Abstract
To facilitate decisions on interventions in medically referred children with idiopathic short stature, the research on psychosocial functioning of these children, possible risk and protective factors influencing adaptation, and effects of hormone treatment were reviewed. Parents ranked the behaviour of their children on average between normal and below normal. The magnitude of these deviations varied from small to large. Little is known about the children's self‐perceived psychosocial functioning. Some risk factors were found: being teased, being juvenilised, being a boy, having a younger but taller sibling, low intelligence, and low socioeconomic status. There have been few studies on the impact of protective factors including temperament, coping strategies, and social support. On average, hormone treatment did not improve psychosocial functioning. The research shows the advantages and disadvantages of hormone treatment that must be considered when choosing a suitable intervention. It is suggested that psychosocial adjustment can be improved by focusing on factors other than height alone.
Keywords: idiopathic short stature, psychological adaptation, social adjustment, growth hormone, risk factors
The availability of biosynthetic growth hormone (GH) initiated the treatment of growth failure of pathological origin.1 Treatment of children with idiopathic short stature (ISS), who have a height below two standard deviations from the mean for age and sex (approximately corresponding to the 3rd centile) without apparent pathology,2 is still under debate. Growth enhancing hormone treatment in short but healthy children can be motivated by the wish to alleviate height related psychosocial suffering, to improve overall psychosocial functioning, and to enhance future prospects in life and society.3,4
The variable results of studies regarding the psychosocial functioning of children with ISS appear to depend on the choice of medically referred or population based samples,5,6 the preferred theoretical concepts such as psychosocial stressors, psychosocial adaptation, or psychopathology,7 the use of generic or complaint specific investigational tools,8 and the respondents of the study such as parents or children.9,10 It has also been suggested that psychosocial functioning of short children depends on several risk and protective factors.11,12
To enable decisions on interventions in children with ISS who come to see a physician, clarity is needed with respect to the kind and severity of their psychosocial problems and with respect to the effects of hormone treatment. To that aim, we systematically reviewed the available research on the psychosocial functioning of medically referred children with ISS and the effects of hormone treatment on this functioning. Our focus was on individual variation in adaptation in order to find out whether subgroups of medically referred children with ISS have specific risks and different outcomes of hormone treatment. Guided by the results of our review, we critically discuss the pros and cons of hormone treatment in children with ISS.
Methods
We searched the Medline and PsycInfo databases using the following search terms: (idiopathic short stature OR short stature) AND (psychosocial OR behavior OR quality of life OR growth hormone). Further articles were sourced from the reference lists of articles ascertained through the search. We included only studies that assessed psychosocial functioning of children and adolescents who were medically referred. Effect sizes were calculated when articles provided appropriate statistics.
Impact of short stature
Table 1 presents a general overview of studies on psychosocial functioning of medically referred children and adolescents with ISS.
Table 1 Competencies and behavioural problems of medically referred children with short stature (SS) compared to control groups (CON).
| Study | n | Age | Scholastic competence | Social competence | Social problems | Externalising problems | Internalising problems | Thought problems | Attention problems | Self‐concept | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| SS | CON | d | d | d | d | d | d | d | d | ||
| Gordon et al17/Richman et al15† | 24 | 23 | 6–12 | −0.10 | −0.66* | 0.29 | 0.77* | −0.38 | |||
| Huisman et al23 | 30 | norms | 5–15 | low | ns | ns | ns | ns | ns | normal | |
| Sandberg18‡§ | 73 | 688 | 6–10 | 0.00 | −0.62*** | 0.21* | −0.21 | 0.10 | 0.42*** | 0.05 | |
| 0.10 | 0.23 | 0.00 | −0.41 | −0.17 | 0.12 | −0.23 | |||||
| Sandberg et al16‡¶ | 258 | norms | 4–18 | −0.38*** | −0.60*** | 0.38*** | 0.13 | 0.30** | 0.21 | 0.20* | |
| −0.44*** | −0.10 | 0.51*** | 0.00 | 0.16 | 0.20 | 0.24 | |||||
| −0.32** | −0.52*** | 0.62*** | 0.17 | 0.42*** | 0.21 | 0.21 | |||||
| −0.45** | 0.00 | 0.30 | −0.15 | −0.09 | −0.26 | 0.18 | |||||
| Siegel13 | 90 | 90 | 8–13 | −0.61*** | −0.58** | 0.47* | 0.74*** | ||||
| Skuse et al14/Gilmour et al19§ | 22 | 22 | 6–11 | ns | ns | 0.90* | ns | ns | 0.84** | 0.99** | −0.30 |
| 0.17 | |||||||||||
| Sandberg et al26‡¶ | 522 | norms | 4–18 | 0.03 | 0.22** | ||||||
| 0.15 | 0.34*** | ||||||||||
| 0.18* | 0.40*** | ||||||||||
| −0.15 | −0.03 | ||||||||||
| Kranzler et al5 | 27 | 29 | 6–12 | −0.49** | 0.54* | 0.15 | 0.68* | ||||
| Visser‐van Balen et al4 | 38 | norms | 10–13 | 0.73** | 0.28 | 0.54* | 0.26 | 0.59* | 0.02 | ||
| Erling et al27 | 33 | norms | 9–15 | ns | |||||||
| Stabler et al25†† | 80 | norms | 5–16 | low | ns | high | high | ||||
*p<0.05, **p<0.01, ***p<0.001, ns = not significant.
