Abstract
Objective
To describe the epidemiology of imported malaria in children in the UK.
Methods
Surveillance data on children with imported malaria, collected through an enhanced surveillance network set up by the Malaria Reference Laboratory (London, UK), diagnosed between January 1999 and December 2003 were analysed.
Results
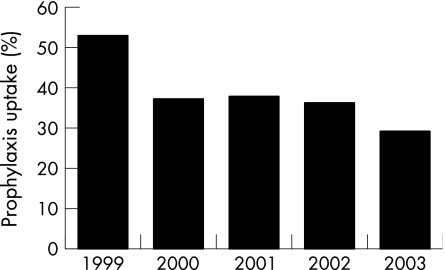
Over the 5‐year study period, 9238 cases were reported to the Malaria Reference Laboratory, and children accounted for 1456 (14.8%) cases. The number of imported paediatric malaria cases fell from 326 in 1999 to 241 in 2003. Malarial infection occurred in children of all ages and the number of patients increased gradually with age. Visiting family and relatives was the most common reason for travel (59.5%), with only 7.2% travelling to an area endemic to malaria on holiday. Most infections (88.4%) were acquired in Africa, and mainly in Nigeria (49.7%). Plasmodium falciparum was responsible for 81.7% of all cases, followed by P vivax (11.1%). The number of both P falciparum and P vivax cases fell gradually from 262 and 45 cases in 1999 to 196 and 20 cases in 2003, respectively. Malaria prophylaxis was taken by 39% of 500 children with malaria who had travelled to a country endemic to malaria. The proportion of children with malaria who had taken malaria prophylaxis decreased steadily from 53% in 1999 to 29% in 2003. Two (0.14%) children died compared with 62 (0.76%) adults over the 5‐year study period (p = 0.007).
Conclusions
Although the incidence of malaria has started to decline, a considerable number of children are still diagnosed with malaria in the UK. In addition, the proportion of children with malaria who had taken malaria prophylaxis is falling. Although it is reassuring to note the low mortality, there is an urgent need to improve preventive measures among families travelling to high‐risk countries.
Malaria remains a major cause of morbidity and mortality in adults and children worldwide.1 The UK has one of the highest rates of imported malaria among non‐endemic countries, second only to France, with around 2000 cases reported every year (http://data.euro.who.int/CISID/?TABID = 98149).2,3 The number of cases due to Plasmodium falciparum, the species responsible for most of the morbidity and mortality associated with malaria,4 continues to rise and is now responsible for >75% of all malaria cases in almost all European countries.2,3,5,6 Children under the age of 16 years account for a considerable proportion (10–20%) of imported malaria cases.7,8 Compared with adults, they are more likely to present with non‐specific febrile illnesses and their condition can deteriorate rapidly with rapid increases in blood parasite densities, particularly if they have not been exposed to malaria previously.7 Despite this, the diagnosis of malaria continues to be missed, mainly because a travel history is not obtained and malaria is not suspected.9 Studies in adults and children have consistently shown that delays in initiating appropriate treatment for malaria is one of the most important risk factors for the development of serious complications or death.5,10,11
We describe recent trends in the epidemiology, the Plasmodium species responsible, uptake of malaria prophylaxis and outcome in children with imported malaria in the UK over a 5‐year period. It is hoped that this study will increase the awareness of imported malaria in children.
Methods
Imported malaria describes an infection that was acquired in an area endemic to malaria by an individual—either a tourist or a native—but was diagnosed in a non‐endemic area after the development of clinical symptoms. An enhanced surveillance network was set up by the Health Protection Agency and Malaria Reference Laboratory (MRL, London School of Hygiene and Tropical Medicine, London, UK) in the mid‐1980s after a dramatic rise in the incidence of imported malaria in most western European countries.2 This enhanced surveillance is independent of the mandatory notification system that requires doctors to inform the designated consultant in communicable disease control within their local authority about all cases of certain infectious diseases (including malaria).12 The MRL identifies malaria cases from routine reports of all positive malaria slides sent by UK hospital laboratories to the Health Protection Agency and from those sent to the MRL for species verification. The MRL also receives notifications of all deaths caused by malaria in the UK. For each case, the MRL sends a two‐page questionnaire to the hospital clinician or general practitioner responsible for the patient, requesting information on the patient's age, sex, ethnicity, country of birth, countries travelled to, uptake of prophylaxis, species responsible and outcome. The information collected is entered into a computer database, which is screened regularly to identify and remove any duplication of cases.
