Abstract
Objectives
To determine the effectiveness of auditory integration training (AIT) or other methods of sound therapy in people with autism spectrum disorders (ASD).
Study design
A systematic review was carried out of randomised controlled trials (RCTs) of adults or children with ASD. Meta‐analysis was attempted.
Results
Six RCTs of AIT, including one crossover trial, were identified, with a total of 171 participants aged 3–39 years. 17 different outcome measures were used, with only two outcome measures used by three or more studies. Meta‐analysis was not possible owing to very high heterogeneity or presentation of data in unusable forms. Three studies did not show any benefit of AIT over control conditions. Three studies reported improvements at 3 months in the AIT group for total mean scores of the Aberrant Behaviour Checklist (ABC), which is of questionable validity. Of these, one study also reported improvements at 3 months in the AIT group for ABC subgroup scores. No significant adverse effects of AIT were reported.
Conclusion
At present there is not sufficient evidence to support its use.
Autism spectrum disorder (ASD), or autism, refers to a wide spectrum of associated cognitive and behavioural disorders. Core features include impairments in socialisation and verbal and non‐verbal communication, and restricted patterns of behaviour and interests.1 Currently, educational, communication and behavioural methods remain the mainstay of treatment.2 However, given the heterogeneity of ASD and the knowledge that there is no single known aetiology, a range of interventions and treatments have been developed. Treatments to overcome variations in auditory sensitivity commonly encountered in people with autism have been developed and are collectively called auditory integration therapies. They include auditory integration training (AIT), the Tomatis method and Samonas sound therapy.
AIT (Berard's method) was first developed in France in 1982.3 Berard postulated that abnormal sensitivity or insensitivity to certain frequencies of sound waves, regardless of overall hearing ability, was associated with a range of behaviour and learning problems,4 and that his technique of AIT would bring about a “re‐education” of the hearing process. The technique gained wide popularity after the publication of Stehli's book,5The sound of a miracle. A child's triumph over autism, which reported the complete recovery of her daughter, Georgie (diagnosed with autism and schizophrenia), after 10 h of training in Berard's clinic. AIT involves 10 h of listening to electronically modified music delivered by headphones during two half‐hour daily sessions over 10 days. The AIT device uses filtering to dampen peak frequencies to which the person is “hypersensitive”, and delivers sounds modulated by random dampening of high and low frequencies and intensities.4
Tomatis sound therapy uses electronically modified human voice and music, delivered through an “electronic ear”.6 Samonas sound therapy involves listening to compact disc recordings of filtered music, voice and sounds of nature through headphones. The therapy was developed by Steinbach, using the work of Tomatis.7
In practice, all three methods of auditory integration require listening to electronically modified music for varying periods of time and are intended to ameliorate auditory processing defects and improve concentration. Therapists seem to be practising their own version of these methods and may modify treatment to suit the individual patient. This raises theoretical concerns as to whether such methods are comparable, owing to the variation in intensity and time.
This systematic review aimed to identify, evaluate and, if appropriate, combine any evidence of the effects of AIT or other methods of delivering sound therapy in people with autism.
Methods
Inclusion and exclusion criteria
We included randomised controlled trials (RCTs) of adults or children with ASD. ASD included pervasive developmental disorders that were described in DSM‐IV8 and ICD‐109 or diagnosed using a standard diagnostic instrument. They excluded child disintegrative disorder and Rett disorder. Types of interventions included were auditory integration therapy (AIT) or other sound therapies that involve listening to music modified by filtering and modulation, where filtering entails attenuating sounds at selected frequencies and modulation refers to random alternating of high and low sounds.4 Control groups could be those having no treatment, on the waiting list, or having the usual therapy or placebo equivalent.
Standardised measures dealing with core features of autism, cognitive ability, auditory sensitivity and processing, quality of life and behaviour were considered to be suitable outcomes, and information about short‐term, medium‐term and long‐term outcomes was sought. Available information regarding adverse events was noted.
Identification of trials
We searched the Cochrane Central Register of Controlled Trials (Cochrane Library Issues 3 and 4, 2004), Medline (1966–February 2005), Embase (1980–February 2005), Cinahl (1982–March 2005), PsycINFO (1887–March 2005), Eric (1965–July 2004), Lilacs (1982–March 2002) and the Health Technology Assessment database using the search terms listed in box 1. There were no language restrictions for the search. The Lilac database search was completed in English, Spanish and Portuguese.
