response format (0-10, Likert-type scale).
METHOD
Participants
There were a total of 283 participants including 124 clinical patients evaluated/treated for insomnia at a private behavioral sleep medicine clinic (clinical sample) and 159 research participants enrolled in insomnia treatment studies (research sample). All participants had a primary complaint of insomnia; research participants met DSM-IV criteria for chronic primary insomnia,23 whereas clinical patients could present primary insomnia or insomnia comorbid with another medical or psychiatric disorder (mostly anxiety and depression). Participants from the research sample but not the clinical sample had to be free of any sleep or other psychotropic medication interfering with sleep at least one month prior to treatment. Additional exclusion criteria for the research sample were the presence of another sleep disorder (e.g., sleep apnea, restless legs syndrome/periodic limb movements during sleep), presence of a major psychiatric disorder (e.g., major affective disorder, psychosis), evidence that insomnia was related to a medical condition, and currently in psychotherapy.
Sample
The total sample (N = 283) was composed predominantly of women (59.5%); the average age was 46.6 years old (SD = 10.4, range 20 to 71 years old), and the mean number of years of education was 14.9 years (SD = 3.7). The average insomnia duration was 14.3 years (SD = 12.5) with a mean age of insomnia onset at 32.5 years old (SD = 13.1). Overall, 7.6% presented sleep-onset insomnia, 20.0% sleep-maintenance insomnia, 1.4% terminal insomnia, and 71.0% mixed sleep onset and maintenance insomnia. Comparisons between clinical and research samples yielded some significant differences. Specifically, clinical participants were younger (M = 42.0 years) than research participants (M = 47.3), t266 = −4.16, P < 0.001, they were more likely to report sleep-onset insomnia (18.5% vs. 2.8% for research sample) but less likely to report sleep-maintenance insomnia (12.3% vs. 23.5% for research sample), χ2(3, N = 210) = 17.46, P <0.001, and their average insomnia duration was shorter (10.0 years) compared to that of the research sample (13.9 years), t262 = −2.62, P = 0.009. There were also more clinical than research patients with a current psychiatric disorder (29.3% vs. 15%, χ2(1, N = 266) = 7.89, P <0.005) and using hypnotic medications either currently or in the past year (67% vs. 39.9%, χ2(1, N = 264) =18.65, P <0.001). No significant difference was found on gender, education, and age at insomnia onset.
Procedure
All participants completed the DBAS, with several other self-report measures, as part of a baseline assessment. In addition, they underwent a clinical evaluation including a semi-structured sleep history interview to diagnose insomnia4 and the Structured Clinical Interview for DSM-IV24 (research sample only) to evaluate the presence of psychiatric disorders. A medical history and physical examination was conducted for research participants. All participants kept daily sleep diaries for ≥ 2 weeks. Seventy-three participants from the research sample completed the DBAS a second time, approximately 2 weeks after the first completion, to assess temporal stability.
Measures
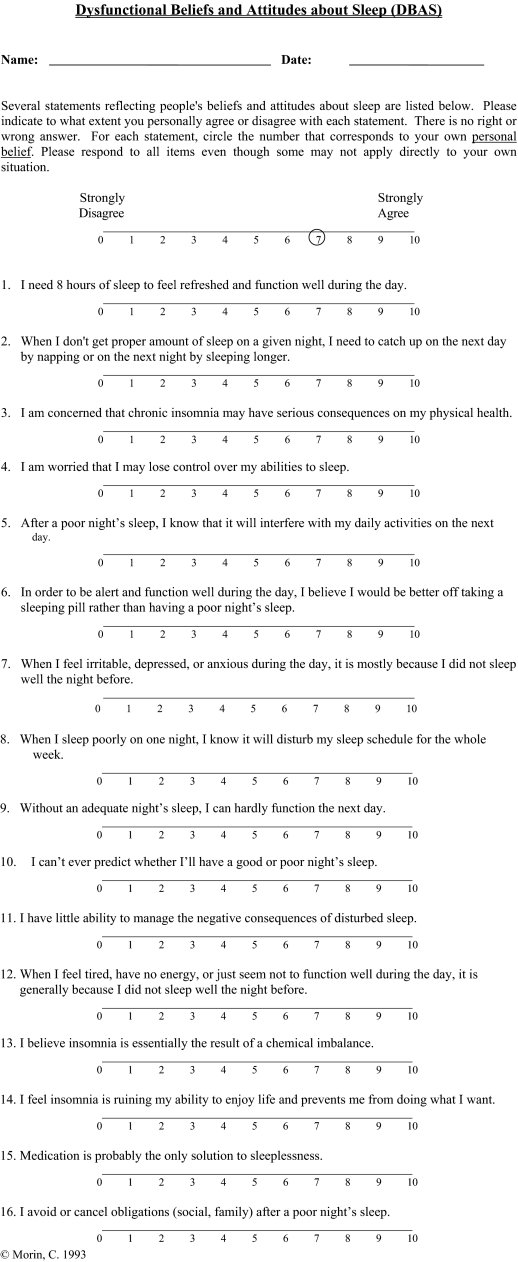
Dysfunctional Beliefs and Attitudes about Sleep Scale
The original DBAS4 is a 30-item self-report questionnaire designed to identify and assess various sleep/insomnia-related cognitions (e.g., beliefs, attitudes, expectations, appraisals, attributions). The initial pool of items was derived from clinical experience with insomnia patients and from psychological conceptualizations of insomnia. They were selected to sample a broad domain of beliefs, thoughts, appraisals, and concerns expressed by patients with insomnia. The nature of these beliefs clustered around 5 conceptually derived themes: (a) misconceptions about the causes of insomnia (e.g., “I believe insomnia is essentially the result of a chemical imbalance”); (b) misattribution or amplification of its consequences (e.g., “I am concerned that chronic insomnia may have serious consequences on my physical health”); (c) unrealistic sleep expectations (e.g., “I must get 8 hours of sleep to feel refreshed and function well the next day”); (d) diminished perception of control and predictability of sleep (e.g., “When I sleep poorly on one night, I know it will disturb my sleep schedule for the whole week”); and (e) faulty beliefs about sleep-promoting practices (e.g., “When I have trouble sleeping, I should stay in bed and try harder”). Earlier validation of the 30-item version showed adequate psychometric properties as evidenced by good internal consistency (Cronbach Alpha = 0.80), moderate item-total correlations (mean rs = 0.37), and adequate convergent and discriminant validity.12,14,22 Additional psychometric data on the original 30-item version, or of altered versions, have also been reported by other investigators.7,15,21