The d values reflect the difference between the short stature and control (reference) groups in standard deviation units. A positive score indicates that the children with short stature have a higher score on that scale than the control group, which means higher competence (positive), more behaviour problems (negative), and higher self‐concept (positive).
The d values have the following common effect sizes: a value smaller than 0.2 reflects no difference, while values between 0.2 and 0.5, between 0.5 and 0.8, and greater than 0.8 reflect small, moderate, and large differences, respectively.37 Asterisks indicate whether the mean scores of the short stature groups significantly differed from the control groups.
†Self‐concept: mean effect size of the six Piers Harris self‐concept scales.
‡Includes other aetiologies, such as growth hormone deficiency.
§First line: boys; second line: girls.
¶First line: boys aged 4–11; second line: girls aged 4–11; third line: boys aged 12–18; fourth line: girls aged 12–18.
††Percentage of children with problems compared to general norms.
The results of our review show most clarity on the social functioning of children with ISS. According to their parents, the short children have lower social competence and show more social problems than children with normal stature.4,13,14,15,16,17,18,19 These findings confirm theories which state that physical appearance has an influence on people's social environments, which might in turn influence social and personality development.20 Society emphasises appearance at every age. Those who are attractive by societal standards get more positive attention than those judged to be less attractive.21 The perceiver's behaviour towards the child will in turn influence the child's behaviour and self‐judgements.22 Clinical impressions that short children tend to play with younger children or seek peer approval by being the group mascot may also reflect social problems.
The intelligence of children with ISS (not shown in table 1) is within the normal range.5,13,14,15,23,24,25 With respect to behaviour problems and scholastic competence, our review shows that medically referred children with ISS are functioning, on average, between normal and below normal.4,5,13,14,15,16,17,18,19,23,25,26,27 When statistically significant deviations were found, the effect sizes were small to moderate for scholastic competence, externalising problems, and internalising problems, and small to large for thought and attention problems (table 1). Early adolescence seems to be a critical period in short children for developing internalising, externalising, and social problems.16,24,26 Perhaps the burden of short stature is relatively large in pubertal children, because in this period stature is more important than in other developmental phases. The wish to be just like the others, and to be liked and accepted because of physical appearance, are important themes of this developmental phase.22
This would suggest that being short is a transient problem. However, studies on the consequences of being short for psychosocial functioning in adulthood are inconclusive (not shown in table 1). The adults in these studies consulted a paediatrician during their childhood for their ISS, but did not receive growth hormone treatment. While two studies reported a relatively low percentage of marriages, a relatively high percentage of unemployment, and self‐reported problems in social functioning among short adults,28,29 two other studies did not find a negative impact of short stature on finding a spouse or job, or on overall psychosocial functioning and wellbeing.30,31
It must be noted that most of the studies among children examined parental reports only. Studies based on reports from teachers and peers did not find lower social competence, or internalising or externalising problems in children with ISS.14,19 When both parent and child reports were used, the parents judged the behavioural problems of their child on the Child Behavior Check List, and the children evaluated their inner feelings (self‐concept). While the parental reports on social functioning, behavioural problems, and school competence give indications for psychosocial dysfunctioning, the children's own reports regarding self‐esteem give relatively few indications for psychosocial problems (table 1). A critical question is whether the children themselves or their parents are the best judges of the children's psychosocial functioning. Children may be unreliable informants because they are too young to give an adequate assessment of their own functioning, lack a time perspective, or have a tendency towards denial. The attitudes of parents to the psychosocial functioning of their short children may be biased because of anxiety about their child's health, future probabilities to find a spouse or job, or negative experiences regarding their own short stature.4,29 There are no studies in which similar concepts have been studied by both parents' and children's reports.
