Abstract
Background and objective
Mental health problems are a public health issue affecting as many as 20% of children in modern communities. Risk factors for externalising and internalising problems can occur in infancy. Infants at high risk live in stressed families with parent mental health problems, substance misuse, relationship conflict, social isolation, financial problems or infant temperamental difficulty. Although current prevention programmes target services to high‐risk groups, targeting can stigmatise families and miss many children in need. The addition of universal prevention programmes for all families could address these concerns. This survey assessed the prevalence of infants at risk attending a primary care service as a delivery point for universal prevention.
Design
Survey of mothers of 6‐month‐old infants attending well‐child clinics across six government areas of Melbourne, Victoria, Australia, between August and September 2004. A brief survey measured sociodemographic characteristics and the following family risks: maternal depression, anxiety, stress, substance misuse, violence at home, social isolation and infant temperamental difficulty.
Results
The survey was completed by 733 mothers, representing 69% of infant births presented to the primary care service. Of these, 39% of infants were classified as at risk for developing mental health problems. The percentage of infants classified as at risk was not markedly dissimilar across socioeconomic levels (low, 42%; middle, 40%; high, 35%).
Conclusions
A substantial number of infants attending routine universal primary care are at risk of developing mental health problems. This primary care setting could provide an ideal platform for preventing early externalising and internalising problems via a universally offered, evidence‐based parenting programme.
Mental health problems are a public health issue affecting about 20% of people in modern western societies.1,2 Childhood mental health problems consist primarily of externalising and internalising problems. Externalising problems include aggression, oppositional defiance and hyperactivity; internalising problems include anxiety and depression. A quarter of children with problems have comorbidity.3 Aggression and conduct problems account for up to half of all youth clinic referrals4 and a third of crime committed is by young people, costing more than AUS$1.5 billion per year. 5 Health policies are now focused on mental health and on promoting healthy development in early childhood.6,7,8
Mental adult mental health problems originate in childhood,9,10 including infancy.11,12,13 Reviews highlight the fact that young children are at risk when they live in families with parental emotional problems, substance misuse, relationship conflict, social isolation and low income, or have a “difficult” temperament.14,15,16,17 These family stresses have been empirically associated with negative parenting,14,18,19 which directly predicts children's externalising and internalising problems.20,21
A public health approach to reducing children's mental health problems includes adequate treatment services partnered with effective prevention programmes.22,23 To date, work on the development of prevention programmes has targeted families at high risk,4,24,25,26 with encouraging results. Olds et al25 found that a 2‐year programme of home visits by nurses to adolescent, unmarried mothers of low socioeconomic status (SES) reduced the rates of child antisocial behaviour in this targeted group. However, targeted prevention for highly prevalent problems has substantial limitations. Firstly, singling out specific population groups as being at high risk can lead to stigmatisation, leading to poor uptake rates,27 and this effect could be more marked if individual mothers were selected on the basis of their own high‐risk characteristics. Secondly, the bulk of children with mental health problems are from families of middle to high SES, without parental depression or substance misuse, simply because these families numerically comprise most of modern society.23 Finally, even if prevention was targeted to preschool externalising symptoms as the most accurate predictor of future conduct disorder, the sensitivity of this measure does not exceed 50%.28 We recommend developing universal prevention programmes for all families, in addition to targeted and clinical services.
The feasibility of universal prevention reaching a broad population, as well as capturing children at risk, has yet to be established. Routine primary care is an access point for developing universal prevention parenting programmes, beginning early in childhood. This study assessed the viability for a universal parenting programme to reach a reasonable number for young children facing risks for mental health problems. We estimated the prevalence of infants living at risk in the population who attended routine early childhood primary care across socioeconomic levels. Consistent with the literature above, infants at risk were defined as living with maternal depression, anxiety, stress, substance misuse, home violence, social isolation or a difficult temperament. We hypothesised that a substantial proportion of at‐risk infants attend primary care across socioeconomic levels and could be captured by a universally offered parenting programme to promote early mental health.