Scoring and Interpretation Guidelines
For each statement, the person rates his or her level of agreement/disagreement on a 100-mm visual analog scale anchored at one end by “strongly disagree” and at the other by “strongly agree.” In order to facilitate scoring of the instrument, the response format was altered during the course of data collection with the research sample from a visual analog scale (i.e., straight 100 mm line) to a Likert-type scale requiring participants to circle a number from 0 (strongly disagree) to 10 (strongly agree) with the same continuous 100-mm line in the background. The visual analogue scale version was completed by 52 participants and the Likert scale version was completed by 107 participants.
Although there is no absolute right or wrong answer for any single item, their dysfunctional nature is reflected by the degree with which patients endorse a particular item. For example, the belief that 8 hours of sleep is needed to function adequately during the day may be valid for most people, yet too strong an endorsement of this statement could potentially trigger some worry and concern when such requirement is not met and contribute to perpetuate insomnia. Thus, the results are quantified in terms of strength of endorsed beliefs. Except for item 23 (on the 30-item version) for which the score is reversed, a higher score indicates more dysfunctional beliefs and attitudes about sleep. The total score is based on the average score of all items. Subscale scores can be computed by adding the sum of scores for the items and dividing by the number of items making up each subscale. The same scoring procedure is recommended for the revised 16-item version, i.e., adding scores for all 16 items and dividing by 16 for an average total score.
Sleep Measures
Participants completed daily sleep diaries during 2 weeks as part of their baseline assessments before initiating treatment. Sleep variables derived from the diary included Sleep-Onset Latency (SOL), Wake after Sleep Onset (WASO; time awake from initial sleep onset to last awakening), Total Wake Time (TWT; SOL+WASO+last awakening before arising), Total Sleep Time (TST), and Sleep Efficiency (SE; ratio of total sleep time divided by time spent in bed and multiplied by 100). Sleep variables were coded each night and weekly means were computed. Research participants completed 3 nights of polysomnographic (PSG) recording as part of their baseline evaluation. Means from the second and third night of recordings were used for the present analyses.
Additional measures
Several additional patient-reported measures were used to examine convergent and discriminant validity. The Insomnia Severity Index4 is a 7-item scale evaluating the perceived insomnia severity. Ratings on a 0 to 4 point scale were obtained on the perceived severity of sleep-onset, sleep-maintenance, early morning awakening problems; satisfaction with current sleep pattern; interference with daily functioning, noticeably of impairment attributed to the sleep problem; and level of distress caused by the sleep problem. The total score ranges from 0 to 28, and higher scores indicate more severe insomnia. The ISI has adequate psychometric properties and has been shown to be sensitive to changes in clinical trials of insomnia.14,25,26 The Beck Depression Inventory27 and the Beck Anxiety Inventory28 were also administered to assess depression and anxiety symptoms. Psychometric properties of those questionnaires are well documented.
RESULTS
Analyses of the Original 30 Items of the DBAS
Several analyses were computed on the original 30 items to guide the decision-making process in reducing the number of items for the final abbreviated scale. In addition to examining internal consistency of the original items, those analyses sought to identify items that were sensitive to floor effect (i.e., low mean and low variance) and items with high rate of missing data. The objective was to reduce the scale to about 16 items (i.e., half of the original scale length) without compromising its psychometric properties or the scope of the sampled domains.