Our review was restricted to short children who were medically referred. Short children who are not medically referred for their height do not appear to have psychosocial problems.5,6,32,33,34,35 This raises the question why some short but healthy children develop psychosocial problems, whereas others seem to function psychologically well. It has been suggested that psychosocial adjustment in short children depends on several risk and protective factors such as aetiology and degree of the short stature, height related psychosocial stress, and coping strategies.7,12,29 Moreover, parents of medically referred short children may misattribute more general psychosocial problems of their child to the short stature,6,7,29,36 a suggestion that cannot be answered from the available research. It is possible that medically referred children with ISS have psychosocial problems because of their short stature, but it is also possible that children with psychosocial problems who are also short may be medically referred relatively often.
In conclusion, medically referred children with ISS have, on average and according to their parents, more psychosocial problems than children with normal stature and children with short stature who are not medically referred. The magnitude of the behavioural deviations was judged to vary from small to large.
Risk and protective factors
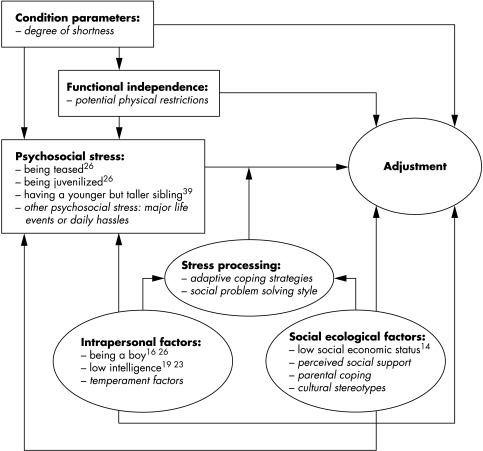
Risk and protective factors that affect psychosocial adaptation in children with ISS include characteristics of the child and environmental factors. The disability–stress–coping model of Wallander38 has been developed to conceptualise possible risk and protective factors influencing the adjustment of the child with a chronic condition. The risk factors in the model are condition parameters, functional independence, and psychosocial stress (illness related stress, major life events, daily hassles). Protective factors are intrapersonal factors (temperament or personality characteristics, intelligence, sex), socioecological factors (socioeconomic status, family functioning, social support, parental adaptation), and stress processing factors (cognitive appraisal, coping strategies). The impact of the risk factors on adjustment are moderated by protective factors. The absence or opposite of a protective factor can also be understood as a risk factor. We used this model to point out which risk and protective factors influence adaptation in children with ISS (fig 1).
Figure 1 The disability–stress–coping model38 applied to idiopathic short stature. Hypothesised effects are represented by italic words, empirical findings by non‐italic words, risk factors by squares, and protective factors by ovals.
Our review suggests some risk factors for maladaptation in children with ISS: being teased,26 being juvenilised,26 being a boy,16,26 having low intelligence,19,23 having a younger but taller sibling,39 and being part of a low socioeconomic status family.14 Studies on the impact of the degree of shortness on adjustment did not find an effect,14,17,26 nor did one study that took into account a child's social problem solving style and perceived social support.19 Not much attention has been paid to potential risk and protective factors, probably because sample sizes of research in children with ISS are generally small. Therefore, the results have to be interpreted with caution.
The reason that no relation has been found between the degree of shortness and adjustment may be that not actual height but perceived height is crucial.40 The studies reporting low intelligence as a risk factor19,23 did not report having included children with low birth weight or born small for gestational age, which has been associated with reduced intelligence and mild neurological dysfunctions.41,42 Low intelligence as well as low socioeconomic status are risk factors for psychosocial consequences in all kinds of conditions, including short stature. Probably boys with short stature have more social problems than girls, because it tends to be an appreciated characteristic of men being taller than women.43 The risk factors having a younger but taller sibling and being juvenilised perhaps both reflect that children feel bad about it and develop behavioural problems as a consequence of being treated as younger than appropriate for their real age. Social comparison among siblings tends to be high and the impact of siblings on developing self‐representations is considerable.44 From Wallander's model it can be expected that a child with ISS who is also experiencing other psychosocial stress (major life events or daily hassles) will respond less adequately to height related stressors and be more vulnerable to psychosocial maladjustment. This was concluded in one study.26
Several risk and protective factors from Wallander's model that are expected to affect adjustment in children with ISS have not been studied; for example, the influence of potential physical restrictions in severely short children. When facing height related psychosocial stress, temperamental factors that promote adaptive coping strategies are important. Approval and acceptance from significant others is positively associated with high self‐esteem and adjustment.22 Studies that examined family functioning in families with short children did not find major differences between families with children of normal stature and those with short children,5,17,25,45 but nothing is known about the potential positive influence of parental coping with the short stature of their children. Finally, cultural stereotypes regarding short stature are a potential source of stress or relief for short children. Children internalise standards and values of the “larger society”, as reflected in, for example, the media. Perceptions of one's physical attractiveness, in relation to the importance that is attached to meeting cultural standards of appearance, contribute to one's overall sense of worth as a person.22
In conclusion, some risk factors influencing adaptation in children with ISS were found, whereas the impact of protective factors has been hardly studied. To decide which intervention a child with ISS is expected to benefit from, insight into risk and protective factors is important. In clinical care, besides the usual medical history, a thorough assessment of psychosocial adjustment should aim at all variables listed in the model.
