Abstract
Aim
To study temporal trends in the incidence of hospitalisations due to infection in children in Denmark.
Methods
A national register based cohort of 1 892 711 Danish children aged 0–5 years were studied from 1980 to 2001. Child and family characteristics were identified in the Danish Civil Registration System; hospitalisations were identified in the Danish National Patient Registry. Annual incidence rates were estimated using log‐linear Poisson regression.
Results
During the studied period, the incidence of hospitalisations from infection increased by 62% in 0–5 year old children. The increase was mainly due to a sevenfold increase in the incidence of infections leading to short term hospitalisation in children aged 0–1 years. Since the increase in incidence was contrasted with a decrease in duration of hospitalisation, no further strain was put on the health services in Denmark.
Conclusion
During the last two decades, the incidence of short term hospitalisations due to infections increased markedly among the youngest children. However, the strain on the health services remained constant. The observed increase in the incidence of short term hospitalisations among the youngest children may reflect changes in hospitalisation practices and utilisation, rather than an increase in incidence of infections.
Keywords: epidemiology, gastrointestinal, incidence, infection, respiration
A recent study1 showed that 33 boys and 23 girls, respectively, were admitted to hospital with a respiratory infection per 1000 risk years in children aged 0–5 years in Denmark. Other epidemiological studies have shown an increase in the rates of hospitalised children during the past decades.2,3,4,5,6,7,8,9 These studies do not agree as to whether the observed increase is due to an increase in morbidity,2 or whether it is due to other factors, such as changed hospitalisation practices and utilisation.3,6,7 To further investigate this, we studied the incidence of hospitalisations due to infections in children aged 0–5 years in the period from 1980 to 2001. This was done in a national prospective register based study, in which annual incidence rates were stratified on types of infection, age groups, and duration of hospitalisation.
Methods
As of 1 January 2001, the population in Denmark was 5 349 212, of which 8% were 0–5 years old.10
Population and hospitalisation data
The present study is based on Danish register data and was approved by the Danish Data Protection Agency. In the Danish Civil Registration System (DCRS)11 we identified all children in Denmark between 0 and 5 years of age in the period from 1980 to 2001. The DCRS was established on 1 April 1968, and all residents and newborns in Denmark have since been given a unique 10‐digit person identification number, which is also recorded in other Danish registers. From the DCRS, information was retrieved regarding date of birth, sex, county of residence and possible date of immigration, emigration, and death of the child. Information on birth order, marital state, and age of the mother at the time of delivery, as well as ethnicity of the child, was subsequently obtained by identifying the parents in the DCRS. The information from the DCRS was linked with information regarding discharge diagnosis and duration of the hospital admission from the Danish National Patient Registry (DNPR).12 Finally, birth weight and gestational age data was obtained from the Danish Medical Birth Registry13 and linked with the information from DCRS and DNPR. The outcome of the study was defined as first inpatient admission to hospital with an infection (main condition only). Diagnoses were classified into groups of upper respiratory infections, lower respiratory infections, gastrointestinal infections, and other infections (table 1).
Table 1 ICD‐8 and ICD‐10 codes according to type of infection.