Descriptive statistics (means, standard deviations, range of scores), for the 30 original items are presented in Table 1. These data show that 3 items, 14 (insomnia as the result of aging), 15 (afraid of dying in sleep) and 26 (alcohol as a solution), exhibited low mean and variance, suggesting the presence of a floor effect (i.e., low sensitivity to individual differences). In addition, item 13 (should sleep as well as bed partner) was not answered by 5% of participants, probably those who did not have a bed partner. Item 2 (need less sleep because of aging) had a low item-total correlation and did not appear to contribute significantly to the total score, possibly because it was not as meaningful to younger as to older adults. Despite some relatively good psychometric properties, some items were also not retained in order to minimize redundancy within a given domain (e.g., consequences of insomnia) sampled by the scale.
Table 1.
Descriptive Statistics for the Original 30 Items of the DBAS (N = 159).
| Item | Mean (SD) | Range of scores (min – max) | Missing (%) |
|---|---|---|---|
| 1. Need 8 hours of sleep | 5.62 (2.86) | 0 - 10 | 0.6 |
| 2. Need to catch up on sleep loss | 5.37 (3.00) | 0 - 10 | 1.3 |
| 3. Need less sleep because getting older | 4.48 (2.75) | 0 - 10 | 0.6 |
| 4. Worried about nervous breakdown | 4.30 (2.89) | 0 - 10 | 0.0 |
| 5. Consequences of insomnia on health | 7.48 (2.31) | 0 - 10 | 0.0 |
| 6. More time in bed insures more sleep | 3.83 (2.68) | 0 - 10 | 0.0 |
| 7. Trying harder will lead to sleep | 4.47 (2.68) | 0 - 10 | 0.0 |
| 8. Fear of losing control of sleep | 6.56 (2.48) | 0 - 10 | 0.0 |
| 9. Should go to bed earlier because of aging | 3.00 (2.30) | 0 - 10 | 0.6 |
| 10. Insomnia interferes with daytime functioning | 6.51 (2.69) | 0 - 10 | 0.0 |
| 11. Better taking sleeping pills | 4.15 (3.16) | 0 - 10 | 0.0 |
| 12. Mood disturbances due to insomnia | 6.61 (2.57) | 0 - 10 | 0.0 |
| 13. Should sleep as well as bed partner | 4.59 (3.05) | 0 - 10 | 5.0 |
| 14. Insomnia as the result of aging | 1.90 (1.90) | 0 - 9.5 | 0.0 |
| 15. Afraid of dying in sleep | 1.27 (2.24) | 0 - 10 | 0.0 |
| 16. Will have to pay after a good night | 2.86 (2.72) | 0 - 10 | 0.0 |
| 17. One poor night disturbs whole week | 2.86 (2.57) | 0 - 10 | 0.0 |
| 18. Cannot function without a good night | 3.59 (2.33) | 0 - 10 | 0.0 |
| 19. Sleep is unpredictable | 7.34 (2.70) | 0 - 10 | 0.0 |
| 20. Unable to manage consequences | 5.80 (2.69) | 0 - 10 | 0.6 |
| 21. Lack of energy due to poor sleep | 7.20 (2.44) | 0 - 10 | 0.0 |
| 22. No control over nocturnal thoughts | 6.70 (2.94) | 0 - 10 | 0.0 |
| 23. Can still lead satisfactory life | 3.86 (2.40) | 0 - 10 | 0.0 |
| 24. Insomnia resulting from chemical imbalance | 3.72 (2.52) | 0 - 8.5 | 1.3 |
| 25. Insomnia destroying life | 5.75 (2.89) | 0 - 10 | 0.0 |
| 26. Alcohol as a solution | 1.41 (1.76) | 0 - 10 | 0.0 |
| 27. Medication as a solution | 2.60 (2.62) | 0 - 10 | 0.0 |
| 28. Sleep is getting worst all the time | 2.94 (2.49) | 0 - 10 | 0.6 |
| 29. Shows in physical appearance | 5.42 (2.94) | 0 - 10 | 0.6 |
| 30. Cancel obligations | 2.87 (2.56) | 0 - 10 | 0.0 |
Additional analyses were performed to compare the 2 response formats, the original visual analog scale (VAS) and the Likert scale versions. A one-way MANOVA revealed a significant difference between the two versions, F30,110 = 2.45, P = 0.0004. However, systematic examination of individual items revealed that about half (13 out of 30) of the items were endorsed more strongly on the VAS scale, whereas a reverse trend was observed (higher mean on the Likert scale version) for the remaining 17 items. Hence, a series of independent t-tests identified only 3 out of 30 significant differences (items #7, 21, and 25) and these differences were no longer significant when applying a Bonferroni correction for alpha error inflation. These results suggest that, while some differences may emerge between the 2 response formats, this effect does not favor systematically one version over the other. Thus, all subsequent analyses were completed with both versions pooled together.
Item Selection of the Brief DBAS
Several psychometric criteria were used to select the final items to be retained in the abbreviated version of the DBAS. For each individual item, the following criteria were considered: (a) normal distribution, (b) moderate variance, (c) moderate endorsement (no low or high mean), (d) use of the entire range of response choice (from 0 to 10), (e) low rate of missing data, (f) adequate item-total correlation on exploratory internal consistency analysis, and (g) associated with only one factor on an exploratory oblique factor analysis (not reported here). Clinical relevance and usefulness of the items, and some balance of the number of items representative of each conceptual domain were also taken into consideration in deriving the final scale. Based on these criteria, 16 items were selected and submitted to further psychometric analyses (See Appendix A).