Effects of hormone treatment
The results of studies on the effect of hormone treatment on final height gain in ISS are variable, with a mean height gain of at best approximately 7 cm and interindividual variation in the long term growth outcome.1 A considerable number of children with ISS remain short compared to the mean for age and sex after hormone treatment.
Table 2 presents a general overview of studies regarding effects of hormone treatment on the psychosocial functioning of children with ISS. On average, hormone treatment did not improve psychosocial functioning. Most studies show that GH treatment does not change psychosocial functioning or even has negative consequences on psychosocial functioning.8,23,46,47,48,49,50 Some of these studies found no indications of psychosocial problems before treatment,23,49 whereas other studies found some social or behavioural problems at baseline.8,50 Only a few studies indicated improvement in problem behaviours.51,52 It could be hypothesised that the children who suffer most from being short do benefit from the intervention, but sample size restrictions prevent the systematic study of individual differences that may affect the psychosocial outcome of hormone treatment.
Table 2 Effects of hormone treatment on psychosocial functioning of children with idiopathic short stature.
| Study | Treatment group | Control group | Age at onset of treatment | Design | Baseline | Negative effects | No change | Improvement |
|---|---|---|---|---|---|---|---|---|
| Huisman et al23 | 26 ISS | – | 5–15 years | Prospective: before and after 2 years GH treatment | = social anxiety, self‐concept (c), behaviour (p); ↑ physical appearance (c) | Physical appearance (c) | Social anxiety, self‐concept (c), behaviour (p) | |
| Boulton et al46 | 66 ISS | – | 5–15 years | Prospective: before, and after 6 and 24 months | = self‐concept | Children's attitudes to being short | ||
| Pilpel et al47 | 65 ISS | 33 ISS | 8–16 years (age of measurement) | Retrospective: comparison of CON and EXP after at least 2 years GH treatment | – | Relationships with family members (c) | = school achievements, leisure activities, self‐esteem, relationships with peers (c) | |
| 15 GHD | ||||||||
| 16 TS | ||||||||
| Rekers‐Mombarg et al48 | 24 ISS | 65 ISS | 19 years or older (age of measurement) | Retrospective: comparison of CON and EXP after GH treatment | – | Less often a spouse (c) | = education level, general health state, personality (c) | |
| Stabler et al51 | 59 ISS | 113 normal stature | 5–16 years | Prospective: comparison of CON and EXP before and yearly during 3 years GH treatment | = intelligence, achievement (c); ↑ internalising, externalising, and total problem behaviour, and all subscales of the CBCL (p) | Intelligence, achievement (c), withdrawn behaviour, somatic complaints, attention and thought problems, aggressive/delinquent behaviour (p) | Total problem behaviour, anxious/depressed behaviour, social problems (p) | |
| Downie et al49 | 15 short normal | 13 short normal | 7–8 years | Prospective: comparison of CON and EXP before and after 3 and 5 years GH treatment | = intelligence, attainment, self‐esteem (c), behaviour (p) | Intelligence, attainment, self‐esteem (c), behaviour (p) | ||
| 15 normal stature | ||||||||
| Theunissen et al8 | 18 ISS | 18 ISS | 4–10 years | Prospective: comparison of CON and EXP before and after 1 and 2 years GH treatment | = quality of life (p, c, ph), perception of self (c); ↓ social functioning (c) | Quality of life: vitality, scholastic competence, physical complaints (c), positive emotions (p) | Quality of life(p), social functioning, self‐esteem (c) | Quality of life (ph) |
| Ross et al52 | 37 ISS | 31 ISS placebo | 9–16 years | Prospective: comparison of CON and EXP before and during 4 years GH treatment | = behaviour (p), self‐concept (c) | Self‐concept (c) | Internalising, externalising, and total problem behaviour (c) | |
| Visser‐van Balen et al50 | 19 ISS/SGA | 19 ISS/SGA | 11–13 years | Prospective: comparison of CON and EXP before and yearly during 3 years GH treatment | = perceived competence, anxiety, personality, depressive mood (c), externalising behaviour (p); ↑ social and attention problems, anxious/depressed behavior (p) | Anxiety, scholastic competence, athletic competence (c) | Externalising behaviour, social and attention problems, anxious/depressed behaviour (p) |
ISS, idiopathic short stature; GHD, growth hormone deficiency; TS, Turner syndrome; SGA, born small for gestational age; CON, control group; EXP, experimental (treatment) group; CBCL, Child Behavior Check List
= same score compared to control group or general norms; ↑ higher score compared to control group; ↓ lower score compared to control group.