Search terms were modified to meet the requirements of individual databases. The search strategy was developed to maximise sensitivity. Reference lists of identified trials and review articles were searched for further relevant publications. Authors of the included trials were contacted about their research. We did not write to other known experts.
Quality assessment
Titles and abstracts from the search were screened independently by two reviewers. Articles that appeared to fulfil the inclusion criteria were retrieved for full‐text assessment and data extraction. Studies under consideration were independently evaluated for methodological quality by three reviewers. Each reviewer assigned each study to a quality category based on allocation concealment, as described in the Cochrane Reviewers' Handbook 4.2.210 (box 2). Study quality was also assessed on the basis of intention‐to‐treat analysis, standardisation and blinding of outcome assessment, and percentage lost to follow‐up. Study quality was not scored on an additive basis.
Data management
Data extraction forms were developed to collect information about study location, methods, participant characteristics (eg, age, sex), frequency of AIT or other forms of sound therapy and outcome measures. Data were extracted by two independent reviewers, and disagreements were resolved by negotiation with a third reviewer. Information from authors was obtained, detailing methods of diagnosis of the participants, randomisation and recruitment. Only one study11 published outcomes suitable for meta‐analysis. All other authors were asked to provide summary statistics suitable for meta‐analysis or de‐identified raw data.
Box 1 Search terms
1 CHILD‐DEVELOPMENT‐DISORDERS‐PERVASIVE*:ME OR
2 SPEECH‐DISORDERS*:ME OR
3 AUTIS* OR
4 (PERVASIVE and (DEVELOPMENTAL and DISORDER*)) OR
5 PDD OR
6 (LANGUAGE next DELAY*) OR
7 (COMMUNICAT* next DISORDER*) OR
8 (SPEECH next DISORDER*)) OR
9 (CHILDHOOD next SCHIZOPHRENIA) OR
10 KANNER* OR
11 ASPERG* OR
12 ((ACOUSTIC or AUDITORY) and STIMULAT*) OR
13 (AUDITORY and ((DISCRIMINAT* or PERCEPTION*) or TRAIN*)) OR
14 (AURAL next LEARN*) OR
15 ((HEARING or SOUND) and THERAP*) OR
16 (LANGUAGE near ACQUI*) OR
17 (LISTEN* near COMPREHEN*) OR
18 (PERCEPTUAL near IMPAIR*) OR
19 (SENSORY next INTEGRAT*) OR
20 TOMATIS or SAMONAS
Box 2 Allocation concealment criteria10
(A) Adequate: concealment of the allocation, eg by telephone randomisation, or by the use of consecutively numbered, sealed, opaque envelopes
(B) Unclear: uncertainty about whether the allocation was adequately concealed, eg where the method of concealment is not reported
(C) Inadequate: allocation was definitely not adequately concealed, eg open random number lists or quasi‐randomisation such as alternate days, odd/even date of birth, or hospital number
(D) Allocation not used as a criterion to assess study validity
Statistical analysis
All outcome data reported in included papers were continuous. Our initial intention was to undertake meta‐analyses, using mean difference and standard deviation to take into account differences between treatment and control groups at baseline. These data were not provided by authors. Where data were available, point estimates and standard errors were calculated from t test scores and post intervention means using comprehensive meta‐analysis software (Biostat). Assessment of suitability of data for meta‐analysis and attempted meta‐analysis was carried out using Review Manager V.4.2.2.
Consistency of results was assessed visually and by examining I2,12 a quantity which describes approximately the proportion of variation in point estimates that is due to heterogeneity rather than sampling error. This was supplemented with a test of homogeneity to determine the strength of evidence that the heterogeneity was genuine. Where heterogeneity was found, the authors looked for an explanation.
Meta‐analysis of Aberrant Behaviour Checklist (ABC) subscores was attempted using inverse variance and a random effects model with 95% confidence intervals. No other meta‐analysis was attempted because studies used different outcome measures, or because data were not available in a usable form.
Although the authors intended to use funnel plots to investigate any relationship between effect size and study precision, the number of studies was too small and the outcome measures used were too inconsistent for this method to be viable.
As meta‐analysis was not possible, neither sensitivity analysis nor subgroup analysis could be used to assess the effect of study quality, participant inclusion criteria or differences in treatment of administration.