Internal Consistency of the DBAS-16
Internal consistency of the DBAS-16 was examined through computation of Cronbach alpha coefficients and item-total correlations. Those results are presented in Table 2, separately for the clinical and research samples. Cronbach alpha values of 0.77 (clinical) and 0.79 (research) indicate adequate internal consistency. Item-total correlations ranged from 0.06 to 0.64 (M = 0.39) for the research sample, and from 0.09 to 0.59 (M = 0.36) for the clinical sample. Two items (19, sleep is unpredictable; and 24, insomnia resulting from chemical imbalance) showed low item-total correlations, a finding not unexpected as both items were retained mainly because of their content validity and clinical relevance to insomnia. Indeed, despite individual differences in anxiety proneness and causal attributions of insomnia, such expectation (sleep is unpredictable) and attribution (insomnia resulting from chemical imbalance) are reported by a subgroup of individuals with insomnia and can be useful for treatment planning. Overall, data about internal consistency were very similar for both research and clinical samples.
Table 2.
Item-Total Correlations and Cronbach Alpha for the DBAS-16.
| Item | Research sample (n = 153) | Clinical sample (n = 113) |
|---|---|---|
| 1. Need 8 hours of sleep | 0.29 | 0.24 |
| 2. Need to catch up on sleep loss | 0.45 | 0.48 |
| 5. Consequences of insomnia on health | 0.44 | 0.25 |
| 8. Worried about losing control of sleep | 0.40 | 0.33 |
| 10. Insomnia interferes with daytime functioning | 0.57 | 0.55 |
| 11. Better taking sleeping pills | 0.47 | 0.30 |
| 12. Mood disturbances due to insomnia | 0.58 | 0.38 |
| 17. One poor night disturbs whole week | 0.47 | 0.46 |
| 18. Cannot function without a good night | 0.64 | 0.52 |
| 19. Sleep is unpredictable | 0.06 | 0.09 |
| 20. Unable to manage consequences | 0.24 | 0.42 |
| 21. Lack of energy due to poor sleep | 0.48 | 0.29 |
| 24. Insomnia resulting from chemical imbalance | 0.13 | 0.19 |
| 25. Insomnia destroying life | 0.46 | 0.59 |
| 27. Medication as a solution | 0.25 | 0.30 |
| 30. Cancel obligations |
0.36 |
0.42 |
| Mean (range) of item-total correlations | 0.39 (0.06 – 0.64) | 0.36 (0.09 – 0.59) |
| Cronbach alpha | 0.79 | 0.77 |
Temporal stability of the DBAS-16
Seventy-three participants of the research sample completed the DBAS-16 twice, with a 2-week interval between administrations. A Pearson correlation coefficient computed between the total scores showed a significant correlation, r(72) = 0.83, P <0.0001, suggesting adequate temporal stability. A paired t-test revealed that the total score of the DBAS-16 decreased significantly from the first (mean = 4.95, SD = 1.35) to the second (mean = 4.57, SD = 1.48) administration. The reduction of 0.38 (95% CI = 0.18 to 0.57) suggests a possible “regression toward the mean.”
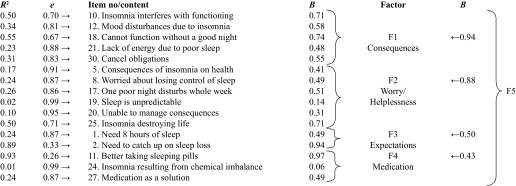
Confirmatory Factor Analysis of the DBAS-16
To investigate whether empirical data from the abbreviated DBAS fits the expected factor structure, the 16 items were submitted to a second-order confirmatory factor analysis (CFA) using a structural equation model analysis. A 4-factor structure was postulated according to our previous work22 and the new data presented in preceding sections. These 4 factors were: (a) consequences of insomnia, (b) worry about sleep, (c) sleep expectations and (d) medication. The CFA model included the 16 items (i.e., manifest variables), 4 factors and a second-order general factor (5 latent variables), yielding about 38 relationships to be estimated (see Table 3). However, because the research sample alone was too small (n = 159) for the specified model (i.e., the number of observations per estimated parameter was <5),29 data from both the clinical and research samples were combined for this analysis. Table 3 presents the results of the confirmatory factor analysis for the total sample (N = 266, excluding 17 observations with some missing values).
Table 3.
Confirmatory factor analysis of the DBAS-16 (clinical and research samples).
Note. B are standardized estimates for the second-order confirmatory factor analysis. Although not displayed here, 2 relationships were set between errors of items 5 and 8 (r = 0.27) and errors of items 12 and 21 (r = 0.21).