(p) parental reports; (c) children's self‐reports (perceived competence); (ph) physicians' reports.
Whereas pre‐ to post‐treatment assessments with standardised questionnaires generally did not reveal changes in psychosocial functioning, the retrospective perception of the hormone treatment of parents and children was generally positive. Although practical adverse effects, including daily injections with growth hormone and regular visits to the paediatrician, were mentioned, parents and children were content; parents reported a positive change regarding social functioning and self‐esteem in their children.8,23,48,53 Perhaps the commonly used standardised instruments are too generic or not sensitive enough to be able to measure changes in psychosocial functioning during hormone treatment. On the other hand, it is unlikely that relevant height specific themes are not more or less reflected in these generic instruments.10 It is also possible that the positive experiences with hormone treatment as shown by interviews are explained by “cognitive dissonance reduction”: people tend to emphasise the positive consequences of their own choices and disregard dissonant information.
Perhaps it is not the alleviation of psychosocial problems, but other factors which motivate children and their parents to want hormone treatment; for example, the appraisal of better future opportunities in society and high expectations of treatment effects in terms of gain in height. Our previous study4 suggested that parental worries about current or future functioning of their children is the most frequent motive to want hormone treatment, while only a small number of referred adolescents appeared motivated by psychosocial problems. To choose and evaluate the most suitable treatment for an individual with short stature, all motives for wanting gain in height are to be considered, not only the experience of current psychosocial problems.
In conclusion, the aggregate of studies does not show that enhancing growth by hormone treatment leads to improvement in psychosocial functioning and wellbeing.
Advantages and disadvantages of hormone treatment in ISS
To facilitate decisions on interventions in medically referred children with ISS, we reviewed and critically discussed the available research on the impact of short stature and the effects of hormone treatment on psychosocial functioning. The focus was on possible individual variation in adaptation. Based on our findings we will discuss the advantages and disadvantages of hormone treatment in children with ISS. The three main conclusions of our review are:
Parents of medically referred children with ISS ranked the behaviour of their children on average between normal and below normal. The magnitude of the behavioural deviations was judged to vary from small to large. Little is known about self‐perceived psychosocial functioning of the children. Medically referred children with ISS have, on average and according to their parents, more psychosocial problems than children with normal stature and children with short stature who are not medically referred.
Some risk factors influencing adaptation in children with ISS have been found, namely being juvenilised, being a boy, having a low intelligence, having a younger but taller brother or sister, and being part of a family with low socioeconomic status. The influence of protective factors such as specific temperamental characteristics, coping strategies, and social support variables has been hardly studied.
On average hormone treatment does not seem to improve psychosocial functioning. It is not known which individual characteristics may affect the psychosocial outcome of hormone treatment.
From the research findings, advantages as well as disadvantages for hormone treatment can be derived (table 3). In choosing a suitable intervention for individuals with idiopathic short stature, physicians, caregivers, and children must weigh these pros and cons. Besides these pros and cons, ethical, economical and practical considerations have to be taken into account.54 It is to be kept in mind that hormone treatment is a means to gain height, but not a means to solve psychosocial problems. Although a lack of sufficiently large research samples may partly explain the lack of evidence based positive effects of hormone treatment on psychosocial adjustment, the multitude of factors influencing psychosocial adjustment should also be considered. Whatever the result of the decision process may be for parents and children, it appears worthwhile to improve psychosocial adjustment by focusing on factors other than height alone.