| Infection | ICD‐8 codes | ICD‐10 codes |
|---|---|---|
| Upper respiratory infection | 032, 075, 381–383, 460–465, 500–501, 503 | A36, B27, H65–H72, J00–J06, J32, J35–J36 |
| Lower respiratory infection | 033, 466, 470–491, 493, 510, 513 | A37, J10–J22, J45.9, J85–J86 |
| Gastrointestinal infection | 000–009, 014, 054.01, 054.08 | A00–A09, B00.2, K93.0 |
| Other infection | 010–027, 035–036, 038–136, 320, 322–323, 360–364, 381.00, 381.01, 381.09, 381.99, 390–391, 420–422, 540–541, 580, 583, 590.10, 590.11, 590.15, 595, 597, 680–686 | A15–A28, A38–A41, A46, A48–A99, B00–B99, G00–G07, H00–H01, H10, H16, H20, H30, H65.0, H66.0, H66.9, I00–I01, I30, I33, I38–I40, K35, K37, L00–L08, N00–N01, N05, N10, N12, N30, N34 |
Statistical methods
Annual incidence rates were estimated as the annual number of cases divided by the annual amount of person‐years at risk. Person‐years at risk were calculated by assuming that children were at risk from one week after birth, immigration, or start of 1980, whichever came first, until the first of the following events: first inpatient admission to hospital with an infection, emigration, death, end of 2001, or 6th birthday. The first week after birth was not included as infections in this period were considered to be due to perinatal complications. Data from the DNPR was available from 1977, but we excluded data before 1980 from our analyses to reduce the risk of a later hospitalisation being counted as the first. Estimation of incidence rates according to other covariates was performed in the same manner within strata of the covariate. When estimating incidence rates according to duration of hospital admission, the annual number of cases was divided according to duration, whereas the annual person‐years at risk were used in all categories. Incidence rate ratios were estimated by log‐linear Poisson regression of the number of cases with the logarithm of person‐years at risk as offset. Estimation was performed by PROC GENMOD in SAS with Poisson error distribution and log link.14
Results
The population under study consisted of 1 892 711 children, of which 51.2% were boys. During follow up, a total of 309 737 first hospital admissions with infections were recorded. Upper respiratory infections were most frequent (41%), followed by lower respiratory infections (29%), other infections (18%), and gastrointestinal infections (12%), respectively. During the period under study 1.4% of the children emigrated and 0.7% died. Mean follow up time was 4.8 years per child.
Temporal trend by type of infection
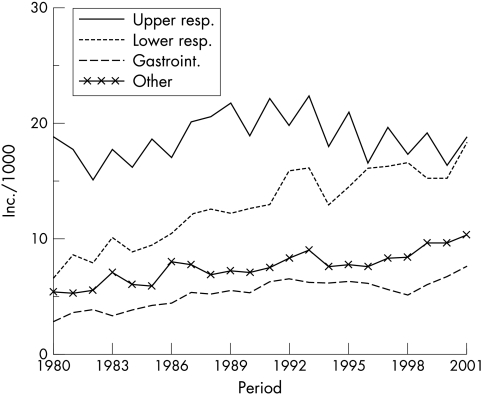
We found an increased incidence of hospitalisations from all types of infections in the studied period. In 1980 the total infection incidence was 35.5 hospitalisations per 1000 risk years in 0–5 year old children in Denmark. In 2001, this figure had increased by 62% to 55.0 hospitalisations per 1000 risk years (data not shown). Figure 1 illustrates the temporal trend in incidence of hospital admissions from the four types of infections. Over the entire period, a constant incidence rate of upper respiratory infections (around 20 hospitalisations per 1000 risk years) was seen. The incidence of lower respiratory infections, gastrointestinal infections, and other infections, respectively, increased steadily; all were approximately doubled during the studied period. In the beginning of the period, hospitalisation for upper respiratory infections was much more frequent than for lower respiratory infections. At the end of the period, there was no difference in the incidence of hospitalisation from upper and lower respiratory infections. The pattern in fig 1 was identical in boys and girls (data not shown).
Figure 1 Hospital admissions per 1000 risk years in children aged 0–5 years, divided into types of infection: upper respiratory infection, lower respiratory infection, gastrointestinal infection, and other infection.
Temporal trend by age
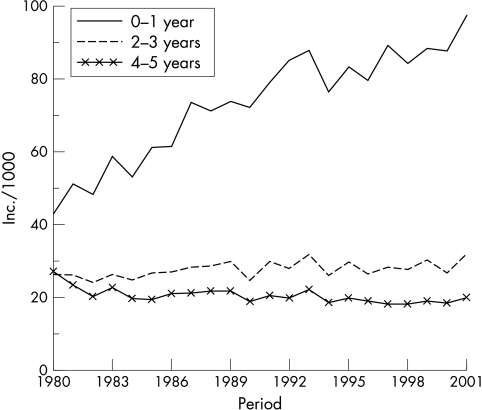
Figure 2 shows that the incidence of hospitalisations from all types of infections increased markedly in children aged 0–1 year. In 1980, 42.8 children aged 0–1 year were admitted to hospital per every 1000 risk years. In comparison, 97.4 children aged 0–1 year were admitted to hospital per 1000 risk years in 2001. This corresponds to a doubling in incidence among 0–1 year old children during the period. Figure 2 also shows a relatively constant incidence in children aged 2 years or more. The trend was similar for the different ages within the three age groups. The age specific temporal trends were identical in boys and girls (data not shown).