Methods
This study presents baseline data from “Toddlers Without Tears” (ISRCTN 77531789), a cluster randomised trial in Victoria, Australia, evaluating a parenting programme to prevent preschool behaviour problems. Victoria has 79 local government areas (LGAs), which were ranked using the census‐derived Socio‐Economic Indexes For Areas (SEIFA)29 Index of Relative Disadvantage (Australian mean 1000 (standard deviation (SD) 100)). To ensure a broad socioeconomic range, two metropolitan LGAs were selected from each of the lowest, middle and highest tertiles of Victorian SEIFA scores.
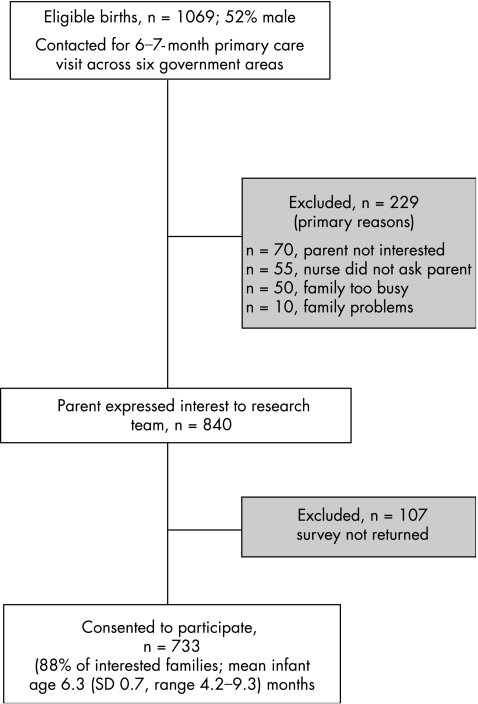
Over a 2‐month period, maternal and child health nurses in the six LGAs consecutively invited all mothers of infants attending 6–7‐month well‐child visits to participate in the trial. Using a study‐designed recruitment record, nurses preidentified all eligible babies registered at their centre turning 6 months old in February–March 2004 (1069 babies identified, 52% boys; fig 1). Mothers with insufficient knowledge of English to complete brief questionnaires were excluded. At the routine 6–7‐month visit, nurses introduced the study to each mother and forwarded contact details of interested mothers to the research team. After telephone contact with mothers to explain the study, the researchers mailed a baseline survey including written informed consent.
Figure 1 Flowchart of participants.
This survey was completed by the infant's primary care giver and included the following measures. Care giver mental health was measured by the Depression Anxiety Stress Scale (DASS),30 a 21‐item scale on which adults rate symptoms of emotional distress experienced (0, not at all; 3, most of the time). Total scores were calculated for subscales of depression, anxiety and stress (seven items for each subscale). DASS clinical cut‐off points were used to dichotomise subscale scores (no problem versus mild–severe problem: depression >9, anxiety >7 and stress >14). Kemper and Kelleher's31 health service‐screening questions (table 2) were included to assess home violence, substance misuse and social isolation (three items each). Mothers who indicated a problem on any item in each domain were scored as problematic in that domain. The Australian Temperament Project's global temperament rating scale32 measured mothers' perception of infant difficulty (1, much easier than average; 5, much more difficult than average). In Victorian normative data, 8% of parents rate their infant as more difficult than average (score 4 or 5).
Table 2 Prevalence of risk factors for developing mental health problems (n = 717–733).
| Variable, including risk definition for each risk factor | n (%) |
|---|---|
| At risk status* | 283 (39.2) |
| Maternal mental health | |
| Depression | 82 (11.3) |
| Anxiety | 58 (8.0) |
| Stress | 96 (13.2) |
| Substance misuse | |
| In the past year have you ever had a drinking problem? (Yes) | 6 (0.8) |
| Have you ever had a drug problem? (Yes) | 21 (2.9) |
| Have you used any drugs in the past 24 h? (Yes, illegal drug listed) | 4 (0.6) |
| Home violence | |
| Do you feel that you live in a safe place? (No) | 13 (1.8) |
| In the past year, have you ever felt threatened in your home? (Yes) | 47 (6.4) |
| In the past year, has your partner or other family member pushed you, punched you, kicked you, hit you or threatened to hurt you? (Yes) | 21 (2.9) |
| Social isolation | |
| Whom can you count on to be dependable when you need help? (Less than two people) | 56 (7.7) |
| How satisfied are you with their support? (Less than fairly satisfied) | 41 (5.6) |
| Can you rely on other people (eg, family, other friends) to support you in your role as a parent? (No) | 76 (10.4) |
| Perception of infant as difficult | 44 (6.1) |
*Infant classified at risk if parent reported depression, anxiety, stress, home violence, substance misuse, social isolation or infant temperamental difficulty.