Table 3 Considerations and findings from a psychosocial viewpoint that plead for and against height enhancing hormone treatment in children with idiopathic short stature.
| Impact of short stature | Risk and protective factors | Hormone treatment | |
|---|---|---|---|
| For | Several of the medically referred children have behavioural and social problems as evaluated by parents. Physical appearance will have consequences in terms of how people are judged and treated by others and may affect future prospects of finding a spouse or job. | Increasing height might be a solution to improve adjustment, because several risk factors affecting adjustment cannot or can hardly be manipulated, e.g. being a boy, having low intelligence, having a younger but taller sibling, or being part of a family with a low socioeconomic status. | Parents and children retrospectively perceive the hormone treatment as positive. |
| Inconclusive | The few studies that have assessed the children's opinion suggest that medically referred children themselves do not perceive psychosocial problems. It is not known whether medically referred children with idiopathic short stature have (according to their parents) psychosocial problems because of their short stature or whether short children with psychosocial problems are medically referred relatively often. | The extent to which adjustment to short stature is affected by common protective factors such as temperament, coping strategies, and support from significant others, is unknown. | Nothing is known about potential determinants of individual differences in psychosocial functioning after hormone treatment. Long term results of hormone treatment are not available yet. |
| Against | Not all medically referred children with idiopathic short stature have psychosocial problems, and short children who are not medically referred do not seem to have psychosocial problems at all. | The risk and protective factor model of adjustment offers several opportunities for psychological guidance and social interventions aimed at psychosocial stressors, coping strategies, and social support. Changing these factors might improve adjustment by protecting the child against the impact of short stature. | There are few evidence based positive effects of the treatment on psychosocial functioning. A considerable part of the hormone treated individuals remains relatively short, leading to the question of how much height needs to be gained to improve psychosocial functioning. |
Footnotes
Competing interests: none declared
References
- 1.Wit J M. Growth hormone therapy. Best Pract Res Clin Endocrinol Metab 200216483–503. [DOI] [PubMed] [Google Scholar]
- 2.Ranke M B. Towards a consensus on the definition of idiopathic short stature. Horm Res 199645(suppl 2)64–66. [DOI] [PubMed] [Google Scholar]
- 3.Sandberg D E, Colsman M. Growth hormone treatment of short stature: status of the quality of life rationale. Horm Res 200563275–283. [DOI] [PubMed] [Google Scholar]
- 4.Visser‐van Balen H, Geenen R, Kamp G A.et al Motives for choosing growth‐enhancing hormone treatment in adolescents with idiopathic short stature: a questionnaire and structured interview study. BMC Pediatr 2005515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kranzler J H, Rosenbloom A L, Proctor B.et al Is short stature a handicap? A comparison of the psychosocial functioning of referred and nonreferred children with normal short stature and children with normal stature. J Pediatr 200013696–102. [DOI] [PubMed] [Google Scholar]
- 6.Voss L D. Short normal stature and psychosocial disadvantage: a critical review of the evidence. J Pediatr Endocrinol Metab 200114701–711. [DOI] [PubMed] [Google Scholar]
- 7.Noeker M, Haverkamp F. Adjustment in conditions with short stature: a conceptual framework. J Pediatr Endocrinol Metab 2000131585–1594. [DOI] [PubMed] [Google Scholar]
- 8.Theunissen N C, Kamp G A, Koopman H M.et al Quality of life and self‐esteem in children treated for idiopathic short stature. J Pediatr 2002140507–515. [DOI] [PubMed] [Google Scholar]
- 9.Erling A, Wiklund I, Albertsson‐Wikland K. Prepubertal children with short stature have a different perception of their well‐being and stature than their parents. Qual Life Res 19943425–429. [DOI] [PubMed] [Google Scholar]
- 10.Theunissen N C, Vogels T G, Koopman H M.et al The proxy problem: child report versus parent report in health‐related quality of life research. Qual Life Res 19987387–397. [DOI] [PubMed] [Google Scholar]
- 11.Haverkamp F, Eiholzer U, Ranke M B.et al Symptomatic versus substitution growth hormone therapy in short children: from auxology towards a comprehensive multidimensional assessment of short stature and related interventions. J Pediatr Endocrinol Metab 200013403–408. [DOI] [PubMed] [Google Scholar]
- 12.Erling A. Why do some children of short stature develop psychologically well while others have problems? Eur J Endocrinol 2004151(suppl 1)35–39. [DOI] [PubMed] [Google Scholar]
- 13.Siegel P. The psychological adjustment of short children and normal controls. In: Stabler B, Underwood LE, eds. Growth, stature, and adaptation. Chapel Hill: University of North Carolina, 1994123–134.