Results
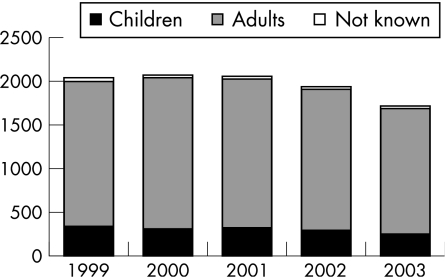
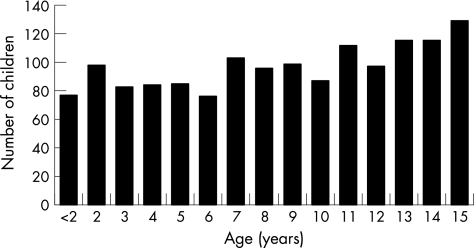
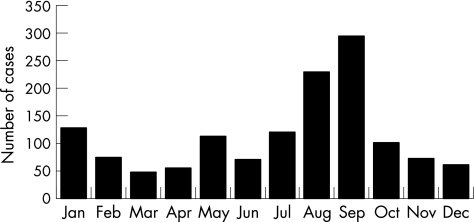
Over the 5‐year study period, 9238 cases were reported to the MRL. The incidence of imported malaria peaked to 2069 cases in 2000 and then declined gradually in the next 3 years to its lowest (1722) in 2003 (fig 1). Children under the age of 16 years accounted for 1456 (14.8%) cases (range 14.0–15.9% of all cases per year). Most cases occurred in children from the UK visiting countries endemic to malaria (70.5%). Around 62% of cases occurred in males. Malaria infection occurred in children of all ages and the number of cases increased gradually with age (fig 2). A bimodal seasonal distribution was observed, with a large peak in July–August and a smaller peak in January–February, reflecting increased travel during school holidays (fig 3).
Figure 1 Total number of malaria cases in the UK (1999–2003).
Figure 2 Number of malaria cases in children by age (1999–2003).
Figure 3 Month of diagnosis of malaria in 1370 children over the 5‐year study period.
Almost half the number of children with malaria (47.4%) were born in Africa—mainly west Africa (44.3% of all children). Most of the children born in Africa came from Nigeria (43.2%), Ghana (16.1%) or Uganda (13.1%). A similar proportion was born in the UK (44.3%). Almost all infections in children were acquired in Africa (88.4%) or Asia (10.8%), with a handful of cases reported from the Middle and Far East, Central America and the Oceanic Islands. In Africa, Nigeria (49.7%), Ghana (15.9%) and Uganda (8.8%) accounted for most cases, with <5% of infections reported from any other African country. Infections in Asia were acquired mainly in Pakistan (75.6%), followed by India (11.8%) and Afghanistan (11%). One case of congenital malaria was also found.
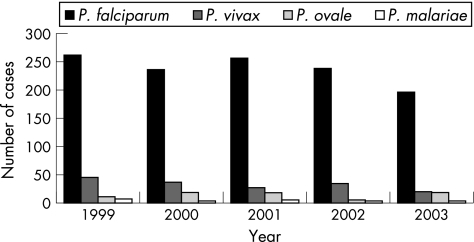
P falciparum was responsible for 81.7% of all cases of paediatric malaria, followed by P vivax (11.1%), P ovale (4.9%) and P malariae (1.5%). All cases of P ovale and P malariae infections and 99.2% of P falciparum infections were acquired in Africa. Nigeria (51.2%), Ghana (15.9%) and Uganda (8.3%) accounted for almost three quarters of all P falciparum cases. By contrast, 87.9% of P vivax infections were acquired in Asia, with only 12 (8.6%) cases reported from Africa. The number of P falciparum and P vivax cases fell gradually from 262 and 45 cases in 1999 to 196 and 20 cases in 2003, respectively (fig 4).
Figure 4 Plasmodium species responsible for malaria in children (by year).
Information regarding the reason for travel was available for 846 children. Visiting family and relatives was the most common reason for travel (59.5%), with only 7.2% of children travelling to an area endemic to malaria on holiday. Over the 5‐year period, the proportion of children travelling to visit family and relatives increased from 51% to 60%, whereas the proportion travelling on holiday fell from 13% to 5%. In all, 160 (18.9%) children were new entrants to the UK and 78 (9.2%) children fell ill while on holiday in the UK.
