Abstract
Ataxia telangiectasia is a rare, multiorgan neurodegenerative disorder with enhanced vulnerability to cancer and infection. Median survival in two large cohorts of patients with this disease, one prospective and one retrospective, is 25 and 19 years, with a wide range. Life expectancy does not correlate well with severity of neurological impairment.
Keywords: survival analysis, cancer, ataxia telangiectasia
Children and adults with ataxia telangiectasia suffer from increased mortality because of lymphoreticular malignancy, infections of the respiratory system, and various rare complications.1 Because ataxia telangiectasia is uncommon, a reasonable assessment of life span, outside of one large survey, has not been possible.2 However, assembly of two cohorts, one prospective from the Ataxia Telangiectasia Clinical Center at Johns Hopkins (ATCC), and one retrospective, from the Ataxia Telangiectasia Children's Project (ATCP), allows for a reasonable estimate of lifespan.
Methods
Since 1995, 230 individuals have been referred for evaluation at the ATCC because of a suspicion of possible ataxia telangiectasia. The diagnosis, made by a constellation of features,3 was considered unambiguous in 183 patients; none was known to have a potentially lethal complication at the time of the initial assessment.
Once seen, patients in the ATCC cohort with a confirmed diagnosis of ataxia telangiectasia are thereafter followed by phone contact or follow up visits. There were 24 deaths through the end of 2004. To estimate the median age at death, a modification of the Kaplan–Meier survival function was employed. This modification makes use of the Cox proportional hazards method to account for loss to follow up (right censoring observations of six individuals) and for staggered entry based on age (left censoring).4,5 Through the use of these methods, the estimates of median survival have been shown to be robust and are based solely on the observed time.
A second cohort of patients with presumed ataxia telangiectasia has been assembled by the disease specific voluntary organisation, the ATCP. Ninety five deaths, extending from 1968 to the present, were identified, along with the age at time of death. The diagnosis of ataxia telangiectasia is unconfirmed in this cohort, but our experience suggests that the diagnosis will be correct in the vast majority. This is because incorrect or uncertain diagnosis is highly correlated with young age. Many live patients are common to both the ATCC and the ATCP cohorts, but their number and identities are not shared for reasons of privacy protection.
The institutional review board of the Johns Hopkins Medical Institutions approved the study, and informed consent was obtained from every subject seen at the ATCC. Information from the ATCP was provided without any personal health information.
Results
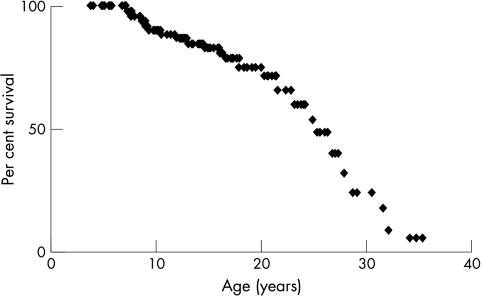
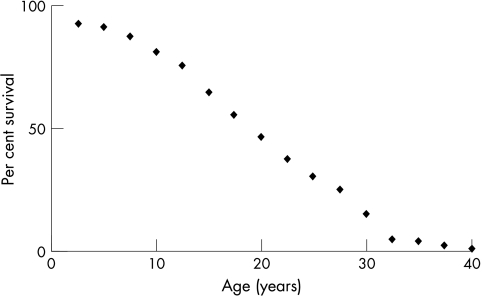
In the prospective ATCC cohort, median survival is calculated to be 25 years (fig 1). In the retrospective ATCP cohort, median survival is 19 years (fig 2). Both cohorts show that age at time of death extended over a wide range. Mortality crossed the 25th and 75th centiles in the prospective ATCC cohort at ages 18 and 28, and at ages 14 and 28 in the retrospective ATCP cohort.
Figure 1 Survival function of ATCC cohort. ATCC, Ataxia Telangiectasia Clinical Center at Johns Hopkins Hospital.
Figure 2 Per cent survival of ATCP cohort (bin width, 2.5 years). ATCP, Ataxia Telangiectasia Children's Project.
Discussion
Although calculated from a smaller number of deaths, we believe the prospective ATCC estimate to be the more accurate of the two different studies, because of methodological concerns associated with retrospective data collection in the ATCP cohort. It is also possible, however, that the difference in these two cohorts reflects a trend of improving survival in more recent years with advances in care. The median date of death in the ATCP cohort was 1993, compared with the median date of death in the ATCC cohort of 2001. The median survival of the older ATCP cohort is similar to that summarised from the two previous overlapping surveys, published in 1972 and 1984.2
Our experience suggests that determination of cause of death for many individuals with ataxia telangiectasia is difficult because of limitations in medical care and records of care, low necropsy rates, frequent unexpected diagnoses in necropsied individuals, and a high incidence of multiple diagnoses. With this significant qualification in mind, however, we can make some approximate statements as to cause of death among the patients in the ATCC cohort: nine apparently died of complications of chemotherapy or cancer, seven of pneumonia, four had significant acute neurological deterioration associated with multiple CNS telangiectatic vascular abnormalities, two died from sudden unknown causes, and two died from complications of chronic lung disease. Overall, many deaths in the ATCC cohort resulted from cancer, or relatively short duration, subacute disease that was not easily predicted from the severity of neurological or immunological dysfunction at the time of intake. Certainly severe dysphagia contributes to the incidence of acute and chronic lung disease. Only a few of the deaths, in the oldest patients, occurred in patients increasingly frail at an end stage of neurological debility, unlike the typical course of patients with other neurodegenerative disorders such as Alzheimer's, Parkinson's, or Huntington's disease. Hence most deaths should be considered to be the result of a complication of ataxia telangiectasia rather than an inevitable consequence of severe neurological debilitation.
Abbreviations
ATCC - Ataxia Telangiectasia Clinical Center at Johns Hopkins Hospital
ATCP - Ataxia Telangiectasia Children's Project
Footnotes
We wish to express our appreciation to the patients and families who have contributed their time and energies to ataxia telangiectasia research. This study was supported by the Ataxia‐Telangiectasia Children's Project, Deerfield Beach, FL and the Pediatric Clinical Research Center, The Johns Hopkins Hospital, Baltimore, MD (grant RR00052, Division of Research Resources, National Institutes of Health).
Competing interests: none declared
References
- 1.Sedgwick R P, Boder E. Ataxia telangiectasia. In: Vinken PJ, Bruyn GW, Klawans HL, et al, editors. Hereditary neuropathies and spinocerebellar atrophies, vol 60, Handbook of clinical neurology. Amsterdam: Elsevier, 1991347–423.
- 2.Morrell D, Cromartie E, Swift M. Mortality and cancer incidence in 263 patients with ataxia Telangiectasia. J Natl Cancer Inst 19867789–92. [PubMed] [Google Scholar]
- 3.Cabana M D, Crawford T O, Winkelstein J A.et al Consequences of the delayed diagnosis of ataxia‐telangiectasia. Pediatrics 199710298–100. [DOI] [PubMed] [Google Scholar]
- 4.Therneau T M, Grambsch P M.Modeling survival data: extending the Cox model. New York: Springer‐Verlag, 2000
- 5.Lin D Y, Wei L J. The robust inference for the Cox proportional hazards model. J Am Stat Assoc 1989841074–1078. [Google Scholar]