Figure 2 Hospital admissions due to all types of infections per 1000 risk years in children aged 0–5 years, divided into age groups: 0–1 year, 2–3 years, and 4–5 years.
Temporal trend by duration of admission
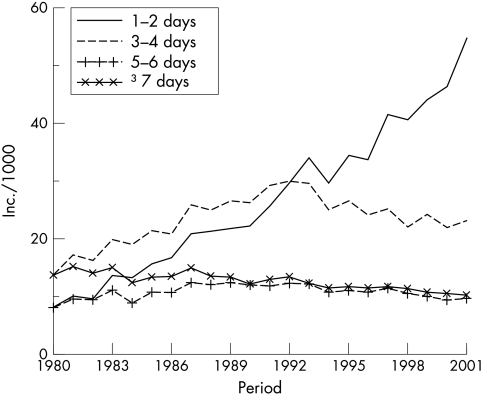
As seen from fig 3, the increased incidence in 0–1 year old children was mainly seen among children admitted to hospital for 1–2 days. In 1980, 7.7 children aged 0–1 year per 1000 risk years were admitted to hospital for 1–2 days. In 2001 this figure had increased to 54.8 per 1000 risk years, corresponding to a sevenfold increase in incidence. Figure 3 also shows a moderate increase in the incidence of hospital admissions lasting 3–4 days in 0–1 year old children. The incidence of hospital admissions lasting 5–6 days and 7 days or more was constant in the studied period in children aged 0–1 year. In children aged 2 years or older, only a minor increase was observed in the incidence of short term hospitalisations. This minor increase was contrasted with a minor decrease in long term hospitalisations (data not shown). Within each of the four groups of duration the trend was similar, and the pattern was identical in boys and girls (data not shown). In 0–1 year old children hospitalised for 1–2 days, the incidence increased primarily during the winter and spring months (data not shown). Over the studied period, the median duration of all hospitalisations from infections decreased from 3.0 days in 1980 to 1.0 day in 2001.
Figure 3 Hospital admissions due to all types of infections per 1000 risk years in children aged 0–1 year, divided into duration of hospital admission: 1–2 days, 3–4 days, 5–6 days, and 7 days or more.
Strain on health services
In a separate analysis, we evaluated whether the observed increase in short term hospitalisations from infections among the youngest children had led to an increased strain on the health services in Denmark. Strain was measured as days admitted to hospital from first admission with an infection, per days at risk. In the studied period, we found the strain on health services to be relatively constant, being approximately 50 hospitalisation days per 100 000 risk days.
Confounding
To evaluate the effect of confounding, we estimated incidence rate ratios according to period. These incidence rate ratios were not changed by adjustment for the following variables: age (quarter‐year intervals), sex, county of residence (time dependent variable), birth order (1, 2, or ⩾3), mother's age at birth of the child (five‐year intervals), ethnicity of the child (both parents born in Denmark versus at least one parent born outside of Denmark), and mother not married or sharing address with the father at the time of birth (yes or no) (data not shown). Furthermore, excluding children with birth weight lower than 2500 g and children born before the 37th week of gestation, respectively, did not change the incidence rates. Thus, crude estimates are presented.
Discussion
The present study points towards a marked increase in the incidence of short term hospitalisations due to infections in 0–1 year old children in the period from 1980 to 2001 in Denmark.
The observed increase may reflect an increase in morbidity from infections in the youngest children, which only require short term hospitalisation. Alternatively it may reflect a change in hospitalisation practices and utilisation, or it may reflect a combination of both. An increase in morbidity could partly be due to the proportion of children attending child care away from their home having increased considerably in the studied period.10 Many epidemiological studies have shown child care away from home to be associated with an increased risk of morbidity from various infectious diseases.15,16,17,18,19,20,21,22 Furthermore, our finding of an increase in incidence primarily during the winter and spring months could imply that an actual increase in morbidity from infections has occurred. On the other hand, there have been major changes in hospitalisation practices and utilisation—for example, many paediatric wards in Denmark established emergency paediatric/monitoring departments during the studied period, mainly in the early and mid 1990s.23 This was done to handle the many incoming acute, but not critically ill children. The admission rate may likewise be influenced by the fact that parents with small children today, to a higher degree than before, wish their child to be attended by a specialist rather than a general practitioner.24 Furthermore, part of the observed increase may reflect a more frequent use of defensive medicine among Danish paediatricians, but this has not been studied. To study whether the observed trend was similar throughout Denmark we stratified analyses on the three major regions of Sealand, Funen, and Jutland. We found similar trends in these regions. Taken together, we suggest that the observed trends may reflect changes in factors not related to morbidity—for example, changes in hospitalisation practices and utilisation. However, we cannot exclude the possibility that such changes have been accompanied by an increase in morbidity in the youngest children.