Sociodemographic factors measured were infant sex, birth order, age of parents, marital status, education, cultural identity and main language spoken at home. Each family was assigned a local neighbourhood SEIFA Index of Relative Disadvantage score by home address postal code. Families had 72 separate postcodes (SEIFA mean (SD) 1044.5 (68.9), range 825–1140). We divided our sample into tertiles based on sample SEIFA scores (low, 825–1041; medium, 1046–1077; high, 1078–1140). Although the study was not designed to be fully representative (rural areas are more disadvantaged and were under‐represented), our sample included families across the socioeconomic spectrum.
Project approval (EHRC 24020A) was obtained from the Ethics in Human Research Committee of the Royal Children's Hospital, Melbourne, Victoria, Australia.
Statistical analyses
The number and percentage of infants classified as being at risk for mental health problems were based on reports of one or more risk indicators (infant perceived as difficult, parent DASS score above the clinical cut‐off point on any subscale, home violence, substance misuse or social isolation). The numbers and percentages of the sample reporting each risk separately are given by socioeconomic group. We examined the association between SES and each risk variable (yes or no) using logistic regression. As clusters (nursing centres) were sampled, within‐cluster correlation was taken into account in the analyses using the Stata33 commands svy:prop and svy:logit.
Results
Population characteristics
Figure 1 shows a flowchart of eligible and consenting participants. Of 1069 eligible families contactable for their infants' 6–7‐month health visit, 840 expressed interest in participating and 733 returned the baseline questionnaire. Table 1 gives the characteristics of the sample. Almost all primary care givers of infants were in partnered relationships. Parents spanned a broad range of educational and socioeconomic levels, and cultures (Anglo‐Australian, European, Asian, Middle Eastern, African, South American, Indian and New Zealander). Mental health of mothers in this sample (table 1) was slightly better than the Australian DASS normative data for adults in their 30s34 (normative mean (SD): depression, 5.4 (7.1); anxiety, 3.7 (5.0); stress 8.9 (8.4)).
Table 1 Sample characteristics (n = 686–733).
| Variable | Statistic |
|---|---|
| Infant | |
| Boys (%) | 51.3 |
| Family position (first born; %) | 53.4 |
| Family | |
| Maternal age in years (mean (SD), range) | 33.2 (4.7), 18.0–46.8 |
| Married/de facto (%) | 96.6 |
| Parents of Anglo‐Australian cultural identity (%) | 78.0 |
| Language other than English mainly at home (%) | 4.0 |
| Education status (% mothers/% fathers) | |
| Did not complete high school | 20.5/31.1 |
| Completed high school | 33.2/29.8 |
| Completed tertiary/postgraduate degree | 46.3/39.1 |
| Household income AUS$ (%) | |
| <30 000 | 9.9 |
| 30 000–60 000 | 32.7 |
| >60 000 | 57.4 |
| Maternal mental health (mean (SD)) | |
| Depression | 3.8 (4.9) |
| Anxiety | 2.0 (3.3) |
| Stress | 8.9 (6.4) |
Prevalence of infants at risk for developing mental health problems
Table 2 reports the prevalence of risks for early externalising and internalising problems. More than a third of infants attending the 6–7‐month health visit lived at risk in families facing stress (39%, 95% CI 36% to 43%). About 10% of mothers had depression and anxiety (mild–severe in range), and a similar proportion reported social isolation. Also, 3% (n = 21) of mothers had faced domestic violence in the past year, 3% noted problems with drugs in their history and 6% perceived their infant as temperamentally difficult.
Table 3 reports the prevalence of infants with risk factors by SES group (low, middle or high). Infants with some specific risks for early mental health problems (parent substance misuse or social isolation) were more likely to be living in socioeconomically disadvantaged areas. However, the percentage of infants at risk based on all indicators was not markedly dissimilar between the socioeconomic groups. Numerically, there were more infants at risk in locations of relative economic advantage (middle and high SES) than in locations of disadvantage (low SES). Combining middle and high socioeconomic locations, 181 infants were at risk compared with 99 from low socioeconomic locations.