Results
Search results
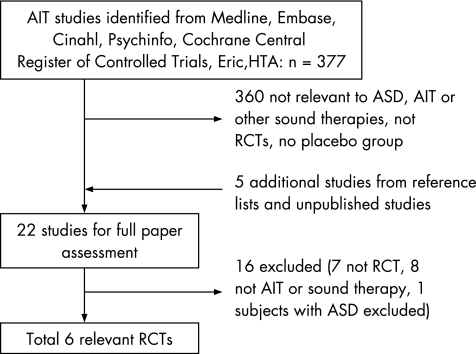
The electronic search yielded 377 titles and abstracts. Figure 1 outlines the study selection process. Six RCTs fulfilled the inclusion criteria: four RCTs from the electronic search and two from reference lists and unpublished data. No trials that used sound therapies other than AIT included participants with ASD.
Figure 1 Flow chart outlining the study selection process. AIT, auditory integration training; ASD, autism spectrum disorder; HTA, Human Technology Assessment; RCT, randomised controlled trial
Characteristics of the studies included
The number of participants in the six studies included11,12,13,14,15,16,17 ranged from 10 to 80; most studies had 20 or fewer participants (table 1). Diagnostic definitions of autism varied between trials (table 1). The participants in the trial by Zollweg et al16 included 21 people with cognitive impairment and nine people with autism. Communication with the author confirmed that all 30 participants would have fulfilled DSM‐IV criteria for an ASD; however, some had arrived in the institution before the introduction of DSM‐IV. Clinicians associated with the participants at the time reaffirmed this (Zollweg W, 15 August 2002).
Table 1 Characteristics of the studies included.
| Study | Trial type | Method of randomisation | Blinding | Duration of follow‐up (months) | Diagnostic criteria | Age (years) | Follow‐up | AIT interventions | Control condition |
|---|---|---|---|---|---|---|---|---|---|
| Bettison,13 n = 80 | Parallel RCT | Random numbers table | Outcome assessors blinded, investigators not blinded | 12 | Autism or Asperger's syndrome diagnosed by an independent agency | 3–17 | No loss to follow‐up | 2×30 min sessions for 10 consecutive days | As for AIT but music unmodified |
| Edelson et al,14 n = 18 | Parallel RCT | Telephone number | Outcome assessors blinded, investigator not blinded | 3 | Autism diagnosed by an independent agency and Rimland Diagnostic E‐2 checklist18 | 4–39 | Data from one control participant excluded due to no match in the AIT group | 2×30 min sessions for 10 consecutive days | As for AIT but music unmodified |
| Mudford et al,15 n = 16 | Crossover RCT | Geographically divided into groups, then into subgroups alphabetically, by the first letter of their name | Investigators and outcome assessors blinded | 14 | Diagnosis: autism (DSM‐IV or ICD‐10 criteria) | 5.75–13.92 | 5 lost to follow‐up due to lack of cooperation, safety issues, transport problems | 2×30 min sessions for 10 consecutive days | As for AIT, but headphones non‐functional and unmodified music played in the room (not through AIT device) |
| Rimland and Edelson,11 n = 17 | Parallel RCT | Last 2 digits of telephone number | Outcome assessors blinded, investigator not blinded | 3 | Autism diagnosed by an independent agency and Rimland Diagnostic E‐2 checklist18 | 4–21 | 1 lost to follow‐up due to transport problems | 2×30 min sessions for 10 consecutive days | As for AIT but music unmodified |
| Veale,17 n = 10 | Parallel RCT | Last 2 digits of telephone number | Outcome assessors blinded, investigator not blinded | 3 | Autism diagnosed by an independent agency | 6–10 (approximately) | No loss to follow‐up | 2×30 min sessions for 10 consecutive days | As for AIT but music unmodified |
| Zollweg et al,16 n = 30 | Parallel RCT | Random numbers table | Investigators and outcomes assessors blinded | 9 | Cognitive impairment including ASD diagnosed by an independent agency | 7–24 | 28 analysed for ABC at 9 months, 22 analysed for loudness discomfort, 14 analysed for pure tone thresholds | 2×30 min sessions for 10 consecutive days | As for AIT but music unmodified |
ABC, Aberrant Behaviour Checklist; AIT, auditory integration training; ASD, autism spectrum disorder; DSM‐IV, Diagnostic Manual of Mental Disorders (4th edn); ICD, International Classification of Diseases; RCT, randomised controlled trial.