In accordance with our results, Wickman and colleagues2 found an increased rate of hospitalisations due to lower respiratory infections over time in children younger than 2 years. The study was conducted in Stockholm County (Sweden) in the period from 1973 to 1992. In a study of Oxford children in the period from 1975 to 1985 by Hill,3 an increased rate of paediatric hospitalisations was found in all age groups until 14 years. The studies of Wickman et al and Hill do not agree on the underlying reasons for the observed increase in hospitalisation rate. Wickman et al conclude that the increased rate of hospitalisation may reflect an increase in morbidity. Hill, on the other hand, argues that the increase in admission rates was due to lower threshold for admission, resulting in part from increased availability of beds. Forfar7 further argues that the role of paediatric departments has changed from admitting children only when they are seriously ill, to also admitting children in order to obtain accurate early diagnosis and treatment.
The general increase in incidence was contrasted by a general decrease in duration of hospitalisations. Therefore strain on health services, measured as days admitted to hospital, was constant in the studied period. Strain measured as workload related to handling the increasing number of short term hospitalisations, however, may have increased. The finding of a decrease in the duration of hospitalisations over time is consistent with previous findings of Pearson and colleagues6 and MacFaul and Werneke.5
In the DNPR, hospital admissions are classified according to the International Classification of Diseases.25 Classifications in the DNPR shifted from the 8th revision to the 10th revision in 1994. This does not seem to have affected our results, however, since the observed trends before and after 1994 are very much the same. The validity and coverage of data regarding infections among children in the DNPR has not been evaluated. However, a Danish study26 has shown that 73.7% of all paediatric diagnoses in the NPR are correct, and furthermore that 13.7% have a reasonable alternative in spite of a wrong diagnosis. All together, 70.4% of infection diagnoses (not only in children) in the DNPR were correct. In another Danish study12 it is concluded that the DNPR is a valuable tool for monitoring disease in the Danish population. Thus, one should expect that our results to a high degree reflect an actual increase in short term hospitalisations in the youngest children.
In conclusion, our study showed a general increase in the incidence of hospitalisations of children aged 0–5 years in the period from 1980 to 2001 in Denmark. The increase was mainly due to a marked increase in short term hospitalisations in 0–1 year old children. Due to a decrease in duration of hospitalisations, the strain from hospitalisation of children with infections on the health services in Denmark was not increased during the period. We suggest that the observed increase in the incidence of short term hospitalisations in the youngest children reflects changes in hospitalisation practices and utilisation rather than an actual increase in the incidence of infections. Future research within the area should evaluate the effect of factors such as child care attendance and hospitalisation practices and utilisation on hospitalisation incidence.
What is already known on this topic
Hospitalisation of children with infections has increased over the past decades in several countries
There is no consensus on the underlying reason for the increase
What this study adds
Hospitalisation with infection has increased more than 60% during the last two decades in 0–5 year old children in Denmark
The increase is almost exclusively seen in short term hospitalisations in 0–1 year old children, suggesting changes in hospitalisation practices and utilisation rather than increase in childhood morbidity as the underlying reason
Abbreviations
DCRS - Danish Civil Registration System
DNPR - Danish National Patient Registry
Footnotes
Funding: The present study received support from the Danish Graduate School in Public Health Science, the Health Insurance Foundation, the Egmont Foundation, the National Union of Nursery and Child‐care Assistance, Rosalie Petersens Fond and Gangstedfonden. All contributing authors are independent of funders.