The CFA model was estimated by maximum likelihood using PROC CALIS30 on the raw variance/covariance matrix. Lagrange tests, used to test for missing relationships, indicated the need to add 2 correlations, one between errors of items 5 and 8, and the other between errors of items 12 and 21, suggesting that the contents (face validity) of both pair of items were clearly related. The final results revealed a good fit between the expected theoretical 4-factor structure and the empirical data. Various standard CFA indices supported this conclusion. Specifically, the Adjusted Goodness of Fit Index (AGFI) was 0.891, suggesting that about 90% of the covariance of items (relationships between all items) could be explained by the theoretical factor structure. Residual indices, which indicated the amount of residual error, were also adequate, Root Mean Square Residual (RMR) = 0.060 and Root Mean Square Error of Approximation (RMSEA) = 0.059. Finally, the Bentler's Comparative Fit Index (CFI) was 0.897, which also revealed a good fit between the observed data and the theoretical factor structure. Taken together, these results generally support the conceptualization of the abbreviated DBAS-16 as a 4-factor measure.
Convergent and discriminant validity of the revised DBAS
To further investigate its convergent and discriminant validity, the DBAS-16 total score and the 4 DBAS subscales scores were correlated with selected demographic, clinical, and sleep parameters (diary and PSG) (see Table 4).
Table 4.
Convergent and Discriminant Validity of the DBAS-16.
| Total | Consequences | Worry | Sleep Expectations | Medication | |
|---|---|---|---|---|---|
| Demographics | |||||
| Age (yr) | −0.12* | −0.20** | −0.07 | −0.02 | 0.09 |
| Education (yr) | −0.20* | −0.14 | −0.04 | −0.14 | −0.27*** |
| Clinical | |||||
| BAI | 0.41*** | 0.41*** | 0.22** | 0.16* | 0.22** |
| BDI | 0.42*** | 0.37*** | 0.30*** | 0.19** | 0.26*** |
| Sleep | |||||
| Insomnia duration (yrs) | −0.07 | −0.02 | −0.07 | −0.13* | −0.01 |
| Age at onset | −0.07 | −0.17* | −0.05 | 0.08 | 0.11 |
| ISI (patient) | 0.45*** | 0.49*** | 0.29** | 0.09 | 0.21** |
| ISI (clinician)a | 0.33*** | 0.36*** | 0.20* | 0.12 | 0.14 |
| Diary | |||||
| Sleep onset latency | 0.14 | 0.13 | 0.03 | −0.02 | 0.20** |
| Wake after sleep onset | 0.03 | 0.03 | 0.01 | 0.02 | 0.01 |
| Total wake time | 0.18* | 0.18* | 0.10 | 0.01 | 0.15* |
| Time in bed | 0.34*** | 0.28*** | 0.13 | 0.41*** | 0.18* |
| Total sleep time | 0.02 | −0.02 | −0.01 | 0.17* | −0.03 |
| Sleep efficiency | −0.12 | −0.14* | −0.06 | 0.07 | −0.13 |
| Polysomnographya | |||||
| Sleep onset latency | 0.02 | 0.09 | −0.11 | 0.04 | −0.05 |
| Wake after sleep onset | 0.02 | 0.00 | −0.02 | 0.07 | 0.02 |
| Total wake time | 0.02 | 0.05 | −0.09 | 0.09 | −0.01 |
| Time in bed | 0.20* | 0.17* | 0.08 | 0.20* | 0.10 |
| Total sleep time | 0.14 | 0.10 | 0.15 | 0.07 | 0.10 |
| Sleep efficiency | 0.02 | −0.01 | 0.11 | −0.05 | 0.03 |
Note. BAI = Beck anxiety inventory, BDI = Beck depression inventory;
* P < 0.05, ** P < 0.01, *** P < 0.001.
Data only available for the research sample
These analyses revealed significant but modest negative relationships with demographic variables such as age (r with total score = −0.12) and gender (r = −0.20). Education level was negatively related to attributions of insomnia to physical/medical causes; participants with lower education levels tended to endorse more strongly the idea that insomnia was caused by physical factors. Depressive (BDI) and anxious symptoms (BAI) were significantly associated (rs from 0.28 to 0.50) with stronger endorsements of beliefs about insomnia consequences, worry about sleep and medication, but not with sleep expectations. Total score from the Insomnia Severity Index (ISI) was strongly associated with the total DBAS score, as well as with insomnia consequence subscale score. Diary and PSG sleep/wake variables did not correlate significantly with dysfunctional beliefs subscales, except for total time in bed, which was significantly related to 2 subscales, insomnia consequences and sleep expectations. This latter result suggests that participants who spend more time in bed tend to have more erroneous expectations about their sleep.
DISCUSSION
The findings obtained from both clinical and research samples of individuals with insomnia provide evidence of the reliability and validity of an abbreviated version of the Dysfunctional Beliefs and Attitudes about Sleep scale (DBAS-16). This self-report questionnaire (see page 1554) was found to have adequate internal consistency and temporal stability, to show acceptable convergent validity with conceptually-related measures, and to present adequate construct validity as evidenced by a factor structure consistent with current psychological conceptualizations of insomnia. The revised Likert-type response format produced equivalent responses to the original visual-analog scales. These findings support the utility of the DBAS-16 in both insomnia research and clinical practice.