Table 3 Number and percentage (95% CI) of infants with risk factors by socioeconomic status.
| Variable | Low SES (n = 238) | Middle SES (n = 241) | High SES (n = 247) | p Value | |||
|---|---|---|---|---|---|---|---|
| n | % (95% CI) | n | % (95% CI) | n | % (95% CI) | ||
| At risk status | 99 | 42.3 (36.1 to 48.5) | 95 | 40.3 (35.2 to 45.3) | 86 | 35.1 (29.7 to 40.5) | 0.18 |
| Home violence | 28 | 11.8 (6.0 to 17.6) | 18 | 7.5 (4.5 to 10.5) | 16 | 6.5 (3.7 to 9.3) | 0.18 |
| Substance misuse | 17 | 7.1 (4.2 to 10.1) | 3 | 1.3 (0.0 to 2.5) | 8 | 3.3 (0.7 to 5.8) | 0.006 |
| Social isolation | 52 | 22.2 (18.3 to 26.1) | 35 | 14.7 (11.1 to 18.3) | 35 | 14.2 (9.5 to 18.8) | 0.003 |
| Maternal mental health (mild–severe problem) | |||||||
| Depression | 28 | 11.9 (7.4 to 16.4) | 35 | 14.6 (10.1 to 19.1) | 19 | 7.8 (4.9 to 10.6) | 0.04 |
| Anxiety | 18 | 7.6 (4.1 to 11.2) | 28 | 11.9 (5.8 to 18.1) | 12 | 4.9 (1.8 to 7.9) | 0.11 |
| Stress | 32 | 13.6 (9.0 to 18.2) | 36 | 15.1 (9.7 to 20.5) | 27 | 11.0 (6.4 to 15.6) | 0.52 |
| Difficult infant temperament | 12 | 5.2 (2.9 to 7.5) | 12 | 5.1 (2.6 to 7.5) | 20 | 8.2 (4.5 to 12.0) | 0.32 |
Discussion
This study estimated that more than a third of infants routinely attending universal primary care services are at risk for developing mental health problems. Consistent with a large body of previous international research, a higher proportion of infants in socioeconomically disadvantaged areas live with family stresses (substance misuse or social isolation). However, numerically more infants living with family stress can be located in middle to high socioeconomic groups, as these comprise the bulk of populations in developed countries.
A strength of this study is that a substantial proportion (69%) of eligible parents in six Victorian government areas attending 6–7‐month health visits participated.35 In community surveys, the number of eligible participants is often unknown and response rates are reported for only those families contacted. If we took this more lenient approach, our response rate would be 88%—high for a community survey.36 In addition, our community sample was diverse with respect to parental age, education, culture and SES. Results may therefore be generalised to the Australian population. However, as eligibility criteria excluded Victorian rural shires and parents with insufficient knowledge of English to complete brief questionnaires, the findings cannot be generalised to these groups.
What is already known on this topic
Mental health problems affect as many as 20% of children.
The aetiology of paediatric mental health problems includes family and child risk factors in infancy.
What this study adds
A large number of infants at risk for developing mental health problems attend existing universal well‐child systems.
Well‐child primary care may provide an ideal universal platform for developing prevention programmes to promote early mental health.
Public health implications
We believe this study supports a public health approach for preventing mental health problems from early childhood offered universally to all families in the community, as well as targeting specialised support to families at highest risk. We do not recommend against targeted prevention, but rather for developing a tiered public mental health system including universal, targeted and tertiary interventions. Targeting evidence‐based parenting programmes only to high‐risk families or locations is likely to miss many infants who develop externalising and internalising difficulties. In Australia, the government is working towards a National Agenda for Early Childhood, including effective early intervention for parents and better coordination among community services. The 2005 Australian Institute of Health and Welfare report on Australian children highlighted the current paucity of data relevant to children's mental health and related family contexts.37 This study adds data to this gap.