Information about malaria prophylaxis was available for 500 of 599 (83.5%) children with malaria who had travelled from the UK to countries endemic to malaria (table 1). Malaria prophylaxis was taken by 39.0% of the children. The proportion of children with malaria who had taken malaria prophylaxis decreased considerably from 1999 to 2003 (fig 5). Children travelling on holiday were more likely to take malaria prophylaxis compared with children visiting relatives (56.9% v 37.4%). Interestingly, only 5.1% of 59 children travelling outside Africa took malaria prophylaxis compared with 43.5% of 439 children travelling to Africa (χ2 = 32.3, p<0.001). The most common reason for travel in both groups was visiting family and relatives (83.6% of 439 children travelling to Africa and 91.5% of 50 travelling outside Africa). Only 7% of children with P vivax infection took malaria prophylaxis compared with 29% of P ovale, 43.8% of P falciparum and 57.1% of P malariae infections. Information about compliance during travel and completion of the recommended course were not routinely collected.
Table 1 Information on malaria prophylaxis for 500 of 599 (83.5%) children travelling to countries endemic to malaria.
| Malaria prophylaxis | No of children |
|---|---|
| None taken | 303 |
| Chloroquine plus paludrine | 65 |
| Chloroquine only* | 44 |
| Paludrine only | 30 |
| Mefloquine | 25 |
| Taken but antimalarial not known | 20 |
| Pyrimethamine plus dapsone | 7 |
| Daraprim | 4 |
| Fansidar | 1 |
| Homeopathic medication | 1 |
| Total | 500 |
*85.1% of children taking chloroquine prophylaxis travelled to west Africa and 10.6% to east Africa.
Figure 5 Prophylaxis uptake in 500 of 599 children with malaria who had travelled from the UK to a country endemic to malaria (1999–2003).
Two (0.14%) children died compared with 62 adults (0.76%) over the 5‐year study period (χ2 = 7.19, p = 0.007). Both children, aged 9 and 11 years, had travelled to west Africa to visit friends and relatives and both died of P falciparum malaria, with a peripheral parasitaemia >10%. One had taken appropriate prophylaxis while abroad but stopped on returning to the UK. This child became unwell a week after returning to the UK, but the diagnosis was made 4 days later and the child died in hospital on the same day. The second child had not taken any prophylaxis and initially presented with fever, vomiting and abdominal pain. This child was examined by two doctors on two separate occasions and was diagnosed with a urinary tract infection. Two days later, the child was brought back to the emergency department by ambulance, but remained unresponsive after having had an asystolic cardiac arrest in the ambulance, and further resuscitation was unsuccessful.
Discussion
The enhanced surveillance network coordinated by the MRL provides important information about trends in the epidemiology of imported malaria in the UK. Over the 5‐year study period, 9238 cases of imported malaria were reported to the MRL. The number of cases peaked in 2000–1 and has been declining since, reaching 1722 cases in 2003. Since 1985, the number of cases per year in the UK has dropped below 1800 only twice—1674 cases in 1988 and 1629 cases in 1992.2 Children under the age of 16 years accounted for almost 15% of all cases and this proportion remained between 14% and 16% since the early 1990s.7 A clear seasonality is found to be associated with imported malaria in children, with a distinct peak in the summer months and a smaller peak in the winter months (fig 3). These peaks coincide with children travelling during school holidays and have been observed in previous studies.9,13,14,15,16 In keeping with adult data, the total number of paediatric cases has been falling, after a peak of 416 cases in 1996 (data not shown) to 326 in 1999 and 241 in 2003. This fall is due to a decrease in malaria caused by all Plasmodium species. In particular, the number of cases of P vivax has decreased dramatically. In the UK, P vivax was the major species responsible for malaria until 1987, after which P falciparum became the predominant species.5 In children, the number of P vivax cases almost halved from 374 cases to 206 cases over the 5‐year study period, a trend that has continued at least since the early 1990s. Between 1991 and 1995, P vivax accounted for 35.7% of all cases of paediatric malaria7 compared with 14% of cases between 1999 and 2003. At the same time, the proportion of cases due to P falciparum increased from 37% in the mid‐1980s to 56% in 1991–57 and 81.7% in 1999–2003. Several possible reasons explain the recent drop in the number of P vivax cases. Firstly, this trend probably reflects changes in travel patterns, with increasing travel to and from Africa, which is the major source of P falciparum infection. Between 1991 and 1995, for example, 34% of all infections were acquired in the Indian subcontinent7 compared with only 9.5% in 1999–2003. Secondly, families travelling to the Indian subcontinent may now stay in large urbanised cities, where the risk of acquiring malaria is considerably lower than in rural areas. Thirdly, families who travel often may self‐medicate with antimalarials acquired abroad when they develop fever. Finally, people developing P vivax malaria generally do not require hospitalisation and are usually managed in the community by the general practitioner. Such cases are less likely to be reported to the MRL and therefore result in a reporting bias.