The 16 items retained on this abbreviated version sample a broad range of themes that are often of concern to individuals with insomnia and that may be clinically relevant for therapy. These domains include expectations about sleep requirements, attributions of the causes and appraisals of the consequences of insomnia, and issues of worry and helplessness about insomnia. There is also one factor concerned with sleep medication and biological attribution of insomnia. Although this abbreviated scale does not cover all domains relevant to a psychological conceptualization of insomnia, themes that are represented on the DBAS have all been hypothesized to play an important role in the etiology of insomnia, particularly in terms of their contribution to cognitive arousal.1,3,4,31 It is likely that other domains related to self-monitoring and rumination, sleep anticipatory anxiety, and sleep effort also contribute to exacerbating insomnia and these themes deserve additional attention in future research.3,32,33
In general, there was significant overlap among the 16 items retained on the abbreviated DBAS version and items previously reported by other investigators to discriminate between insomniacs and good sleepers21,22 or to be sensitive to detect changes with psychological therapy of insomnia.7 For example, at least 10 of the 16 items retained on the current scale were also found to discriminate between poor and good sleepers,21,22 and 8 of the 10 items previously reported to be sensitive to therapeutic changes7 were retained on the current version. While there are some inevitable discrepancies among those different versions, this is not unexpected because our selection of items was based on a combination of both statistical and clinical criteria rather than relying only on statistical ones. Indeed, we selected items that were psychometrically sound, fit the theory, and were clinically relevant to the study of insomnia. Although some of the selected items may not always discriminate poor from good sleepers, we believe that such items (e.g., I need 8 hours of sleep) are useful to identify individuals who might be at risk for developing insomnia and to sample domains that are relevant for therapy (i.e., correcting unrealistic expectations). Likewise, other domains (e.g., insomnia interferes with daytime functioning, cannot function without a good night's sleep) may not be readily responsive to short-term therapy, but would still represent important treatment target given their potential role in turning a situational sleep problem into chronic insomnia. Additional studies are needed to further examine how each item and factor are associated with insomnia severity, how well they discriminate among different insomnia subtypes, how sensitive they are to cognitive therapy, and how initial changes on specific sleep related beliefs and attitudes are associated with long-term outcome. Further psychometric validation using Item Response Theory would be useful to examine the probability of endorsing different items as a function of insomnia severity or comorbidity.
Current scoring guidelines involve a simple average of the scores from all 16 items, with the interpretation being that a stronger endorsement of sleep-disruptive beliefs is maladaptive. This interpretation is supported, at least partially, by the positive correlations between the DBAS total and subscale scores and convergent measures of insomnia severity (ISI) and measures of anxiety (BAI) and depressive symptomatology (BDI). Surprisingly, the associations with specific sleep parameters, whether based on subjective sleep diaries or on PSG data, were generally weak and nonsignificant. The reason for the lack of relationship, particularly between 2 self-reported measures, is unclear. One could argue that it is due to a lack of variability on sleep measures in the present samples composed exclusively of individuals with insomnia. Another plausible explanation might be that ratings of beliefs and attitudes about sleep fluctuate over time and may not relate to specific sleep/wake parameters averaged over periods of 2 weeks (diary) or 3 nights (PSG). Using ecological momentary assessment methodology could yield more precise estimates of these relationships, as recently reported in the assessment of the relationship between insomnia and daytime symptoms.34,35 Additional research would be useful to evaluate further the relationships of beliefs and attitudes about sleep, as well as other sleep cognitions, to the genesis of insomnia. It would also be of interest to have sleep and insomnia experts rate the extent to which they believe the DBAS items/statements are dysfunctional or maladaptive in nature. Such information would help to develop and validate more refined interpretative guidelines. Normative data would also be useful to evaluate the clinical significance of change scores following treatment, as would indices of sensitivity and specificity to identify at risk individuals in the general population.26
The DBAS can serve 2 primary functions, one qualitative and one quantitative. The DBAS was designed initially to assist clinicians in identifying a subset of potentially sleep-disruptive cognitions to be addressed in therapy. This objective can be achieved with either the current 16-item version or with the original 30-item version, which provides a broader sampling of sleep-disruptive beliefs. This qualitative approach can be complemented with a more quantitative approach whereby the DBAS is used as an outcome or process measure. This latter quantitative approach has already been used by several investigators in studies of primary insomnia9,13,16,17,19,20,36–39 or insomnia associated with medical or psychiatric conditions.18,40
The development of reliable and valid instruments is essential to move forward the field of insomnia.41 A panel of experts made recommendations for using standardized assessment in insomnia research.10 Along these recommendations, the objective of this paper was to validate an abbreviated version of the DBAS in order to encourage use of a standard version of this instrument among clinicians and researchers. As multiple measures are typically administered to the same individuals, an abbreviated version of the DBAS can reduce burden on research participants. Although the original 30 items measure remains psychometrically sound and clinically useful, it is hoped that the validation of this abbreviated version will lead more clinicians and researchers to include this brief measure in their insomnia assessment battery and, more importantly, to use the same abbreviated version to facilitate comparisons of results across studies.
ACKNOWLEDGMENTS
Research supported in part by grants from the National Institute of Mental Health (MH-60413) and the Canadian Institutes of Health Research (MT42504), and from a Canada Research Chair.