Policy implications are to develop evidence‐based parenting programmes and deliver these to all families across the socioeconomic spectrum. Existing routine primary care is ideally placed to deliver such programmes, as it has regular contact with most families. For the minority of parents who are unwilling or unable to access routine primary care, targeted outreach support would be needed. We know little about the extent to which preventive early childhood parenting programmes could be delivered on a public health scale. Sustaining quality over time will be crucial and will require adequate funding for professional development of staff and evaluation of quality assurance evaluation. Developing evidence‐based parenting programmes for universal delivery in early childhood has the potential to effectively prevent mental health problems in the future.
Acknowledgements
We thank the Maternal and Child Health nurses and families from the cities of Glen Eira, Greater Geelong, Kingston, Maribyrnong, Nillumbik and Stonnington who participated in this study.
Abbreviations
DASS - Depression Anxiety Stress Scale
LGA - local government area
MCH - maternal and child health
SEIFA - Socio Economic Indexes For Areas
SES - socioeconomic status
Footnotes
Funding: This project was funded by the Telstra Community Development Fund.
Competing interests: None.
References
- 1.Anderson J C. Epidemiological issues. In: Ollendick TH, King NJ, Yule W, eds. International handbook of phobic and anxiety disorders in children and adolescents. New York: Plenum Press, 199443–65.
- 2.Sawyer M G, Arney F M, Baghurst P A.et alThe mental health of young people in Australia. Australia: Mental Health and Special Programs Branch, Commonwealth Department of Health and Aged Care, 2000
- 3.McConaughy S H, Achenbach T M. Comorbidity of empirically based syndromes in matched general population and clinical samples. J Child Psychol Psychiatr 1994351141–1157. [DOI] [PubMed] [Google Scholar]
- 4.Barlow J, Stewart‐Brown S. Review article: behaviour problems and parent training programs. J Dev Behav Pediatr 200021356–370. [DOI] [PubMed] [Google Scholar]
- 5.Bor W, Najman J M, O'Callaghan G M.et al Aggression and the development of delinquent behaviour in children. Trends and issues in crime and criminal justice. Series No: 201, Canberra: Australian Institute of Criminology 2001. http://www.aic.gov.au
- 6.Australian Health Ministers National mental health plan 2003–2008. Canberra: Australian Government, 2003
- 7.Onunaku N.Improving maternal and infant mental health: focus on maternal depression. Los Angeles: National Center for Infant and Early Childhood Health Policy at UCLA, 2005
- 8.Zeanah P, Nagle G, Stafford B, Halfon N, Rice T, Inkelas M.et al Addressing social‐emotional development and infant mental health in early childhood systems: executive summary. In: eds. Building state early childhood comprehensive systems. Series No: 12, National Center for Infant and Early Childhood Health Policy 2004
- 9.Commonwealth Department of Health and Aged Care Promotion, prevention and early intervention for mental health—a monograph. Canberra: Mental Health and Special Programs Branch, Commonwealth Department of Health and Aged Care, 2000
- 10.Tremblay R E.Developmental origins of aggression. New York: Guilford Press, 2005
- 11.Warren S L, Huston L, Egeland B.et al Child and adolescent anxiety disorders and early attachment. J Am Acad Child Adolesc Psychiatry 199736637–644. [DOI] [PubMed] [Google Scholar]
- 12.Oberklaid F, Sanson A, Pedlow R.et al Predicting preschool behaviour problems from temperament and other variables in infancy. Pediatrics 199391113–120. [PubMed] [Google Scholar]
- 13.Rothbart M K, Bates J E. Temperament. In: Damon W, Eisenberg N, eds. Handbook of child psychology. 5th edn. Vol 3. Social, emotional, and personality development. New York: Wiley, 1998105–176.
- 14.Cicchetti D, Toth S L. The development of depression in children and adolescents. Am Psychol 199853221–241. [DOI] [PubMed] [Google Scholar]
- 15.Sanders M R, Gooley S, Nicholson J.Early intervention in conduct problems in children. Adelaide, SA: The Australian Early Intervention Network for Mental Health in Young People, 2000
- 16.Shaw D S, Keenan K, Vondra J I.et al Antecedents of preschool children's internalising problems: a longitudinal study of low‐income families. J Am Acad Child Adolesc Psychiatry 1997361760–1767. [PubMed] [Google Scholar]
- 17.Shaw D S, Owens E B, Giovannelli J.et al Infant and toddler pathways leading to early externalising disorders. J Am Acad Child Adolesc Psychiatry 20014036–43. [DOI] [PubMed] [Google Scholar]
- 18.Beardslee W R, Wheelock I. Children of parents with affective disorders: empirical findings with clinical implications. In: Reynolds WM, Johnston HF, eds. Handbook of depression in children and adolescents. New York: Plenum Press, 1994463–479.