Information about malaria prophylaxis was available for almost 85% of children with malaria. Around 40% of children with malaria who had travelled from the UK to a country endemic to malaria had taken some form of prophylaxis, but it was not possible to determine whether they took it regularly or completed the recommended course. These findings are similar to two other recent UK studies that reported prophylaxis uptake in 42% of 173 children with malaria in east London between 1996 and 2001 (although only 15% took them, according to recommended guidelines),9 and 41% of 249 children in southwest London between 1975 and 1999.13 The second study noted that although the proportion of symptomatic children returning from sub‐Saharan Africa who had taken prophylaxis remained constant over the 25 years, the total number not taking prophylaxis had increased.13 In our study, however, there was a marked and constant drop over the 5‐year study period in the proportion of children with malaria who had taken malaria prophylaxis. Furthermore, children who acquired malaria in Africa were much more likely to take malaria prophylaxis than those travelling outside Africa. These observations have not been reported previously.
One of the major reasons for the decreasing uptake of malaria prophylaxis is the recent increase in travel by families belonging to ethnic minority groups who were born in a country endemic to malaria and are now settled in the UK. These families often travel to their home towns in rural areas to visit friends and relatives for prolonged periods of weeks to months and often do not take any preventive measures (including malaria prophylaxis) because of the false assumption by the parents that they and their children are protected from malaria.5 One retrospective study of adult and paediatric malaria cases, for example, found that 78% of British Caucasian travellers took prophylaxis as compared with only 13.5% of travellers of ethnic minority origins.17
It is reassuring to note that mortality due to malaria remains low in children: a finding reported by several recent large studies on malaria.8,9,13 Unfortunately, the two deaths that did occur in children are a strong reminder to take a travel history and consider malaria in the differential diagnosis for any unwell child returning from an area endemic to malaria. Currently, there is a need for more robust clinical information on children who develop imported malaria. Information relating to whether families seek pre‐travel medical advice, clinical presentation, the risk and presentation of severe malaria, and development of any acute and long‐term complications is limited to retrospective case series, of which few include enough patients to interpret the results with any confidence. A nationwide British Paediatric Surveillance Unit study on imported malaria in children in the UK and Ireland began in January 2006 and will continue until January 2007. The British Paediatric Surveillance Unit study aims to estimate the incidence of imported childhood malaria and to describe the epidemiological features, clinical presentation, management, complications and outcome. It is hoped that this study will identify high‐risk populations and regions in the UK and Ireland and lead to the development of strategies that target such populations to prevent imported malaria by, for example, improving malaria prophylaxis uptake and directing services to provide specialist care where it is most needed. Table 2 gives a list of useful websites and references relating to imported malaria in children.
Table 2 List of useful websites and references for paediatricians.
| Useful websites |
| Health Protection Agency website for malaria: http://www.hpa.org.uk/infections/topics_az/malaria/menu.htm |
| Health Protection Agency Malaria Reference Laboratory website: http://www.hpa.org.uk/infections/topics_az/malaria/default.htm |
| British National Formulary website for antimalarials: |
| http://www.bnf.org.uk/bnf/bnf/51/4013.htm |
| London School of Hygiene and Tropical Medicine Malaria Centre website: http://www.lshtm.ac.uk/malaria/ |
| National Electronic Library of Infection (NeLi) Malaria website: |
| http://www.neli.org.uk/IntegratedCRD.nsf/NeLI_Organisms?OpenForm&Seq |
| = 2#_RefreshKW_Parasites |
| World Health Organization Malaria website: www.who.int/topics/malaria/en/ |
| Malaria prophylaxis for long‐term travellers: http://www.hpa.org.uk/cdph/issues/CDPHvol6/No3/6(3)p200‐208.pdf |
| Useful references |
| Maitland k, Nadel S, Pollard AJ, et al. Management of severe malaria in children: proposed guidelines for the United Kingdom. BMJ 2005;331:337–43. http://bmj.bmjjournals.com/cgi/content/extract/331/7512/337 |
| Anon. Severe falciparum malaria. Trans R Soc Trop Med Hyg 2000;94(Suppl 1):1–90. |
| Guidelines for malaria prevention in travellers for the United Kingdom for 2003: http://www.hpa.org.uk/cdph/issues/CDPHvol6/No3/6(3)p180‐99.pdf |
| Update to the above guidelines for malaria prevention in travellers for the United Kingdom for 2003: http://www.hpa.org.uk/infections/topics_az/malaria/pdf/further_update _guidelines.pdf |
What is already known about this topic
The UK has one of the highest reported rates of imported malaria among non‐endemic countries, with around 2000 cases every year, of which children <16 years account for 10–20%.