- 14.Skuse D, Gilmour J, Tian C S.et al Psychosocial assessment of children with short stature: a preliminary report. Acta Paediatr Suppl 199440611–17. [DOI] [PubMed] [Google Scholar]
- 15.Richman R A, Gordon M, Tegtmeyer P.et al Academic and emotional difficulties associated with constitutional short stature. In: Stabler B, Underwood LE, eds. Slow grows the child: psychosocial aspects of growth delay. Hillsdale, NJ: Lawrence Erlbaum Associates, 198613–26.
- 16.Sandberg D E, Brook A E, Campos S P. Short stature: a psychosocial burden requiring growth hormone therapy? Pediatrics 199494832–840. [PubMed] [Google Scholar]
- 17.Gordon M, Crouthamel C, Post E M.et al Psychosocial aspects of constitutional short stature: social competence, behavior problems, self‐esteem, and family functioning. J Pediatr 1982101477–480. [DOI] [PubMed] [Google Scholar]
- 18.Sandberg D E. Short stature in middle childhood: a survey of psychosocial functioning in a clinic‐referred sample. In: Stabler B, Underwood LE, eds. Growth, stature, and adaptation. Chapel Hill: University of North Carolina, 199419–34.
- 19.Gilmour J, Skuse D. Short stature—the role of intelligence in psychosocial adjustment. Arch Dis Child 19967525–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zebrowitz L A, Collins M A, Dutta R. The relationship between appearance and personality across the life span. Pers Soc Psychol Bull 199824736–749. [Google Scholar]
- 21.Langlois J H, Kalakanis L, Rubenstein A J.et al Maxims or myths of beauty? A meta‐analytic and theoretical review. Psychol Bull 2000126390–423. [DOI] [PubMed] [Google Scholar]
- 22.Harter S.The construction of the self. A developmental perspective. New York, London: The Guilford Press, 1999
- 23.Huisman J. Medisch‐psychologische bijdragen aan nieuwe behandelingswijzen in de kindergeneeskunde (The contribution of behavioral medicine to interventions in pediatrics), PhD thesis. Amsterdam: Free University, 1993
- 24.Holmes C S, Karlsson J A, Thompson R G. Longitudinal evaluation of behavior patterns in children with short stature. In: Stabler B, Underwood LE, eds. Slow grows the child: psychosocial aspects of growth delay. New Jersey: Lawrence Erlbaum Associates, 19861–12.
- 25.Stabler B, Clopper R R, Siegel P T.et al Academic achievement and psychological adjustment in short children. The National Cooperative Growth Study. J Dev Behav Pediatr 1994151–6. [DOI] [PubMed] [Google Scholar]
- 26.Sandberg D E, Michael P. Psychosocial stress related to short stature: does their presence imply psychological dysfunction? In: Drotar D, ed. Measuring health‐related quality of life in children and adolescents; implications for research and practice. Mahwah, NJ: Lawrence Erlbaum Associates, 1998287–312.
- 27.Erling A, Wiklun I, Albertsson Wikland K. Psychological functioning in boys of short stature: effects of different levels of growth hormone secretion. Acta Paediatr 200291966–971. [DOI] [PubMed] [Google Scholar]
- 28.Sartorio A, Morabito F, Peri G.et al The social outcome of adults with constitutional growth delay. J Endocrinol Invest 199013593–595. [DOI] [PubMed] [Google Scholar]
- 29.Busschbach J J, Rikken B, Grobbee D E.et al Quality of life in short adults. Horm Res 19984932–38. [DOI] [PubMed] [Google Scholar]
- 30.Crowne E C, Shalet S M, Wallace W H.et al Final height in boys with untreated constitutional delay in growth and puberty. Arch Dis Child 1990651109–1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zimet G D, Owens R, Dahms W.et al The psychosocial functioning of adults who were short as children. In: Haverkamp F, Voss L, eds. Growth, stature, and psychosocial well‐being. Seattle/Toronto: Hogrefe & Huber Publishers, 199947–58.