The treatment period was uniform for all trials, consisting of AIT for 10 consecutive days, with two 30 min sessions per day. Studies used different machine models and types of music. Control conditions were the same for five studies—namely, listening to unmodified music through headphones for the same time period as for the treatment group. In one study,15 the music was played directly in the room for the control group, with non‐functional headphones.
A total of 17 different outcome measures were used in the studies. Five of the trials used the ABC19 as an outcome measure. Three studies11,15,16 presented total and subgroup scores, with the remaining two14,17 presenting total scores only. Three trials used Fisher's Auditory Problems Checklist—Parent,20 and two trials used Conners' Rating Scales—Parent,21 Leiter International Performance Scale22 or pure tone discomfort test. The 12 other outcomes were each used by only one study.
Methodological quality of included studies
Although all six studies stated that participants were randomised, no information about methods of randomisation or allocation concealment was reported in five of the papers. After contact with the authors (S Edelson, 21 September 2002, 9 May 2003; O Mudford, 5 September 2002; W Zollweg, 15 August 2002; and S Bettison, 16 September 2002) allocation concealment was deemed inadequate for all of the studies (box 2). In four of the included studies,11,13,14,17 the principal investigators were not blinded to the intervention but had little or no interaction with the outcomes assessors (as described in the study or confirmed by personal communication with the authors). The investigators were not blinded as they needed to set and give treatment.
The number of participants lost to follow‐up varied (table 1). There were considerably fewer participants for audiological and sound sensitivity data for two trials14,16 owing to the difficulty in obtaining reliable scores in the patient population. Intention‐to‐treat analysis was not used in the four trials in which there was loss to follow‐up.11,14,15,16
Five of the trials were of a parallel design and one15 was a crossover study. The crossover study included a washout period of at least 4 months between treatments. It is not certain whether the washout period was adequate.
Outcome measures
All trials used at least one standardised behaviour scale outcome. Of the five studies11,14,15,16,17 that used the ABC,19 all published total scores, including group means or difference scores. The ABC consists of five subgroup scores. The tool is not designed to calculate a total or grand mean score; therefore, a meta‐analysis of total ABC scores was not carried out (communication with Dr Michael Aman, 24 June 2003, 2 December 2004). Meta‐analysis of changes in the ABC subgroup scores 3 months post intervention was attempted for two eligible studies.11,16 Inconsistency between these studies was extremely high (I2 ranging from 55.4% for hyperactivity to 87.8% for stereotypic behaviours subgroups); therefore, meta‐analysis was deemed inappropriate. This inconsistency may have been due to the many differences between the studies, notably participant characteristics and data collection.
The largest trial13 by Bettison did not use the ABC as an outcome measure and instead used the Autism Behavior Checklist,23 which is part of a broader tool, the Autism Screening Instrument for Educational Planning.24 Using this instrument, Bettison reported improvement in both groups, but no significant between‐group differences were found when the effects of group and time and their interaction were analysed. One study11 reported a significant improvement (p<0.05) in Fisher's Auditory Problems Checklist20 scores for the treatment group at the 3‐month follow‐up. Veale17 reported no significant improvement for the Conners' Rating Scales—Parent,21 the Fisher's Auditory Problems Checklist or the ABC, only a “trending towards positive therapeutic effects” at the 3‐months follow‐up. Mudford et al15 used direct observational data in addition to behaviour rating scales.15 Overall, combined data from parents, teachers and observers did not show a benefit with AIT. No other measures of behavioural problems were used by more than one study or reported in suitable form for meta‐analysis.
Mudford et al did not report marked cognitive improvements for either the AIT or control groups after 14 months of follow‐up, whereas Bettison described improvement in both groups at 6 and 12 months. All data were presented as group mean scores before intervention and after intervention.
Sound sensitivity outcome measures differed between trials and were non‐standardised, and meta‐analysis was not possible.
Two of the trials11,13 sought to measure the adverse effects of therapy. Minor physical complaints were reported by parents in both groups for both studies, and no significant differences were found between treatment and control groups. Mudford et al15 mentioned minor side effects reported anecdotally by parents at the end of the study. Three studies14,16,17 did not report the recording of adverse events in their trials. No study reported specific deterioration in behaviour measured on a standardised test.