- 19.Collins W A, Maccoby E E, Steinberg L.et al Contemporary research on parenting: the case for nature and nurture. Am Psychol 200055218–232. [PubMed] [Google Scholar]
- 20.Bayer J K, Sanson A V, Hemphill S A. Parent influences on early childhood internalising difficulties. J Appl Dev Psychol 2006. in press
- 21.Brenner V, Fox R A. Parental discipline and behaviour problems in young children. J Genet Psychol 1998159251–256. [DOI] [PubMed] [Google Scholar]
- 22.Bayer J K, Oberklaid F. Happy family, happy child, happy health system. Balance J Mental Health Assoc (Queensland, Aust) 200422–27.
- 23.Offord D R, Chmura Kraemer H, Kazdin A E.et al Lowering the burden of suffering from child psychiatric disorder: trade‐offs among clinical, targeted, and universal interventions. J Am Acad Child Psychiatry 199837686–694. [DOI] [PubMed] [Google Scholar]
- 24.Beardslee W R, Versage E M, Wright E J.et al Examination of preventive interventions for families with depression: evidence of change. Dev Psychopathol 19979109–130. [DOI] [PubMed] [Google Scholar]
- 25.Olds D, Henderson C R, Cole R.et al Long‐term effects of nurse home visitation on children's criminal and antisocial behaviour: 15‐year follow‐up of a randomised controlled trial. JAMA 19982801238–1244. [DOI] [PubMed] [Google Scholar]
- 26.Rapee R M, Kennedy S, Ingram M.et al Prevention and early intervention of anxiety disorders in inhibited preschool children. J Consult Clin Psychol 200573488–497. [DOI] [PubMed] [Google Scholar]
- 27.Stewart‐Brown S. Public health implications of childhood behaviour problems and parenting programmes. In: Buchanan A, Hudson B, eds. Parenting, schooling and children's behaviour. Aldershot, UK: Ashgate Press, 199821–33.
- 28.Bennett K J, Lipman E L, Racine Y.et al Annotation: do measures of externalising behaviour in normal populations predict later outcome? Implications for targeted interventions to prevent conduct disorder. J Child Psychol Psychiatr 1998391059–1070. [PubMed] [Google Scholar]
- 29.Australian Bureau of Statistics Census Basic Community Profile and Snapshot. 2001. http://www.ausstats.abs.gov.au/ausstats/2001maps.nsf (accessed 22 Sep 2006)
- 30.Lovibond P F, Lovibond S H. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther 199533335–343. [DOI] [PubMed] [Google Scholar]
- 31.Kemper J J, Kelleher K J. Family psychosocial screening: instruments and techniques. Ambulatory Child Health 19961325–339. [Google Scholar]
- 32.Sanson A, Oberklaid F, Pedlow R.et al Risk indicators: assessment of infancy predictors of pre‐school behavioural maladjustment. J Child Psychol Psychiatry 199132609–626. [DOI] [PubMed] [Google Scholar]
- 33.StataCorp Stata Statistical Software: release 9.0. College Station, TX: Stata Corporation, 2005
- 34.Lovibond S H, Lovibond P F.Manual for the Depression Anxiety Stress scales. Sydney: Psychology Foundation Monograph, 1995
- 35.Soloff C, Lawrence D, Johnstone R.Growing up in Australia. The longitudinal study of Australian children: an Australian Government initiative. LSAC Technical Paper No: 1, Melbourne: AIFS 2005
- 36.Reuband K, Blasius J. Face‐to‐face, telephone‐ and mail questionnaires: response rates and pattern in a large city. Kolner Z Soziol Soz 199648296–318. [Google Scholar]
- 37.Australian Institute of Health and Welfare A picture of Australia's children. Canberra: Australian Institute of Health and Welfare, 2005