- 32.Sandberg D E, Voss L D. The psychosocial consequences of short stature: a review of the evidence. Best Pract Res Clin Endocrinol Metab 200216449–463. [DOI] [PubMed] [Google Scholar]
- 33.Voss L D, Mulligan J. Bullying in school: are short pupils at risk? Questionnaire study in a cohort. BMJ 2000320612–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ulph F, Betts P, Mulligan J.et al Personality functioning: the influence of stature. Arch Dis Child 20048917–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sandberg D E, Bukowski W M, Fung C M.et al Height and social adjustment: are extremes a cause for concern and action? Pediatrics 2004114744–750. [DOI] [PubMed] [Google Scholar]
- 36.Sandberg D E, Kranzler J, Bukowski W M.et al Psychosocial aspects of short stature and growth hormone therapy. J Pediatr 1999135133–134. [DOI] [PubMed] [Google Scholar]
- 37.Cohen J.Statistical power analysis for the behavioral sciences. New York: Academic Press, 1977
- 38.Wallander J L, Varni J W, Babani L.et al Disability parameters, chronic strain, and adaptation of physically handicapped children and their mothers. J Pediatr Psychol 19891423–42. [DOI] [PubMed] [Google Scholar]
- 39.Sandberg D E. Experiences of being short: should we expect problems of psychosocial adjustment? In: Eiholzer U, Haverkamp F, Voss LD, eds. Growth, stature, and psychosocial well‐being. Seattle/Toronto: Hogrefe & Huber Publishers, 199915–26.
- 40.Hunt L, Hazen R A, Sandberg D E. Perceived versus measured height. Which is the stronger predictor of psychosocial functioning? Horm Res 200053129–138. [DOI] [PubMed] [Google Scholar]
- 41.Lundgren E M, Cnattingius S, Jonsson B.et al Intellectual and psychological performance in males born small for gestational age. Horm Res 200359(suppl 1)139–141. [DOI] [PubMed] [Google Scholar]
- 42.van Pareren Y K, Duivenvoorden H J, Slijper F S.et al Intelligence and psychosocial functioning during long‐term growth hormone therapy in children born small for gestational age. J Clin Endocrinol Metab 2004895295–5302. [DOI] [PubMed] [Google Scholar]
- 43.Hensley W E. Height as a basis for interpersonal attraction. Adolescence 199429469–474. [PubMed] [Google Scholar]
- 44.Feiring C, Taska L S. Family self‐concept: ideas on its meaning. In: Bracken B, ed. Handbook of self‐concept: developmental, social, and clinical considerations. Oxford: John Wiley & Sons, 1996317–373.
- 45.Starke M, Erling A, Moller A.et al Family function in families with children of normal height and in families with short children. Acta Paediatr 200089983–988. [DOI] [PubMed] [Google Scholar]
- 46.Boulton T J, Dunn S M, Quigley C A.et al Perceptions of self and short stature: effects of two years of growth hormone treatment. Acta Paediatr Scand Suppl 199137720–28. [DOI] [PubMed] [Google Scholar]
- 47.Pilpel D, Leiberman E, Zadik Z.et al Effect of growth hormone treatment on quality of life of short‐stature children. Horm Res 1995441–5. [DOI] [PubMed] [Google Scholar]
- 48.Rekers‐Mombarg L T, Busschbach J J, Massa G G.et al Quality of life of young adults with idiopathic short stature: effect of growth hormone treatment. Dutch Growth Hormone Working Group. Acta Paediatr 199887865–870. [DOI] [PubMed] [Google Scholar]
- 49.Downie A B, Mulligan J, McCaughey E S.et al Psychological response to growth hormone treatment in short normal children. Arch Dis Child 19967532–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Visser‐van Balen H, Geenen R, Moerbeek M.et al Psychosocial functioning of adolescents with idiopathic short stature or persistent short stature born small for gestational age during three years of combined growth hormone and gonadotropin‐releasing hormone agonist treatment. Horm Res 20056477–87. [DOI] [PubMed] [Google Scholar]
- 51.Stabler B, Frank N C. Quality of life and the psychiatric status of individuals treated with growth hormone in childhood. In: Drotar D, ed. Measuring health‐related quality of life in children and adolescents; implications for research and practice. Mahwah: Lawrence Erlbaum Associates, 1998273–286.
- 52.Ross J L, Sandberg D E, Rose S R.et al Psychological adaptation in children with idiopathic short stature treated with growth hormone or placebo. J Clin Endocrinol Metab 2004894873–4878. [DOI] [PubMed] [Google Scholar]
- 53.Leiberman E, Pilpel D, Carel C A.et al Coping and satisfaction with growth hormone treatment among short‐stature children. Horm Res 199340128–135. [DOI] [PubMed] [Google Scholar]
- 54.Macklin R. Ethical dilemmas in pediatric endocrinology: growth hormone for short normal children. J Pediatr Endocrinol Metab 200013(suppl 6)1349–1352. [DOI] [PubMed] [Google Scholar]