Footnotes
Disclosure Statement
This is not an industry supported study. Dr. Morin has received research support from Sanofi-Aventis; has consulted for Sepracor, Pfizer, Neurocrine, Takeda, and Shire Biochem; and has participated in speaking engagements for Takeda, Sanofi-Aventis, and Merck. The other authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Espie CA. Insomnia: conceptual issues in the development, persistence, and treatment of sleep disorders in adults. Annu Rev Psychol. 2002;53:215–43. doi: 10.1146/annurev.psych.53.100901.135243. [DOI] [PubMed] [Google Scholar]
- 2.Edinger JD, Fins A, Glenn DM, et al. Insomnia and the eye of the beholder: are there clinical markers of objective sleep disturbances among adults with and without insomnia complaints? J Consult Clin Psychol. 2000;68:586–93. [PubMed] [Google Scholar]
- 3.Harvey AG. A cognitive theory of and therapy for chronic insomnia. Journal of Cognitive Psychotherapy: An International Quarterly. 2005;19:41–60. [Google Scholar]
- 4.Morin CM. Insomnia: psychological assessment and management. New York, NY: Guilford Press; 1993. [Google Scholar]
- 5.Morin CM, Espie CA. Insomnia: a clinical guide to assessment and treatment. New York: Kluwer Academic/Plenum Publishers; 2003. [Google Scholar]
- 6.Morin CM, Bootzin RR, Buysse DJ, Edinger JD, Espie CA, Lichstein KL. Psychological and behavioral treatment of insomnia: an update of recent evidence (1998-2004) Sleep. 2006;29:1398–1414. doi: 10.1093/sleep/29.11.1398. [DOI] [PubMed] [Google Scholar]
- 7.Espie CA, Inglis SJ, Harvey L, Tessier S. Insomniacs' attributions: psychometric properties of the dysfunctional beliefs and attitudes about sleep scale and the sleep disturbance questionnaire. J Psychosom Res. 2000;48:141–8. doi: 10.1016/s0022-3999(99)00090-2. [DOI] [PubMed] [Google Scholar]
- 8.Edinger JD, Wohlgemuth WK, Radtke RA, Marsh GR, Quillian E. Does cognitive-behavioral insomnia therapy alter dysfunctional beliefs about sleep? Sleep. 2001;24:591–9. doi: 10.1093/sleep/24.5.591. [DOI] [PubMed] [Google Scholar]
- 9.Morin CM, Blais FC, Savard J. Are changes in beliefs and attitudes about sleep related to sleep improvements in the treatment of insomnia? Behav Res Ther. 2002;40:741–52. doi: 10.1016/s0005-7967(01)00055-9. [DOI] [PubMed] [Google Scholar]
- 10.Buysse DJ, Ancoli-Israel S, Edinger JD, Lichstein KL, Morin CM. Recommendations for a standard research assessment of insomnia. Sleep. 2006;29:1155–73. doi: 10.1093/sleep/29.9.1155. [DOI] [PubMed] [Google Scholar]
- 11.National Institutes of Health. National Institutes of Health State of the Science Conference Statement: manifestations and management of chronic insomnia in adults. Sleep. 2005;28:1049–57. doi: 10.1093/sleep/28.9.1049. [DOI] [PubMed] [Google Scholar]
- 12.Morin CM. The Behavior Therapist. Summer. 1994. Dysfunctional beliefs and attitudes about sleep: Preliminary scale development and description; pp. 163–4. [Google Scholar]
- 13.Bastien CH, Morin CM, Ouellet MC, Blais FC, Bouchard S. Cognitive-behavioral therapy for insomnia: comparison of individual therapy, group therapy, and telephone consultations. J Consult Clin Psychol. 2004;72:653–9. doi: 10.1037/0022-006X.72.4.653. [DOI] [PubMed] [Google Scholar]
- 14.Blais FC, Gendron L, Mimeault V, Morin CM. Évaluation de l'insomnie: validation de trois questionnaires [Evaluation of insomnia: validation of three questionnaires] Encephale. 1997;23:447–53. [PubMed] [Google Scholar]
- 15.Coradeschi D, Novara C, Morin CM. Dysfunctional beliefs and attitudes about sleep questionnaire: versione italiana ed analisi della fedeltà. Psicoterapia Cognitiva e Comportamentale. 2000;6:33–44. [Google Scholar]
- 16.Edinger JD, Sampson WS. A primary care “friendly” cognitive behavioral insomnia therapy. Sleep. 2003;26:177–82. doi: 10.1093/sleep/26.2.177. [DOI] [PubMed] [Google Scholar]
- 17.Lichstein KL, Riedel BW, Wilson NM, Lester KW, Aguillard RN. Relaxation and sleep compression for late-life insomnia: a placebo controlled trial. J Consult Clin Psychol. 2001;69:227–39. doi: 10.1037//0022-006x.69.2.227. [DOI] [PubMed] [Google Scholar]
- 18.Rybarczyk B, Lopez M, Benson R, Alsten C, Stepanski E. Efficacy of two behavioral treatment programs for comorbid geriatric insomnia. Psychol Aging. 2002;17:288–98. [PubMed] [Google Scholar]
- 19.Ström S, Pettersson R, Andersson G. Internet-Based Treatment for Insomnia: a Controlled Evaluation. J Cons Clin Psychol. 2004;72:113–20. doi: 10.1037/0022-006X.72.1.113. [DOI] [PubMed] [Google Scholar]