Discussion
In this systematic review, data synthesis was limited by statistical and clinical heterogeneity. Studies reported a disparate range of clinical outcomes, many of which were used by only one study each. Variation in statistical methods between studies was common, and data were presented in forms that could not be converted for use in meta‐analysis software. The largest studies13,16 did not report a difference between treatment and control conditions. A power analysis to calculate sample size was carried out in only one study13 (using two standardised behavioural checklists) and included a total of 80 participants. One small crossover trial15 also reported no long‐term benefits of AIT. Although three small trials11,14,17 reported an improvement in ABC scores in the AIT group at 3 months, the clinical relevance of these results is uncertain, because the total score of the ABC is not, according to the person who developed the instrument, a clinically meaningful outcome.19 The author of the instrument has stated that the use of a “total aberrant score” is incorrect and inconsistent with the instrument's design. Results should be presented as the five subscale scores.19 The only trial that used such subscales11 did note a statistically significant improvement in ABC subscale scores in the AIT group at 3 months. The age range of participants was wide in this review. It was not possible to analyse the results for different age groups, nor was this discussed in any of the studies. Given that language skills are best acquired in young children, it is possible that greater improvements would be seen in a younger sample or that improvement in language in younger participants might be blinded by fewer gains in a generally older sample. Likewise, duration of follow‐up for a lifetime condition such as autism is important. Follow‐up in trials included in this review did not exceed 14 months.15
Berard4 did not specify the outputs intended for AIT. However, questions have been raised on the potential harms of AIT,25 particularly regarding whether output levels of the machines exceed safe limits. Lucker25 concluded that AIT will not put listeners at risk of hearing loss, provided practitioners use lower rather than maximal settings on the equipment. Four of the trials described the output used for their machines13,14,15,16 and described compliance with manufacturers' recommendations or adjustment to comfort level.
A statement issued by the American Academy of Pediatrics26 in 1998 suggested limitation of the use of AIT to research protocols only, based on the available information at the time. This included concerns about the validity and theoretical basis of the therapy.27 Recent reviews28,29 have reached similar conclusions. AIT continues to be practised worldwide,30 despite evidence that shows it to be still an experimental treatment at best, and one which may be only available at a considerable cost to the family.
Acknowledgements
We thank Dr Andrew Hayen, Centre for Epidemiology and Research, NSW Department of Health, and Dr Jon Deeks, University of Sydney, for their advice and assistance with meta‐analysis; Dr Jane Dennis and Jo Abbott for the Cochrane Developmental, Psychosocial and Learning Problems Group. We also thank the authors associated with the trials: Dr Tina Veale, Dr Sue Bettison, Dr Stephen Edelson, Dr Bill Zollweg and Dr Oliver Mudford.
Abbreviations
ABC - Aberrant Behaviour Checklist
AIT - auditory integration training
ASD - autism spectrum disorders
RCT - randomised controlled trial
Footnotes
Competing interests: None.
Reprints will not be available from the authors
This paper is based on a Cochrane review first published in the Cochrane Library (copyright Cochrane Library, reproduced with permission): Sinha Y, Silove N, Wheeler D, Williams K. Auditory integration training and other sound therapies for autism spectrum disorders. Cochrane Database Syst Rev 2004;(1):CD003681 (see www.thecochranelibrary.com). The Cochrane version of this review will be updated as new evidence emerges, and in response to comments and criticisms. The results of a Cochrane review can be interpreted differently, depending on people's perspectives and circumstances. Please consider the conclusions presented carefully. They are the opinions of review authors, and are not necessarily shared by The Cochrane Collaboration.
References
- 1.Filipek P A, Accardo P J, Baranek G T.et al The screening and diagnosis of autism spectrum disorders. J Autism Dev Disord 199929439–484. [DOI] [PubMed] [Google Scholar]
- 2.Barker P. Pervasive developmental disorders. In: Basic child psychiatry. 6th edn. Cambridge: Blackwell Science, 1995131–144.