Competing interests: none declared
References
- 1.Jensen‐Fangel S, Mohey R, Johnsen S P.et al Gender differences in hospitalization rates for respiratory tract infections in Danish youth. Scand J Infect Dis 20043631–36. [DOI] [PubMed] [Google Scholar]
- 2.Wickman M, Farahmand B Y, Persson P G.et al Hospitalization for lower respiratory disease during 20 yrs among under 5 yr old children in Stockholm County: a population based survey. Eur Respir J 199811366–370. [DOI] [PubMed] [Google Scholar]
- 3.Hill A M. Trends in paediatric medical admissions. BMJ 19892981479–1483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Spencer N J, Lewis M A. Multiple admissions under 2 years of age. Arch Dis Child 199166938–940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.MacFaul R, Werneke U. Recent trends in hospital use by children in England. Arch Dis Child 200185203–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pearson G, Barry P, Timmins C.et al Changes in the profile of paediatric intensive care associated with centralisation. Intensive Care Med 2001271670–1673. [DOI] [PubMed] [Google Scholar]
- 7.Forfar J O. Trends in paediatric medical admissions. BMJ 19892981711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nielsen A, Lie H, Keiding L.et al Admissions in hospital. In: The health of children in Denmark. Copenhagen: Danish Institute of Clinical Epidemiology, 199850–54.
- 9.Durojaiye L I, Hutchison T, Madeley R J. Improved primary care does not prevent the admission of children to hospital. Public Health 1989103181–188. [DOI] [PubMed] [Google Scholar]
- 10. http://www.statbank.dk 2004
- 11.Malig C.The Civil Registration System in Denmark. IIVRS technical paper. Bethesda, MD: International Institute for Vital Registration and Statistics, 1996661–6. [Google Scholar]
- 12.Andersen T F, Madsen M, Jorgensen J.et al The Danish National Hospital Register. A valuable source of data for modern health sciences. Dan Med Bull 199946263–268. [PubMed] [Google Scholar]
- 13.Knudsen L B, Olsen J. The Danish Medical Birth Registry. Dan Med Bull 199845320–323. [PubMed] [Google Scholar]
- 14.SAS Institute Inc SAS/STAT software release 8.2. Cary, NC: SAS Institute Inc, 2001
- 15.Collet J P, Burtin P, Gillet J.et al Risk of infectious diseases in children attending different types of day‐care setting. Epicreche Research Group. Respiration 199461(suppl 1)16–19. [DOI] [PubMed] [Google Scholar]
- 16.Klein J O. Infectious diseases and day care. Rev Infect Dis 19868521–526. [DOI] [PubMed] [Google Scholar]
- 17.Louhiala P J, Jaakkola N, Ruotsalainen R.et al Form of day care and respiratory infections among Finnish children. Am J Public Health 1995851109–1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Louhiala P J, Jaakkola N, Ruotsalainen R.et al Day‐care centers and diarrhea: a public health perspective. J Pediatr 1997131476–479. [DOI] [PubMed] [Google Scholar]
- 19.Nafstad P, Hagen J A, Oie L, Magnus P.et al Day care centers and respiratory health. Pediatrics 1999103753–758. [DOI] [PubMed] [Google Scholar]
- 20.Stahlberg M R. The influence of form of day care on occurrence of acute respiratory tract infections among young children. Thesis, University of Turku 1980
- 21.Uldall P. [Forms of care and children's infections. 1. Occurrence and causal factors]. Ugeskr Laeger 19901522345–2348. [PubMed] [Google Scholar]
- 22.Wald E R, Guerra N, Byers C. Frequency and severity of infections in day care: three‐year follow‐up. J Pediatr 1991118509–514. [DOI] [PubMed] [Google Scholar]
- 23.Kastrup K W, Andersen K V. [Emergency pediatric/monitoring department. The Danish Pediatric Society]. Ugeskr Laeger 20011631693. [PubMed] [Google Scholar]
- 24.Lindenskov L, Bronderslev L, Andersen K V. [Why do parents of small children visit casualty ward when their children suffer of acute illness?]. Ugeskr Laeger 20011631089–1092. [PubMed] [Google Scholar]
- 25.International Classification of Diseases WHO Collaborating Centers. Epidemiol Bull 1998197–11. [PubMed] [Google Scholar]
- 26.Mosbech J, Jorgensen J, Madsen M.et al [The national patient registry. Evaluation of data quality]. Ugeskr Laeger 19951573741–3745. [PubMed] [Google Scholar]