- 20.Vincent NK, Hameed H. Relation between adherence and outcome in the group treatment of insomnia. Behav Sleep Med. 2003;1:125–39. doi: 10.1207/S15402010BSM0103_1. [DOI] [PubMed] [Google Scholar]
- 21.Carney CE, Edinger JE. Identifying critical beliefs about sleep in primary insomnia. Sleep. 2006;29:444–53. [PubMed] [Google Scholar]
- 22.Morin CM, Stone J, Trinkle D, Mercer J, Rembserg S. Dysfunctional beliefs and attitudes about sleep among older adults with and without insomnia complaints. Psychol Aging. 1993;23:263–71. doi: 10.1037//0882-7974.8.3.463. [DOI] [PubMed] [Google Scholar]
- 23.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders – Text Revisions (DSM-IV-TR) Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 24.First MB, Gibbon M, Spitzer RL, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders SCID I: Clinician version, administration booklet. Washington, DC: American Psychiatric Press; 1997. [Google Scholar]
- 25.Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 26.Smith, Trinder J. Detecting insomnia: comparison of four self-report measures of sleep in a young adult population. J Sleep Res. 2001;10:229–35. doi: 10.1046/j.1365-2869.2001.00262.x. [DOI] [PubMed] [Google Scholar]
- 27.Beck AT, Steer RA, Brown GK. Manual. 2nd ed. San Antonio, TX: Psychological Corp; 1996. Beck Depression inventory. [Google Scholar]
- 28.Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56:893–7. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- 29.Bentler PM, Chou CP. Practical issues in structural modeling. Sociological Methods and Research. 1987;16:78–117. [Google Scholar]
- 30.SAS Institute. SAS/STAT User's Guide, Version 8; Volumes 1, 2, and 3. Cary, NC: SAS Institute; 2001. [Google Scholar]
- 31.Perlis ML, Smith MT, Pigeon WR. Etiology and pathophysiology of insomnia. In: Kryger MH, Roth T, Dement WC, editors. Principles and practice of sleep medicine. fourth edition. Philadelphia: Elsevier Saunders; 2005. pp. 714–25. [Google Scholar]
- 32.Ree MJ, Harvey AG. Interpretative biases in chronic insomnia: An investigation using a priming paradigm. Behav Ther. 2006;3:248–58. doi: 10.1016/j.beth.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 33.Espie CA, Broomfield NM, MacMahon KM, Macphee LM, Taylor LM. The attention-intention-effort pathway in the development of psychophysiologic insomnia: a theoretical review. Sleep Med Rev. 2006;4:215–45. doi: 10.1016/j.smrv.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 34.Buysse DJ, Thompson W, Scott J, et al. Daytime symptoms in primary insomnia: A prospective analysis using ecological momentary assessment. Sleep Med. 2007;8:198–208. doi: 10.1016/j.sleep.2006.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Moul DE, Nofzinger EA, Pilkonis PA, Houck PR, Miewald JM, Buysse DJ. Symptom reports in chronic severe insomnia. Sleep. 2002;25:555–63. [PubMed] [Google Scholar]
- 36.Espie CA, Inglis SJ, Harvey L. Predicting clinically significant response to cognitive behavior therapy for chronic insomnia in general medical practice: analyses of outcome data at 12 months posttreatment. J Consul Clin Psychol. 2001;69:58–66. doi: 10.1037//0022-006x.69.1.58. [DOI] [PubMed] [Google Scholar]
- 37.Means MK, Lichstein KL, Epperson MT, Johnson CT. Relaxation therapy for insomnia: nighttime and day time effects. Behav Res Ther. 2000;38:665–78. doi: 10.1016/s0005-7967(99)00091-1. [DOI] [PubMed] [Google Scholar]
- 38.Mimeault V, Morin CM. Self-help treatment for insomnia: bibliotherapy with and without professional guidance. J Consult Clin Psychol. 1999;67:511–9. doi: 10.1037//0022-006x.67.4.511. [DOI] [PubMed] [Google Scholar]
- 39.Vallières A, Guay B, Morin CM. Sequential use of medication and behavioural therapies for chronic insomnia: an exploratory study. Behav Res Ther. 2005;43:1611–30. doi: 10.1016/j.brat.2004.11.011. [DOI] [PubMed] [Google Scholar]
- 40.Savard J, Simard S, Ivers H, Morin CM. Randomized study on the efficacy of cognitive-behavioral therapy for insomnia secondary to breast cancer, part I: Sleep and psychological effects. J Clin Oncol. 2005;23:6083–96. doi: 10.1200/JCO.2005.09.548. [DOI] [PubMed] [Google Scholar]
- 41.Morin CM. Measuring outcome in randomized clinical trials of insomnia therapies. Sleep Med Rev. 2003;7:263–79. doi: 10.1053/smrv.2002.0274. [DOI] [PubMed] [Google Scholar]