- 3.Berard G.Audition egale comportement. Sainte‐Ruffine: Maisonneuve, 1982
- 4.Berard G.Hearing equals behaviour. New Canaan, CT: Keats Publishing, 1993
- 5.Stehli A.The sound of a miracle. A child's triumph over autism. New York: Doubleday, 1991
- 6.Baumgaertel A. Alternative and controversial treatments for attention deficit hyperactivity disorder. Pediatric Clin North Am 199946977–992. [DOI] [PubMed] [Google Scholar]
- 7.Boon R. Learning discoveries psychological services: Samonas sound therapy. http://home.iprimus.com.au/rboon/SamonasSoundTherapy.htm (accessed 18 Aug 2006)
- 8.American Psychiatric Association Diagnostic and statistical manual of mental disorders. 4th edn. Washington, DC: American Psychiatric Association, 1994
- 9.World Health Organisation The ICD‐10 classification of mental and behaviour disorders: diagnostic criteria for research. Geneva: World Health Organisation, 1993
- 10.Higgins J P T, Green S. eds. Selection bias. Cochrane Handbook for systematic reviews of interventions 4.2.5 (updated May 2005), Section 6. 3. http://www.cochrane.org/resources/handbook/hbook.htm (accessed 18 Aug 2006)
- 11.Rimland B, Edelson S. Brief report: a pilot study of auditory integration training in autism. J Autism Dev Disord 19952561–70. [DOI] [PubMed] [Google Scholar]
- 12.Higgins J P T, Thompson S. Quantifying heterogeneity in meta‐analysis. Stat Med 200221539–1558. [DOI] [PubMed] [Google Scholar]
- 13.Bettison S. The long‐term effects of auditory training on children with autism. J Autism Dev Disord 199626361–374. [DOI] [PubMed] [Google Scholar]
- 14.Edelson S, Arin D, Bauman M.et al Auditory integration training: a double‐blind study of behavioural and electrophysiological effects in people with autism. Focus Autism Other Dev Disabil 19991473–81. [Google Scholar]
- 15.Mudford O, Cross B, Breen S.et al Auditory integration training for children with autism: no behavioural benefits detected. Am J Mental Retard 2000105118–129. [DOI] [PubMed] [Google Scholar]
- 16.Zollweg W, Palm D, Vance V. The efficacy of auditory integration training: a double blind study. Am J Audiol 1997639–47. [Google Scholar]
- 17.Veale T. Effectiveness of AIT using the BCG device (Clark method): a controlled study. Proceedings of the World of Options International Autism Conference. Canada: Toronto, 16 July, 1993
- 18.Rimland B.Diagnostic checklist for behavior‐disturbed children (form E‐2). San Diego: Autism Research Institute, 1971, http://www.autismwebsite.com/ARI/intro/e23.htm (accessed 1 September 2006)
- 19.Aman M, Singh N.The aberrant behaviour checklist; manual. New York: Slosson Educational Publications, 1986
- 20.Fisher L.Fisher's auditory problems checklist (FAPC). Cedar Rapids, IA: Grant Woods Area Education Agency, 1980
- 21.Connors C K.Manual for Conners rating scales. Toronto: Multi‐Health Systems, 1990
- 22.Roid G, Miller L.Leiter International Performance Scale Instruction manual (rev. ed.). Wood Dale, IL: Stoelting, 1995
- 23.Krug D A, Arick J, Almond P. Behaviour checklist for identifying severely handicapped individuals with high levels of autistic behaviour. J Child Psychol Psychiatry 198021221–229. [DOI] [PubMed] [Google Scholar]
- 24.Krug D A, Arick J, Almond P.Autism screening instrument for educational planning. Los Angeles: Western Psychological Services, 1978
- 25.Lucker J. Is auditory integration safe? J Autism Dev Disord 199828267–268. [DOI] [PubMed] [Google Scholar]
- 26.Auditory integration training and facilitated communication for autism American Academy of Pediatrics. Committee on children with disabilities. Pediatrics 1998102431–433. [PubMed] [Google Scholar]
- 27.Gravel J. Auditory integration training: placing the burden of proof. Am J Speech Lang Pathol 19944229–247. [Google Scholar]
- 28.Goldstein H. Response to Edelson, Rimland, and Grandin's commentary. J Autism Dev Disord 200333553–555. [DOI] [PubMed] [Google Scholar]
- 29.Tochel C. Sensory or auditory integration therapy for children with autistic spectrum disorders. Succinct Timely Evaluated Evidence Rev. 2003;3. Wessex Institute for Health Research and Development, University of Southampton and Bazian Ltd. http://www.signpoststeer.org/ (accessed 18 Aug 2006)
- 30.Autism Research Institute Auditory integration training. http://www.autismwebsite.com/ARI/treatment/ait.htm (accessed 1 September 2006)