The number of cases due to P falciparum, the malaria species responsible for most of the morbidity and mortality, continues to rise and is now responsible for >75% of all malaria cases in almost all European countries.
What this study adds
The number of reported cases of imported childhood malaria due to all Plasmodium species has been falling since 2001.
The proportion of children with malaria who had taken malaria prophylaxis during travel has been falling every year, from 53% in 1999 to 29% in 2003.
Acknowledgements
We thank Professor Peter Chiodini and Dr Christopher Whitty for their constructive comments.
Abbreviations
MRL - Malaria Reference Laboratory
Footnotes
Competing interests: None declared.
References
- 1.Bryce J, Boschi‐Pinto C, Shibuya K.et al WHO estimates of the causes of death in children. Lancet 20053651147–1152. [DOI] [PubMed] [Google Scholar]
- 2.Sabatinelli G, Ejov M, Joergensen P. Malaria in the WHO European Region (1971–1999). Eur Surveill 2001661–65. [PubMed] [Google Scholar]
- 3.Muentener P, Schlagenhauf P, Steffen R. Imported malaria (1985–95): trends and perspectives. Bull World Health Organ 199977560–566. [PMC free article] [PubMed] [Google Scholar]
- 4.Anonymous Severe falciparum malaria. World Health Organization, Communicable Diseases Cluster. Trans R Soc Trop Med Hyg 200094(Suppl 1)S1–90. [PubMed] [Google Scholar]
- 5.Bradley D, Warhurst D, Blaze M.et al Malaria imported into the United Kingdom in 1992 and 1993. Commun Dis Rep CDR Rev 19944R169–R172. [PubMed] [Google Scholar]
- 6.Jelinek T, Schulte C, Behrens R.et al Imported falciparum malaria in Europe: sentinel surveillance data from the European network on surveillance of imported infectious diseases. Clin Infect Dis 200234572–576. [DOI] [PubMed] [Google Scholar]
- 7.Brabin B J, Ganley Y. Imported malaria in children in the UK. Arch Dis Child 19977776–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Minodier P, Lanza‐Silhol F, Piarroux R.et al Imported pediatric malaria in Marseille. Arch Pediatr 19996935–943. [DOI] [PubMed] [Google Scholar]
- 9.Ladhani S, El B H, Patel V S.et al Childhood malaria in East London. Pediatr Infect Dis J 200322814–819. [DOI] [PubMed] [Google Scholar]
- 10.Moore C S, Cheong I. Audit of imported and domestic malaria cases at Kuala Lumpur Hospital. Br J Clin Pract 199549304–307. [PubMed] [Google Scholar]
- 11.Greenberg A E, Lobel H O. Mortality from Plasmodium falciparum malaria in travelers from the United States, 1959 to 1987. Ann Intern Med 1990113326–327. [DOI] [PubMed] [Google Scholar]
- 12.McCormick A. The notification of infectious diseases in England and Wales. Commun Dis Rep CDR Rev 19933R19–R25. [PubMed] [Google Scholar]
- 13.Williams J P, Chitre M, Sharland M. Increasing Plasmodium falciparum malaria in southwest London: a 25 year observational study. Arch Dis Child 200286428–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cilleruelo Ortega M J, Mellado Pena M J, Barreiro C G.et al Malaria in childhood. Report of 26 cases. An Esp Pediatr 198828101–104. [PubMed] [Google Scholar]
- 15.Legros F, Gay F, Belkaid M.et al Imported malaria in continental France in 1996. Eur Surveill 1998337–38. [DOI] [PubMed] [Google Scholar]
- 16.Rivera‐Matos I R, Atkins J T, Doerr C A.et al Pediatric malaria in Houston, Texas. Am J Trop Med Hyg 199757560–563. [DOI] [PubMed] [Google Scholar]
- 17.Elawad B B, Ong E L. Retrospective study of malaria cases treated in Newcastle General Hospital between 1990 and 1996. J Travel Med 19985193–197. [DOI] [PubMed] [Google Scholar]